Abstract
Problem-based learning (PBL) is still a controversial teaching method. A study of the effectiveness of PBL compared to traditional teaching in gross anatomy courses of first year medical students was evaluated by comparing the examination performances and student’s responses to the questionnaires. It was hypothesised that the PBL method would result in improved scores and satisfaction for students. A total of 89 first year medical students at Tabriz Medical University, Iran were taught gross anatomy with traditional teaching for one half of a semester and PBL for the other one half. Examination scores from both methods and an assessment of completed questionnaires were evaluated by the present study. The PBL method resulted in better examination scores than did traditional teaching for the same students. Students were more satisfied with PBL and believed that this method increased their problem solving abilities. Our study found that PBL was more successful than traditional teaching of gross anatomy.
Keywords: anatomy, methods, instruction, medical student
Introduction:
Problem-based learning (PBL) was first developed by Howard Barrows at McMaster University in Canada in the mid 1960’s (1) and allows students to learn material by applying processes of reasoning rather than by rote memorization of facts. (2) Since its genesis, this teaching method has been the subject of considerable interest and debate in medical undergraduate and increasingly, postgraduate education.(3) The effectiveness of PBL versus conventional teaching methods has been the matter of many studies.
Meta-analyses have indicated that PBL results in performances on clinical examinations that are equal to if not better than performances following traditional teaching methods.(4–7) A number of studies have compared the basic sciences knowledge of PBL to non-PBL students. When differences in basic sciences knowledge are found, there are usually in favor of non-PBL students. (5–6, 8–9) Nandi et al. (10) stated that a combination of both traditional teaching and PBL may provide the most effective training for undergraduate medical students. Musal et al. (11) implied that the increase in PBL experience of students paralleled the development of their discussion skills using different learning resources. Abu-Hijleh et al. (12) found that senior medical students are more successful at applying anatomical concepts during surgical clerkships following a PBL curriculum. However, Hinduja et al. (13) found that students taught with a traditional course have a greater level of anatomical knowledge than those taught with an integrated course. Percac and Godenough (14) observed that PBL group discussions of clinical anatomy, after the traditional dissecting anatomy course, provided students with both horizontal and vertical integration within the curriculum.
Gross anatomy is an important basic science that if deficient in, the student may feel inadequately prepared for clinical courses thus, pinpointing the best teaching method warrants investigation. We present our findings comparing PBL to the traditional teaching for a gross anatomy course taught to first year medical students at Tabriz Medical University, Iran.
Methods
Subjects
The study sample consisted of all first year medical students at our University for 2004 (n=89). The duration of undergraduate medical education in the Iranian medical education curriculum is seven years. During the first five semesters of education, students take their basic science courses which include gross anatomy. This was the first time that PBL was implemented in the teaching of gross anatomy course with the purpose of comparing this method to the traditional one. We used written multidisciplinary anatomical problems for the problem-based procedure.(1) Table 1 demonstrates the breakdown of regions taught in our gross anatomy courses.
Table (1). Breakdown of anatomy curiculm taught to medical students.
| Lecture | Applied | |
|---|---|---|
| First Semester | Anatomy of Limbs | - |
| Second Semester | Anatomy of Trunk | Anatomy of Limbs |
| Third Semester | Anatomy of Head & Neck | Anatomy of Trunk |
| Fourth Semester | - | Anatomy of Head & Neck |
| Fifth Semester | - | - |
Procedure
For the first half of the semester during the teaching of the limbs, traditional teaching was used and an examination was taken. Student’s satisfaction from this method was evaluated by a short questionnaire. PBL methods were used for the second half of the semester, and as before, after taking an examination, student’s satisfaction was evaluated by another questionnaire. Comparison of the two methods was then performed. The examinations were composed of 10 descriptive questions, 20 yes/no questions, and 30 multiple-choice questions (MCQ). The maximal grade possible was 100 points. Both examinations were paper-based.
Questionnaires
The first questionnaire is seen below :
How much anatomical knowledge do you think you have mastered via the traditional teaching method?
Does the traditional method prevent students from group discussion? If yes, to what degree?
The second questionnaire is seen below :
How much anatomical knowledge do you think you have mastered via PBL?
Does PBL promote students’ critical thinking and reasoning of gross anatomy better than the traditional teaching method? How much?
Students could choose to answer each question in one of five ranges, 0–20%, 21–40%, 41–60%, 61–80%, and 81–100%.
Statistical Analyses
We first calculated Cronbach alpha for reliability for the questionnaires. Then, we analyzed the data extracted from the first questions of both questionnaires with a Man-Whitney U test. We used one sample sign test of median to report the students’ view about traditional teaching and PBL. We used t-test to examine the differences between the mean test scores in the examinations comparing both teaching methods. Results were obtained using statistical software SPSS and Minitab.
Results
Participants
The male and female distribution was 33.7 male and 66.3% female, respectively. The mean age of the students was 20.9 years. The results did not demonstrate any significant relationship between test scores, age, or gender. Of the 89 students, data from 83 was examined as data from six of the students were lost.
Questionnaires
An alpha of 0.93 was found for the reliability for the first questionnaire and 0.98 for the second questionnaire. Table 2 demonstrates the responses to the first question of both questionnaires.
Table (2). Students’ beliefs regarding the anatomical knowledge acquired in traditional teaching versus PBL.
| Frequency | Percent | Cumulative Percent | ||||
|---|---|---|---|---|---|---|
| Choices | Traditional Teaching | PBL | Traditional Teaching | PBL | Traditional Teaching | PBL |
| 0–20% | 30 | 6 | 34.1 | 6.8 | 34.1 | 6.8 |
| 21–40% | 30 | 6 | 34.1 | 6.8 | 68.2 | 13.6 |
| 41–60% | 14 | 12 | 15.9 | 13.6 | 84.1 | 27.3 |
| 61–80% | 7 | 27 | 8.0 | 30.7 | 92.0 | 58.0 |
| 81–100% | 7 | 37 | 8.0 | 42.0 | 100.0 | 100.0 |
| Total | 88 | 88 | 100.0 | 100.0 | ||
Students declared that they had acquired more knowledge of anatomy in PBL than the traditional teaching (p= 0.0000). For the second question of the first questionnaire, the p-value was 0.0000. Students strongly believed that traditional teaching often prevented them from group discussions (Table 3).
Table (3). Students’ beliefs regarding traditional teaching preventing group discussions.
| Choices | Frequency | Percent | Cumulative Percent |
|---|---|---|---|
| 0–20% | 7 | 8.0 | 8.0 |
| 21–40% | 7 | 8.0 | 15.9 |
| 41–60% | 18 | 20.5 | 36.4 |
| 61–80% | 26 | 29.5 | 65.9 |
| 81–100% | 30 | 34.1 | 100.0 |
| Total | 88 | 100.0 |
Table (4) demonstrates that most of the students thought that PBL had increased their creativity in relation to their understanding of anatomical concepts compared to traditional teaching (p= 0.0000).
Test Results
Statistical analyses revealed that the mean score for questions asked following a traditionally taught section was 63.3% (n = 83, SD = 25), and the mean score for questions asked following PBL was 71.6 (p <0.05) (n = 83, SD = 21.8). The total number of students participated in the study was 88 but 5 students refused to take part in the test that is why the total number of test scores are 83 while it is 88 for questionnaires.
Discussion
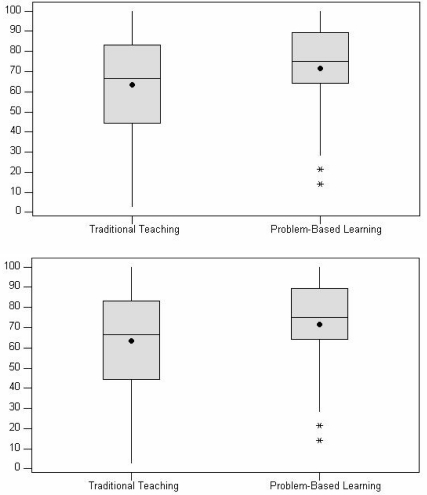
According to our results, the mean score on tests which had been taught to students traditionally and via PBL demonstrate that the PBL method was probably more effective in helping students to learn the material and gain higher scores. The differences can also be observed in the box plots of students’ scores in the examinations after traditional teaching and PBL (Fig. 1).
Fig. (1). Box plots of students’ scores for examinations following traditional teaching and PBL (the total score is 100).
Figure 1 demonstrates that the median and the mean obtained for these methods are in favor of PBL. These findings are comparable to those of other authors (4–5, 9,15) The p values obtained from our questionnaires demonstrated that the PBL improved student’s perception regarding their anatomical knowledge, which has also been reported by others e.g. Musal et al. (11)
In conclusion, the results of our study showed that first year medical students believed that PBL was effective and more beneficial than a traditional teaching regimen.
Table (4). Students’ beliefs regarding how PBL promoted their critical thinking compared to traditional teaching.
| Choices | Frequency | Percent | Cumulative Percent |
|---|---|---|---|
| 0–20% | 6 | 6.8 | 6.8 |
| 21–40% | 6 | 6.8 | 13.6 |
| 41–60% | 18 | 20.5 | 34.1 |
| 61–80% | 47 | 53.4 | 87.5 |
| 81–100% | 11 | 12.5 | 100.0 |
| Total | 88 | 100.0 |
Acknowledgments
We would like to acknowledge Prof. Mohammad Hossein Zarrintan, Department of Pharmaceutics, Faculty of Pharmacy, Tabriz University of Medical Sciences, Iran for his support during this research and preparation of the article. We would also like to thank the Student Research Center of Tabriz University of Medical Sciences, Tabriz, Iran for kind support of this research.
References
- 1.Barrows H, Tamblyn R. An evaluation of problem-based learning in small groups utilizing a stimulated patient. J Med Edu. 1976;51:52–54. [Google Scholar]
- 2.Chakravarty M, Latif NA, Abu-Hijleh MF, Osman M, Dharap AS, Ganguly PK. Assessment of anatomy in a problem-based medical curriculum. Clin Anat. 2005;18:131–136. doi: 10.1002/ca.20038. [DOI] [PubMed] [Google Scholar]
- 3.Kilroy DA. Problem-based learning. Emerg Med J. 2004;21:411–413. doi: 10.1136/emj.2003.012435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norman GR, Schmidt HG. The psychological basis of problem-based learning: a review of the evidence. Acad Med. 1992;67:557–565. doi: 10.1097/00001888-199209000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Vernon DTA, Blake RL. Does problem-based learning work? A Meta analysis of evaluative research. Acad Med. 1993;68:550–65. doi: 10.1097/00001888-199307000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Albanese MA, Mitchell S. Problem-based learning: a review of literature on its outcomes and implementation issues. Acad Med. 1993;68:52–81. doi: 10.1097/00001888-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Percac S, Armstrong EG. Introducing a problem-based learning anatomy course in a traditional curriculum: a Croatian experience. Med teacher. 1998;20:114–117. [Google Scholar]
- 8.Schmidt HG, Dauphinee WD, Patel VL. Comparing the effects of problem-based and conventional curricula in an international sample. J Med Ed. 1987;62:305–315. doi: 10.1097/00001888-198704000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Verhoeven BH, Verwijnen GM, Scherpbier AJJA, Holdrinet RSG, Oeseburg B, Bulte JA, Van der Vleuten CPM. An analysis of progress test results of PBL and non-PBL students. Medical Teacher. 1998;20:310–316. [Google Scholar]
- 10.Nandi PL, Chan JN, Chan CP, Chan P, Chan LP. Undergraduate medical education: comparison of problem-based learning and conventional teaching. Hong Kong Med J. 2000;6:301–306. [PubMed] [Google Scholar]
- 11.Musal B, Gursel Y, Taskiran HC, Ozan S, Tuna A. Perceptions of first and third year medical students on self-study and reporting processes of problem-based learning. BMC Med Educ. 2004;4:16. doi: 10.1186/1472-6920-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abu-Hijleh MF, Chakravarty M, Al-Shboul Q, Kassab S, Hamdy H. Integrating applied anatomy in surgical clerkship in a problem-based learning curriculum. Surg Radiol Anat. 2005;2:152–157. doi: 10.1007/s00276-004-0293-4. [DOI] [PubMed] [Google Scholar]
- 13.Hinduja K, Samuel R, Mitchell S. Problem-based learning: is anatomy a casualty. The Surgeon. 2005;3:84–87. doi: 10.1016/s1479-666x(05)80067-8. [DOI] [PubMed] [Google Scholar]
- 14.Percac S, Goodenough DA. Problem-based teaching and learning as a bridge from basic anatomy to clinical clerkships. Surg Radiol Anat. 1998;20:203–207. doi: 10.1007/BF01628896. [DOI] [PubMed] [Google Scholar]
- 15.Ganske I, Su T, Loukas M, Shaffer K. Teaching methods in anatomy courses in North American medical schools: the role of radiology. Acad Radiol. 2006;13:1038–1046. doi: 10.1016/j.acra.2006.03.021. [DOI] [PubMed] [Google Scholar]