Abstract
Objectives:
Diabetes, hypertension and coronary artery disease are emerging threats to the health status in Saudi Arabia. These diseases are attributed largely to unhealthy dietary habits and lack of physical activity. Health education through primary health care (PHC) centers can play a significant role in changing behaviors and reducing the burden of non-communicable diseases.
Methods:
We present the results of analysis of a moderately large dataset on dietary practices, physical activity and exposure to health education among patients visiting the PHC centers in Qassim region of Saudi Arabia. We examined this cross-sectional data to identify the relationships between these three variables after controlling for the effects of age, sex, marital status, education and disease status.
Results:
Our results suggest that women, older people, divorced and widowed persons and those with low education are more likely to have poor dietary habits and lack of physical activity. Patients suffering from chronic illnesses are more likely to be exposed to health education from PHC centers, which help to significantly improve their dietary practices and, to some extent, increase physical activity at all ages. Our analysis indicates that health education provided through the PHC centers plays a modest but significant role in improving lifestyles and dietary practices.
Conclusion:
We conclude that better emphasis on high quality health education would significantly reduce the burden of non-communicable diseases in our target population.
Introduction
Non-communicable diseases have emerged as a serious threat in developing countries. In Saudi Arabia, diabetes mellitus, hypertension and ischemic heart disease are among the top ten causes of death. These lifestyle-related diseases are sometimes referred to as ‘the diseases of affluence’ and the increase in their prevalence is attributed to decreased physical activity and changes in dietary patterns (such as a growing culture of fast foods).(1,2) Spread of non-communicable diseases is the greatest challenge for the health system in Saudi Arabia.(3) For example, prevalence of type 2 diabetes mellitus is 24% among 30–70 years age-group, and the prevalence of obesity, coronary artery disease and hypertension is increasing.(5) These diseases are likely to become the principal global cause of morbidity and mortality in Saudi Arabia during the next decade.(6) Promoting healthy lifestyles through health education is the only solution to this problem, as recognized by many researchers.(4)
Health is high on the political agenda of Saudi Arabia, and controlling non-communicable diseases through health education is national policy. The role of Primary Health Care (PHC) Centers in health promotion by providing health education is duly recognized. The concept of PHC deems that the people are the custodians of their own health and they themselves are the resources, users and decision makers regarding the use of health information; they decide about the activities to be undertaken to ensure attainment of health.(7) The aim of PHC in Saudi Arabia is to facilitate people to lead healthy, safe and independent lives. However, no studies have so far attempted to measure the impact of health education through PHC Centers.
In this paper, we examine the inter-relationship between dietary habits, physical activity and health education provided at the PHC Centers in the Qassim region of Saudi Arabia.
Methodology
The primary objective of our study is to identify the dietary patterns among adult Saudi citizens visiting the PHC Centers in Qassim region, and to determine if there is a relationship between the dietary patterns, physical activity and the health education provided at the PHC Centers in the region.
Study design
The data used in this analysis arise from two separate studies, both conducted in the PHC Centers in Qassim region. The first of these was an operations research (OR) study, which was designed to assess the impact of health education on the community’s knowledge about the risk factors of lifestyle-related diseases. Respondents were randomly selected from among the patients visiting the PHC Centers. The second was a case-control study, which was designed to identify the lifestyle-related risk factors associated with type 2 diabetes mellitus in the same population. Cases (diabetic patients) and controls were randomly selected from among the patients visiting the PHC Centers. The questionnaires in both studies elicited the dietary patterns, level of physical activity and exposure to health education of the respondents. Interviews were conducted by the PHC Center’s staff including physicians and nurses using pre-coded questionnaires. The overall refusal rate was less than 5%. Data were entered and analyzed in SPSS Version 11.5 (SPSS Inc., 2007).
Sample size and sampling techniques
Sample size for the OR study was calculated to estimate the change in participants’ knowledge of the risk factors associated with diabetes, hypertension and coronary artery disease; sample size for the case-control was calculated to determine the association between dietary habits and physical activity and type 2 diabetes mellitus. The combined sample included in the present analysis is 2,789 participants (2,265 from the OR study and 524 from the case-control study). The present analysis attempted to quantify the association between dietary habits, physical activity and health education, after controlling for the effects of age, education, gender, and disease status. Our sample size has 90% power to detect a moderately strong association between dietary habits, physical activity and health education (at a confidence level of 95%). We believe that the combined sample is representative of adult Saudi population visiting the PHC Centers in Qassim region.
Statistical analysis
We used factor analysis to generate a common indicator of dietary practices. Food items routinely consumed during a typical 24-hour day were included in the factor analysis (Kabsa, barbecued meats, French fries/potato chips, fish, eggs, fresh vegetables, juices and beverages, fresh fruit, dates and bakery items). The score generated by factor analysis was a continuous variable with mean of zero and standard deviation of 1; it incorporated the correlation between food items and at the same time captured the variation in dietary habits. We converted this score into a binary variable representing ‘healthy’ and ‘unhealthy’ dietary practices by classifying score ≤ 0 into ‘healthy’ and score > 0 into ‘unhealthy’ dietary pattern. The binary variable was consistent with actual dietary practices, as follows: Healthy dietary pattern represented preference for fish, vegetables, fresh fruits and barbecued meats; unhealthy dietary pattern represented preference for Kabsa, eggs, French fries/potato chips, juices/soft drinks and bakery items. Preference for dates was similar among both groups.
We also developed a binary variable representing physical activity (yes/no); ‘yes’ represented the respondents who were in the habit of walking, jogging or engaging in a sports activity and/or having a job requiring some physical exertion, while ‘no’ represented respondents who had a sedentary lifestyle and whose job did not require any physical exertion.
We applied Chi-squared test to estimate the statistical significance of relationship between variables. The strength of association between dietary pattern, physical activity and exposure to health education was evaluated through logistic regression; adjusted odds ratios were obtained after controlling for age, gender, education, marital status, and history of chronic illness.
Results
Our sample included 1,806 (64.8%) men and 981 (35.2%) women. Table 1 presents the distribution of respondents by age-group, marital status, education, history of chronic diseases and family history of diabetes mellitus by gender. Significantly more females were divorced and widowed than males; females were also more likely to be suffering from hypertension and diabetes. Females are less likely to have secondary school and university education. Due to a large sample size, all of these differences are statistically significant.
Table (1). Demographic characteristics, medical history and family history of respondents.
| Percentage distribution of respondents | Male | Female |
|---|---|---|
| Number of respondents | 1,804 | 980 |
| Age-group: | ||
| < 30 years | 20.3 | 18.8 |
| 30 – 39 years | 25.2 | 30.4 |
| 40 – 49 years | 22.8 | 25.0 |
| 50 – 59 years | 18.1 | 17.7 |
| ≥ 60 years | 13.7 | 8.2 |
| Marital status: | ||
| Married | 70.4 | 58.7 |
| Divorced | 14.4 | 22.2 |
| Widowed | 0.3 | 5.0 |
| Single (never married) | 15.0 | 14.1 |
| Education (highest level of schooling): | ||
| Primary school | 20.6 | 41.7 |
| Preparatory school | 12.3 | 10.4 |
| Secondary school | 27.1 | 14.4 |
| University degree | 34.4 | 26.4 |
| Other (professional diploma, etc.) | 5.7 | 7.2 |
| Respondents suffering from a chronic disease: | ||
| Hypertension | 14.2 | 19.8 |
| Type 2 diabetes mellitus | 26.9 | 29.9 |
| Coronary artery disease | 2.7 | 2.1 |
| Family history of diabetes mellitus: | ||
| Mother has diabetes mellitus | 27.0 | 36.3 |
| Father has diabetes mellitus | 17.6 | 16.7 |
Nearly half (49.1%) of males and 34.7% females had received health education from the PHC Center. Patients suffering from hypertension, diabetes and/or coronary artery diseases were more likely to receive health education than the patients who were not suffering from these diseases. In both categories, significantly greater proportion of males than females received health education. Similarly, older persons were more likely to receive health education, but in each age-group, fewer women had exposure to health education (Table 2).
Table (2). Percentage of respondents having exposure to health education from PHC Center, by sex and history of chronic illness and age-group.
| Percent of respondents who received health education from a PHC Center | Male | Female |
|---|---|---|
| Suffering from any chronic disease*: | ||
| No | 42.8 | 26.6 |
| Yes | 61.0 | 47.3 |
| Age-group*: | ||
| < 30 years | 42.8 | 22.3 |
| 30 – 39 years | 42.6 | 32.9 |
| 40 – 49 years | 47.4 | 38.4 |
| 50 – 59 years | 60.4 | 41.4 |
| ≥ 60 years | 57.9 | 43.8 |
| All respondents* | 49.1 | 34.7 |
| Number | 1,806 | 981 |
Differences between males and females are statistically significant (P < 0.05)
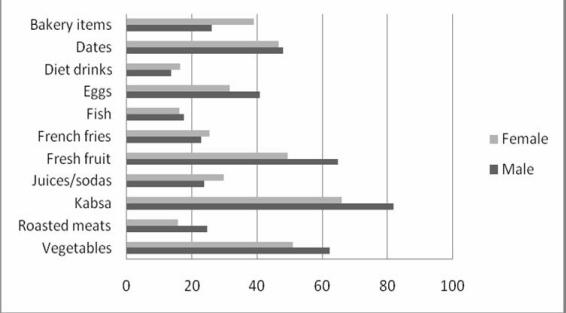
Figure (1) shows the percentage distribution of respondents by dietary habits and gender. Kabsa, a traditional meat and rice dish, is the most popular food item. Dates, bakery items, eggs and juices and soft drinks are also popular. Interestingly, fresh vegetables and fresh fruits are also routinely included in the diet. There are differences in dietary habits of males and females: eggs, Kabsa, roasted meats and fruits and vegetables are relatively more popular among men than women.
Fig. (1). Regular diet in 24 hours (Percent).
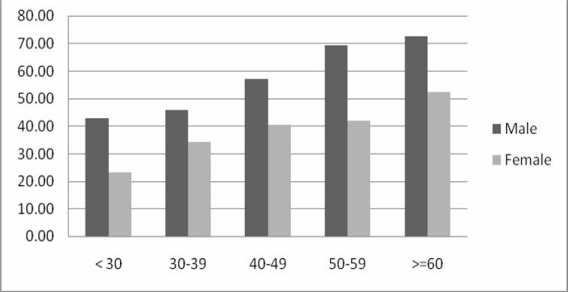
Figure (2) presents the percent of healthy dietary pattern by age-group and sex. The proportion of respondents having healthy diet steadily increases with age among both males and females; however, the proportion of healthy diet among females is lower than the males at each age.
Fig. (2). Percent of respondents having healthy dietary pattern by age-group and sex.
Table (3) presents results of logistic regression analysis where dietary pattern (healthy or unhealthy) is the dependent variable. With reference to married persons, single and divorced/widowed persons are more likely to have unhealthy dietary pattern. Females are nearly twice more likely to have unhealthy dietary patterns than males. However, increasing age and presence of a chronic disease have a protective effect against unhealthy dietary patterns. Previous exposure to health education reduces the risk of having unhealthy dietary pattern by 30%. This effect is statistically significant after controlling for the effects of age, sex, marital status, education and presence of chronic disease. Being physically active also reduces the risk of having unhealthy dietary pattern. Education does not have any effect on the dietary pattern when adjusted for the other variables shown in the table.
Table (3). Adjusted odds ratios1 and 95% confidence limits for unhealthy dietary patterns, by selected characteristics of respondents.
| Adjusted odds ratio | 95% confidence limits | |
|---|---|---|
| Gender: | ||
| Male (reference category) | 1.0 | |
| Female | 1.9 | 1.6 – 2.3 |
| Age-group: | ||
| < 30 years (reference category) | 1.0 | |
| 30 – 39 years | 1.0 | 0.7 – 1.3 |
| 40 – 49 years | 0.7 | 0.5 – 0.9 |
| 50 – 59 years | 0.5 | 0.3 – 0.7 |
| ≥ 60 years | 0.4 | 0.2 – 0.5 |
| Education level (highest level achieved): | ||
| Primary school (reference category) | 1.0 | |
| Preparatory school | 0.9 | 0.6 – 1.2 |
| Secondary school | 1.0 | 0.8 – 1.3 |
| University degree | 0.9 | 0.7 – 1.3 |
| Other (professional diploma, etc.) | 0.7 | 0.5 – 1.0 |
| Marital status: | ||
| Married (reference category) | 1.0 | |
| Single (never married) | 1.8 | 1.4 – 2.4 |
| Divorced/widowed | 1.9 | 1.5 – 2.4 |
| Chronic illness: | ||
| No (reference category) | 1.0 | |
| Yes | 0.8 | 0.6 – 1.0 |
| Received health education from PHC Center: | ||
| No (reference category) | 1.0 | |
| Yes | 0.7 | 0.6 – 0.8 |
| Physical activity: | ||
| Not physically active (reference category) | 1.0 | |
| Physically active | 0.7 | 0.6 – 0.9 |
Computed through logistic regression analysis (SPSS Inc. 2007); odds ratio for each variable is adjusted by controlling the effects of all of the rest of the variables shown in this table.
Table 4 presents the logistic regression model with physical activity (yes/no) as dependent variable. Divorced/widowed persons are twice more likely to be physically active than the married persons, but there is no difference between the married and the single persons in this regard. Those suffering from a chronic disease are also more likely to be physically active. Those having secondary school and university level education are also significantly more likely to be physically active. Physical activity drastically reduces with age: those 60 years and above are 70% less likely to be physically active than those < 30 years of age. Previous exposure to health education through the PHC does not seem to have any impact on physical activity. However, those having an unhealthy dietary pattern are also less likely to be physically active. Finally, women are about 50% less likely to be physically active than men.
Table (4). Adjusted odds ratiosi and 95% confidence limits for physical activityii, by selected characteristics of respondents.
| Adjusted odds ratio | 95% confidence limits | |
|---|---|---|
| Gender: | ||
| Male (reference category) | 1.0 | |
| Female | 0.5 | 0.4 – 0.6 |
| Age-group: | ||
| < 30 years (reference category) | 1.0 | |
| 30 – 39 years | 0.7 | 0.5 – 0.9 |
| 40 – 49 years | 0.6 | 0.4 – 0.8 |
| 50 – 59 years | 0.5 | 0.3 – 0.7 |
| ≥ 60 years | 0.3 | 0.2 – 0.4 |
| Education level (highest level achieved): | ||
| Primary school (reference category) | 1.0 | |
| Preparatory school | 1.3 | 0.9 – 1.7 |
| Secondary school | 1.4 | 1.1 – 1.7 |
| University degree | 1.7 | 1.3 – 2.1 |
| Other (professional diploma, etc.) | 1.3 | 0.9 – 1.8 |
| Marital status: | ||
| Married (reference category) | 1.0 | |
| Single (never married) | 1.2 | 0.9 – 1.5 |
| Divorced/widowed | 2.0 | 1.6 – 2.4 |
| Chronic illness: | ||
| No (reference category) | 1.0 | |
| Yes | 1.3 | 1.1 – 1.6 |
| Received health education from PHC Center: | ||
| No (reference category) | 1.0 | |
| Yes | 1.1 | 0.9 – 1.8 |
| Dietary pattern: | ||
| Healthy (reference category) | 1.0 | |
| Unhealthy | 0.7 | 0.6 – 0.9 |
Computed through logistic regression analysis (SPSS Inc. 2007); odds ratio for each variable is adjusted by controlling the effects of all of the rest of the variables shown in this table.
Physical activity is defined as a person who is reasonably active (walks, does regular exercise, participates in sports activities and/or has a job that requires physical exertion).
Discussion
Our study has several limitations and the results must be interpreted with caution. Firstly, the original studies supplying data for this analysis were different in design, although both collected data through one-time encounters with the respondents. Secondly, while the logistic regression models provide estimates for association between variables, a temporal relationship is impossible to establish. However, logic can be applied to guess the direction of cause-effect relationship. Finally, an information bias may also exist, whereby the information provided by respondents may have been influenced by the environment in which the interview was being conducted.
In spite of these weaknesses, the study provides an insight into the issue of relationship between dietary habits, physical activity and the impact of health education on either or both of these variables. In summary, women and unmarried persons are more likely to have unhealthy dietary practices and be physically less active. Presence of a chronic disease appears to be a motivation to eat right and be physically active. With increasing age, people are more likely to eat healthier but, at the same time, they become less active. Education does not seem to have an association with dietary patterns but educated people are more likely to be physically active. And, finally, health education provided at the PHC Centers has a positive impact on dietary practices, but is not associated with increased physical activity.
Studies from other parts of the world have shown that health education might change behaviors. Singapore’s National Healthy Lifestyle Program has been shown to significantly decrease smoking prevalence and increase regular exercise over a six years’ period. The prevalence rates of obesity and diabetes mellitus also stabilized over this period, although prevalence of high total blood cholesterol and hypertension increased.(9) More or less similar results are shown by a national program in Mauritius during 1990 – 1995.(10)
A disconcerting finding of our study was that women lead less healthy lives than men. From anecdotal evidence, it appears that since women engage in daily household chores they do not have the time or the desire to engage in regular exercise. However, exercise is equally important for males and females. Recent studies have shown that household chores do not provide women a good protection against the risk of non-communicable disease and strenuous exercise such as brisk walking is necessary.(11)
In Saudi Arabia, the ‘culture’ of a healthy lifestyle is yet to gain popularity. It has been shown that such environment does have a direct impact on the lifestyle, particularly with regard to regular exercise.(12).
Lifestyle practices tend to ‘cluster’ among individuals. For example, those having a prudent lifestyle tend to be non-smokers, do regular exercise and also have good dietary practices. On the other hand, individuals who have poor dietary habits also lack physical activity. Both sets of behavior are determined by inherent beliefs and the level of awareness, the latter group, for example, having their own definition of a ‘healthy lifestyle.’ The interrelation of unhealthy lifestyle and misinformation about causation of disease has been demonstrated in a study in the Netherlands.(13) A review study of a substantial number of published articles, conducted during the 1980s, also found that interrelationship between the known risk behaviors exists.(14) It has been shown that physical inactivity, obesity, smoking and alcoholism tend to be interrelated.(14) We have successfully identified these clusters through factor analysis, and forged out a single variable that captures the correlations between various dietary practices.
Application of these findings from literature to our study population is rather straight forward: In Saudi Arabia, like in any other society having similar characteristics, an upsurge in the prevalence of non-communicable diseases is related directly to a host of behavioral factors, which can be modified through community-based health education. Promoting a healthy lifestyle and informing the public about the hazards of sedentary life and unhealthy diet is the only way to control and contain the unprecedented increase in the lifestyle-related diseases in Saudi Arabia. From our study, it is clear that health education provided at the PHC centers already plays a modest but significant role in improving dietary habits.
Conclusions and Recommendations
Certain population subgroups (women, older people, divorced and widowed persons and those with low education), are at a greater risk of having unhealthy lifestyles and should be targeted through customized health education programs. Patients suffering from chronic illnesses are more likely to receive health education from the PHC centers, which helps to improve their dietary practices but does not have the desired impact on physical activity. Therefore, improving the quality and scope of health education would significantly reduce the burden of non-communicable diseases in our target population.
We conclude that greater emphasis on high quality health education, provided through the PHC centers, would have a larger and significant positive impact on the lifestyles in our target population, and by extension to the rest of the population in Saudi Arabia.
Acknowledgments
This study was made possible by a grant from the Deanship of Research, Qassim University, Saudi Arabia. We are indebted to the Ministry of Health, Qassim region, and the staff of the primary health care centers where the study was conducted for their cooperation. The authors take full responsibility of the contents of this article; views expressed are not necessarily those of Qassim University, the Deanship of Research, or the Ministry of Health, Saudi Arabia.
References
- 1.Al-Hazzaa HM. Prevalence of physical inactivity in Saudi Arabia: a brief review. East Mediter Health J. 2004;10(4/5):663–670. [PubMed] [Google Scholar]
- 2.Al-Rukban MO. Obesity among Saudi male adolescents in Riyadh, Saudi Arabia. Saudi Med J. 2003:27–33. [PubMed] [Google Scholar]
- 3.Alwan A. Non-communicable diseases: a major challenge to public health in the region. East Mediter Health J. 1997:6–16. [Google Scholar]
- 4.World Health Organization. WHO; Geneva: 2003. Annual global movement for health initiative: A concept paper. (WHO Ref. WHO/NMH/PAH/03.1) [Google Scholar]
- 5.Ministry of Health Kingdom of Saudi Arabia . Riyadh; Sauid Arabia: 2004. Guidelines of Chronic Diseases, Introduction (Hamad Al Manea) [Google Scholar]
- 6.Mickey Chopra, Sarah Galbraith, Ian Darnton-Hill. Introduction to PHC Bulletin of World Health Organization Vol. 80 No.12. Geneva: 2002. [Google Scholar]
- 7.Ministry of Health Kingdom of Saudi Arabia Principles and Practice of PHC. 2002. Health Education, P101.
- 8.Dawber TR, Meadors GF, Moore FE. Epidemiological Approaches to Heart Disease. The Framingham Study Presented at Joint Session of American Public Health Association’s 78th Annual Meeting; St. Louis, Mo., USA. November 3, 1950; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cutter J, Yian Tan B, Kai Chew S. Levels of cardiovascular disease risk factors in Singapore following a national intervention program. Bulletin of the World Health Organization. 2001;79:908–915. [PMC free article] [PubMed] [Google Scholar]
- 10.Dowse GK, et al. Changes in population cholesterol concentrations and other cardiovascular risk factor levels after five years of the non-communicable disease intervention program in Mauritius. Br Med J. 1995;311:1255–1259. doi: 10.1136/bmj.311.7015.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawlor DA, Taylor M, Bedford C, Ebrahim S. Is housework good for health? Levels of physical activity and factors associated with activity in elderly women. Results from British Women’s Heart and Health Study. J Epidemiol Comm Health. 2002;56:473–478. doi: 10.1136/jech.56.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sundquist J, Malstorm M, Johansson SE. Cardiovascular risk factors and the neighborhood environment: a multilevel analysis. Intern J Epidemiol. 1999;28:841–845. doi: 10.1093/ije/28.5.841. [DOI] [PubMed] [Google Scholar]
- 13.Kok FJ, Matroos AW, van den Ban AW, Hautvast AJ. Characteristics of individuals with multiple behavioral risk factors of coronary heart disease: The Netherlands. Am J Pub Health. 1982;72:986–991. doi: 10.2105/ajph.72.9.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blair SN, Jacobs DR, Jr, Powell KE. Relationship between exercise or physical activity and other health behaviors. Public Health Reports. 1985 Mar–Apr;100(2):172–180. [PMC free article] [PubMed] [Google Scholar]