Abstract
Background:
No studies have assessed psychopathology among benign paroxysmal positional vertigo (BPPV) patients. The General Health Questionnaire allows for distinguishing patients suffering from psychiatric problems from those in good mental health.
Objective:
To assess the psychiatric illness in Saudi patients with BPPV.
Methods:
The study was cross-sectional in nature. Institutional ethics committee approval and individual informed consent from study participants were obtained. Fifty patients with BPPV with unknown psychiatric illness were given the General Health Questionnaire-28 (GHQ-28) questionnaire to complete.
Results:
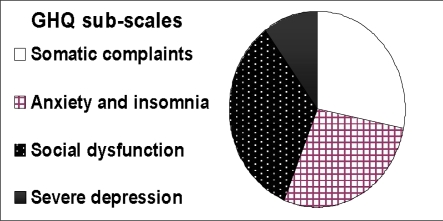
Complete data were available for 50 patients. Thirty patients (60%) with BPPV scored above the conventional threshold. Their subgroups were: somatic complaints 28%, anxiety and insomnia 28%, social dysfunction 34%, and severe depression 10%.
Conclusions:
Greater attention needs to be paid to BPPV patients. Vulnerable female patients may have high levels of psychiatric symptomatology that may benefit from assessment and intervention.
Introduction
Dizziness ranks among the most common complaints in medicine, affecting approximately 20% to 30% of the general population. (1,2) However, the term dizziness encompasses a variety of different sensations that point in distinct diagnostic directions. Vestibular dizziness is rotational vertigo or other illusory sensations of motion, whereas other sensations like unsteadiness, faintness, light-headedness or drowsiness imply a non-vestibular origin. Patients often use these terms interchangeably, and few physicians other than otoneurologists clearly differentiate between the two.(3) In vestibular dizziness, the most frequent cause of vestibular vertigo is benign paroxysmal positional vertigo (BPPV), which typically lasts less than 30 seconds. (4,5)
BPPV is characterised by brief attacks of rotatory vertigo and concomitant positioning rotatory ± linear nystagmus, which is elicited by rapid changes in head position relative to gravity. It is a mechanical disorder of the inner ear in which the precipitating positioning of the head causes abnormal stimulation, usually of the posterior SCC of the undermost ear, and less frequently of the horizontal SCC. Typical posterior canal BPPV is caused by canalolithiasis, a free-floating clot within the endolymph of the posterior SCC
In 20%–50% of all dizziness states, psychiatric disorders appear to exert an important influence on the course of the illness. (6–11) Untreated psychiatric disorders in the presence of comorbid conditions may result in chronification and greater handicap, more frequent clinic visits, increased costs, extended hospitalisation, and reduced compliance and quality of life. (12,13) Particularly in these cases, a comorbid or reactive psychiatric disorder is often overlooked and consequently left untreated. (14) Moreover, failure to evaluate comorbid psychiatric disorder may lead to serious consequences, such as suffering, hopelessness, suicidal thoughts, and decreased treatment compliance. (15,16)
Otolaryngologists should be aware of the psychiatric disorder of BPPV patients to allow them to detect and treat problems earlier, or to refer them to a psychiatrist for more appropriate follow-up.
To the best of our knowledge, comorbid psychiatric conditions of BPPV (the most frequent organic causes of peripheral vestibular dizziness (14) have not been evaluated before. In the present study, we planned to explore the levels of psychological symptomatology in BPPV. The secondary aim was to explore factors that associated with high levels of psychological symptomatology. We used the 28-item form of the General Health Questionnaire (GHQ) in our study population as a general indication of a possible psychiatric case. The results will afford greater understanding of the psychological sequelae of BPPV and the mental health needs of these patients.
Methods
Patients were recruited from the Specialised Neurotology Clinic at King Abdulaziz University Hospital (KAUH) and Al-Habeeb Medical Centre (HMC). These are tertiary care clinics managing different causes of dizziness which are run by a trained neurotologist experienced in dealing with all ear causes of dizziness. Ethical approval was granted by the research ethics committee of King Saud Medical College. The two centres (KAUH and HMC) agreed to participate in this study using the same protocol. The study was funded by the College of Medicine Research Center (CMRC) at King Saud University in Riyadh, Saudi Arabia (Grant number 06-553).
The inclusion criteria of patients were as follows:
Age above 18 years
Active BPPV
History supporting the diagnosis of BPPV
Positive Dix–Hallpike manoeuvre
Exclusion criteria were
Contra-indications for Dix–Hallpike or Epley manoeuvre
Concomitant causes of dizziness (vestibular and non-vestibular)
Previous history of ear disease
Previous history of psychiatric illness
The study was cross-sectional in nature. All patients who had BPPV, which improved after performing the Epley manoeuvre by a treating neurotologist, were approached for participation in this study. After an initial BPPV counselling, inclusion and exclusion criteria were checked. If the patient was suitable for participation in this study, they signed the consent and then the General Health Questionnaires GHQ-28 with demographic data was given to the patient to complete independently without input from the staff. Questions were rated on a four point scale (e.g. from ‘better than usual’ to ‘much worse than usual’). The 28-item version (17) of the GHQ provided scaled scores in four domains: somatic complaints, anxiety and insomnia, social dysfunction and severe depression. These sub-scales do not reflect psychiatric diagnoses and are not independent. The categorical scoring method involves the application of weights to the four response alternatives (0–0–1–2). A cut-off of 5 was used as threshold for morbidity level. For each of the four seven-item sub-scales, the method of scoring was applied (0–1–2–3)(18)
The demographic variables of age, sex, and education status were collected. Unfortunately, there is very limited clinical data on this subject to allow us to make a clear sample size calculation. However, it was planned to recruit a total of 50 patients over a period of one year. All data were entered into an Excel database program and SPSS statistical software for statistical analyses.
Results
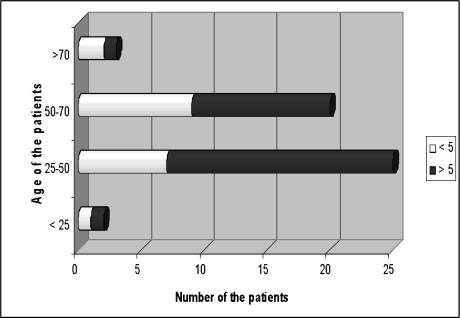
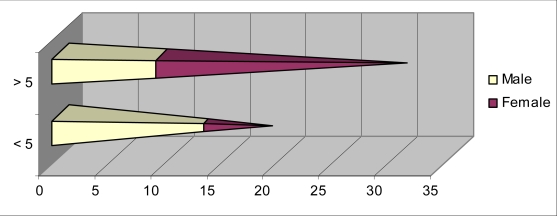
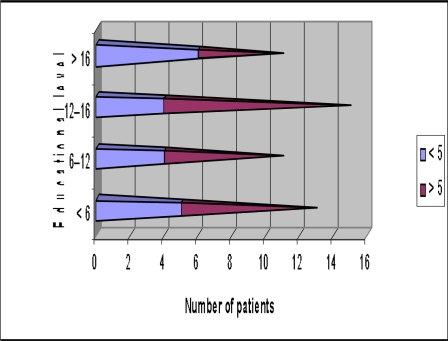
Informed consent was obtained from all 50 patients. Seven patients were seen at KAUH and the rest were seen at HMC. All respondents completed the 28-item General Health Questionnaire (GHQ–28; Goldberg & Hillier, 1979), which provides an indication of current psychological health. Thirty patients (60%) with BPPV scored above the conventional threshold score of 5. Our patients had a mean age of 46.7 years (range 18–91 years) (Figure 1) a male: female ratio of 1: 1.3 (Figure 2), and varying educational levels (Figure 3). Their subgroups included somatic complaints 28%, anxiety and insomnia 28%, social dysfunction 34% and severe depression 10% (Figure 4).
Fig. (1).
Age distribution of the patients with and without psychological illness.
Fig. (2).
Gender represensation with and without psychological illness.
Fig. (3).
Educational level of our patients with and without psychological illness.
Fig. (4).
The GHQ sub-scales of our patients.
Discussion
The early identification of patients at risk assumes considerable importance for the prevention of mental health problems. Several screening tools have been developed, but the General Health Questionnaire is certainly one of the most frequently used tools and has been the subject of the most research.(19) The GHQ(18) was designed to be a self-administered screening test that is aimed at detecting the psychological components of poor health. It measures an individual’s inability to carry out ‘normal healthy’ functions and the appearance of distress-related symptoms. It detects disorders of less than two weeks duration, and is reported to be sensitive to transient disorders. The GHQ-28 is the favoured version of the GHQ for research purposes since it allows for an assessment of four dimensions relevant to psychological health: somatic symptoms, e.g., Have you recently been feeling run down and out of sorts?
Anxiety and insomnia, e.g., have you recently found everything getting on top of you? Social dysfunction, e.g., Have you recently felt on the whole you are doing things well?
Severe depression, e.g., have you recently found yourself wishing you were dead and away from it all?(20)
However, a positive result in the questionnaire does not exactly mean that the subject has a psychiatric disease. The respondent is not asked how long they have experienced symptoms. Therefore, disorders of less than two weeks duration are counted, unlike systems such as DSM-IV-TR which require symptoms to have been present for at least two weeks.
The published literature on the management of BPPV has focused mainly on the management of vertigo, with success or failure of care dependent on stopping the attacks. However, a more holistic approach in care is required which includes a psychological cure since BPPV usually occurs suddenly in healthy middle-aged people who are afraid of brain cancer or cerebro-vascular incidents. This is the first study to specifically explore the levels of psychological symptomatology of BPPV.
In up to 50% of all dizziness states, psychiatric disorders appear to exert an important influence on the course of the illness (6–11). Our results show a high strength of association between BPPV and psychiatric disorder (60%). This is greater than gastroesophageal reflux (38.3%), (21) stalking victims (36.4%) (22) and 30% breast cancer patients (23), all of whom used GHQ. However, there is a possibility that bias may have affected the results. Bias may result from studying clinic samples where patients who have more anxiety will visit ORL doctors. However, a control group may not solve this problem and community study is very difficult for this rare disease. A second possibility is that there was confounding, particularly arising from an association between severity and recurrence of physical illness and inability of emergency or family doctors to treat or explain this disease to the patients lead to delayed management.
We have found an association of vestibular vertigo with the female sex, which has been previously reported for BPPV.(24) Case series have suggested that premenstrual or oral contraceptive–related hormonal changes may increase the risk of vestibular disorders, (25,26) but this was not consistently confirmed in a large cohort study. (27) Moreover in our study, women have higher psychological distress than men which was shown in other studies (28,29). This may be associated with the prevalence of such disease that is higher in women. Another explanation for this difference between genders might be that women suffer a greater psychological impact from vertigo than men. (30)
According to Medline (until 2007), 1,196 studies have been published using GHQ studies to evaluate different populations’ responses to all kinds of stress exposures ranging from daily hassles via upsetting life events to distress related to physical illness and disasters. This questionnaire takes a few minutes from the patient and it helps in identifying the patient who may need extra care. Moreover, patients may benefit from being offered additional emotional and social support during their education about BPPV since few of the symptomatic BPPV will accept contact with psychiatric or counselling services. The consequences of unrecognised and untreated psychiatric symptomatology are potentially serious, including increased risk-taking behaviour and suicide (31,32)
To the best of our knowledge, there is no study that has addressed the psychological condition of the BPPV patient. Our response rate was high (100%). The study was exploratory and has identified issues for further research. This study has a number of limitations. Participants were recruited from two institutions, which may limit generalisability. The present sample experienced a generally high level of psychiatric disorder, and the study lacked a non-vertiginous control group. A further criticism concerns the exclusion criteria of past psychiatric history. This exclusion may have reduced the extent to which one may generalise from the results and may have underestimated the degree of distress experienced by a BPPV patient. Future research employing a longitudinal design is needed to explore BPPV in more detail.
Conclusion
We conclude that greater attention needs to be paid to BPPV patients. In general, these vulnerable female patients may have high levels of psychiatric symptomatology that may benefit from assessment and intervention. The aim of the healthcare professionals must be to reassure BPPV and minimise the disability that impacts their life. Further work is needed to identify the most effective screening and interventions.
Acknowledgments
The research was funded by CMRC at King Saud University in Riyadh, Saudi Arabia (Grant No06-553) and Hearing disabilities research chair (RCHD). The author would like to thank the participating medical centres (KAUH and HMC), and particularly the patients who participated in the study.
References
- 1.Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Intern Med. 1993;153(21):2474–2480. [PubMed] [Google Scholar]
- 2.Yardley L, Owen N, Nazareth I, Luxon L. Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Pract. 1998;48(429):1131–1135. [PMC free article] [PubMed] [Google Scholar]
- 3.Neuhauser HK, von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, et al. Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology. 2005;65(6):898–904. doi: 10.1212/01.wnl.0000175987.59991.3d. [DOI] [PubMed] [Google Scholar]
- 4.Massoud EA, Ireland DJ. Post-treatment instructions in the nonsurgical management of benign paroxysmal positional vertigo. J Otolaryngol. 1996;25(2):121–125. [PubMed] [Google Scholar]
- 5.Fetter M, Sievering F. Three-dimensional eye movement analysis in benign paroxysmal positioning vertigo and nystagmus. Acta Otolaryngol. 1995;115(3):353–357. doi: 10.3109/00016489509139328. [DOI] [PubMed] [Google Scholar]
- 6.Alvord LS. Psychological status of patients undergoing electronystagmography. J Am Acad Audiol. 1991;2(4):261–265. [PubMed] [Google Scholar]
- 7.Eagger S, Luxon LM, Davies RA, Coelho A, Ron MA. Psychiatric morbidity in patients with peripheral vestibular disorder: a clinical and neuro-otological study. J Neurol Neurosurg Psychiatry. 1992;55(5):383–387. doi: 10.1136/jnnp.55.5.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kroenke K, Lucas CA, Rosenberg ML, Scherokman B, Herbers JE, Jr, Wehrle PA, et al. Causes of persistent dizziness. A prospective study of 100 patients in ambulatory care. Ann Intern Med. 1992;117(11):898–904. doi: 10.7326/0003-4819-117-11-898. [DOI] [PubMed] [Google Scholar]
- 9.McKenna L, Hallam RS, Hinchcliffe R. The prevalence of psychological disturbance in neurotology outpatients. Clin Otolaryngol Allied Sci. 1991;16(5):452–456. doi: 10.1111/j.1365-2273.1991.tb01038.x. [DOI] [PubMed] [Google Scholar]
- 10.Yardley L, Redfern MS. Psychological factors influencing recovery from balance disorders. J Anxiety Disord. 2001;15(1–2):107–119. doi: 10.1016/s0887-6185(00)00045-1. [DOI] [PubMed] [Google Scholar]
- 11.Yardley L, Medina SM, Jurado CS, Morales TP, Martinez RA, Villegas HE. Relationship between physical and psychosocial dysfunction in Mexican patients with vertigo: a cross-cultural validation of the vertigo symptom scale. J Psychosom Res. 1999;46(1):63–74. doi: 10.1016/s0022-3999(98)00056-7. [DOI] [PubMed] [Google Scholar]
- 12.Atesci FC, Oguzhanoglu NK, Baltalarl B.Psychiatric disorders in cancer patients and associated factor Turk J Psychiatry 14145–152.2003. Ref Type: Generic [PubMed] [Google Scholar]
- 13.Valente SM, Saunders JM. Diagnosis and treatment of major depression among people with cancer. Cancer Nurs. 1997;20(3):168–177. doi: 10.1097/00002820-199706000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Eckhardt-Henn A, Breuer P, Thomalske C, Hoffmann SO, Hopf HC. Anxiety disorders and other psychiatric subgroups in patients complaining of dizziness. J Anxiety Disord. 2003;17(4):369–388. doi: 10.1016/s0887-6185(02)00226-8. [DOI] [PubMed] [Google Scholar]
- 15.Bottomley A. Depression in cancer patients: a literature review. Eur J Cancer Care (Engl) 1998;7(3):181–191. doi: 10.1046/j.1365-2354.1998.00100.x. [DOI] [PubMed] [Google Scholar]
- 16.Roth AJ, Holland JC.Treatment of depression in cancer patients Primary Care Cancer 1423–29.1994. Ref Type: Generic [Google Scholar]
- 17.Goldberg D.Manual of the General Health Questionnaire 1978.Slough: NFER-Nelson; Ref Type: Generic [Google Scholar]
- 18.Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med. 1979;9(1):139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27(1):191–197. doi: 10.1017/s0033291796004242. [DOI] [PubMed] [Google Scholar]
- 20.Ireland JL, Boustead R, Ireland CA. Coping style and psychological health among adolescent prisoners: a study of young and juvenile offenders. J Adolesc. 2005;28(3):411–423. doi: 10.1016/j.adolescence.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Diaz dL, Yarnoz C, Artieda C, Flores L, Garde C, Romeo I, et al. Gastroesophageal reflux: prevalence of psychopathological disorders and quality of life implications. Dis Esophagus. 2006;19(5):373–376. doi: 10.1111/j.1442-2050.2006.00597.x. [DOI] [PubMed] [Google Scholar]
- 22.Purcell R, Pathe M, Mullen PE. Association between stalking victimisation and psychiatric morbidity in a random community sample. Br J Psychiatry. 2005;187:416–420. doi: 10.1192/bjp.187.5.416. [DOI] [PubMed] [Google Scholar]
- 23.Millar K, Purushotham AD, McLatchie E, George WD, Murray GD. A 1-year prospective study of individual variation in distress, and illness perceptions, after treatment for breast cancer. J Psychosom Res. 2005;58(4):335–342. doi: 10.1016/j.jpsychores.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 24.Katsarkas A. Benign paroxysmal positional vertigo (BPPV): idiopathic versus post-traumatic. Acta Otolaryngol. 1999;119(7):745–749. doi: 10.1080/00016489950180360. [DOI] [PubMed] [Google Scholar]
- 25.Rybak LP. Metabolic disorders of the vestibular system. Otolaryngol Head Neck Surg. 1995;112(1):128–132. doi: 10.1016/S0194-59989570312-8. [DOI] [PubMed] [Google Scholar]
- 26.Andrews JC, Ator GA, Honrubia V. The exacerbation of symptoms in Meniere's disease during the premenstrual period. Arch Otolaryngol Head Neck Surg. 1992;118(1):74–78. doi: 10.1001/archotol.1992.01880010078020. [DOI] [PubMed] [Google Scholar]
- 27.Vessey M, Painter R. Oral contraception and ear disease: findings in a large cohort study. Contraception. 2001;63(2):61–63. doi: 10.1016/s0010-7824(01)00176-7. [DOI] [PubMed] [Google Scholar]
- 28.Yardley L. Contribution of symptoms and beliefs to handicap in people with vertigo: a longitudinal study. Br J Clin Psychol. 1994;33(Pt 1):101–113. doi: 10.1111/j.2044-8260.1994.tb01100.x. [DOI] [PubMed] [Google Scholar]
- 29.Siirala U, Gelhar K. Further studies on the relationship between Meniere, psychosomatic constitution and stress. Acta Otolaryngol. 1970;70(2):142–147. doi: 10.3109/00016487009181869. [DOI] [PubMed] [Google Scholar]
- 30.Monzani D, Casolari L, Guidetti G, Rigatelli M. Psychological distress and disability in patients with vertigo. J Psychosom Res. 2001;50(6):319–323. doi: 10.1016/s0022-3999(01)00208-2. [DOI] [PubMed] [Google Scholar]
- 31.Hollis C. Depression, family environment, and adolescent suicidal behavior. J Am Acad Child Adolesc Psychiatry. 1996;35(5):622–630. doi: 10.1097/00004583-199605000-00017. [DOI] [PubMed] [Google Scholar]
- 32.Neiger BL, Hopkins RW. Adolescent suicide: character traits of high-risk teenagers. Adolescence. 1988;23(90):469–475. [PubMed] [Google Scholar]