Abstract
The myths surrounding electroconvulsive therapy (ECT) and the misconceptions held by the general public, clinicians, and patients have interfered with acceptance of this treatment throughout its history. Misunderstandings surrounding ECT, and its consequent stigmatization, are reviewed, including negative depictions of ECT in film, print media, and on the Internet. Clinicians involved in the delivery of ECT benefit from gaining an understanding of how ECT may be perceived by patients and other mental health professionals; they can play a vital role in educating patients and helping ensure the delivery of a successful course of ECT. Guidance is provided for clinicians on how to support patients and families through the ECT process using a model team approach. Anxiety reduction, meeting individual needs, patient and family psychoeducation, assessment of psychosocial supports, and discharge planning are discussed.
Keywords: electroconvulsive therapy, stigma, depression, media, public perception, psychoeducation, assessing supports, discharge planning
The first article in this two-part series addressed common misconceptions about ECT by presenting a historical perspective and discussed indications for treatment, research initiatives, technical features, and treatment side effects. This second half of the series first traces how ECT came to be misunderstood and stigmatized by the media and the public. It then focuses on patients’ and the publics’ perceptions of ECT, and proposes a team approach to effectively educate and support patients and families through treatment.
Since convulsive therapy was introduced as a means of treating severe psychiatric illness in the United States during the 1930s, countless numbers of acutely ill patients have received various forms of “shock” therapy, with significant positive results. The stigmatization of ECT, which led to a repudiation of this potentially life-saving treatment, was a function of many factors, not the least of which involved the unmodified and perhaps overly extensive use of ECT in its early days. The use of ECT to treat severe psychiatric illnesses began to decline in the 1960s, most likely due to the following two factors: 1) the introduction of pharmacologic agents to treat depression, specifically the tricyclic antidepressants (TCAs) and the monoamine oxidase inhibitors (MAOIs),1 and 2) a growing negative public reaction to ECT due to cognitive (i.e., memory) side effects, physical discomfort, and the implications of social control associated with the treatment.
HOW ECT CAME TO BE MISUNDERSTOOD AND STIGMATIZED
Medication: The New Panacea
The antidepressant properties of imipramine, the first drug used to treat depression, were initially noted as a result of some serendipitous findings.1 The idea that a medication could be used to treat mood disorders was a difficult concept to grasp, given that ECT was the only successful treatment for these disorders at the time. Imipramine, an iminodibenzyl initially marketed unsuccessfully as an antihistamine and then as an antipsychotic, was noted to have mood elevating effects in a group of patients with schizophrenia in 1955. However, the concept of using medications to adjust mood imbalances caught on quickly, and the 1960s and early 1970s saw the rise of psychotropic medication through development and marketing as standard treatment for severe mental disorders.1 Many clinical trials assessing the efficacy of imipramine versus placebo were conducted from the 1950s through the early 1970s. A review was published in 19752 that analyzed the results of 30 such studies conducted between 1958 and 1973. The efficacy of imipramine compared with placebo in acute endogenous depression, using the nomenclature of the times, was firmly established. However, as concerns about side effects (e.g., parkinsonism associated with antipsychotics, cardiovascular effects of TCAs) and disappointing efficacy with medications increased during the 1970s,3 there was a resurgence of interest in ECT, although this did not occur without controversy.
Resurgence of ECT and Public Reaction
Although many studies done during the 1970s attested to the efficacy of ECT, misinformation, public protest, and legal restrictions tended to overshadow empirical evidence. Ironically, as scientific methodology improved and ECT was modified to become more humane and easier to tolerate, public concern and anti-ECT lobbying and legislation increased. ECT was an easy target, especially since its early application had unfortunately often violated the biomedical ethical principles of autonomy and beneficence.4 For example, it is true that ECT was sometimes applied without patients’ consent, and that it was widely—and sometimes inappropriately—used. Standards for informed consent, now firmly adhered to, were initially established in a 1978 report from an American Psychiatric Association (APA) Task Force.5 It is also true that unmodified ECT resulted in significant physical discomfort and at times injury (e.g., fractures) and could be an ordeal for both patients and staff,6,7 creating the image of a dangerous and frightening treatment with considerable risk for which patients were unprepared. However, such problems occurred before the widespread implementation of procedural modifications, including anesthesia, oxygenation, and muscle relaxants, which were first introduced in the 1950s. With regard to cognitive side effects, ECT was usually delivered bilaterally at this early juncture, using an inefficient sinusoidal waveform that produced an unfavorable side-effect profile. In addition, in the past, a course of ECT may have included a greater number of and more frequent treatments than currently used, exacerbating the side-effect profile (see Part I of this two-part series8 for a more detailed discussion of the side effects of ECT and how they can be minimized). A case in point is the use of “intensive” or “regressive” ECT in the United States and abroad.9 With these treatment schedules, ECT was delivered at least once daily in a misguided attempt to “reorganize” chronically ill patients entirely through the “arresting” of higher mental functions. This reorganization would supposedly herald a return to normal functioning. Intensive ECT was unfortunately used in public and private settings for a variety of diagnoses, most often in people with severe, treatment-resistant schizophrenia. Use of intensive ECT declined sharply in the early 1950s subsequent to public outcry and the introduction of pharmacologic approaches.9
When considering any aspect of ECT treatment, it is vital to keep in mind that the problems that arose during the early years of ECT use occurred when few other effective treatments were available to treat those suffering from major mental illnesses.8,9 Alternate available treatments such as psychosurgery and insulin coma had considerably more daunting side effects. In lieu of spontaneous remissions, the lives of patients with schizophrenia and major mood disorders were fraught with the torturous symptoms of their illnesses, confinement in long-term facilities, and complete hopelessness.9 Early forms of ECT, including the unmodified and regressive treatment techniques described, and their consequent unwanted effects, were utilized prior to decades of rigorous research aimed at altering the electrical stimulus to control side effects while maintaining efficacy. Despite the developments and changes that have taken place in the past three decades, images drawn from those early years of ECT persist in the public mind, as illustrated in the following case:
\Ms. H., a 54-year-old woman, was admitted to our hospital for a severe treatment-resistant depression in 2002. The patient had a college education, lived in our metropolitan area, and had been receiving mental health care since her early 20s. However, she and her husband were very frightened at the prospect of ECT and nearly refused. When asked what they knew about the treatment, her husband replied that his only exposure involved his own mother, who was treated with ECT for schizophrenia in the mid 1940s. She had been held down and put in four point restraints to receive the treatment. The couple had no specific information about his mother’s response but had heard reports that Mr. H.’s mother was “never the same” afterward. Ms. H. and her husband were given the opportunity to obtain more balanced information through a structured psychoeoducatiaonal program about ECT in order to assist them in making a decision about treatment options. This program included a review of patient information literature, meetings with other patients, and a tour of the facility. Following this program, Ms. H. agreed to receive ECT.
In sum, factors that contributed to the vilification of ECT and the decline in its use included the growing hegemony of other psychotherapeutic approaches, especially during the 1950s and 1960s, followed by the formation of lay anti-ECT groups, the ideology of the anti-psychiatry movement, and the growing influence of the pharmaceutical industry on postgraduate psychiatry training (for complete reviews, see Shorter and Healey9 and Ottosson and Fink10).
PERCEPTION OF ECT BY THE PUBLIC
Despite years of social, political, and legal attacks and lack of acceptance by the general public, approximately 100,000 people in the United States and over 1,000,000 worldwide receive ECT annually, although this is apparently not well known.10–12 For example, when the authors, and other clinicians who work with patients being treated with ECT, discuss this work with acquaintances or people in other professions, we routinely hear responses such as “Oh, do they still do that? I thought that was outlawed. That must be an awfully depressing job.” Andrews and Hasking hypothesized that the extreme nature of anti-ECT images in the media and the arts exerts an egregious effect on public perceptions.13 They suggested that it is the public’s lack of factual knowledge and exposure to the treatment that allows these images to hold sway and ultimately influence decisions regarding ECT treatment. Pettinati et al.14 pointed out the importance of reconciling the imbalance between the mostly positive perceptions of patients who have experienced ECT and the impassioned resistance by the lay public that continues to endanger the viability of ECT. Dowman et al.15 and Endler7 stated that a major goal for all clinicians who work with patients receiving ECT should be to educate the public and those they train about the treatment and to close the gap between reality and distortion. The dissemination of accurate information about ECT has been hindered by the lack of public information and positive media representations of the treatment as it is administered today. In contrast, in 2002, for example, the pharmaceutical industry spent approximately 30%–35% of its total revenue (approximately $21 billion) on education and promotion, with about 86% of this activity directed at physicians.16 Psychiatrists form a large part of the target audience for these materials, since medications that target the central nervous system account for over 22% of pharmaceutical sales and are quite profitable.16 Although an educational campaign concerning ECT aimed at both the medical community and the lay public might help to offset its negative image, such a campaign has never been undertaken.
Misinformation about ECT has been promulgated through four major avenues: 1) the media, including articles in the lay press and television news; 2) depictions in films; 3) coalitions lobbying for anti-ECT legislation, and 4) the Internet.
Media Depictions of ECT
Distortions of information concerning ECT have appeared in the lay press and in television news programs. Hirshbein and Sarvananda17 recently published a very comprehensive review of print-based accounts of ECT since 1940, and how they have been used by both opponents and proponents of psychiatry. Dukakis and Tye18 discussed the growing antipathy to ECT among this country’s intellectual classes, perhaps heralded by the effect of psychotically depressed and alcoholic writer Ernest Hemingway’s treatment with ECT and subsequent suicide. The impact of this event was exacerbated by publication of Ken Kesey’s One Flew Over the Cuckoo’s Nest in 1962, which was followed by news of novelist Sylvia Plath’s depression, ECT treatment, and suicide in 1963.19 In 1972, ECT catapulted into the headlines when it was announced that Senator Thomas Eagleton, democratic vice presidential candidate, had been successfully treated with ECT for a psychiatric disorder in the past. His name was withdrawn from the ticket regardless of the fact that he had successfully served as Senator from Missouri following his treatment.6,19 In 1974, government economist Marilyn Rice, employing a pseudonym, described the memory-related side effects she experienced following ECT to author Berton Roueche, which he depicted in his article “As Empty as Eve.” The author paid little attention to the reasons for Rice’s treatment and her eventual recovery, but rather focused on her pronounced memory loss (Roueche 1974, as cited in Ottosson and Fink10).
In 1990, a series of female ECT recipients appeared on an episode of Geraldo and spoke of their treatment by ECT psychiatrists in horrific terms. This group included several women, including the feminist writer Kate Millett, diagnosed and treated for bipolar disorder, as well as several members of the lay community who had received unusually large numbers of ECT treatments under what was portrayed as forced and inhuman conditions. It also included Linda Andre, a former writer who claimed that ECT completely destroyed her memory and writing ability. Ms. Andre may have experienced an uncommon degree of memory loss, as did Anne Donahue, as described in the first article in this series. The individuals who presented their scenarios on this episode of Geraldo were unusual in the scope and circumstances of their treatment. The counterpoint to their collective point of view was the disembodied voice of ECT expert Harold Sackeim on the phone, which did not do enough to underscore the point that, when ECT is delivered in a medically sound manner, this treatment, like other medical treatments, is generally safe and effective.
In 1995, reporter Dennis Cauchon wrote a series of short articles on ECT for USA Today.20 He stated that ECT use was financially motivated, particularly in treatment of the elderly, given that the likelihood of receiving ECT increased dramatically when patients became eligible for Medicare. This claim was contradicted by results of a study done by Sackeim et al.21 In a prospective review of the clinical consequences of ECT in 7 community facilities (N = 347), these researchers found that the average age of the patients was 56.7 years, with a standard deviation of 17.6 years, and that the age range of patients referred for ECT in this community sample was 39.1 to 74.3 years. Cauchon also claimed that the death rate from ECT, particularly in elderly recipients, was 1 in 200.20 This claim was contradicted by empirical data that show the death rate associated with ECT treatment to be approximately 2–10 in 100,000, which is equivalent to the rate seen with anesthesia alone.12,22 Members of the public, unaware of any problems with the accuracy of Cauchon’s reports, submitted comments that were supportive of the series. A rejoinder from the psychiatric community by William Reid relied on current clinical data from his state of Texas, the most restrictive regarding the application of and reporting concerning ECT, to counter these claims.23 Reid referred to ECT as a safe and lifesaving treatment and vehemently disagreed with Cauchon’s conclusions.
More recently, several public figures have disclosed their battles with depression and treatment with ECT. For example, Dick Cavett disclosed his long-standing bipolar disorder and treatment with ECT. His experience was quite positive and he referred to ECT as a “magic wand.”24 Kitty Dukakis wrote about her struggles with major depression and alcoholism, and her reliance on regular schedules of ECT to stave off reoccurrences of her depression.18 Dukakis did not deny that she experienced memory loss as a result of her treatment. In fact, she referred to the control that ECT provided her over her depressive episodes and the consequent memory loss as a quid pro quo, and for her, worth the costs.18 Other public figures who have disclosed their treatment and its positive consequences include the pianist Vladimir Horowitz and New York Philharmonic timpanist Roland Kohloff.25
Depictions of ECT in Film
In 2001, McDonald and Walter published an objective and very comprehensive review of the portrayal of ECT in American films.26 In this article, they discussed 20 films that refer to or depict ECT, starting with The Snake Pit in 1947 and ending with A Requiem for a Dream in 2001. The authors noted that ECT was depicted as a severe but helpful remedy for psychological distress in earlier films, but that the depiction of ECT changed over the last few decades to that of a brutal, harmful procedure with little or no therapeutic benefit. This review led McDonald and Walter to conclude that negative attitudes about ECT among patients, families, health professionals, and the general public stem in large part from film portrayals, particularly Milos Forman’s 1973 film version of One Flew Over the Cuckoo’s Nest.
In a study published in 2002, Walter et al. surveyed 94 medical students from the United Kingdom and Australia concerning their baseline knowledge of and attitudes towards ECT; they then examined how these variables were affected by watching five recent films that depicted the treatment.27 While students had little knowledge of and generally negative attitudes towards ECT at the outset of the study, viewing the scenes involving ECT decreased support for the treatment by a third, with the percentage of students saying that they would dissuade family members from seeking ECT rising from 10% to 25% after viewing the films.
Coalitions Lobbying for Anti-ECT Legislation
Lobbying against ECT began in earnest in the 1970s, initiated by ECT “survivors” (people who had undergone unmodified ECT or who had suffered severe cognitive impairment after receiving ECT). The lobbying resulted in legislative and judicial efforts to regulate ECT that were purportedly aimed at protecting patients’ rights. The effectiveness of anti-ECT lobbying is illustrated by the passage of various restrictions on the use of ECT, many of which are still in place. For example, in 1974, Governor Reagan signed a highly restrictive Assembly bill (AB 4481) regulating use of ECT in California. It was later challenged by the Association for Convulsive Therapy (ACT) and replaced by the less restrictive AB 1032.28,29 These modifications remained in effect until 19879; however, ECT use continued to decline in California.29 In 1982, what was referred to as the Berkeley Ban was instituted, in which citizens of Berkeley approved a bill by referendum that made administration of ECT in city hospitals a crime punishable by a $500 fine. This was subsequently reversed on a technicality. In 1993, the Texas legislature banned the use of ECT for patients under 16 and instituted strict reporting requirements for all practitioners, creating a disincentive to prescribe ECT. As Winslade et al.30 pointed out, excessive regulation, as was imposed on ECT treatment, may infringe on medical practice in the form of time, cost, and psychological burden. They hypothesized that due to restrictions, doctors may not have recommended ECT in some cases when it would have been of significant value. In addition, their review of practices in the 15 most populous states two decades ago revealed vast differences in factors such as diagnoses, reporting requirements, clinical circumstances, and qualifications of physicians.
Support for the anti-ECT movement has also come from the medical and sociological communities. The psychiatrists Thomas Szasz and Peter Breggin and the sociologist Erving Goffman in the United States, as well as Ronald Laing and Michel Foucault in Europe25 published anti-psychiatry treatises in the early 1960s, a period which heralded a biological approach to the assessment and treatment of mental illnesses. Szasz, considered that definitions of mental illness were socially constructed and educed to describe deviations from the psychosocial or ethical norms of a particular society, and were not true illnesses in the medical sense.31 For Szasz, a mental illness was not a true disease if there was no means of assessing it as a corporeal disease process, as in a physical illness. He thus deemed the concept of mental illness to be “logically absurd” and said that it was begging the question to expect that medical action would be an appropriate remedial approach.31 Szasz’s student, the psychiatrist Peter Breggin, while credentialed and extensively published, paradoxically became an avid and controversial anti-psychiatry voice during the 1970s. His basic discourse focused on what he considered to be the negative iatrogenic effects of conventional psychiatry, particularly medication and somatic treatments such as ECT.32 Although his views were widely disputed and his nonscientific methodology questioned, he remained an active voice within the anti-psychiatry movement. Finally, the sociologist Erving Goffman also questioned the very roots of conceptualizations of mental illnesses and their treatment. His theoretical treatise on symbolic interaction posited that individuals must form contracts and strategies to adapt to inherently oppressive societies to survive successfully in those societies.33 His view of mental institutions was based on the belief that patients’ ways of behaving in institutions represented adaptations that were a function of what the institution imposed on those patients, rather than a function of an inherent disease.33 Although these and similar contributions to the ongoing debate about psychiatric coercion were not founded in empirical evidence, these theorists were influential at the time and continue to maintain some following.
Faced with lobbying, protesting patients, and the absence of consensus among the psychiatric community, legislators could easily find justification for regulation. The APA’s Task Force 145 was set up in 1975 as a counterweight to the anti-ECT backlash, with its goal being to review the practice of ECT in the United States and make recommendations. This Task Force helped set standards for obtaining consent, for qualifications of psychiatrists, and for other issues. A consensus conference sponsored by NIMH in 1985 clarified new practice recommendations for ECT and also made recommendations regarding education, training, and privileging of ECT providers.34 In 1990, another APA Task Force, which was given the mandate of establishing recommendations, published the first edition of The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging.35 (For a comprehensive review of these developments, see the second edition of this publication which appeared in 200112).
Information on the Internet
The influence of the Internet, which contains both positive and negative portrayals of ECT, has increased very rapidly. Websites developed by mental health organizations, as well as more objective personal accounts, counter some of the many dramatic, frightening, and mendacious images that appear on websites posted by the anti-ECT coalitions (Table 1). Thus, a patient looking for information on ECT is likely to encounter both positive and negative images, as illustrated in the following case:
Mr. I was admitted for ECT. He was experiencing a fairly severe, medication-resistant depression and also had a host of psychosocial problems. Although he was ambivalent, he had consented to be treated with ECT. However, once on the inpatient unit, research on the Internet led him to believe that ECT was damaging and frightening. Despite the efforts of staff, he refused treatment and was discharged on medication with little change in his condition.
Table 1.
Sources of positive and negative information on ECT on the Internet
| Positive information | |
| American Psychiatric Association | www.psych.org |
| National Alliance for Mental Illness and its local chapters |
www.nami.org www.medhelp.org/lib/ect.htm |
| National Mental Health Association | www.nmha.org |
| Personal account by patient | www.electroboy.com/electroshocktherapy.htm |
| Negative information | |
| Coalition Against Psychiatric Assault | capacanada.wordpress.com |
| Coalition for the Abolition of Electroshock in Texas | www.endofshock.com |
| Committee for Truth in Psychiatry |
http://www.ect.org/ctip_about.shtml Also provides links to other websites including the following: www.healthyplace.com/communities/depression/ect/ctip_about.asp www.harborside.com/~equinox/ect.htm www.ect.org |
| Citizens’ Commission on Human Rights | www.cchr.org |
| Site created by a lawyer | www.antipsychiatry.org/ect.htm |
| Site created by a neurologis | www.idiom.com/~drjohn/ect.html |
| Wittenberg Center to End Electroshoc | Wittenbergces.blogspot.com/2007/07/anti-ect-websites.html |
PATIENT PERCEPTIONS OF ECT
By the 1970s, the beneficial effects of ECT had been established and modifications in the techniques used to deliver treatment were in place. However, rather than gaining greater acceptance among the lay public, it was apparent to ECT practitioners that many patients and families continued to view the recommendation for and prospect of ECT with horror, and that this phenomenon warranted research. Thus, various researchers utilized descriptive surveys, both retrospective and prospective, to investigate patients’ subjective views of ECT. In the first such study, published in 1975, a psychiatric nurse interviewed 96 patients 24 hours after each ECT treatment they received, for a total of 500 consecutive treatments.36 The aspects of ECT that patients disliked involved their experience of fear, especially of permanent memory loss and general intellectual impairment. However, none of the patients found the treatment worse than anticipated, and 80% found it better. Patients reported a low incidence of side effects, with muscle pain the most frequently reported side effect, although only by 8% of patients; about 3% reported memory impairment or headache.
Several retrospective studies were conducted during the 1980s; the results of these studies highlighted the positive effects of exposure to ECT on patients’ perceptions of the treatment. Freeman and Kendell interviewed 166 patients who had received ECT, 106 of whom were treated 1 year earlier and 60 of whom were treated 6 years earlier (the sample was combined since no significant differences were found between the groups).37 Of these 166 patients, few rated specific aspects of the treatment, such as premedication (15.7%), waiting for treatment (19.9%), the staff (3.0%), anesthetic injections (6.6%), waking up (20.5%), and immediate recovery (17.5%) as unpleasant. About 50% stated it was no more unpleasant than a trip to the dentist; 79% found it a helpful and useful procedure; and 65.6% felt that it relieved their depression faster than medication. Only 34.4% stated they would not have it again. However, 63.9% reported a subjective sense of memory loss. Using a similar questionnaire, Hughes et al. interviewed 72 patients who had received ECT: 83% said they had improved; 81% stated they would have ECT again if needed; and 50% reported memory loss.38 Benbow assessed patients’ attitudes following a completed course of ECT and found that the majority had not found it especially frightening and would agree to have the treatment again.39
In a study published in 1994, Pettinati et al. compared two groups to investigate the effects of exposure to ECT vs. no exposure, on depressed patients’ perceptions of the treatment.14 They surveyed a sample of 56 depressed patients before and after ECT treatment and compared their responses with those of 22 depressed patients who had never received ECT. Almost all (98%) of the treated group stated they would be willing to have ECT again if needed, while 70% of those who had not received ECT expressed willingness to consider ECT treatment in the future. Of the patients who had received ECT, 62% percent rated the experience as less upsetting than a tooth extraction, while 14% of the untreated group thought ECT would be less upsetting. However, it is worth noting that, when interviewed after treatment, regardless of the time interval, many patients in the studies described above—about 60% among Freeman and Kendell’s respondents, 50% in the sample from Hughes et al., and 64% in the Benbow study—stated that they had inadequate or no knowledge about what the treatment involved, why it was given, or how it worked. Although the cognitive effects associated with ECT may have precluded retention of information in some cases, perception can overrule reality. Thus, clinicians should strive to make patient education a consistent priority. The trust and reduction in anxiety achieved by providing and reinforcing information can have a significant impact on patient perceptions and willingness to complete treatment.
PERCEPTIONS OF ECT AMONG MENTAL HEALTH PROFESSIONALS
The differences in patients’ views related to actual exposure to ECT are paralleled by findings in studies of healthcare workers. This is particularly salient, as the knowledge and attitudes of mental health professionals are pivotal in reducing fear and promoting understanding of ECT among patients and families. This phenomenon has been researched extensively using descriptive survey methodologies (see Dowman et al. 200515 for a recent meta-analysis and Janicak et al. 198540 for a review of earlier surveys). For example, in attempting to elucidate attitudes toward ECT within the psychiatric community, APA Task Force 14 on ECT surveyed 4,000 psychiatrists regarding their views of ECT.5 Of those surveyed, 72% stated that ECT was appropriate for certain diagnoses and was safe, less expensive, and more effective than other treatments. Only 7% felt it was an obsolete treatment. In 1981, Pippard and Ellam41 reported the results of a survey of 3,221 psychiatrists in the United Kingdom, 87% of whom felt that ECT was an effective treatment, but only for specific psychiatric diagnoses. In their 1985 publication mentioned above, Janicak et al. investigated differences among subcategories of mental health workers in their knowledge of and attitudes towards ECT.40 They distributed an ECT Knowledge and Attitude scale to 200 mental health workers, including psychiatrists, nurses, social workers, and psychologists, and found that psychiatrists and nurses had the highest knowledge scores, while social workers had the lowest. Attitudes towards and willingness to receive ECT were positively associated with the individual’s knowledge base. In addition, this study revealed that years of professional experience affected the willingness of physicians, nurses, and social workers but not psychologists (the only group of professionals whose knowledge base did not grow with increased clinical experience) to recommend ECT as a treatment for their patients. The authors hypothesized that psychologists had the least amount of actual exposure to the treatment.
In a related study published in 1981, Kalayam and Steinhart distributed a 7-item Likert-style questionnaire on attitudes and emotional responses to ECT to 1,043 individuals, 587 of whom completed it.42 The respondents represented a broad range of groups, including 76 psychiatrists or residents, 85 nurses, 67 clinical psychologists, 72 psychiatric social workers, 63 patients who had received ECT, and 224 members of the general public. Although there was a general positive trend in the responses, there were significant differences among the groups. In response to the statement, “ECT is appropriate for certain psychiatric conditions,” psychiatrists agreed most strongly, while psychologists and the general public disagreed most strongly. Patients who had received ECT showed the least fear about the treatment, followed by psychiatrists, while social workers and psychologists were the most fearful. Psychologists, interestingly, were more fearful than the general public.
It is intriguing that a study done 20 years later had similar results. In a study published in 2001, Lutchman et al.43 distributed a “Questionnaire on Attitudes and Knowledge of ECT” (QuAKE) to 268 professionals in the United Kingdom, 74% of whom responded. Generally, these researchers found broad differences among the professions in their knowledge of and attitudes towards ECT. For example, while psychiatrists and nurses stated that ECT was more likely to be beneficial than harmful (83% and 69%, respectively), only 32% of social workers and 14% of psychologists agreed with this statement.
The differences in patients’ views associated with actual exposure to ECT noted by Pettinati et al.14 (see previous section) are paralleled by findings in studies of healthcare workers. In a study published in 1992, Szuba et al. surveyed 33 medical students and 18 first-year psychiatry residents about their attitudes towards, knowledge of, and opinions about ECT before and after inpatient rotations that involved exposure to ECT.44 They found that all those surveyed demonstrated significantly greater knowledge and positive attitudes towards ECT following their rotations and that, after exposure, they stated they would undergo ECT if recommended. Thus, exposure to ECT has been found to foster more positive attitudes towards the treatment in both patients and clinicians (strategies for patient education are discussed in more detail later in the article).
ROLE OF MENTAL HEALTH PROFESSIONALS IN SUCCESSFUL ECT
An important issue, highlighted by Lutchman et al.,43 involves the attitudes, beliefs, and perceptions of members of the mental health community, and most saliently, the ECT team. A recommendation for ECT exposes potential patients as well as their family members and support systems to a plethora of negative images. Because this treatment is still shrouded in myth and misconceptions, a recommendation for ECT can generate a higher level of anxiety in patients and families than any other psychiatric treatment.45 It is the responsibility of all clinicians involved in the patient’s treatment to convey comprehensive, accurate, and supportive information to assist patients and family members in making an informed choice about receiving ECT. Once the decision has been made, clinicians need to help patients and families obtain access to treatment, and provide support to help them remain in treatment.
Patients are usually referred for ECT by psychiatrists or primary care physicians, who have the initial opportunity to address the negative image of ECT and dispel myths by providing the most accurate information possible.46 The treating psychiatrist will often have developed a relationship with and earned the trust of the patient and his or her family. The importance of this type of support is illustrated in the following case.
Ms. J., a 56-year-old patient with bipolar disorder and features of borderline personality disorder, had developed severe, melancholic, agitated depression. Her psychiatrist was closely connected to our hospital and knew the indications for ECT quite well. He had supported the patient and her family through numerous exacerbations of her illness, and they generally accepted his treatment recommendations without question. Rather than alter her medications for this severe episode, Ms. J.’s psychiatrist referred her for ECT. She received 10 treatments, following which she experienced a full remission, with her Hamilton Depression Rating Scale (Ham-D)47 score dropping from 27 before ECT to 4 at 2 weeks post treatment. Ms. J. returned to her family and weekly treatment with her psychiatrist and remained well 1 year later
On the other hand, when a patient’s treating psychiatrist or therapist harbors and communicates negative attitudes about ECT, in the form of disparaging statements or a refusal to recommend ECT, this can pose serious challenges, as illustrated in the following case.
Mr. K., a 30-year-old man with an 18-year history of depression, had been receiving weekly treatment involving medication management and psychotherapy with the same psychiatrist. However, ECT had never been recommended. The patient’s mother had done her own research and pursued ECT treatment for her son. Despite lack of support from the psychiatrist. Mr. K. came to our hospital, and received treatment. After 8 treatments, his Ham-D scores dropped from 21 to 6, 1 week after completing the course of ECT. He was discharged to his home state and a new psychiatrist. When Mr. K.’s original psychiatrist was questioned as to why he never recommended ECT, his response was “My only exposure to ECT was as a resident 30 years ago, and it was not a positive one.”
Perhaps the greatest opportunity to provide accurate, objective information about ECT exists within the ECT team itself. The studies by Freeman and Kendell,37 Hughes et al.,38 and Benbow39 discussed above highlighted a common problem—the majority of patients in those studies were found to lack information about the treatment and its side effects. Although severe anxiety often interferes with patients’ ability to learn before many medical procedures,48–50 the short-term cognitive effects associated with ECT may preclude retention of the information patients have received about the treatment. Thus, those working with patients who are receiving ECT need to provide consistent information and support to help mitigate concerns that frequently arise when a recommendation for ECT is made. The following section presents some specific approaches for doing so.
SUPPORTING PATIENTS AND FAMILIES DURING THE ECT PROCESS
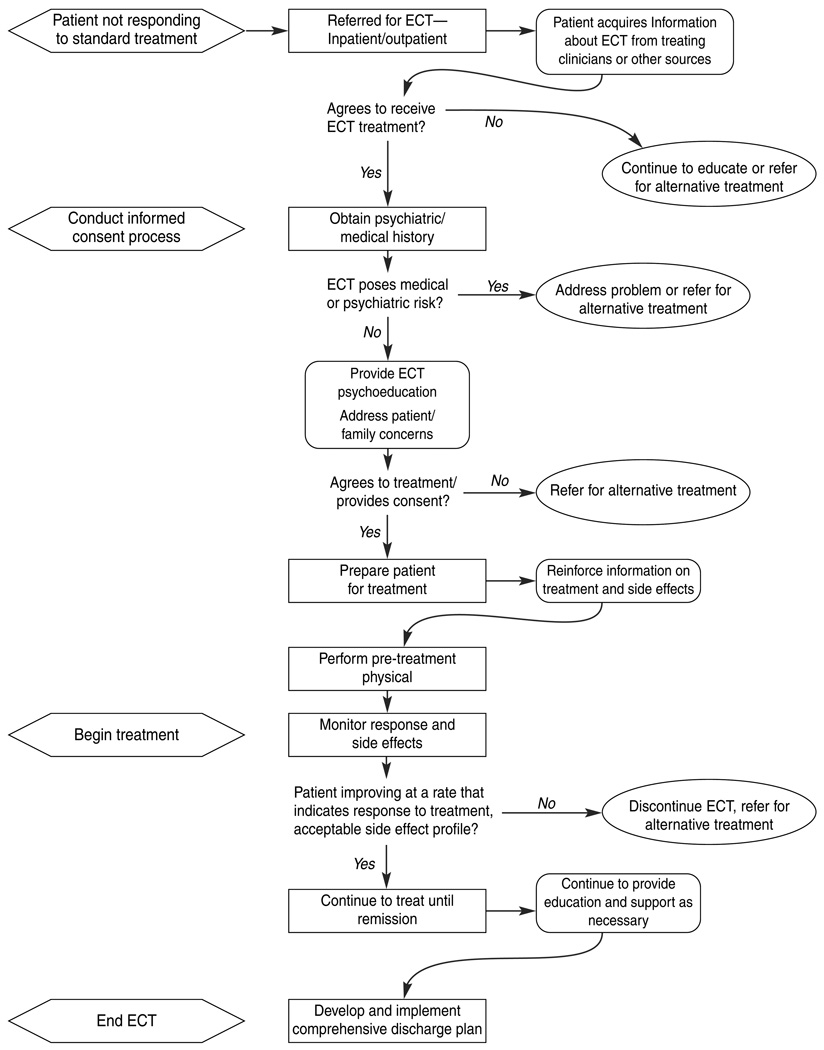
Although the number of facilities that provide outpatient ECT is growing,25 most ECT is still carried out in inpatient settings. While reliance on the referring psychiatrist is greater when ECT is provided in outpatient settings, it is still the ECT psychiatrist and other members of the ECT team who have the greatest opportunity, and indeed responsibility, to work with patients and families. As Wilkinson and Daoud reminded us in an article published in 1998,51 “Trust me, I’m a doctor” is not enough in this case. Figure 1 highlights the salient phases in the referral process from the time the recommendation for ECT is first made, and includes clinical decision points as well as opportunities to provide patient education and support.
Figure 1.
The ECT process: Phases, clinical decisions, and patient education
Patients receiving ECT present two unique challenges for clinicians to ensure a successful course of treatment and continued wellness beyond ECT. First, there is a vital need for patient and family psychoeducation, which involves providing factual information as well as the supportive clinical interventions that are critical in the treatment of severe mental illness.52 A patient’s decision to seek or continue a course of ECT may be influenced by the manner in which the staff communicates information. Patients and families receive comprehensive information about ECT from the ECT psychiatrist during the informed consent process, which will be discussed. The quality of this interaction is vital, as consent for ECT is a process which continues throughout the course of treatment.12 However, Lutchman et al. demonstrated that psychiatrists and psychiatric nurses, in general, may be in the minority in regarding ECT as safe, effective, and not necessarily a treatment of last resort, perhaps because they have had more professional exposure to the treatment.43 Hence, they cautioned clinicians that salient inconsistencies in perspective can exist among members of a multidisciplinary team. Although psychiatrists leading such teams may be unaware of these often subtle, even nonverbal, differences, they can create confusion in patients or even lead them to refuse treatment. Lutchman et al.43 and Dillon45 stressed the importance of striving to ensure that all members of a treatment team present a consistent message. It is therefore vital that psychiatrists who are leading an ECT team periodically review their own knowledge, beliefs, and images, those of their team members, and what is being conveyed to patients. When ECT recipients are treated on an inpatient basis, the clinical staff on inpatient units can also be a source of support or of concern. It is more difficult for ECT team members to assess clinical staff’s attitudes and communications to patients about ECT. However, we have found that regular conferencing and updates on the treatment can serve to promote accuracy and objectivity.
The second challenge involves a comprehensive assessment of the patient’s psychosocial supports and stressors. A clear assessment of psychosocial factors that might cause a patient to refuse or discontinue treatment or not to adhere to recommended follow-up is vitally important and should begin as soon as the patient agrees to treatment. This sort of assessment, although difficult, can help identify patients who are at high risk for refusal or non-completion of treatment.
Psychoeducation
The challenges involved in providing psychoeducation and assessing psychosocial supports begin the moment an ECT patient is recommended for treatment and continue to be relevant until treatment is completed. The benefits of providing education to patients and families prior to any medical procedure have been well documented.48–50,52 Such education is a prerequisite for making an informed decision and signing consent for all medical procedures. Once a patient is referred for and agrees to pursue ECT, psychoeducation is initiated during the consent process and should continue throughout treatment.
Although a complete discussion of the consent process for ECT is beyond the scope of this article (see the 2001 APA Recommendations12 for a full review), a brief review of some key points is warranted. The three basic requirements of informed consent for ECT proposed by the 1978 APA Task Force5 are still in place: “1. Provision of adequate information 2. A patient capable of understanding and acting reasonably on such information, 3. The opportunity to consent in the absence of coercion” (p. 97). Provision of information should include the risks and benefits of, and alternatives to ECT, how ECT is delivered, possible side effects, and probable outcomes. The physician must be able to assess the patient’s ability to understand and act reasonably. Thus, the quality of the interaction between the ECT psychiatrist and the consenter is an important aspect of the informed consent process. The consent process provides a unique opportunity for the psychiatrist (as well as other members of the treatment team) to connect with patients and families and help them understand and accept the treatment. As Abrams noted, this may be the first real explanation of the treatment that patients and families receive.28
Before providing specific information about ECT, it is important for the ECT psychiatrist and other members of the treatment team to obtain information from the patient and family members. First, clinicians should obtain a comprehensive history; they need to become familiar with the patient’s psychiatric and medical history, baseline functioning in life roles, and current condition. Second, it is also helpful to inquire about the impact the illness has had on the patient’s life and the patient’s perception of his or her relationships with outpatient clinicians. Third, it is important to consider factors related to the mindset, knowledge, and perceptions of the patient, as well as of family members if they are involved. Factors such as patients’ previous experiences, how they have obtained information, their ability to learn new material, and how they experience their depression have a factual (objective) component as well as a more subjective component that may be more difficult for clinicians to assess. Clinicians need to recognize that patients’ verbal reports may provide only a superficial idea of their concerns, fears and often painful subjective experiences, as outlined in Table 2. Therefore it is often necessary to probe further to help patients express their true feelings, to ensure that questions are answered, and to develop trust. This process helps clinicians be prepared for issues that may arise once patients consent to and prepare for treatment. In addition, as we learned in our discussions with participants in our CME course on electroconvulsive therapy, how clinicians assess and work with these fears and concerns can vary greatly as a function of several factors. These include the patient’s status (e.g., whether the patient is voluntary or involuntary and whether he or she is experiencing psychotic symptoms), the referral scenario (e.g., whether the patient has been referred specifically for ECT from an outpatient psychiatrist or is already an inpatient and is now being referred after other treatments have failed), and the setting (e.g., private or academic setting versus a state or Veterans Affairs facility).
Table 2.
Concerns of the ECT patient
| Objective (general areas of concern) | Subjective (unspoken concerns and fears) |
|---|---|
| Diagnosis of severe mood disorder | Double stigma of having mental illness and ECT |
| Clinical picture/illness course | Long history of illness and related losses |
| Prior response to standard treatment | Poor prior response (may contribute to hopelessness) |
| Prior experiences with ECT | Prior experience may not have been positive |
| Pending hospitalization | Fear of other patients and loss of freedom and personal space |
| Family interaction | Communication failures, family stress, role changes |
| Family support | Family members/partners may not be supportive of ECT |
| Financial status | Loss of position and status, financial difficulties |
| Concerns about effectiveness | ECT is a miracle cure/last resort (failure to respond may lead to increased hopelessness/increased potential for suicide) |
| Concerns about safety | ECT will damage my brain |
| Concerns about side effects | ECT will cause permanent memory loss |
| Conversations with others/exposure to media: film, popular press, Internet | May have received inaccurate, frightening information |
| Conversations with own practitioners | Practitioner may be ambivalent |
| Language barrier/comprehension difficulties | May cause embarrassment/unwillingness to query |
The information obtained by asking these comprehensive questions can help the treatment team determine strong and weak systems in a patient’s life, as well as demonstrating concern for individual needs.
A Model for Engaging Patients and Families in Treatment
Dillon45developed an intervention that involved engaging and providing psychoeducation to ECT patients and their families to help create a trusting relationship, reduce anxiety, and provide specific information. In this five-step intervention, various members of the ECT team participate at different points and collaborate with clinical staff. The stages of this process are outlined in the following sections.
1. Assessment and development of a therapeutic relationship
Engaging with patients and families early in the treatment process is a fundamental element in developing rapport and a continuing successful relationship. While there may be unfortunate cases in which a patient’s unwillingness or severe objections by family members preclude such engagement or actually prevent treatment (see Ottosson and Fink10 for examples of such cases), a model for engagement can be helpful when it can be applied. One means of engaging at this stage involves asking relevant questions that can help clinicians identify ways to assist patients through their treatment, as well as identifying “red flags” in their treatment history. During the informed consent process, as mentioned, the ECT psychiatrist obtains a comprehensive history from patient and family members and become familiar with the course of the patient’s illness, baseline functioning, and current condition. However, prior to patients beginning ECT treatment, it is also helpful for ECT clinicians to continue to inquire about the impact the illness has had on the patient’s life and his or her relationship with outpatient clinicians. The information obtained by asking these comprehensive questions can demonstrate concern for individual needs, help the treatment team determine strong and weak systems in a patient’s life, and identify general perceptions patients may have about psychiatry that could facilitate or impede treatment.
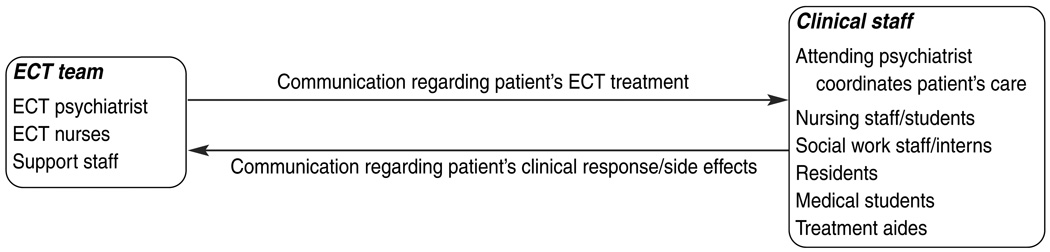
Another means of connecting with patients early in the treatment process is by communicating information about the treatment team. Patients often remark that they experience considerable confusion regarding the roles and distinctions among the clinicians responsible for different aspects of their care; thus it is helpful to explain the roles of the different members of the treatment team. While it may be the case that the ECT treatment team and clinical team on an inpatient unit are one in the same, in some settings, they may not be. In such cases, while the ECT team consists of the ECT psychiatrist and psychiatric nurses, unit staff members also play vital clinical roles in treating and caring for the ECT patient. In addition, in teaching hospitals, students in each discipline are also involved. Figure 2 illustrates these important interrelationships, the potential for confusion, and underscores the importance of all involved clinicians communicating with one another about the status of the ECT patient.
Figure 2.
Communication model: Caring for the ECT patient
2. Exploring fears and concerns
It is important to avoid making assumptions about patients’ fears and anxieties, since patients have different concerns. While acknowledging the universality of anxiety related to ECT, it is important to focus on what the patient may be communicating, verbally and nonverbally, legitimize the patient’s feelings, and try to address any specific concerns or fears the patient or family may have.
3. Identifying teaching tools
As discussed above, the consent process gives the treating psychiatrist and team an opportunity to disseminate information, answer questions, and reduce anxiety. It can be helpful to provide the patient and family with educational brochures and perhaps videotapes or DVDs. These materials should be easy to understand and targeted for lay audiences. There is no definitive evidence that one educational format is more effective than another, so that it is important to ask patients what learning mode they prefer. Andrews and Hasking,13 Baxter et al.,53 and Jenaway54 assessed effects of written material and media (e.g., educational DVDs, downloaded news programs) on patients’ levels of knowledge and anxiety. While these researchers were not able to conclude that patients preferred or benefited more from one method over another, they did find that written material and the consent process itself added to knowledge and reduced anxiety to a greater extent than videos, which tended to create more questions than they answered. Although our group prefers written material, particularly since few patients request a visual learning aid, it is important to keep in mind that patients may not retain information they receive. This may occur initially due to anxiety and symptoms of depression, and later because of the cognitive effects of ECT itself. Thus, the treatment team needs to provide consistent reinforcement, no matter what teaching methods are used. It can also be helpful for patients to speak with other patients who have had positive experiences with ECT. Finally, a physical tour of the ECT suite before treatment can help reduce anxiety for some patients.
4. Anxiety reduction coping strategies
It is helpful to ask patients what strategies have helped them cope with other stressful situations, particularly medical situations, and encourage them to use these strategies to help deal with their anxiety about receiving ECT. While anxiety about ECT often decreases with exposure as patients begin to understand what to expect, it can also increase at times, with certain patients developing “learned” anxiety as treatment progresses.55 Although the cause of this relatively uncommon phenomenon is not understood, clinicians should be alert for it, especially in patients who have received numerous treatments. It is generally helpful to teach patients some basic relaxation exercises and reinforce their use during the course of treatment. As patients become more familiar with unit staff, they may also identify a specific person with whom they feel most comfortable when they are anxious.
5. Evaluation
It is important to document in the patient’s chart that information was provided as well as any actual or potential problems the person may have with learning and retention. Because patients often forget they were told about a specific aspect of their treatment, it is essential to continue reinforcing the teaching, particularly during the course of ECT. As discussed in Part I of this two-part series,8 a range of different types of memory deficits with different causes can occur during ECT. Two methods we have found particularly helpful in ensuring that patients have access to important information as treatment progresses are journal writing and the creation of a Pre-Treatment Information Log.
Some patients (e.g., Mr. D. described in Part I of this series) may need a good deal of support to use journal writing successfully. It can be helpful to provide patients with a journal or pad, stress the importance of keeping track of what is happening with their treatment, and even assist them in making entries. We have found that patients find this process empowering during treatment, even if they initially resist keeping a journal. Patients often express a wish to keep track of information such as:
Discussions with staff members
Treatment decisions
Who visited or called
Important public events
Important personal events
Staff can also suggest that patients keep a subjective record of their mood in order to help track improvements.
An ECT Pre-Treatment Information Log is a structured method that allows patients to organize and have ready access to important information, including personal and work details, contact information, important telephone numbers and passwords, personal services, outside medical and psychiatric care, and important dates and events within their close social circle. The case of Ms. F, described in Part I of this series, who lost the password for her grant application, illustrates the need for such an instrument. Our staff offers to maintain this information in a secure place due to its potentially sensitive nature. This process is especially helpful and important when family members are not available to assist with keeping this type of information during and following treatment.
Assessing Psychosocial Supports
The second key component in working with ECT patients involves assessing their psychosocial environment. The patient’s family, friends, work, community, financial status, education, and access to mental health and medical services all affect and are affected by the person’s ability to get well. These effects occur at a number of different levels.56 The first level involves those closest to the patient—i.e., in whatever way the patient defines “family” (e.g., one patient brought his building superintendent to a family psychoeducation meeting at our hospital). Level 2 includes individuals in the patient’s close psychosocial circle and activities that may contribute to wellness. Level 3 involves the support systems and services the patient uses in his or her daily life and to stay well. Level 4 includes larger policy-related issues (e.g., mental health or housing policies, changes in Medicaid rules) that could affect the patient’s wellness. A thorough analysis of the patient’s psychosocial scenario can help the treatment team understand and plan for factors that can affect patients at each level. Table 3 provides examples of these factors; however it is vital to acknowledge that patients should have a major influence over what recovery means to them57 and how these factors are defined, and that each situation is different: Thus, no specific example can be comprehensive.
Table 3.
Factors to evaluate in the patient’s psychosocial environment
| Level 1. Immediate circle | Level 2. Affiliations | Level 3. Support systems |
Level 4. Policies and programs |
|---|---|---|---|
| Patient Partner/spouse Parents Adult children Other close relatives |
Extended family Close friends Therapist Psychiatrist Physician Neighbors Religious affiliation Work and work affiliations Opportunity for social/leisure activity Fitness/wellness Educational pursuits Volunteer activity |
Housing Transportation Basic needs (food, clothing) Neighborhood environment/safety Child care Health insurance Financial status Access to mental and physical health treatment |
Mental health policies/programs Stigma Social security legislation (Disability, SSI) Housing policies/programs Public assistance/Medicaid Judicial system |
Based on formulation in Hepworth et al., 1997, pp 20658
The level of family support, while often difficult to assess, can be one of the most influential positive or negative factors for a patient. Families are systems and readers are referred to a 2006 publication by Hepworth et al.56 for a discussion of multiple approaches to family system theory. Social work staff, in particular, will find an understanding family dynamics valuable in helping patients accept and remain in treatment and in identifying some of the factors that may interfere with continued wellness. It is important to keep in mind that anything that affects one member of a family system affects all the other members. For example, the rather sudden wellness of a family member who has been ill for some time can have a significant effect on family relations and communications,59 as illustrated in the following case:
Mr. L, a 28-year-old homosexual Hispanic man, lived with his family not far from our hospital. He had a history of major depression for the past 5 years, during which time he had become increasingly debilitated and unable to work. He spent time at home with his mother, who was also quite depressed. Mr. L came in for a screening and was deemed appropriate for ECT. He informed us several days later than he had decided not to pursue treatment at that time due to lack of support from his family, and that he needed time to work with them. We asked the patient to suggest that his family might come in and speak with us through a translator. The patient assured us that this was not necessary. Two weeks later, Mr. L expressed confidence in his family’s support and entered the hospital for ECT. After four treatments, Mr. L started to respond and his Ham-D score dropped from 35 to 19. He then stated that he wished to stop ECT and be discharged because he “could not stand the hospital experience” and missed his parents and brother who refused to visit him. We insisted that the patient’s family come in and obtained a translator for a family meeting. Mr. L’s mother and father appeared to be estranged; his father would not speak directly to Mr.L., which appeared to be a long-standing pattern due to the patient’s homosexuality. During the meeting, Mr. L.’s mother responded to our educational efforts and the evidence that her son was doing well and should continue treatment by saying that he should do “whatever he wants.” Unfortunately, despite all of our efforts, Mr. L insisted on being discharged against medical advice that day.
It became apparent to us in conferencing about this case that Mr. L was a high-risk patent. The dynamic in this family involved a severely depressed mother who needed her depressed son to stay home and be her companion, since he was serving as a replacement for her failed marriage. It would have been helpful if our treatment team could have met with this patient and his family prior to treatment, once we learned about their reluctance to be involved. This case illustrates the complexity of assessing just one of the potential influences on a patient’s course of treatment.
THE DISCHARGE PLAN
Considerations in Discharge Planning
The decision to choose ECT as a treatment and complete a full course, regardless of how helpful it may be, represents a significant commitment. Patients who remit, even those who have a partial response, may attain a level of wellness they have not experienced in years. It is important to keep in mind that methods of assessing response vary greatly from one clinical scenario to another and can include clinical observation, use of the Clinical Global Impressions (CGI) scale,60 or a standardized scale such as the Ham-D.47,61 A detailed discussion of how to define remission and relapse is beyond the scope of this article. According to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM IV-TR),62 for patients to be considered in remission, they must be free of depressive symptoms for 2 months. Patients would be considered relapsed if they again met diagnostic and temporal criteria for major depressive disorder. Although the conceptualization of depression is changing to include a chronic presentation with less defined phases of wellness and relapse,63,64 patients may indeed respond to ECT with improvement that has not occurred with any other treatment. While this is, of course, heartening to all involved, the high incidence of relapse in depression generally and post-ECT specifically is a very serious problem that must be addressed no matter what form of treatment is provided. Thus, the point of discharge from ECT treatment is a critical and challenging juncture. Efforts to develop a discharge plan should start as early as possible in a patient’s treatment and should involve collaboration among the ECT team, unit staff, the outpatient psychiatrist, other mental health professionals who will be following the patient, and the patient’s family/support system. To the greatest extent possible, discharge plans should reflect the plethora of biopsychosocial factors discussed above that could affect the patient and reduce or eradicate the benefits gained from ECT.
Although the factors that can precipitate or contribute to a depressive relapse are legion, it is helpful for clinicians to be cognizant of the most salient of these when planning for discharge. Clinical predictors shown to be associated with potential relapse include history of depressive episodes, duration of the current episode, presence of psychotic symptoms or double depression, previous hospitalizations, comorbid illness, and age of onset of illness.65–67 Patients who have treatment-resistant depression also show reduced response to, and earlier relapse rates following, ECT.68–70 Psychosocial factors that may affect risk of relapse include general family functioning,71,72 the presence of dysfunctional family communications styles (e.g., high “expressed emotion,” a concept with a controversial history),73,74 marital discord,75–77 and degree and perceived quality of social support.66,78,79 The effect of personality disorders (PDs), particularly Cluster B disorders80 on the course of mood disorders81–86 as well as on ECT outcomes and continued wellness following ECT80,87,88 has also been extensively researched. While some studies have found that depressed patients with and without PDs have equivalent acute responses to ECT 80,82,87, others have found poorer acute outcomes for depressed patients with PDs following ECT.89,90 Generally, depressed patients with PDs who respond to ECT have higher rates of relapse and rehospitalization than patients without PDs. A longitudinal prospective study87 found that, at 6 months post-ECT, 62% of patients with major depressive disorder and PDs had been rehospitalized, as opposed to 8% of patients with major depressive disorder only. While there are clearly challenges in reliably diagnosing PDs,89 clinicians are urged to utilize standard assessment tools if a patient’s history or presenting problems suggest a PD. The greater potential for relapse of depressed patients with comorbid PDs should also be considered when developing treatment and discharge plans.81
Choice of treatment regimen following an acute course of ECT can have a significant effect on whether patients stay well. To respond to any treatment regimen, a patient must have an adequate trial, which requires adherence to treatment. Unfortunately, depression itself can affect patients’ adherence to medical advice in general, as well as adherence to specific medication regimens, psychiatric oversight, and other types of therapy.79,91 The relationship that has developed between a patient and members of his or her treatment team can help foster adherence and, hopefully, wellness. A major focus of research on post-ECT medication regimens has been to determine which medication or combination of medications is most effective in staving off a depressive relapse. In one of the earliest double-blind, randomized studies of this kind,92 hospitalized depressed inpatients were randomized to either the tricyclic antidepressant amitriptyline or to diazepam after an acute ECT course to assess which medication class was more effective in staving off relapse. Although the drop-out rate in this study was over 50%, patients randomized to amitriptyline experienced clear advantages in the form of lower depression ratings, less need for an additional course of ECT, and no suicides. Given our increased understanding that depression is a chronic illness and that relapse after acute treatment remains a significant problem, research in this area has remained an important focus. In 2001, Sackeim et al.93 found that combined treatment with nortriptyline plus lithium increased the chances of staying well following an acute course of ECT for unipolar depression. In this randomized, controlled, 5-year trial of 84 patients, relapse was defined as a new episode of depression occurring 6 months or more after the last ECT treatment. Sackeim et al. found a relapse rate of 84% among the patients in the placebo group (i.e., those who were not receiving post-ECT medication). Patients treated with nortriptyline alone had a relapse rate of 60%. Combined treatment produced a significantly lower relapse rate of 39%. In a study published in 2006, Van den Broek et al. compared the efficacy of treatment with imipramine versus placebo after successful ECT in preventing relapse in a cohort of patients who had been unresponsive to pharmacotherapy in the past.94 Although the sample size in this study was small (n = 11 in the treatment group and n = 15 in the placebo group) and relapse was defined based on a CGI assessment rather than the score on a rating scale, such as the Ham-D, these authors found that 18% (2/11) in the treatment group relapsed, versus 80% (12/15) in the placebo group.
For patients who are at greatest risk for relapse (e.g., those with conditions that are medication-resistant, who are medication intolerant, or who have a history of relapse after ECT) continuation ECT (C-ECT) may be recommended. C-ECT is a course of treatment that can continue for up to 6 months for the express purpose of staving off relapse.95 Indications include a 1) history of response, 2) patient preference, and 3) the ability to consent and adhere to the treatment schedule.10 Longer term maintenance ECT (M-ECT), defined as prophylactic use of ECT for longer than 6 months after the end of a patient’s index episode, is aimed at preventing a reoccurrence.12,95
In a review of 14 studies in which C-ECT was provided to patients of various ages with mood disorder diagnoses (e.g., recurrent, single episode, psychotic/non-psychotic major depressive disorder or bipolar disorder), C-ECT was found to be well tolerated and in fact a safer option for elderly or medically compromised patients who may experience adverse effects of ongoing pharmacologic treatments. It was also found to reduce inpatient stays and increase recipients’ productivity, and thus to be cost effective 95
Although most research in this area has been retrospective,12,96 a large, prospective, randomized controlled trial by Kellner et al. published in 200663 found that C-ECT is as efficacious in preventing relapse as the most effective post-ECT pharmacology regimen. In this first multisite, randomized controlled trial of C-ECT versus medication after an acute course of ECT, the investigators randomized 184 patients to either C-ECT or a combination of lithium and nortriptyline after successful remission of symptoms following a course of ECT. This was a strong study involving a large and diverse sample. While there was no compelling difference in relapse rates between the treatments, both C-ECT and continuation pharmacotherapy were shown to be superior to a historical placebo group.93 However, the side-effect profiles of the two treatment groups were markedly different. The side-effect profile for ECT included cognitive effects and headache, nausea and muscle aches on treatment days, while side effects associated with the psychopharmacology regimen included anticholinergic and lithium-specific effects. Kellner et al. made the point that these side-effect profiles are qualitatively different from one another, but did not characterize either as preferential. They also pointed out that relapse after ECT generally occurs early during continuation treatment (i.e., 50% of relapses occurred within the first 4–6 weeks after acute treatment) and that the choice of one treatment over another should be based on patient characteristics and preferences.63 While both treatment arms were relatively effective in staving off a relapse, the authors noted, as did Prudic et al. in their 2004 review of ECT in community settings,90 that rates of relapse following an acute course of ECT are still unacceptably high.
Further work is needed to optimize treatment strategies, including combinations of C-ECT and augmented medication regimens, as well as symptom driven schedules of C-ECT. Because adverse cognitive effects seem to be contingent on the time interval between treatments, it is difficult to develop a consensus statement about these effects.95,96 With the growing realization of the limits of pharmacotherapy, there has been a resurgence of interest in C-ECT and its use is expanding in the United States.97 Treatment schedules for C-ECT vary. The most appropriate frequency of C-ECT treatments as well as how long C-ECT should be continued are determined initially by collaboration between the patient and the ECT team, and then between the patient, the outpatient psychiatrist, and the outpatient ECT provider. Decisions about optimal methods of administration must take into account such factors as individual clinical requirements, insurance coverage, and geographic proximity.96
Developing the Discharge Plan
Multiple variables can affect whether a patient remains well after achieving remission from a depressive episode with ECT (or for that matter any treatment). Once ECT is effective, it is discontinued, and patients, family, and staff collaborate on developing a discharge plan. The support provided by the treatment team during this process is vital. After the cessation of ECT treatment, a patient’s access to psychiatric follow-up and consistent care and the adequacy of his or her support systems are essential factors in helping prevent relapse. These factors must be considered when developing a discharge plan. The plan reflects the input of all parties involved and should be spelled out in writing. Questions that need to be answered as fully as possible in developing a discharge plan are outlined in Table 4:
Table 4.
Questions to address in developing a discharge plan after ECT
| • | Who will follow the patient after the course of ECT is completed? |
| Will the patient return to the original or a new treatment team? | |
| How will information about the patient’s treatment be relayed for follow-up? | |
| Is there an effective alliance between the patient and the outpatient treatment team? | |
| • | What is the recommended post-ECT treatment regimen? |
| Will medication, continuation ECT, or a combination of these be prescribed? | |
| Will the patient receive psychotherapy? If so, in what form (e.g., cognitive-behavioral therapy, psychodynamic)? | |
| What is the patient’s comfort level with these recommendations? | |
| What is the patients’ pharmacologic treatment history? | |
| Does the patient have a history of tolerating prescribed medications? | |
| Will the patient have difficulty obtaining these medications? | |
| If the patient is a candidate for continuation ECT, how can this be arranged? | |
| Are there any specific medical concerns with regard to the prescribed regimen? | |
| Has the inpatient team addressed psychosocial concerns through family/professional collaboration? | |
| What are the patient’s and family members’ primary concerns and fears, and have they been answered/addressed? | |
| Are there psychosocial factors (e.g., compromised housing, marital/family discord, substance abuse in the household or in the patient’s history, difficulty obtaining health/mental health care for geographic reasons) that can be addressed before discharge? | |
| • | Where will patient live and how will he or she spend time during recuperation? |
| Will the patient be discharged to residence or other alternative upon discharge? | |
| Will the patient be referred to a step-down facility, such as a day hospital? | |
| Will the patient return to work/school? What is an appropriate timetable? | |
| Will the patient need to be referred to a supportive program prior to a return to work and/or school? | |
| • | Has the patient’s cognitive status been assessed prior to discharge? |
| Have visual-spatial safety concerns been addressed, especially the patient’s need to drive? | |
| Has the patient been assessed (e.g., by an occupational therapist) for ability to carry out activities of daily living, particularly if the patient lives alone? | |
A major impediment to developing a comprehensive discharge plan is time. Unfortunately, after hospitalized patients have completed an acute course of ECT, it is often the insurance company or the patient’s own ability to pay out of pocket that determines how much longer the person can remain in the treatment setting. These restrictions may even prevent a patient from completing the course of ECT. It can be more difficult to work closely with patients and families when they are being treated on an outpatient basis. However, if a patient is involved in a clinical trial, the costs of treatment to the patient may be minimal and there is likely to be more time to develop and implement comprehensive discharge plans.
CONCLUSION
Clinicians and treatment teams involved in providing ECT have a unique opportunity and responsibility to usher patients through a life-changing transition. This responsibility should not be taken lightly nor should the contributions clinicians can make to a successful outcome be underestimated. Yet ECT is a treatment that continues to be surrounded by controversy. The public and some professionals still lack accurate information about the current practice of ECT. When we view the issues related to ECT through the lens of biomedical ethical principles, as reviewed by Ottosson and Fink10 and Reiter-Theil,4 the seriousness of the considerations facing clinicians becomes clearer. As Reiter-Theil states, the inherent and perhaps most challenging conflict clinicians face in providing treatment with ECT involves balancing patient autonomy (respect for the individual), on the one hand, and the principle of beneficence (doing good or, in this case, helping people get well), on the other. This is particularly problematic with regard to ECT, since patients’ autonomy and ability to consent to this somatic treatment may be compromised by their illness.
The principles of biomedical ethics exemplified in the Belmont Report of 1979, itself a function of the National Research Act of 1974, were developed to protect human subjects involved in biomedical and behavioral research.98 These principles are also used as guidelines for the conduct of clinical practice.10As mentioned, they include autonomy (respect for the individual), beneficence (doing good), non-malfeasance (not doing harm), and justice (fairness in application). Appropriate use of the consent process and a thorough risk-benefit analysis can promote sound medical decisions that maintain both respect for patients’ autonomy and the principle of beneficence. Although difficult to ensure in a free-market society, promoting justice or equal application of a medical treatment among those it could benefit is the final cornerstone in this quadrant of ethical principles.10 Unfortunately for the legacy of ECT, the principles of biomedical ethics were developed and enforced long after the early application of ECT in the treatment of severe psychiatric illness. Thus, if viewed retrospectively, these principles would, at times, have been violated during those early years. Images of early ECT treatment have promulgated a regrettable legacy which survives in the form of negative perceptions, fears, and distortions. Unfortunately, provision of ECT today that is less than state of the art does nothing to dispel these images. In the best of all possible worlds, ECT would be delivered in a technically optimal manner to patients who are not overly fearful, who will benefit from the treatment, who will be assisted in resuming their lives, and whose families will be supportive. While this is, of course, not always the case, each success story and positive experience a patient has can help to re-create the image of this potentially lifesaving treatment. From our perspective, there is tremendous satisfaction gained from facilitating the transition from profound illness to equally profound recovery.
Acknowledgments
This paper was supported in part by NIMH Grant R37 MH35636-21
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
Contributor Information
Nancy A. Payne, New York University (NYU) Silver School of Social Work.
Joan Prudic, New York State Presbyterian Hospital, Columbia campus and New York State Psychiatric Institute
References
- 1.Healy D. The antidepressant drama. In: Weisman MM, editor. Treatment of depression: bridging the 21st century. Washington, DC: American Psychiatric Press; 2001. [Google Scholar]
- 2.Rogers SC, Clay PM. A statistical review of controlled trials of imipramine and placebo in the treatment of depressive illnesses. Br J Psychiatry. 1975;127:599–603. doi: 10.1192/bjp.127.6.599. [DOI] [PubMed] [Google Scholar]
- 3.Fink PJ, Tasman A. The stigma of electroconvulsive therapy: A workshop. In: Fink PJ, Tasman A, editors. Stigma and mental Illness. Washington, DC: American Psychiatric Press; 1992. pp. 189–201. [Google Scholar]
- 4.Reiter-Theil S. Autonomy and beneficence: Ethical issues in electroconvulsive therapy. Convuls Ther. 1992;8:237–244. [PubMed] [Google Scholar]
- 5.American Psychiatric Association Task Force on ECT. Electroconvulsive therapy (Task Force Report # 14) Washington, DC: American Psychiatric Association; 1978
- 6.Lebensohn ZM. Electroconvulsive therapy: Psychiatry’s villain or hero? Am J Soc Psychiatry. 1984;4:39–43. [Google Scholar]
- 7.Endler NS. A holiday of darkness: A psychologist’s personal journal out of his depression. Toronto: Wall & Thompson; 1990. [Google Scholar]
- 8.Payne NA, Prudic J. Electroconvulsive therapy: Part I. A perspective on the evolution and current practice of ECT. J Psychiatr Pract. 2009;15:348–368. doi: 10.1097/01.pra.0000361277.65468.ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shorter E, Healy D. Shock therapy: A history of electroconvulsive treatment in mental illness. Rutgers: Rutgers University Press; 2007. [Google Scholar]
- 10.Ottosson JO, Fink M. Ethics in electroconvulsive therapy. New York: Brunner-Routledge; 2004. [Google Scholar]
- 11.Senter NW, Winslade WJ, Liston EH, et al. Electroconvulsive therapy: The evolution of legal regulation. Am J Soc Psychiatry. 1984;4:11–15. [Google Scholar]
- 12.American Psychiatric Association. second edition. Washington, DC: American Psychiatric Press; 2001. The practice of ECT: Recommendations for treatment, training and privileging. [Google Scholar]
- 13.Andrews M, Hasking P. Effect of two educational interventions on knowledge and attitudes towards electroconvulsive therapy. J ECT. 2004;29:230–236. doi: 10.1097/00124509-200412000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Pettinati HM, Tamburello TA, Ruetsch CR, et al. Patient attitudes toward electroconvulsive therapy. Psychopharmacol Bull. 1994;30:471–475. [PubMed] [Google Scholar]
- 15.Dowman J, Pate A, Rajput K. Electroconvulsive therapy: Attitudes and misconceptions. J ECT. 2005;21:84–86. doi: 10.1097/01.yct.0000161043.00911.45. [DOI] [PubMed] [Google Scholar]
- 16.Brodkey AC. The role of the pharmaceutical industry in teaching psychopharmacology: A growing problem. Acad Psychiatry. 2005;29:222–229. doi: 10.1176/appi.ap.29.2.222. [DOI] [PubMed] [Google Scholar]
- 17.Hirshbein L, Sarvananda S. History, power and electricity: American popular magazine accounts of electroconvulsive therapy, 1940–2005. J Hist Behav Sci. 2008;44:1–18. doi: 10.1002/jhbs.20283. [DOI] [PubMed] [Google Scholar]
- 18.Dukakis K, Tye L. Shock: The healing power of electroconvulsive therapy. New York: Penguin; 2006. [Google Scholar]
- 19.Endler NS, Persad E. Electroconvulsive therapy: The myths and the realities. Toronto: Hans Huber; 1988. [Google Scholar]
- 20.Cauchon D. Controversy and questions—Shock therapy—patients often aren’t informed of full danger. USA Today. 1995 December 6;:1A. 4D, 6D. [Google Scholar]
- 21.Sackeim H, Prudic J, Fuller R, et al. The cognitive effects of electroconvulsive therapy in community settings. Neuropsychopharmacology. 2007;32:244–254. doi: 10.1038/sj.npp.1301180. [DOI] [PubMed] [Google Scholar]
- 22.Shiwach RS, Reid W, Carmody TJ. An analysis of reported deaths following electroconvulsive therapy in Texas, 1993–98. Psychiatr Serv. 2001;52:1095–1097. doi: 10.1176/appi.ps.52.8.1095. [DOI] [PubMed] [Google Scholar]
- 23.Reid W. Don’t malign treatment. USA Today. 1995 December 8;:12A. [Google Scholar]
- 24.News and Notes. Dick Cavett and ECT. Convuls Ther. 1992;8:300–301. [Google Scholar]
- 25.Fink M. Electroshock: Restoring the mind. New York: Oxford University Press; 1999. [Google Scholar]
- 26.McDonald A, Walter G. The portrayal of ECT in American movies. J ECT. 2001;17:264–274. doi: 10.1097/00124509-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Walter G, McDonald A, Rey JM, et al. Medical student knowledge and attitudes regarding ECT prior to and after viewing ECT scenes from movies. J ECT. 2002;18:43–46. doi: 10.1097/00124509-200203000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Abrams R. Electroconvulsive therapy, 3rd edition. New York: Oxford University Press; 2002. [Google Scholar]
- 29.Kramer BA. The use of ECT in California revisited, 1984–1994. J ECT. 1999;15:245–251. [PubMed] [Google Scholar]
- 30.Winslade WJ, Liston EH, Ross JW, et al. Medical, judicial, and statutory regulation of ECT in the United States. Am J Psychiatry. 1984;141:1349–1355. doi: 10.1176/ajp.141.11.1349. [DOI] [PubMed] [Google Scholar]
- 31.Szasz T. The myth of mental illness: Foundations of a theory of personal conduct. New York: Harper & Row; 1974. [Google Scholar]
- 32.Breggin P. Toxic psychiatry: Why therapy, empathy and love must replace the drugs, electroshock, and biochemical theories of the ‘New Psychiatry.’. New York: St. Martin’s Press; 1991. [Google Scholar]
- 33.Goffman E. Asylums: Essays on the social situation of mental patients and other inmates. New York: Doubleday; 1961. [Google Scholar]
- 34.National Institute of Mental Health Consensus Development Panel: Mood disorders: Pharmacologic prevention of recurrences. Am J. Psychiatry. 1985;142:469–476. doi: 10.1176/ajp.142.4.469. [DOI] [PubMed] [Google Scholar]
- 35.American Psychiatric Association: The Practice of ECT: Recommendations for treatment, training, and privileging. Washington DC: American Psychiatric Press; 1990. [Google Scholar]
- 36.Gomez J. Subjective side effects of ECT. Br J Psychiatry. 1975;127:609–611. doi: 10.1192/bjp.127.6.609. [DOI] [PubMed] [Google Scholar]
- 37.Freeman CP, Kendell RE. ECT I: Patients’ experiences and attitudes. Br J Psychiatry. 1980;137:8–16. doi: 10.1192/bjp.137.1.8. [DOI] [PubMed] [Google Scholar]
- 38.Hughes J, Barraclough BM, Reeve W. Are patients shocked by ECT? J R Soc Med. 1981;74:283–285. doi: 10.1177/014107688107400409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benbow SM. Patients’ views on electroconvulsive therapy on completion of a course of treatment. Convuls Ther. 1988;4:146–152. [PubMed] [Google Scholar]
- 40.Janicak PG, Mask J, Trimakas KA, et al. ECT: An assessment of mental health professionals’ knowledge and attitudes. J Clin Psychiatry. 1985;46:262–266. [PubMed] [Google Scholar]
- 41.Pippard J, Ellam L. Electroconvulsive treatment in Great Britain. Br J Psychiatry. 1981;139:563–568. doi: 10.1192/bjp.139.6.563. [DOI] [PubMed] [Google Scholar]
- 42.Kalayam B, Steinhart MJ. A survey of attitudes on the use of electroconvulsive therapy. Hosp Community Psychiatry. 1981;32:185–187. doi: 10.1176/ps.32.3.185. [DOI] [PubMed] [Google Scholar]
- 43.Lutchman RD, Stevens T, Bashir A, et al. Mental health professionals’ attitudes towards and knowledge of electroconvulsive therapy. J Ment Health. 2001;10:141–150. [Google Scholar]
- 44.Szuba MP, Guze BH, Liston EH, et al. Psychiatry resident and medical student perspectives on ECT: Influence of exposure and education. Convuls Ther. 1992;8:110–117. [PubMed] [Google Scholar]
- 45.Dillon P. Electroconvulsive therapy patient/family education. Convuls Ther. 1995;11:188–191. [PubMed] [Google Scholar]
- 46.Weiner RD, Coffey CE. When ECT is recommended for your patient. Med Aspects Hum Sex. 1988 June;:20–24. [Google Scholar]
- 47.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 48.Nelmes M. Preoperative teaching helps reduce anxiety. Dimens Health Serv. 1989;66:23–25. [PubMed] [Google Scholar]
- 49.Nyamathi A, Kashiwabara A. Preoperative anxiety: Its effect on cognitive thinking. AORN J. 1988;47:164–169. doi: 10.1016/s0001-2092(07)70065-0. [DOI] [PubMed] [Google Scholar]
- 50.Davis L, Rosenthal GT, Soper B. Structuring and anxiety reduction prior to myelography. Psychol Rep. 1990;66:1171–1176. doi: 10.2466/pr0.1990.66.3c.1171. [DOI] [PubMed] [Google Scholar]
- 51.Wilkinson D, Daoud J. The stigma and enigma of ECT. Int J Geriatr Psychiatry. 1998;13:833–835. doi: 10.1002/(sici)1099-1166(1998120)13:12<833::aid-gps884>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 52.Lukens EP, Thorning H. Psychoeducation and severe mental illness: Implications for social work practice and research. In: Williams JBW, Ell K, editors. Advances in mental health research: Implications for practice. Washington, DC: NASW Press; 1998. [Google Scholar]
- 53.Baxter LR, Roy-Byrne P, Liston EH, et al. Informing patients about electroconvulsive therapy: Effects of a videotape presentation. Convuls Ther. 1986;2:25–29. [PubMed] [Google Scholar]
- 54.Jenaway A. Educating patients and relatives about electroconvulsive therapy: The use of an information leaflet. Psychiatr Bull. 1993;17:10–12. [Google Scholar]
- 55.Fox H. Patients’ fear of and objection to electroconvulsive therapy. Hosp Community Psychiatry. 1993;44:357–360. doi: 10.1176/ps.44.4.357. [DOI] [PubMed] [Google Scholar]
- 56.Hepworth DH, Rooney RH, Rooney GD, et al. Direct social work practice: Theory and skills, 5th edition. Belmont, CA: Thomson Brooks/Cole; 2006. [Google Scholar]
- 57.Deegan P. Recovery as a self-directed process of healing and transformation. In: Brown C, editor. Recovery and wellness: Models of hope and empowerment for people with mental illness. New York: Haworth Press; 2001. pp. 5–22. [Google Scholar]
- 58.Hepworth DH, Rooney RH, Larsen J. Direct social work practice: Theory and skills, 5th edition. Pacific Grove, CA: Brooks/Cole Publishing; 1997. [Google Scholar]
- 59.Rosen LE, Amodor XF. When someone you love is depressed: How to help your loved one without losing yourself. New York: Free Press; 1996. [Google Scholar]
- 60.Guy W. ECDEU assessment manual for psychopharmacology-revised (DHEW Publ. No ADM 76-338) Rockville, MD: U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976:218–222.
- 61.Endicott J, Cohen J, Nee J, et al. Hamilton depression rating scale. Extracted from regular and change versions of the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry. 1981;38:98–103. doi: 10.1001/archpsyc.1981.01780260100011. [DOI] [PubMed] [Google Scholar]
- 62.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 4th edition, text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 63.Kellner CH, Knapp RG, Petrides G, et al. Continuation electroconvulsive therapy vs pharmacotherapy for relapse prevention in major depression: A multisite study from the Consortium for Research in Electroconvulsive Therapy (CORE) Arch Gen Psychiatry. 2006;63:1337–1344. doi: 10.1001/archpsyc.63.12.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Üstün TB. The worldwide burden of depression in the 21st century. In: Weissman MM, editor. Treatment of depression: Bridging the 21st century. Washington DC: American Psychiatric Press; 2001. pp. 35–45. [Google Scholar]
- 65.Giles DE, Jarrett RB, Biggs MM, et al. Clinical predictors of recurrence in depression. Am J Psychiatry. 1989;146:764–767. doi: 10.1176/ajp.146.6.764. [DOI] [PubMed] [Google Scholar]
- 66.Belsher G, Costello CG. Relapse after recovery from unipolar depression: A critical review. Psychol Bull. 1988;104:84–96. doi: 10.1037/0033-2909.104.1.84. [DOI] [PubMed] [Google Scholar]
- 67.Bourgon LN, Kellner CH. Relapse of depression after ECT: A review. J ECT. 2000;16:19–31. doi: 10.1097/00124509-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 68.Prudic J, Sackeim HA, Devanand DP. Medication resistance and clinical response to electroconvulsive therapy. Psychiatr Res. 1990;31:287–296. doi: 10.1016/0165-1781(90)90098-p. [DOI] [PubMed] [Google Scholar]
- 69.Prudic JM, Sackeim HA, Rifas S. Medication resistance, response to ECT, and prevention of relapse. Psychiatr Ann. 1994;24:228–231. [Google Scholar]
- 70.Sackeim HA, Prudic J, Devanand DP, et al. The impact of medication resistance and continuation pharmacotherapy on relapse following response to electroconvulsive therapy in major depression. J Clin Psychopharmacol. 1990;10:96–104. doi: 10.1097/00004714-199004000-00004. [DOI] [PubMed] [Google Scholar]
- 71.Keitner GI, Ryan CE, Miller IW, et al. Recovery and major depression: Factors associated with twelve-month outcome. Am J Psychiatry. 1992;149:93–99. doi: 10.1176/ajp.149.1.93. [DOI] [PubMed] [Google Scholar]
- 72.Keitner GI, Ryan CE, Miller IW, et al. Role of the family in recovery and major depression. Am J Psychiatry. 1995;152:1002–1008. doi: 10.1176/ajp.152.7.1002. [DOI] [PubMed] [Google Scholar]
- 73.Hooley JM, Orley J, Teasdale JD. Levels of expressed emotion and relapse in depressed patients. Br J Psychiatry. 1986;148:642–647. doi: 10.1192/bjp.148.6.642. [DOI] [PubMed] [Google Scholar]
- 74.Veiel HOF, Kuhner C. Relatives and depressive relapse: The critical period after discharge from inpatient treatment. Psychol Med. 1990;20:977–984. doi: 10.1017/s0033291700036680. [DOI] [PubMed] [Google Scholar]
- 75.Whisman MA, Bruce ML. Marital dissatisfaction and incidence of major depressive episode in a community sample. J Abnorm Psychol. 1999;108:674–678. doi: 10.1037//0021-843x.108.4.674. [DOI] [PubMed] [Google Scholar]
- 76.Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and family process in depression: A scientific foundation for clinical practice. Washington DC: American Psychological Association; 2001. pp. 3–24. [Google Scholar]
- 77.Whiffen VE. Disentangling causality in the associations between couple and family processes and depression. In: Pinsof WM, Lebow JL, editors. Family psychology: The art of the science. New York: Oxford University Press; 2005. pp. 375–395. [Google Scholar]
- 78.Barnett PA, Gotlib IH. Psychosocial functioning and depression: Distinguishing among antecedents, concomitants, and consequences. Psychol Bull. 1988;104:97–126. doi: 10.1037/0033-2909.104.1.97. [DOI] [PubMed] [Google Scholar]
- 79.Thase ME. The roles of psychosocial factors and psychotherapy in refractory depression: Missing pieces in the puzzle of treatment resistance? In: Nolen WA, Zohar J, Roose SP, et al., editors. Refractory depression: Current strategies and future directions. New York: John Wiley and Sons; 1994. [Google Scholar]
- 80.DeBattista C, Mueller K. Is electroconvulsive therapy effective for the depressed patients with comorbid personality disorder? J ECT. 2001;17:91–98. doi: 10.1097/00124509-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 81.Black DW, Bell S, Hulbert J, et al. The importance of Axis II in patients with major depression: A controlled study. J Affect Disord. 1988;14:115–122. doi: 10.1016/0165-0327(88)90053-5. [DOI] [PubMed] [Google Scholar]
- 82.Pfohl B, Stangl D, Zimmerman M. The implications of DSM-III personality disorders for patients with major depression. J Affect Disord. 1984;7:309–318. doi: 10.1016/0165-0327(84)90052-1. [DOI] [PubMed] [Google Scholar]
- 83.Pilkonis PA, Frank E. Personality pathology in recurrent depression: Nature, prevalence, and relationship to treatment response. Am J Psychiatry. 1988;145:435–441. doi: 10.1176/ajp.145.4.435. [DOI] [PubMed] [Google Scholar]
- 84.Shea MT, Pilkonis PA, Beckham E, et al. Personality disorders and treatment outcome in the NIMH treatment of depression collaborative research program. Am J Psychiatry. 1990;147:711–718. doi: 10.1176/ajp.147.6.711. [DOI] [PubMed] [Google Scholar]
- 85.Torgerson AR. Personality and personality disorders predict development and relapses of major depression. Acta Psychiatr Scand. 1997;95:336–342. doi: 10.1111/j.1600-0447.1997.tb09641.x. [DOI] [PubMed] [Google Scholar]
- 86.Gunderson JG, Morey LC, Stout RL, et al. Major depressive disorder and borderline personality disorder revisited: Longitudinal interactions. J Clin Psychiatry. 2004;65:1049–1056. doi: 10.4088/jcp.v65n0804. [DOI] [PubMed] [Google Scholar]
- 87.Zimmerman M, Coryell W, Pfohl B, et al. ECT response in depressed patients with and without a DSM-III personality disorder. Am J Psychiatry. 1986;143:1030–1032. doi: 10.1176/ajp.143.8.1030. [DOI] [PubMed] [Google Scholar]
- 88.Kramer BA. Poor response to electroconvulsive therapy in patients with a combined diagnosis of major depression and borderline personality disorder. The Lancet. 1982;2(8306):1048. doi: 10.1016/s0140-6736(82)90083-6. [DOI] [PubMed] [Google Scholar]
- 89.Sareen J, Murray E, Guertin J. The impact of clinically diagnosed personality disorders on acute and one-year outcomes of electroconvulsive therapy. J ECT. 2000;16:43–51. doi: 10.1097/00124509-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 90.Prudic J, Olfson M, Marcus SC, et al. Effectiveness of electroconvulsive therapy in community settings. Biol Psychiatry. 2004;55:301–312. doi: 10.1016/j.biopsych.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 91.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 92.Kay DWK, Kahy T, Garside RF. A 7-month double blind trial of amitriptyline and diazepam in ECT-treated patients. Br J Psychiatry. 1970;117:667–671. doi: 10.1192/bjp.117.541.667. [DOI] [PubMed] [Google Scholar]
- 93.Sackeim HA, Haskett RF, Mulsant BH, et al. Continuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: A randomized controlled trial. JAMA. 2001;285:1299–1307. doi: 10.1001/jama.285.10.1299. [DOI] [PubMed] [Google Scholar]
- 94.van den Broek WW, Birkenhäger TK, Mulder PG, et al. Imipramine is effective in preventing relapse in electroconvulsive therapy-responsive depressed inpatients with prior pharmacotherapy treatment failure: A randomized, placebo-controlled trial. J Clin Psychiatry. 2006;67:263–268. doi: 10.4088/jcp.v67n0213. [DOI] [PubMed] [Google Scholar]
- 95.Rabheru K, Persad E. A review of continuation and maintenance electroconvulsive therapy. Can J Psychiatry. 1997;42:476–484. doi: 10.1177/070674379704200503. [DOI] [PubMed] [Google Scholar]
- 96.Sackeim H. Continuation therapy following ECT: Directions for future research. Psychopharmacol Bull. 1994;30:501–521. [PubMed] [Google Scholar]
- 97.Sackeim H, Lisanby S. Physical treatments in psychiatry. In: Weissman MM, editor. Treatment of depression: Bridging the 21st century. Washington DC: American Psychiatric Press; 2001. pp. 151–174. [Google Scholar]
- 98.National Institute of Health (NIH) Regulations and ethical guidelines. [accessed August 12, 2009];Washington, DC: NIH; no date (Available at http://ohsr.od.nih.gov/guidelines/belmont.html,)