Abstract
Objective
To compare the circadian variation of hourly heart rate variability (HRV) on work and non-workdays among boilermaker construction workers.
Method
A panel study of 18 males monitored by 24-h ambulatory ECG over 44 observation-days on paired work and non-workdays was conducted. ECGs were analysed and the SD of normal-to-normal beats index (SDNNi) was calculated from 5-min data and summarised hourly. SDNNis over work and non-workdays were compared using linear mixed-effects models to account for repeated measures and harmonic regression to account for circadian variation.
Results
Both work and non-work hourly HRV exhibited circadian variation with an increase in the evening and a decrease in the afternoon. SDNNi was lower on workdays as compared with non-workdays with the largest, statistically significant differences observed between 10:00 and 16:00, during active working. Lower SDNNi, albeit smaller yet statistically significant differences, was also observed in the evening hours following work (17:00–21:00) and early morning (4:00). In regression models using all time periods, an average workday SDNNi was 8.1 ms (95% CI –9.8 to –6.3) lower than non-workday SDNNi. The circadian pattern of HRV exhibited two peaks which differed on work and non-workdays.
Conclusion
While workday and non-workday HRV followed a circadian pattern, decreased HRV and variation of the circadian pattern were observed on workdays. Declines and changes in the circadian pattern of HRV is a concern among this exposed population.
BACKGROUND
Like many cardiovascular parameters including blood pressure and inflammatory markers, heart rate variability (HRV), a marker of cardiovascular autonomic control, exhibits cyclical fluctuations over 24-h periods, known as circadian variation. The 24-h patterns in HRV result from endogenous influences including homeostatic control mechanisms as well as exogenous influences such as physical and mental activity or smoking.1 While impaired or absent circadian fluctuation of HRV is observed following cardiovascular events including stroke,2 research also suggests that disturbance in the circadian rhythm of cardiovascular parameters may be a risk factor for cardiovascular outcomes.3 4
Investigations of air pollution exposures have demonstrated particle-induced cardiovascular effects including altered cardiac autonomic function demonstrated by consistent declines in HRV following particle exposures.5 Statistically significant (p<0.05) declines in HRV have also been observed in our previous investigation of welders; we observed an early (2–3 h) and late (9–13 h) HRV response following metal-rich particle exposures.6 However, it remains unclear whether in addition to causing post-exposure HRV declines, workday particle exposures also cause a disruption in the circadian variation of HRV. In a panel study of welders, we compared the circadian variation of HRV over two 24-h periods on work and non-workdays.
What this paper adds.
▶ Like many cardiovascular parameters, heart rate variability (HRV) exhibits circadian variation.
▶ The influence of occupational exposures on the circadian variation of HRV is unknown.
▶ Among a panel of welders, HRV exhibits a circadian variation over both workdays and non-workdays with lower HRV and a change in circadian pattern on workdays.
▶ Studies investigating the cardiovascular effects of environmental and workplace exposures should consider changes in the circadian pattern of cardiovascular measures including HRV.
METHODS
The Institutional Review Board at the Harvard School of Public Health approved the study protocol, and written informed consent was obtained from each adult prior to participation. From 1999 to 2006, we recruited apprentice boilermaker construction workers or ‘boilermakers’ from a union to participate in a paired work and non-workday panel study. Participants were monitored by ambulatory ECG at a training school over the duration of a work shift and while at home for up to 24 h. For the current study, 18 participants who were monitored for a minimum of 22 h starting between 8:00 and 11:00 were eligible for inclusion in the analysis.
Over a work shift, boilermakers received instruction and practised shielded metal arc (stick) and gas metal arc welding, most commonly using base metals of mild steel and stainless steel. Personal, integrated, gravimetric particulate matter with an aerodynamic diameter of <2.5 μm (PM2.5) samples were collected over the duration of the work shift as previously described in detail.7 Like workday monitoring, non-workday monitoring occurred at the union hall when participants were not welding and while at home over a 24-h period. Non-workday monitoring occurred within 5 months of workday monitoring, although 86% occurred within the same week. While the majority (64%) of workers were monitored once, four workers were monitored twice during different years.
A self-administered questionnaire was used to collect information on medical history, medication use, and smoking history. Participants were fitted with a standard 5-lead ECG Holter monitor each workday or non-workday morning. Each cardiac tape was sent to Raytel Cardiac Services (Haddonfield, NJ, USA) for processing and analysis using a DelMar Avionic (Irvine, CA, USA) Model Strata Scan 563. Trained technicians, blinded to the work and non-work periods, used standard criteria to accept or reject all normal or abnormal findings. The duration between consecutive R waves of the ECG (RR interval) was identified and only beats with an RR interval between 0.6 and 1.5 s and ratio of 0.8–1.2 were included in the analysis. Tapes were analysed in the time domain, and the SD of all normal-to-normal intervals (SDNN) was calculated for all 5-min segments. The SDNN index (SDNNi), calculated from the mean of the 5-min SDNN, was summarised hourly.
Since declines in HRV are observed up to 14 h following welding,6 the entire 24-h period from the start of the work shift was considered to be the work period. To account for correlated outcomes among workers who participated over multiple years, linear mixed-effects regression models with random intercepts for individuals, an indicator variable for work/non-work period and unstructured covariance, were used to examine the difference between work and non-work SDNNi within hourly individual models. Using a repeated, balanced study design, each participant served as their own control, which eliminates confounding by individual factors that effect HRV, such as age or smoking status.
Each hourly measurement was pooled into one model to assess disruption in the circadian pattern and to identify the mean difference in SDNNi between work and non-work over the entire measurement period. A linear mixed-effects model with random intercepts for each individual, an indicator variable for work period, and the first and second harmonic regression coefficients for time [sin (2π(t)/24); cos(2π(t)/24); sin (2π(t)/12); and cos(2π(t)/12), where t is the time of day] were used with an interaction term between the four harmonic regression variables and work to investigate whether the circadian pattern of HRV varied over time. Model fit for harmonic and interaction terms was assessed using the likelihood ratio test and χ2 distributions. Statistical significance was assessed at the α=0.05 level. Analyses were performed using SAS version 9.1.
RESULTS
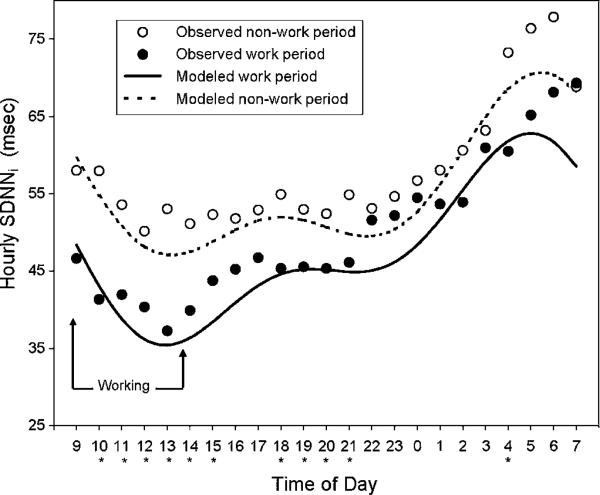
The 18 male participants had a mean (SD) age of 44 (12) years. Seventeen males were Caucasian and one was Hispanic. Seven (39%) were active smokers and four (22%) were hypertensive. Hourly SDNNi on work and non-workdays exhibited a circadian pattern, increasing in the sleeping hours, peaking at 6:00 on a non-workday and 7:00 on a workday (figure 1). Hourly SDNNi was consistently lower on workdays as compared with non-workdays.
Figure 1.
The observed and modelled circadian variation of hourly SD of normal-to-normal beats index (SDNNi) by work and non-work periods among 18 male boilermakers monitored over 22 paired occasions.
*Statistically significant (p<0.05) difference between work and non-work period.
On average, participants started work at 9:15 (range 8:00–10:50) and ended at 14:17 (range 11:30–15:30) and the mean (SD) work shift PM2.5 exposure was 1.10 (1.11) mg/m3. While working, hourly SDNNi gradually declined until 13:00 when SDNNi increased (figure 1). Beginning at 14:00, when an average workday ended, hourly SDNNi increased over the remainder of the 24-h period, yet remained lower than non-workday SDNNi. The largest differences in workday and non-workday hourly SDNNi were observed while working. Smaller, yet statistically significant (p<0.05), differences in SDNNi were also observed in the evening (18:00–21:00) and early morning (4:00).
These findings were consistent in the pooled analysis with HRV from all time periods and a harmonic regression coefficient for time (figure 1). On average, workday SDNNi was 8.1 ms (95% CI –9.8 to –6.3) lower than non-workday SDNNi. The circadian pattern of SDNNi exhibited two peaks over time as both the first and second harmonic regression terms improved model fit (test statistic of 279, p<0.0001). The pattern of circadian variation differed by work and non-work periods, as indicated by an improved model fit after the inclusion of an interaction term for the work period (test statistic of 18.8, p<0.001).
DISCUSSION
In a panel study of welders, work and non-workday SDNNi exhibited circadian variation with lower SDNNi on workdays as compared with non-workdays. The largest difference in SDNNi was observed during active work although statistically significant lower SDNNi was also observed from 18:00 to 21:00 and 4:00, which is consistent with the early (2–3 h) and late (9–13 h) response previously observed in this cohort.6 The pattern of circadian rhythm was altered on workdays as evident by the significant interaction terms between the harmonic terms and work in the analysis of all time points. The non-workday peak in SDNNi in the early morning hours occurred at 6:00 on non-workdays and was delayed until 7:00 on workdays.
While declines in HRV are clearly associated with impaired cardiovascular health,8 the clinical significance of disruption of the circadian variation of HRV remains a topic of current investigation. Toxicological investigations suggest that circadian dysregulation of cardiovascular parameters may be an aetiological cause of cardiovascular disease.4 Discordance between internal and external rhythms and links between cardiovascular organ damage have been demonstrated in hamsters9 and mice.10 11 While large-scale disruption of circadian rhythms, as is observed in shift workers, is associated with cardiovascular morbidity and mortality,12 it is unclear whether the small shift in HRV observed within this cohort is clinically significant.
While PM2.5 exposures were monitored during active working, exposure monitoring was not performed following work or on non-workdays. Therefore, the study cannot discern what workday factor, such as metal-rich particles, increased activity, or whether noise may be responsible for the declines in SDNNi. Activity levels differed between work and non-work periods with statistically significant differences in heart rate from 9:00 to 21:00 (data not shown). However, when we adjusted the SDNNi analysis for heart rate (HR), a surrogate of physical activity, the decline in SDNNi over the workday persisted. Our previous investigation within this cohort found statistically significant exposure–response relationships between hourly changes in SDNNi and PM2.5.6 It is plausible that disruption of the circadian rhythm of HRV, which is a reflection in the variation in autonomic nervous system activity as well as the sympathetic-parasympathetic autonomic balance,1 is a response to particle elicited autonomic responses.5 Growing research in the areas of circadian rhythms and cardiovascular function including the role of circadian clock genes and diurnal variation of gene expression13 may provide further insight into the role of environmental exposures and cardiovascular disease.
In summary, while SDNNi exhibited circadian variation on work and non-workdays, hourly SDNNi was lower on workdays as compared to non-workdays and the difference was greatest during active working. The pattern of circadian variation varied by work and non-workdays. The circadian variation of cardiovascular parameters and the influence of environmental exposures on circadian disruption should be considered in epidemiological investigations.
Acknowledgements
This research was supported by NIEHS grants ES009860 and ES00002. JMC was supported by T32 ES 07069, T42 OH008416, The Flight Attendants Medical Research Institute. The authors thank R Hauser, R Herrick, JY Kim, S Magari, J Schwartz, and the International Brotherhood of Boilermakers, Local 29, Quincy, MA, USA.
Funding Other funders: NIH; Flight Attendants Medical Research Institute.
Footnotes
Competing interests None declared.
Ethics approval This study was conducted with the approval of the Harvard School of Public Health.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Guo YF, Stein PK. Circadian rhythm in the cardiovascular system: chronocardiology. Am Heart J. 2003;145:779–86. doi: 10.1016/S0002-8703(02)94797-6. [DOI] [PubMed] [Google Scholar]
- 2.Korpelainen JT, Sotaniemi KA, Huikuri HV, et al. Circadian rhythm of heart rate variability is reversibly abolished in ischemic stroke. Stroke. 1997;28:2150–4. doi: 10.1161/01.str.28.11.2150. [DOI] [PubMed] [Google Scholar]
- 3.Montagnana M, Salvagno GL, Lippi G. Circadian variation within hemostasis: an underrecognized link between biology and disease? Semin Thromb Hemost. 2009;35:23–33. doi: 10.1055/s-0029-1214145. [DOI] [PubMed] [Google Scholar]
- 4.Martino TA, Sole MJ. Molecular time: an often overlooked dimension to cardiovascular disease. Circ Res. 2009;105:1047–61. doi: 10.1161/CIRCRESAHA.109.206201. [DOI] [PubMed] [Google Scholar]
- 5.Brook RD. Is air pollution a cause of cardiovascular disease? Updated review and controversies. Rev Environ Health. 2007;22:115–37. doi: 10.1515/reveh.2007.22.2.115. [DOI] [PubMed] [Google Scholar]
- 6.Cavallari JM, Fang SC, Eisen EA, et al. Time course of heart rate variability decline following particulate matter exposures in an occupational cohort. Inhal Toxicol. 2008;20:415–22. doi: 10.1080/08958370801903800. [DOI] [PubMed] [Google Scholar]
- 7.Cavallari JM, Eisen EA, Fang SC, et al. PM2.5 metal exposures and nocturnal heart rate variability: a panel study of boilermaker construction workers. Environ Health. 2008;7:36. doi: 10.1186/1476-069X-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93:1043–65. [PubMed] [Google Scholar]
- 9.Martino TA, Oudit GY, Herzenberg AM, et al. Circadian rhythm disorganization produces profound cardiovascular and renal disease in hamsters. Am J Physiol Regul Integr Comp Physiol. 2008;294:R1675–83. doi: 10.1152/ajpregu.00829.2007. [DOI] [PubMed] [Google Scholar]
- 10.Martino TA, Tata N, Belsham DD, et al. Disturbed diurnal rhythm alters gene expression and exacerbates cardiovascular disease with rescue by resynchronization. Hypertension. 2007;49:1104–13. doi: 10.1161/HYPERTENSIONAHA.106.083568. [DOI] [PubMed] [Google Scholar]
- 11.Anea CB, Zhang M, Stepp DW, et al. Vascular disease in mice with a dysfunctional circadian clock. Circulation. 2009;119:1510–17. doi: 10.1161/CIRCULATIONAHA.108.827477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawachi I, Colditz GA, Stampfer MJ, et al. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92:3178–82. doi: 10.1161/01.cir.92.11.3178. [DOI] [PubMed] [Google Scholar]
- 13.Young ME. Anticipating anticipation: pursuing identification of cardiomyocyte circadian clock function. J Appl Physiol. 2009;107:1339–47. doi: 10.1152/japplphysiol.00473.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]