Abstract
Objective:
To compare the three types of urinary diversion namely Ileal Conduit, MAINZ Pouch II and Ileal Neobladder in terms of patient preference, post-operative hospital stay, early and late complications, continence rates, quality of life and patient satisfaction.
Method:
From January 2003 to October 2007, 30 patients (28 males and 2 females) of muscle invasive carcinoma urinary bladder (mean age 57.7 years) were operated upon by radical cysto- prostatectomy or anterior pelvic exenteration and urinary diversion was performed by Ileal conduit, Mainz pouch II or Ileal neobladder. The patient preference for the type of diversion was determined pre-operatively after discussing all the three types of urinary diversions. Post-operative hospital stay, early and late complications, continence rates, quality of life and patient satisfaction with the type of diversion were evaluated on follow up.
Results:
60% of the patient’s preferred Ileal neobladder, 10% preferred Ileal conduit and 10% preferred Mainz pouch II as their 1st choice diversion; 20% left the decision to the operating surgeon. The mean post-operative hospital stay was 15.0 days in Ileal conduit group, 17.8 days in Mainz pouch II group and 19.7 days in Ileal neobladder group. The mean follow up was 27.7 months. Early complications (within 1 month of surgery) were observed in 46.2% of patients in Ileal conduit group, 38.5% in Mainz pouch II group and 50.0% in Ileal neobladder group. Late complications (after 1 month of surgery) were seen in 61.5% of patients in Ileal conduit group, 46.2% in Mainz pouch II group and 50.0% in Ileal neobladder group. In Mainz pouch II group 92.3% of the patients achieved daytime continence and 84.6% achieved night time continence 3 to 6 months after surgery. In Ileal neobladder group, 75.0% patients achieved day time continence and 50.0% achieved night time continence 3 to 6 months after surgery. Patient satisfaction and overall quality of life was described ‘Good’ by majority of patients in Ileal conduit group and ‘Very Good’ by majority of patients in Mainz pouch II group and Ileal neobladder group.
Conclusion:
There are inherited advantages and disadvantages to each form of urinary diversion and patient selection is important to identify the most appropriate method of diversion for an individual.
Introduction
Bladder cancer is the second most common cancer of the genito-urinary tract. Radical cysto-prostatectomy in male patients and anterior pelvic exenteration in female patients coupled with en-bloc pelvic lymphadenectomy remains the standard surgical approach to muscle invasive cancer of the urinary bladder in the absence of metastatic disease. Determining the optimal mode of urinary tract reconstruction following cystectomy is a challenge for the urological surgeon.
Virtually every segment of gastro-intestinal tract has been used to create urinary reservoirs or conduits. The first reported urinary diversion following cystectomy into the segment of bowel was by Simon in 1852.(1) He attempted the so called Uretero-sigmoidostomy in an exostrophy patient.
Prior to the 1950’s, the use of anal sphincter for continence established uretero-sigmoidostomy as the urinary diversion of choice. In 1950, Bricker (2) popularized the use of Ileum as a urinary conduit. Until recently bowel conduits were considered the gold standard and represented the most popular form of urinary tract restoration. (3,4) However, the nagative body image associated with an external ostomy appliance, as well as the risk of renal damage, led to the development of continent urinary diversion and bladder replacement reconstruction to improve outcomes for patients who undergo cystectomy. (5, 6) Camey and Le Duc (7) reintroduced the concept of neobladder in 1979, and other investigators improved the technique by applying the experiences of the early continent urinary diversions. (8) No single technique is ideal for all patients and clinical situations.
Factors that affect the choice of urinary diversion include patients age, body habitus, manual dexterity, physical and mental status, renal function, prognosis of primary disease, existing bowel pathology, prior radiation or chemotherapy, the presence of urethral disease, the exceptions, preferences, fears of the patient and the experience and preference of the surgeon. Since there is no unanimous choice for the best method of urinary diversion, all options should be considered.
Methods
A total of 30 patients were operated upon in the Department of Urology, Sher-i-Kashmir institute of medical sciences, Srinagar, from January 2003 to October 2007. All the patients had muscle invasive carcinoma urinary bladder and were treated with standard radical cysto-prostatectomy in males and anterior exenteration in females with reconstruction of the lower urinary tract by Ileal conduit, Mainz pouch II or Ileal neobladder.
All patients had transtional cell carcinoma demonstrated histologically on trans-urethral resection biopsies. A detailed history was taken in all patients regarding the presenting symptoms with special reference to the history of any previous abdominal or pelvic surgery, intestinal resections, diverticulitis, feacal incontinence or irradiation for any pelvic malignancy. Detailed general physical and systemic examination was done in each patient including assessment of manual dexterity, physical and mental status of the patient. In all the patients CBC, Serum chemistry studies, Coagulation profile, Urine examination and culture, Chest X- ray and USG abdomen/pelvis was done. Other investigations included Cystoscopic resection biopsy of the tumour, CECT abdomen/pelvis, Retension enema for checking anal sphincter integrity, Barium enema/Colonoscopy to rule out diverticulitis or colon polyps and Bone scan in selected patients to rule out bone metastasis.
Preoperative Counseling and Preparation
A detailed discussion of the objectives and potential complications of radical cystectomy and the advantages / dis-advantages of each method of urinary diversion was done with the patients before taking for surgery. The patient preference for each specific type of diversion was noted. The patients were also explained that the ultimate decision about the type of diversion to be performed would be done at the time of surgery, as per the intra-operative findings and frozen section analysis of the distal surgical margin. Stoma site was selected and marked pre-operatively and the patient evaluated in lying, sitting and standing positions. A standard mechanical and oral antibiotic bowel cleansing was started 2 days prior to surgery in each patient. Anemic patients were given blood transfusion to bring haemoglobin above 10 gms/dl before surgery. For each patient, at least 3 points of blood were cross matched and reserved for surgery.
Surgical Intervention
All the patients were operated upon under general anaesthesia. A standard midline abdominal incision was made in all patients. Distant metastasis was ruled out at the beginning of the laparotomy. Radical cysto-prostatectomy with bilateral pelvic lymphadenectomy was done in male patients which includes the removal of bladder and prostate with its surrounding fat and peritoneal attachments, prostate and the seminal vesicles enbloc. In the female patient’s anterior pelvic exenteration with pelvic lymphadenectomy was done which includes the removal of uterus, fallopian tubes, ovaries, bladder, urethra and a segment of anterior vaginal wall.
Urinary diversion was performed using Ileal Conduit, Mainz Pouch II or Ileal Neobladder. The patient selection criteria for the 3 types of diversions included Patient preference as discussed with each patient pre-operatively, Pre-operative investigations and Intra-operative findings.
Ileal neobladder was performed in patients who had disease confined to the bladder, without urethral or prostate stromal involvement as determined by the intra-operative frozen section analysis, those without any evidence of extensive pelvic disease, those possessing necessary motor and intellectual skills as how to and when to self catheterize per urethra, and those with normal renal function.
Mainz pouch II was performed in patients with normal anal sphincter integrity, those without any evidence of diverticulitis or colon polyps and with serum creatinine < 1.5 mg/dl.
Ileal conduit was performed in elderly patients without any history of short bowel syndrome or inflammatory small bowel disease and good renal function if not normal.
The patient preferred procedure was performed if the other investigations and findings were suitable for that type of diversion.
Ileal Neobladder was reconstructed as per the technique described by Hautmann and ureteric implantation as described by Camey – Le Duc.
Mainz pouch II was performed as per the technique described by Fisch and Hohenfelloner and ureteric implantation as described by Camey-Le Duc.
Ileal conduit was performed as per the technique described by Bricker.
Post Operative Care
Routine post operative care was followed in all patients with institution of soft diet soon after return of bowel activity.
In the Ileal neobladder group, ureteral stents were removed on 5th or 6th post operative day. Pouchogram was done on 10th day. Patients were discharged with the per urethral Foley’s catheter which was routinely removed after 3 weeks on follow up. After removing the per urethral Foley’s catheter, the patients were demonstrated the proper technique of clean intermittent self catheterization and various perineal exercises which aid in voiding and continence.
In the Mainz pouch II group, rectal tube was routinely removed on 3rd to 5th post operative day and ureteral stents around 8th day. Pouchogram was performed around 15th post operative day and all the patients were discharged on prophylactic oral alkalinization therapy.
In the Ileal conduit group, ureteral stents were removed on 5th or 6th post operative day. Pouchogram was routinely done on 10th day and the patients were discharged after removing the Foley’s catheter from the conduit and demonstrating the proper application of the urostoma bag and the care of skin surrounding the ostoma site.
In all the patients, routine post operative investigations such as CBC, KFT, ABG and Serum Electrolytes were monitored during the post-operative period in the hospital.
Follow up
The patients were followed on Outpatient Department basis weekly for the first month, 3 monthly for the 1st year, 6 monthly for the 2nd year and yearly there after. Investigations on follow up included CBC, KFT, LFT, ABG and Serum Electrolytes, USG abdomen / pelvis to know the status of upper urinary tract, X- ray chest to rule out lung metastasis.
All the complications either related to the surgery or to the specific type of diversion were recorded and divided into early (within 1 month of surgery) and late (after the first month of surgery).
Continence was assessed between 3 to 6 months after surgery in patients with Mainz pouch II and Ileal neobladder diversion.
Patient satisfaction with the type of diversion and Assessment of the quality of life (social, emotional and physical well being) was made at each interaction with the patient on follow up and graded as ‘Very Good’, ‘Good’ or ‘Poor’.
Results
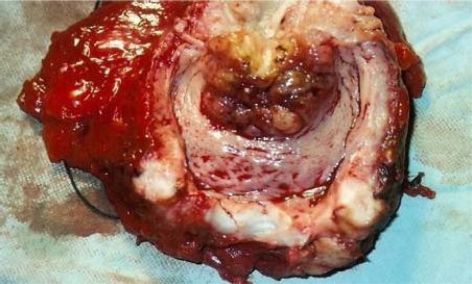
The study included 28 males (93.3%) and 2 females (6.7%) with the overall mean age of 57.7 years (range 35 to 75 years). The mean age was 59.0 years in the Ileal conduit group, 56.5 years in the Mainz pouch II group and 53.3 years in the Ileal neobladder. All the 30 patients (100%) had transitional cell carcinoma (TCC) documented histologically on trans-urethral biopsies. (Fig 1)
Fig. (1).
Specimen of urinary bladder opened to demonstrate the tumour.
After proper pre-operative counseling and discussion of the advantages and disadvantages of all the 3 forms of urinary performed in our department, 18 patients (60%) preferred Ileal neobladder, 3 patients (10%) preferred Ileal conduit and 3 patients (10%) preferred Mainz pouch II as their 1st choice diversion. However, 6 patients (20%) deferred the decision to be taken by the operating surgeon.
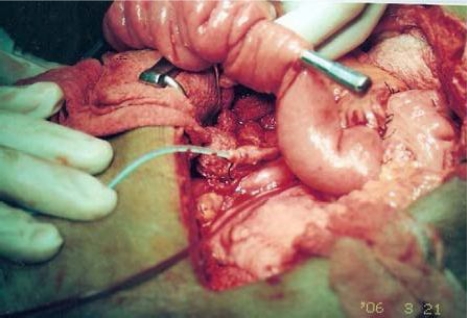
Ileal conduit was performed in 13 patients (43.3%), Mainz pouch II in 13 patients (43.3%) and Ileal neobladder in 4 patients (13.4%). (Fig 2–6)
Fig 2:
Ileal conduit being formed (stented ureter also seen in the picture).
Fig (6).
Patient with Ileal Conduit Urinary Diversion.
Intra operative frozen section analysis of the distal surgical margin at the level desired for an orthotopic neobladder reconstruction (keeping a sufficient urethral stump for anastomosis with the neobladder) was free of tumour in 8 patients (26.8%), out of which 4 patients were taken for Ileal neobladder diversion, as they also fulfilled the other essential criteria necessary for an Orthotopic neobladder diversion. In rest of the patients, to achieve tumour clearance of the distal surgical margin, either the urethral stump was too short for Ileal neobladder reconstruction or simultaneous urethrectomy was needed to achieve complete clearance of the tumour. Such patients were either taken for Ileal conduit or Mainz pouch II diversion as per the patient preference and other criteria necessary for the two diversions respectively.
There were no operative mortalities. The mean post-operative hospital stay for Ileal conduit group was 15 days (range 11 to 20 days), for Mainz pouch II group was 17.8 days (range 13 to 27 days) and for Ileal neobladder group was 19.7 days (range 16 to 25 days).
The mean follow up was 27.7 months (range 3 months to 53 months). Three patients were lost to follow up after attending our Outpatient department for one year.
Four patients died in the follow up period between 24 to 36 months; 2 of metastatic disease and 2 from some unrelated medical problems.
Early complications were seen in 6 patients (46.2%) in the Ileal conduit group, 5 patients (38.5%) in the Mainz pouch II group and 2 patients (50.0%) in the Ileal neobladder group.
In the Ileal conduit group prolonged ileus (ileus, more than 48 hours after surgery) and wound infection were the two main early complications. However, both these complications responded to conservative measures. One patient developed wound dehiscence on the 6th post-operative day and was managed by secondary suturing of the wound. Temporary urine leak from conduit at the uretero-intestinal anastomotic site was seen in one patient who stopped after Foley’s catheter drainage of the conduit and did not need any operative intervention. One patient developed intra abdominal abscess which was managed by open drainage.
In the Mainz pouch II group, wound infection and wound dehiscence were the two main early complications. 2 patients developed wound infection but responded to conservative treatment, 2 patients with wound dehiscence were managed by secondary suturing. One elderly patient developed pneumonia with bilateral pleural effusion and was managed by antibiotics and intercostal drainage. One patient had dislodgement of ureteral stent in the early post-operative period but did not develop any complication secondary to it.
In Ileal neobladder group, prolonged ileus (ileus, more than 48 hours after surgery) was seen in 1 patient who responded to conservative treatment. One patient developed wound infection who responded to antibiotics after wound culture and sensitivity.
Late complications were seen in 8 patients (61.5%) in the Ileal conduit group, 6 patients (46.2%) in the Mainz pouch II group and 2 patients (50%) in the Ileal neobladder group.
In Ileal conduit group, the most common late complication was skin excoriation (para-stomal dermatitis) around the urostoma site seen in 4 patients (30.8%). 1 patient (7.7%) developed para-stomal hernia which needed surgical correction. Biochemical evidence of renal deterioration was observed in 2 patients (15.4%). Frequent episodes of mucous urinary retention in the conduit was seen in 1 patient (7.7%) during the initial few months following surgery which settled with frequent flushing of the conduit with normal saline and soda-bicarbonate through a Foley’s catheter. Stomal stenosis was seen in 1 patient (7.7%) who needed re-fashioning.
In Mainz pouch II group, although all the patients were put on prophylactic oral alkalinization medication on discharge from hospital, 2 patients (15.4%) who had stopped medication of their own developed severe metabolic acidosis and needed re-hospitalization. 1 patient (7.7%) was admitted for acute pyelo-nephritis and was managed by antibiotics. 2 patients (15.4%) developed biochemical evidence of renal dysfunction. Uretero-colonic stricture was seen in 1 patient (7.7%) who needed an open repair.
In Ileal neobladder group, 1 patient (25%)) developed acute pyelo-nephritis and needed hospitalization but responded to conservative treatment. One patient (25%) complained of frequent episodes of urinary retention during the early months after surgery which needed clean intermittent self catheterization.
In Mainz Pouch II group, 12 patients (92.3%) achieved day time continence and 11 patients (83.6%) achieved night time continence 3 to 6 months after surgery. One patient remained incontinent day and night and refused any conversion procedure.
In Ileal neobladder group, 3 patients (75%) achieved day time continence and 2 patients (50%) achieved night time continence 3 to 6 months after surgery. One patient (25%) suffered occasional incontinence during day and night time and needed pad protection.
In Ileal conduit group, the patient satisfaction with the diversion and the overall quality of life was described as ‘Very Good’ by 2 patients (15.4%), ‘Good’ by 8 patients (61.5%) and ‘Poor’ by 3 patients (23.1%).
In Mainz Pouch II group, the patient satisfaction with the diversion and the overall quality of life was described as ‘Very Good’ by 8 patients(61.5%), ‘Good’ by 3 patients (23.1%) and ‘Poor’ by 2 patients (15.4%).
In Ileal neobladder group, the patient satisfaction with the diversion and the overall quality of life was described as ‘Very Good’ by 3 patients (75%), and ‘Good’ by 1 patient (25%).
Discussion
Determining the optimal mode of urinary tract reconstruction following cystectomy is a challenge for the urologic surgeon. No single technique is ideal for all patients and clinical situations. While deciding which of the diversions to recommend to a patient, one must consider the functional outcome, the potential short term and long term complications and the physical and psychosocial re-adjustments required following surgery. Our study was aimed to achieve a comparison between the three types of urinary diversion performed in the Department of Urology, Sher-i-Kashmir institute of Medical Sciences, Srinagar.
Mean age of the patients in our study was 57.7 years which was consistent with the studies by Cengiz et al 58.2 years (9), Momose et al 60.9 years (10) and Hadzi et al 56.7 years. (11) The mean age of the patients in all the three groups was comparable.
Our study included 28 males (93.3%) and 2 females which was comparable with studies conducted by Cengiz et al 94.8% males and 5.2% females (9) and Gburekh et al 93.8% males and 6.2% females in Ileal neobladder group and 100% males in Ileal conduit group (12) All the patients in the Ileal neobladder group and Mainz pouch II group were males. Eleven patients in the Ileal conduit group were males and 2 were females.
All the patients in our study (100%) had histologically proved transitional cell carcinoma (TCC) on trans-urethral biopsies which was consistent with studies conducted by Cengiz et al 100% TCC (9) and Yiu T F et al 100% TCC. (13)
Seventy percent of the patients in our study preferred a continent urinary diversion (60% preferred Ileal neobladder, 10% preferred Mainz pouch II) and 10% preferred Ileal conduit as their 1st choice diversion. 20% of the patients deferred the decision to the operating surgeon. Cengiz et al (9), in their study observed that 96.6% patients preferred a continent urinary diversion as their first choice and half of them wanted to be completely dry. Only 3.4% of patients preferred an Ileal loop procedure while 32.7% deferred the decision to the operating surgeon. Although a very high percentage of patients in our study preferred Ileal neobladder as their first diversion, it was possible to construct Ileal neobladder in a small percentage (13.4%) of patients, who besides patient preference fulfilled the other criteria necessary for an Orthotopic neobladder reconstruction, most important being the distal surgical margin negativity for the tumour (at the level desired for Ileal neobladder reconstruction) as revealed by intra-operative frozen section analysis. Cengiz et al (9) in their study performed an Orthotopic neobladder reconstruction in patients with tumour confined to the bladder without urethral or prostatic stromal involvement. Richard E Hautmann et al(14) in their study excluded patients with prostatic urethral involvement by tumour for Ileal neobladder diversion. Singh P B et al (15) in their study ruled out prostatic urethral involvement by random punch biopsies from prostatic urethra before taking patients for Ileal neobladder diversion and in patients with insufficient urethral stump, Ileal conduit was performed. The mean hospital stay was comparable between the 3 groups.
The mean hospital stay was 15 days in Ileal conduit group, 17.8 days in Mainz pouch II group and 19.7 days in Ileal neobladder group. Gburekh et al (12) in their study report a mean hospital study of 13 days in both Ileal conduit and Ileal neobladder group.
Early complications were seen in 46.2% patients in the Ileal conduit group of our study and comparable to other studies. Early complication rates for Ileal conduit as reported in other studies range from 31.8% by Frank P .P.M et al (16), 39% by Onishi et al (17), 33.3 % by Momose et al (10), and 38% by Ariyoshi et al (18)
Early complication for Mainz pouch II group of our study was 38.5% which was higher as compared to other studies. Early complication rates for Mainz pouch II as reported in other studies range from 13.6% by Triantafyllidis et al (19) 10.9% by Hadzi et al (11) and 28.6% by Omaya Nassar et al (20)
Early complication rate for Ileal neobladder group of our study was 50% which was comparable to other studies. Early complication rate for Ileal neobladder as reported in other studies range from 18% by Gburekh et al (12), 20% by Mahmoud Bassiouny et al (21), 33.3% by Yiu TF et al (13), and 48% by Jensen JB et al. (22)
Late complications were observed in 61.5% patients in Ileal conduit group of our study which was comparable to other studies. Late complication rate for Ileal conduit group as reported in other studies range from 31.6% by Momose et al (10) with parastomal dermatitis being most common (37.3%), 41% by Johnson et al (23), 36% by Micheal J et al (24), 51% by Ariyoshi et al (18), 62% by Onishi et al (17) with stoma related complications in 35% and renal dysfunction in 7.2%. Late complications were observed in 46.2% patients in Mainz pouch II group of our study which was again higher than mentioned in other studies. Late complication rate for Mainz pouch II group as reported in other studies range from 14.2% by Omaya Nassar et al (20) to 19.1% by Fisch et al. (25) Late complications were observed in 50.0% patients in Ileal neobladder group of our study which was comparable to the rates mentioned in other studies. Late complication rate in the Ileal neobladder group as reported by other series range from 21% by Gburekh et al (12), 30% by Miyoshi et al (26) and 48% by Jensen J B et al. (22)
In Mainz pouch II group of our study 93.3% patients achieved day time continence and 83.6% patients achieved night time continence 3 to 6 months after surgery which was comparable to other studies. The continence rates in the Mainz pouch II group as reported by other series are D’elia G et al (27) day and night continence rates of 97% and 95% respectively, Fisch et al (25) day time continence in 94.5% and night time continence in 98.6%, Fournier et al (28) nocturnal 82% and diurnal 85.5%. In Ileal neobladder group of our study 75.0% achieved day time and 50.0% achieved night time continence 3 to 6 months after surgery which was comparable to other studies. The continence rates in the Ileal neobladder group as reported by other series are 89.4% day time and 53.3% night time continence by Mahmoud Bassiouny (21), 92.0% day time and 80.0% night time continence by Hautmann et al (29), 90% day time and 65% night time continence rates by Jensen JB et al. (22)
Conclusion
Although a high percentage of patients in our study preferred Ileal neobladder as their first choice diversion, it was possible only in a small percentage of patients who fulfilled all the criteria’s necessary for an Orthotopic neobladder reconstruction. The mean post operative hospital stay was comparable between the 3 groups. The early and late complications were comparable between the 3 groups. The continence rates were also comparable between Mainz pouch II group and Ileal neobladder group.
However the patient satisfaction and the quality of life was described better by patients with a continent diversion (Ileal neobladder and Mainz pouch II) as compared to those with Ileal conduit diversion.
So we conclude that there are inherited advantages and dis advantages to each form of urinary diversion and the patient selection is important to identify the most appropriate method of diversion for an individual. The Ileal conduit diversion is an appropriate method of diversion because of its simplicity and good satisfaction in the quality of life. However more attention should be paid to the condition of peristomal skin.
The Mainz pouch II diversion is a simple and reliable alternative for continent diversion resulting in a very good quality of life for patients without altering their appearance. Although it carries the risk of life time oral alkalinization therapy, it is a good alternative for patients who prefer to be dry.
The Ileal neobladder is a good choice for male patients provided there is no evidence of prostatic or urethral tumour invasion. Patient satisfaction at voiding through natural passage is incomparable to other forms of urinary diversion.
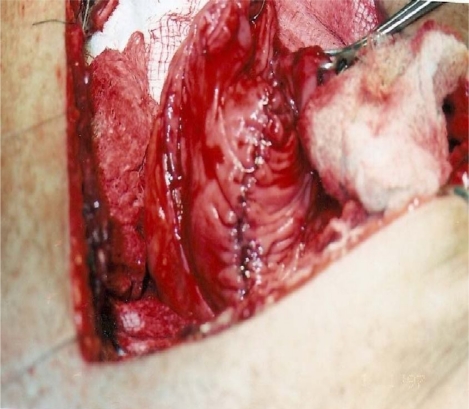
Fig. (3).
Mainz pouch II being reconstructed.
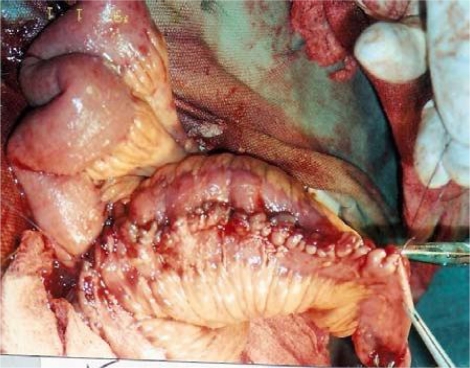
Fig (4).
Ileal neobladder being reconstructed.
Fig (5).
Patient of ileal conduit diversion with urine collecting bag fitted with an abdominal belt.
References
- 1.Simon J. Operation for directing the ureteral orifices into the rectum, temporary success, subsequent death, autopsy. Lancet. 1852;2:568–570. [Google Scholar]
- 2.Bricker EM. Bladder substitution after pelvic evisceration. Surg Clin North Am. 1950;30:1511–1521. doi: 10.1016/s0039-6109(16)33147-4. [DOI] [PubMed] [Google Scholar]
- 3.Taylor RA, Grune MT.Urinary diversions and reconstructions: Vogelzang JN, Scardino PT, Shipley UW Comprehensive text book of genitourinary Oncology Baltimore;Md: Williams and Wilkins; 1996. chapter 29:472–479. [Google Scholar]
- 4.Zinman L, Libertino JA. Ileocaecal conduit for temporary and permanent urinary diversion. J Urol. 1975;113:317–323. doi: 10.1016/s0022-5347(17)59471-9. [DOI] [PubMed] [Google Scholar]
- 5.Kock NG, Nilson AE, Norlen LS. Urinary diversion via a continent ileal reservoir: clinical results in 12 patients. J Urol. 1982;128:469–475. doi: 10.1016/s0022-5347(17)53001-3. [DOI] [PubMed] [Google Scholar]
- 6.Thuroff JW, Alken P, Ried Miller H. The Mainz pouch for bladder augmentation and continent diversion. J Urol. 1986;136:17–26. doi: 10.1016/s0022-5347(17)44714-8. [DOI] [PubMed] [Google Scholar]
- 7.Camey M, Le Duc A. Entero-cystoplastic area cystoprostatectomie totale pour cancer de la vessie. Am Urol. 1979;13:114–123. [Google Scholar]
- 8.Hautmann RE, Egghart G, Frohneberg D, et al. The Ileal neobladder. J Urol. 1988;139:39–42. doi: 10.1016/s0022-5347(17)42283-x. [DOI] [PubMed] [Google Scholar]
- 9.Girgin Cengiz, Sezer Akif, Ozer Kutan, Tarhan Huseyin, Bolukbasi Ahmat, Gurel Gozen. Comparison of three types of continent urinary diversion in a single centre. Ataturk Training Hospital Urology Department, Izmir, Turkey. Scientific World Journal. 2004 Jun 7;4(suppl 1):135–41. doi: 10.1100/tsw.2004.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Momose H, Hirao Y, Tanaka N, Ozono S, Yamada K. Complications and quality of life in patients with ileal conduit diversion. Hinyokika Kiyo. 1995 Nov.41(11):927–35. [PubMed] [Google Scholar]
- 11.Hadzi D, Jokic JB, Jokic JB, Basic DT. Mainz pouch II: Analysis Of outcome and complications in 220 patients. BJU Int. 2006 Mar.97(3):587–91. doi: 10.1111/j.1464-410X.2006.05995.x. [DOI] [PubMed] [Google Scholar]
- 12.Gburekh BM, Lieber MM, Blute ML. Comparison of ileal neobladder and ileal conduit urinary diversion with respect to peri-operative outcome and late complications. J Urol. 1998;160(1):721–723. doi: 10.1016/S0022-5347(01)62767-8. [DOI] [PubMed] [Google Scholar]
- 13.Yiu TF, Chan AYT. Early experience in ileal neobladder reconstruction. J Hong Kong Med Assoc. 1994 Dec.46(4) [Google Scholar]
- 14.Hautmann Richard E, Miller Kurt, Steiner Ursula, Wenderoth Ulrich. The ileal neobladder: 6 years experience with more than 200 patients. The Journal of Urology. 1993 Jul;150:40–45. doi: 10.1016/s0022-5347(17)35392-2. [DOI] [PubMed] [Google Scholar]
- 15.Singh PB, Saraf SK. Ileal neobladder: 5 years follow up. Indian Journal of Urology. 1997;13(2) [Google Scholar]
- 16.Frank PPM, pernet, Jonas Udo. Ileal conduit urinary diversion. Early and late complications in 132 cases. World Journal of Urology. 1985 Dec.3(140–144) [Google Scholar]
- 17.Onishi T, Kinbara H, Anima K, Sugimura Y. Urinary diversion: the key of reducing surgical complications-ileal conduit. Hinyokika Kiyo. 2006 Jun;52(6):421–5. [PubMed] [Google Scholar]
- 18.Ariyoshi A, Saqiyama K, Hasno K, Oshima K, Yamaquchi A, Komatsu K. A seven-year experience with ileal conduit urinary diversion: early and late complications. Nippon Hinyokika Zasshi. 1990;81(10):1555–62. doi: 10.5980/jpnjurol1989.81.1555. [DOI] [PubMed] [Google Scholar]
- 19.Triantafyllidis A, Rambis V, Papatsoris A, Touloupidis S. Sigma rectal (Mainz II) pouch for continent urinary diversion in bladder cancer. International J Urol. 2005 Jun;12(6):599–602. doi: 10.1111/j.1442-2042.2005.01100.x. [DOI] [PubMed] [Google Scholar]
- 20.Nassar Omaya. Mainz pouch II: A simple continent urinary diversion after cystectomy. Journal of the Egyptian Nat Cancer Inst. 2002 Dec.14(4):267–274. [Google Scholar]
- 21.Bassiouny Mahmoud, Helmy Ahmad, Amin Ayman, Aboul Kassem Hatem. The ileal neobladder following radical cystectomy.: Experience and results of 50 cases. Journal of the Egyptian Nat Cancer Inst. 2003 Jun;15(2):155–162. [Google Scholar]
- 22.Jensen JB, Landbeck F, Jensen KM. Complications and neobladder function of the Hautmann orthotopic ileal neobladder. BJU Int. 2006 Dec;98(6):1289–94. doi: 10.1111/j.1464-410X.2006.06449.x. [DOI] [PubMed] [Google Scholar]
- 23.Johnson DE, Camey SM. Complications of ileal conduit urinary diversion: A review of 214 cases. J Urol. 1997 Feb.117(2):171–3. [Google Scholar]
- 24.Micheal J, Metro MD. Long term effects of ileal conduit diversion on upper urinary tract. Uro Today. 2006 Aug.68(2):324–327. doi: 10.1016/j.urology.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 25.Fisch M, Wammade R, Hohfellner R. The sigma-rectum pouch (Mainz pouch II) World J Urol. 1996;14:68–72. doi: 10.1007/BF00182560. [DOI] [PubMed] [Google Scholar]
- 26.Miyoshi S, Iwasaki A, Inove H, Oka D, Takao T, Mizutani S. Clinical experience of ileal neobladder for bladder cancer. Hinyokika Kiyo. 1998 Jan.44(1):7–11. [PubMed] [Google Scholar]
- 27.D’elia G, Pahernik S, Fisch M, Hohenfellner R, Thuroff JW. Mainz pouch II technique: 10 years experience. J Urol. 2005 Mar;173(3):885. doi: 10.1111/j.1464-410X.2003.04777.x. [DOI] [PubMed] [Google Scholar]
- 28.Fournier F, Bon D, Dore B, Aubert J. Ureterosigmoidostomy after total cystectomy in cancer: Long term results in 60 patients. Prog Urol. 1997 Dec.7(6):967–75. [PubMed] [Google Scholar]
- 29.Hautmann RE, Volkmer BG, Schwend MC, G Schend JE. Long term results of the ileal neobladder. World J Urol. 2006 Aug.24(3):305–14. doi: 10.1007/s00345-006-0105-z. [DOI] [PubMed] [Google Scholar]
- 30.prevalence estimates of human papillom-avirus infection. Int J Cancer. 1989;43(2):260–2. doi: 10.1002/ijc.2910430216. [DOI] [PubMed] [Google Scholar]