Abstract
OBJECTIVES
Hearing loss is the most common congenital condition screened for at birth in the United States and more than 95% of newborns are currently screened for hearing. Newborn hearing screening is most effective when infants receive timely and effective interventions. Unfortunately follow-up rates for babies not passing their initial hearing screens are as low as 50% in some states. Midwives are well positioned to encourage families to follow-up with their neonatal providers when babies are referred for further testing. Newborn hearing screening is a relatively new practice in the United States and to date there has been no research regarding the informational needs and practices of certified nurse midwives or certified midwives related to hearing screens. This study examined the knowledge, attitudes, and follow-up practices of midwives related to newborn hearing screening and intervention.
METHODS
A survey instrument was developed and sent to 5,255 ACNM members in 50 states and 2 territories. Five hundred and eighteen surveys were returned, yielding a response rate of 9.9%.
RESULTS
Only 68% of respondents said it was very important to screen all newborns for hearing loss. Respondents reported significant gaps in their knowledge about screening procedures, steps for referral, and the availability of resources when newborns did not pass the test. Midwives also reported the need for information about hearing loss conditions and genetics, screening guidelines, protocols for follow up, referral networks, and therapies available.
DISCUSSION
Current practices in newborn hearing screening and intervention programs can be enhanced by strengthening the basic midwifery knowledge of and rationale for follow-up when newborns fail their hearing screens. Midwives can play an integral role in optimizing hearing, speech, and family interaction by assuring that each baby born into midwife hands accesses the best hearing screening and referrals.
Keywords: newborn hearing screening, certified nurse midwives, certified midwives, knowledge, childhood hearing loss, sensorineural hearing loss
Hearing loss is the most common congenital condition screened for at birth in the United States, and 3 per 1000 infants are born with permanent hearing loss. Left undetected, hearing loss in infants can negatively affect speech, language, academic and psychosocial development.1 However, research demonstrates that these negative consequences can be minimized or prevented through early identification and intervention.2–5 Because of this, the National Institutes of Health's Consensus Development Conference on Early Identification of Hearing Loss concluded that all infants should be screened for hearing impairment, preferably prior to hospital discharge.6
Universal Newborn Hearing Screening Programs have been implemented nationwide over the past decade and currently 95% of newborns are screened for hearing loss at birth.1 This initiative was driven in part by the availability of cost-effective and valid objective screening measures, called Otoacoustic Emissions and Auditory Brainstem Response Testing. Although hearing screens are not legally required in all states, voluntary screening augments the newborn hearing screening programs that are legislatively mandated in 43 states.1 Prior to newborn hearing screening, it was common for children with hearing loss to be identified after two years of age or later, resulting in delays in speech, language and social development.1 The expansion of newborn hearing screening in the past decade has been successful in reducing the average age of identification of infants with permanent childhood hearing loss,1,2 allowing families and professionals to optimize infants’ auditory, speech and language learning.2–5 The history of newborn screening and the pathophysiology of hearing loss have recently been reviewed in the Journal of Midwifery and Women’s Health.7
The success of newborn hearing screening programs depends on the ability to link screening with timely and effective diagnosis and intervention. In 2002, the American Academy of Pediatrics (AAP) and the National Center for Hearing Assessment and Management disseminated Guidelines for Pediatric Medical Home Providers, a flowchart that emphasizes the importance of (1) completing newborn hearing screening before 1 month of age, (2) diagnosing hearing loss before 3 months, and (3) enrolling those identified with hearing loss in early intervention before 6 months.8 Accomplishing these goals requires timely follow-up at each stage.
Two issues currently threaten the effectiveness of the newborn hearing screening effort: (1) failure to follow-up newborns not passing the initial hearing screen and (2) failure to screen universally. In some regions, follow up rates are as low as 50 percent.4 Midwives can address the rates of screening by ensuring universal testing of all midwifery births, regardless of the place of birth. Midwives can be proactive in urging families to follow through on evaluations and referrals for their newborns who do not pass the initial hearing screen. Midwives are poised during the maternity cycle as educators and advocates to inform families of best practices in newborn hearing screening, with the goal of optimizing hearing health in their children.
Studies of the knowledge and practices of healthcare providers related to newborn hearing screening and follow-up are rare. Two recent studies explored the knowledge needs and learning preferences of pediatricians in relation to early hearing detection and intervention.9,10 Results indicated that pediatricians supported the effort, but needed more information on this topic to adequately support families in their care. They requested action-oriented, practical resources that guided them in patient management. To date, no similar studies have been conducted with CMs and CNMs. Because of the role they play in caring for families and newborns immediately after birth, research with this group is critically needed.
The current study comprises a national survey of CMs and CNMs on the topic of newborn hearing screening and follow-up. Specific goals of the survey were to understand current midwifery practices related to newborn hearing screening and follow-up, and to assess attitudes and related knowledge needs.
METHODS
A convenience sample was obtained through the American College of Nurse Midwives (ACNM) membership list. Solicitation of CNM/CM1 participants for this study was approved by the ACNM Division of Research in coordination with the ACNM Senior Staff Researcher. Approval from the Boys Town National Research Hospital Institutional Review Board was granted for the project and for waiving written consent before surveys was mailed. A copy of the survey tool is available. (See Supporting information: Appendix S1)
In total 5,255 questionnaires were mailed. Reminder postcards were mailed two weeks after the original mailings. Identification of non-respondents was not possible because replies were anonymous.
The survey tool was modified from a survey used previously with primary care providers.9, 10 The original survey was adapted by the first author to make it pertinent to the midwifery context. It was pilot-tested with midwifery providers in a Midwestern city.
RESULTS
Respondents
Of the mailed questionnaires, 518 (9.9%) useable surveys were returned within the established 4-month timeline. Responses were received from midwives in 46 states and two territories. The survey respondents were primarily female (99.6% of the sample) and were well distributed geographically, comprising 50.1% from metropolitan areas, 21.2% from small cities, and 20.2% from rural communities. The respondents came from a variety of practice settings, including hospital or women's health centers (38.1%), private OBGYN practices (32.0%) and CNM Midwifery practices (13.3%). The mean years of practice among respondents was 16.1 years (range = 1 – 52; SD = 10.3) and the majority (92.2%) reported that their hospitals or birth centers were participating in NHS. Table 1 summarizes demographic characteristics of the current sample, compared to a recent demographic survey conducted by ACNM.11
Table 1.
Demographic characteristics of current study respondents compared to ACNM Membership Survey 2006–2008.
| Newborn Hearing Screening Survey (N=5255), % |
2008 ACNM Member Survey N=5847), % |
|
|---|---|---|
| Response Rate, n(%) | 518 (9) | 2435 (42) |
| Percentage female | 99.6 | 98.2 |
| Average age, y (SD) | 49 (9.0) | 50 (IS THERE A SD?) |
| Years of practice, y (SD) | 16.1 (10.3) | 15.24 (9.57) |
| Practice Setting | ||
| Hospital practice | 38.1 | 29.7 |
| Private physician’s office | 32.0 | 22.5 |
| Midwifery owned practice | 13.3 | 7.5 |
| Hospital-based birth midwives | 79.8 | 67.4 |
| Free-standing birth center | 5.3 | 4.2 |
| Home birth | 2.4 | 3.6 |
| University/Academic | 2.2 | 10.7 |
| Responses by US Region (current survey) |
||
| East | 26.7 | |
| Southeast | 21.5 | |
| Midwest | 22.2 | |
| West | 18.6 | |
| Southwest | 8.8 | |
| Territories | 1.0 | |
| No response | 1.2 | |
Experiences, Attitudes and Role Perceptions
More than half of the responding midwives judged themselves as very familiar (30.0%) or somewhat familiar (30.9%) with newborn hearing screening. However, 89.1% reported that they were not directly involved in the newborn hearing screening programs. Almost all (91.0%) were aware that their state mandated some type of newborn hearing screening. Yet, most (89.1%) reported that they were unfamiliar with any state or national hearing resources such those provided through State Early Hearing Detection and Intervention programs. Furthermore, 51.5% reported that they never receive the results of newborn hearing screening for newborns in their care.
The present survey documented that 68.5% of responding midwives viewed newborn hearing screening as very important. However, 31.5% expressed uncertainty about the need, including 12.6% who judged newborn hearing screening to be "unimportant." When asked about their perceptions of the accuracy of newborn hearing screening measures, 24.3% of respondents were unsure and another 39.8% were only "somewhat confident." A universal screening procedure may be contraindicated if it prompts undue anxiety on the part of parents. Our data indicate that 78.6% of midwives currently do not see parental anxiety as a major barrier precluding universal newborn hearing screening. Midwives were asked to report what they perceived as barriers to follow up of screening results, based on their observations and experiences. The most frequent responses were that newborn hearing screening is “is not my responsibility” (91.1%), and they “lack the knowledge to guide families” (92.9%). Other frequent replies were that they did not know what to say (47.1%) and that they had to deal with other more pressing issues (43.9%).
Respondents were asked an open-ended question about what they believed the role of midwives to be in newborn hearing screening. Among those who answered this question (n = 460), 12.4% indicated they had no role. Others envisioned a role in educating families (41.4%), ensuring that screening is completed (29.5%), providing advocacy and support (3.5%), conducting screening (3.5%), or answering questions (1.7%).
Knowledge and Informational Needs
When asked how they learned about newborn hearing screening, 70.3% described on-the-job training as a primary or occasional training source. When asked about how well basic midwifery education prepared them about newborn hearing screening, 66.3% reported, “not at all” while 14.6% responded, “well.” In contrast, 51.2% of respondents indicated that on-the-job training prepared them “well” to address this topic, yet 29.9% perceived that it was of no help.
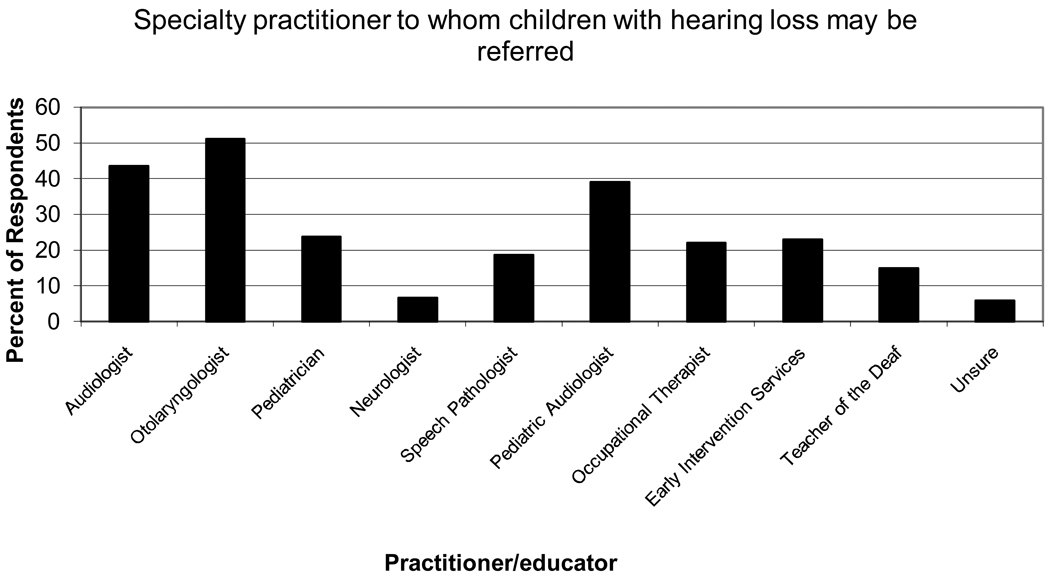
Midwives indicated a need for further information on follow-up practices in order to best counsel and refer parents after diagnosis. For example, 56.0% of respondents indicated they were either unprepared or not well-prepared to promote follow up for failed newborn hearing screens. Figure 1 summarizes the level of awareness of respondents about appropriate referrals for babies diagnosed with hearing loss. Only about half knew that a referral to an Ear, Nose & Throat physician (51.1%) or a pediatric audiologist (43.6%) was important.
Fig 1.
Summary of respondents’ open-ended replies to the question “to whom should an infant with hearing loss be referred?”
Many midwives were unaware of the earliest ages at which infants can receive various services for hearing health care. For example, even though definitive diagnosis of hearing loss is possible at 1 month of age, 4 45% thought it could not happen until 3–6 months of age or later (see Table 2). Similarly, babies can be fit with hearing aids as young as 1 month of age,4 but 63.6% thought that could not happen until 3–6 months of age or later.
Table 2.
Summary of respondents’ knowledge about the ages at which specific follow-up procedures should be implemented for children who do not pass initial hearing screening. The percentages of responses within each age category are reported.
| Q9. What is your best estimate of the earliest age at which: |
≤1 mo | 1–3 mos | 3–6 mos | 6–9 mos | 9–12 mos |
≥12 mos |
|---|---|---|---|---|---|---|
| a. A newborn not passing the hearing screening should receive additional testing |
58.3 | 36.2 | 1.5 | 3.1 | .7 | 0 |
| b. A child can be definitively diagnosed as having a permanent hearing loss |
22.3 | 32.5 | 25.7 | 3.1 | 11.87 | 4.3 |
| c. A child can begin wearing hearing aids |
17.9 | 17.9 | 30.9 | 3.7 | 19.7 | 9.3 |
| d. A child with permanent hearing loss should be referred to early intervention services |
38.6 | 20.7 | 23.5 | 1.1 | 10.5 | 5.1 |
Note: The grey area in the table signifies the percentage of responses that were inconsistent with the best practice recommendations for follow-up ages. The shaded area signifies inaccurate responses.
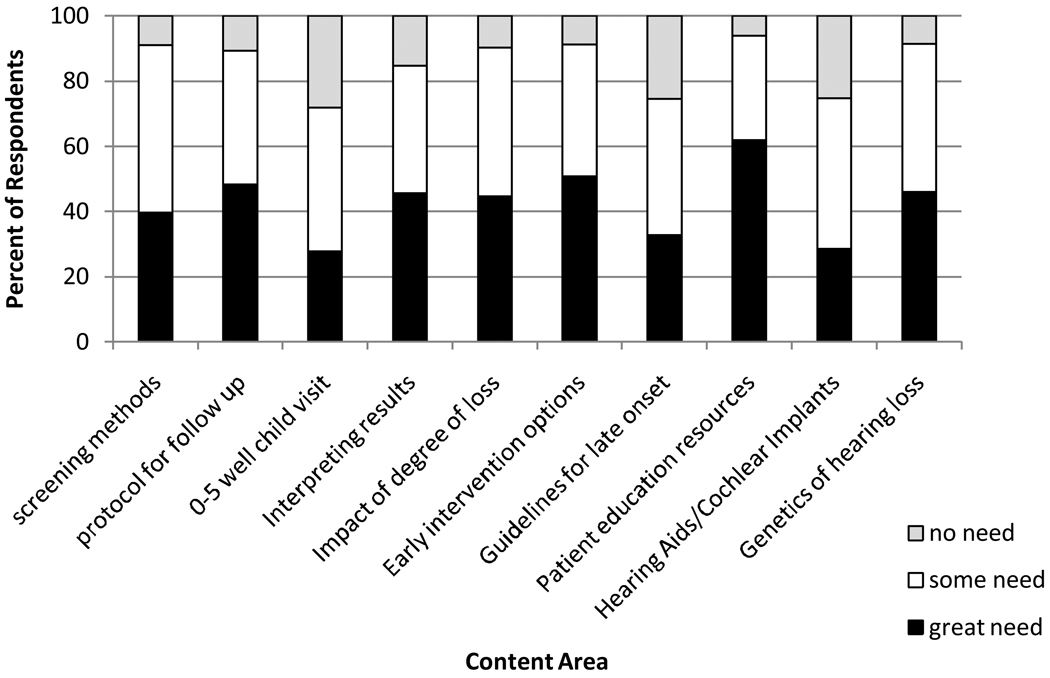
As shown in Figure 2, more than half of the respondents described themselves as uninformed about the following topics related to hearing loss: incidence (54.5%), medical interventions (62.6%) including cochlear implants (71.9%), hearing aids (61.7%), educational interventions (68.1%), and genetics (63.8%). Midwives self-identified content areas in which they wanted more continuing education concerning newborn hearing loss. The vast majority of midwives indicated that there was some or a great need for more information about screening methods (91.0%), protocols for follow up (89.4), impact of hearing loss on infant language development (90.4%), early intervention options (91.3%), patient education resources (93.9%), and the genetic factors related to hearing loss (91.4%).
Fig 2.
Specific topics recognized as continuing education needs by midwives.
When asked about mechanisms for learning about newborn hearing screening, respondents preferred the following resources: (1) parent education materials (93.2%), (2) protocol algorithms showing follow-up referrals and procedures (80.9%), and (3) web-based resources for learning about this topic (90.0%). Midwives expressed clear preferences for resources that support them in meeting the needs of families and promoting sound hearing health care for infants.
DISCUSSION
Experiences, Attitudes and Role Perceptions
The current study is the first to survey the attitudes and knowledge needs of midwifes on the topic of newborn hearing screening. Midwives are in a position to help improve one of the biggest problems with current programs, which is loss to follow up. The majority of participants in this study practiced in settings where newborn hearing screening was implemented, yet they reported that they are not involved in screening, do not typically receive results, and have limited awareness of resources provided through their State Early Hearing Detection and Intervention Program. These results suggest that existing programs are not well integrated into midwifery practices. Communication with midwives could be strengthened by having screening reports sent to midwifery practice sites. Provision of information and links to pregnant and newly delivered families through midwives could strengthen practices related to hearing screening, diagnosis and follow-up.
Attitudes, not just knowledge, are important to promote changes in healthcare practices.10 The results of this survey suggest the need to address midwives’ attitudes about the validity of screening tests and the importance of universal newborn hearing screening, as well as their perceived roles in screening and follow-up. Midwives need continuing education about screening procedures, acceptable false positive rates, and test validity. There is considerable evidence that newborn hearing screening tests are accurate12 and that most experts and physicians believe in the value of such screening.9, 10 Beliefs about the importance of newborn hearing screens may be linked to midwives’ clear understanding of the consequences for babies with hearing loss on their speech development, language acquisition, and learning. A clear understanding that even minimal hearing loss has consequences for the development of speech and language13 will put midwives in a better position to guide families.
Most midwives stated that newborn hearing screening is not their responsibility and that they lack the knowledge to guide families. These attitudes may interact; midwives who perceive limited responsibility for screening may not pursue education on this topic. It is likely that perceptions about limited midwifery roles in newborn hearing screening influenced the response rate for this survey research. A majority of respondents perceived that they had a role in educating families generally, as well as in ensuring the completion of screening, making referrals, and providing advocacy and support for families. These attitudes might be capitalized on to educate midwives about follow up of screening results.
The majority of respondents reported the belief that newborn hearing screening does not cause parents undue anxiety. The accuracy of this belief has been supported by evidence in the literature.14, 15 Nevertheless, individual differences in parental responses exist; it is difficult to predict an individual family’s response to a failed screening result and/or after confirmation of permanent hearing loss.15 This suggests the need for midwives to be prepared to offer support for families of newborns in their care who do not pass screening.
Knowledge and Informational Needs
Midwives reported that most of what they know about newborn hearing screening was learned from on-the-job training. But, it is unclear if “on-the-job” training can provide sufficient and accurate information about critical topics such as genetic syndromes in deafness, causes of hearing loss in infants, or links between hearing loss and language delays.
Findings from this study support the need for educational programs and resources that are tailored to address knowledge and practice gaps that are reported by midwives. The vast majority of midwives reported specific gaps in their knowledge concerning appropriate management of infants with newly diagnosed hearing loss. Many respondents reported a lack of understanding of genetic issues in hearing loss. Given that at least 50% of infants who received a diagnosis of congenital hearing loss have a genetic cause,16, 17 it is essential that midwives understand the need to collaborate with geneticists in managing pregnancies where there is a family history of permanent hearing loss.17 After a complete genetic consultation, the midwife will be in a good position to discuss any concerns family members may have about their baby’s diagnosis and results of genetic testing. Continuing education in this area should sensitize midwives to cultural considerations, including the fact that some deaf parents may be opposed to genetic testing for their children or surgical interventions like cochlear implants.18
The survey results suggest that many midwives do not understand best practices related to the ages at which infants can receive various hearing health services. This finding supports the need for more emphasis in continuing education on appropriate referral ages for fitting of hearing aids and the unique specialization required for infant hearing evaluation (i.e., pediatric audiologists). Midwives also should be educated about the medical needs of children with hearing loss. For example, children with sensorineural hearing loss are two to three times more likely than children with normal hearing to experience visual acuity problems, underscoring the need for careful newborn follow up to promote optimal development.4 They should be informed about current candidacy criteria for cochlear implants (e.g., severe-profound bilateral deafness) and that infants commonly undergo implantation surgery around 12 months of age. Midwives, at a minimum, should know where to send families of deaf children for more information.4
It is interesting that midwives in the current study requested information resources other than didactic lectures on topics related to newborn hearing screening. Resources that were judged as most useful were action-oriented; that is, they could be used to support immediate practice applications (e.g., laminated protocol cards, patient education materials). These preferences are consistent with meta-analytic findings on the effectiveness of various formats for medical continuing education.19, 20 They also requested Web-based materials and online CME courses. The American Academy of Pediatrics (AAP) has developed online training modules for their members, which may serve as a model for midwifery organizations. The AAP also sponsors a Chapter Champions program, which designates 1 pediatrician in each state as a leader for disseminating information and resources on newborn hearing screening. A similar program could be successfully implemented through the ACNM. This program is consistent with the evidence on the effectiveness of local opinion leaders on clinical practices in the health care arenas.20 Midwives should also be informed about the numerous resources related to newborn hearing screening on the Internet.21 Continued efforts to create and disseminate these types of materials, especially those with interactive media, seem to be warranted.
A number of topics were identified by participants as priorities for education related to newborn hearing screening. These self-appraisal opinions, paired with an analysis of responses to knowledge questions, provide some priorities for continuing education, including: protocol steps for follow-up, patient education resources, information on early intervention, contacts for more information, and impact of varying degrees of hearing loss on infant language. These topics have direct application to working with families in the health care setting. Responses to this survey highlighted the need for information on practical issues like patient education, genetic disorders associated with hearing loss, specific protocols for interpreting abnormal results, steps for follow up and early intervention strategies to improve newborn hearing. These categories point to midwifery’s emphasis on being both primary preventive and health promotion care providers. The midwife’s designated role of family health educator may be the impetus for the expressed interest in detailed, concrete, and precise information to share in the antepartal and peripartal period, concerning newborn hearing screening and ongoing developmental surveillance. Midwives requested training resources (such as patient education brochures and websites) that were double-edged, capable of educating families and updating providers about screening, services, and best practices for hearing loss. A partial list of resources related to the identification and management of children with hearing loss can be found in Appendix A.
There are several limitations to our study. The overall return rate was low (9.9%), which may suggest some non-respondent bias and the possibility that a propensity of responses were from midwives with greater interest in newborn hearing screening. If this is the case, then some of the findings about gaps in knowledge and misunderstandings are even more alarming because we would expect midwives most engaged in newborn hearing screening to be better informed. Midwives also may have become aware of their own knowledge gaps in the process of completing the survey. This may have biased their responses to questions about needed topic areas and resources. Furthermore, there was no attempt to measure directly the impact of knowledge or attitudes on midwives’ effective care of families who have newborns with diagnosed hearing loss. A comparison of the demographics between ACNM membership survey11 and this NHS research was presented in Table 1. Although many characteristics of the two samples are comparable, the table shows the limitations of participant numbers and addresses the need for a more comprehensive sampling of midwives. Considering that 7.9% of all births, and 11.3% of vaginal births are attended by midwives, data from the most recent national birth statistics reflects a trend of increasing midwifery care in the United States.22 Future research to determine midwife participation in hearing health is needed to address these questions for a growing number of midwives.
CONCLUSIONS
Results of this survey suggest that midwives could play a key role in promoting newborn hearing screening and follow up practices. Logical roles include parent education, teaming with local and state newborn hearing screening programs, and making appropriate referrals. The following steps would help harness the potential and important contributions of midwives. First, provide responsive continuing education resources that address attitudinal barriers. These resources should address: (a) the importance of early identification in fostering neurological, auditory and language development, (b) the documented accuracy of newborn hearing screening methods and appropriate false positive rates, and (c) roles midwives can take in the screening process in all birth settings. Next, address knowledge gaps through provision of (a) action-oriented resources (algorithms/protocol cards, parent education materials), (b) Web-based materials, and (c) online continuing medical education and materials for peer education. Third, provide training resources that are capable of educating families and updating providers about screening, services, and best practices for hearing loss. Materials are needed to better support and educate families in preparing for hearing screens, interpreting results, and facing concerns about newly identified babies with hearing loss. And finally, provide resources and support for midwives to take a more active role as advocates for early intervention for infants by helping them to understand the critical connections between hearing and communication development and the universal need for assistive technologies to promote hearing.
Supplementary Material
ACKNOWLEDGMENTS
This project was supported in part by National Institute on Deafness and Other Communication Disorders grant DC006460-02 and the Maternal and Child Health Bureau cooperative agreement MCHB61 MC-00006.
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
In the interest of brevity, these professionals will be referred to as midwives in the remainder of the article.
Contributor Information
Martha Hoffman Goedert, FACNM is an Assistant Professor at Seattle University, College of Nursing, Seattle, Washington.
Mary Pat Moeller, Director of the Center for Childhood Deafness, Boys Town National Research Hospital, Omaha, Nebraska.
Karl R. White, founder of the National Center on Hearing Assessment and Management, and Professor of Psychology, Utah State University, Logan, Utah.
References
- 1.White KR, Forsman I, Eichwald J, Munoz K. The evolution of early hearing detection and intervention programs in the United States. Semin Perinatol. 2010;34(2):170–179. doi: 10.1053/j.semperi.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 2.Yoshinaga-Itano C. Levels of evidence: Universal newborn hearing screening (UNHS) and early hearing detection and intervention systems (EHDI) Journal of Communication Disorders. 2004;37:451–465. doi: 10.1016/j.jcomdis.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy C, McCann D, Campbell MJ, Kimm L, Thornton R. Universal newborn screening for permanent childhood hearing impairment: An 8-year follow-up of a controlled trial. Lancet. 2005;366:660–662. doi: 10.1016/S0140-6736(05)67138-3. [DOI] [PubMed] [Google Scholar]
- 4.Joint Committee on Infant Hearing. [Accessed April 29, 2010];Year 2007 Position Statement: Principles and guidelines for early hearing detection and intervention programs. 2007 Available at http://www.asha.org/docs/html/PS2007-00281.html.
- 5.Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. [Accessed April 29, 2010];Pediatrics. 2000 106(3):E43. doi: 10.1542/peds.106.3.e43. Available at http://pediatrics.aappublications.org/cgi/content/full/106/3/e43. [DOI] [PubMed]
- 6.National Institutes of Health (NIH) NIH Consensus Statement. Early identification of hearing impairment in infants and young children. 1993;11(1):1–24. [PubMed]
- 7.Biernath K, Holstrum WJ, Eichwald J. Hearing screens for newborns: The midwife’s role in early hearing detection and intervention. Journal of Midwifery and Women’s Health. 2009;54:18–26. doi: 10.1016/j.jmwh.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 8.National Center for Hearing Assessment and Management (NCHAM) and American Academy of Pediatrics (AAP) [Accessed April 29, 2010];Universal newborn hearing screening, diagnosis, and intervention-guidelines for pediatric medical home providers. Available at http://www.medicalhomeinfo.org/screening/Screen%20Materials/Algorithm.pdf.
- 9.Moeller MP, Eiten LE, White KR, Shisler L. Strategies for educating physicians about newborn hearing screening. Journal of Academy of Rehabilitative Audiology. 2006;39:452–465. [PMC free article] [PubMed] [Google Scholar]
- 10.Moeller MP, White KR, Shisler L. Primary care physicians’ knowledge, attitudes and practices related to newborn hearing screening. Pediatrics. 2006;118:1357–1370. doi: 10.1542/peds.2006-1008. [DOI] [PubMed] [Google Scholar]
- 11.Schuiling KD, Sipe TA. Fullerton, Findings from the analysis of the American College of Nurse-Midwives’ Membership Surveys: 2006–2008. Journal of Midwifery and Women’s Health. 2010;XXX:1–11. doi: 10.1016/j.jmwh.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Norton SJ, Gorga MP, Widen JE, Folsom RC, Sininger Y, Cone-Wesson B, Vohr BR, Fletcher KA. Identification of neonatal hearing impairment: A multicenter investigation. Ear and Hearing. 2000;21(5):348–356. doi: 10.1097/00003446-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Moeller MP, Tomblin JB, Yoshinaga-Itano C, Connor CM, Jerger S. Current state of knowledge: Language and literacy of children with hearing impairment. Ear and Hearing. 2007;28(6):740–753. doi: 10.1097/AUD.0b013e318157f07f. [DOI] [PubMed] [Google Scholar]
- 14.Vohr BR, Letourneau KS, McDermott C. Maternal worry about neonatal hearing screening. Journal of Perinatology. 2001;21:15–21. doi: 10.1038/sj.jp.7200475. [DOI] [PubMed] [Google Scholar]
- 15.Young A, Tattersall H. Parents’ of deaf children evaluative accounts of the process and practice of universal newborn hearing screening. Journal of Deaf Studies and Deaf Education. 2005;10:134–145. doi: 10.1093/deafed/eni014. [DOI] [PubMed] [Google Scholar]
- 16.Schimmenti LA, Martinez A, Fox M, Crandall B, Shapiro N, Telatar M, Sininger Y, Grody W, Palmer C. Genetic testing as part of the early hearing detection and intervention (EDHI) process. Genetics in Medicine. 2004;6(6):521–525. doi: 10.1097/01.gim.0000144187.21727.28. [DOI] [PubMed] [Google Scholar]
- 17.Palmer CGS, Martinez A, Fox M, Crandall B, Shapiro N, Telatar M, Sininger Y, Grody WW, Schimmenti LA. Genetic testing and the early hearing detection and intervention process. The Volta Review. 2003;103:371–390. [Google Scholar]
- 18.Martinez A, Linden J, Schimmenti L, Palmer C. Attitudes of the broader hearing, deaf, and hard-of-hearing community toward genetic testing for deafness. Genetics in Medicine. 2003;5:106–112. doi: 10.1097/01.GIM.0000055200.52906.75. [DOI] [PubMed] [Google Scholar]
- 19.Farmer A, Legare F, Turcot L, Grimshaw J, Harvey E, McGowan J, Wolf F. Printed educational materials: Effects on professional practice and health care outcomes. Cochrane Database Systems Review. 2008;6(3):CD004398. doi: 10.1002/14651858.CD004398.pub2. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien T, Freemantle N, Oxman AD, Wolf F, Davis DA, Herrin J. Continuing education meetings and workshops: Effect on professional practices and health care outcomes. Cochrane Database Systems Review. 2001;2:CD003030. doi: 10.1002/14651858.CD003030. [DOI] [PubMed] [Google Scholar]
- 21.National Center for Hearing Assessment and Management (NCHAM) [Accessed Apr 22, 2010];Links to website information regarding Early Hearing Detection and Intervention. Available at http://www.infanthearing.org/resources/links.html.
- 22.Hamilton BE, Martin JA, Ventura SJ. Births: Preliminary data for 2007. National Vital Statistics Report. 2009;57:16–17. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.