Abstract
Background
Children with spina bifida often present with functional deficits of the lower limb associated with neurosegmental lesion levels and require orthotic management. The most used orthosis for children with spina bifida is the ankle–foot orthosis (AFO). The AFO improves ambulation and reduces energy cost while walking. Despite the apparent benefits of using an AFO, limited evidence documents the influence of factors predicting the ability of an AFO to improve function and when they are indicated. These variables include AFO design, footwear, AFO–footwear combination, and data acquisition. When these variables are not adequately considered in clinical decision-making, there is a risk the AFO will be abandoned prematurely or the patient’s stability, function, and safety compromised.
Purpose
The purposes of this study are to (1) describe the functional deficits based on lesion levels; (2) identify and describe variables that influence the ability of an AFO to control deformities; and (3) describe what variables are indicated for the AFO to control knee flexion during stance, hyperpronation, and valgus stress at the knee.
Methods
A selective literature review was undertaken searching MEDLINE and Cochrane databases using terms related to “orthosis” and “spina bifida.”
Results
Based on previous studies and gait analysis data, suggestions can be made regarding material selection/geometric configuration, sagittal alignment, footplate length, and trim lines of an AFO for reducing knee flexion, hyperpronation, and valgus stress at the knee.
Conclusion
Further research is required to determine what variables allow an AFO to improve function.
Introduction
Children with spina bifida frequently present with neurologic levels of lesion with functional deficits leading to diminished walking. Lesion levels commonly extend from “high lumbar” to “low sacral” and often cause skeletal malalignment, sensory loss, and motor weakness. These factors can create instability across the lower limbs that impair a child’s ability to walk [1].
Depending on the functional deficit, the use of an ankle–foot orthosis (AFO) will often help improve alignment and walking for children with spina bifida [23]. AFOs can address deficits related to walking and can improve temporal spatial gait characteristics [9], reduce energy cost [21], and decrease pathologic moments across the ankle and knee [9]. The AFO is the most frequently used orthosis for spina bifida for the lower limbs although its use is dependent on the level of lesion [23]. Recognizing the benefits and frequency of AFO use is helpful, but understanding what makes the AFO improve function is of greater value for successful treatment.
For an AFO to improve alignment and walking, a comprehensive evaluation of the patient is required and best achieved with input from the entire medical team [2, 11]. A comprehensive evaluation should include: (1) status of proprioceptive/sensory impairment; (2) level of neurological involvement; (3) degree of musculoskeletal deformity; (4) acquired obesity; (5) status of existing muscle strength; (6) perception impairment (visual/motor); (7) patient/family motivation; and (8) family support [1, 7, 18, 20]. General indications for use of an AFO include excessive knee flexion, hyperpronation, and valgus stress at the knee.
Despite the apparent benefits of using an AFO, there is little objective evidence regarding the influence specific variables can have on the ability of an AFO to restore alignment and walking ability. These variables include data acquisition and impression techniques, sagittal alignment of the orthosis–footwear combination, footplate length of the AFO, lateral/medial trim lines of the AFO, and posting considerations. For an AFO to help with alignment and walking, it is important to know how these variables will influence a specific child with spina bifida. When specific variables that influence the ability of an AFO to improve function are not considered, there is a greater possibility that orthotic management will be abandoned prematurely, the AFO will need to be remade, alternative treatment pursued, or patient stability and function compromised.
Therefore, the purposes of this article are to: (1) describe the functional deficits based on lesion levels; (2) identify and describe variables that influence the ability of an AFO to improve function; and (3) describe what variables are indicated for the AFO to manage knee flexion during stance, hyperpronation, and valgus stress at the knee.
Functional Deficits Associated With Each Lesion Level
For children with spina bifida, the level of lesion, in large part, is the determining factor of a child’s functional deficits. Lesion levels typically extend from high lumbar to low sacral. The former usually presents with a more distinct motor absence, whereas the later exhibits greater motor variability characterized by fatigue. For the purpose of this discussion, the low lumbar, high sacral, and low sacral lesion levels require further consideration.
A low lumbar lesion characteristically presents with motor deficits of ankle plantarflexors/dorsiflexors, hip abductors, and extensors, resulting in a crouch pattern of gait. The distinct features include posterior trunk lean, excessive hip, knee, ankle flexion, excessive pelvic rotation, and obliquity and lateral trunk lean.
A patient with a high sacral lesion exhibits greater overall strength across the hip compared with a patient with a low lumbar lesion. Although active, the hip extensors and abductors will still exhibit some weakness and should be monitored for endurance. Dorsiflexion strength presents with some variation, whereas plantarflexor strength remains absent. Gait deviations closely resemble that of the low lumbar level lesion.
Compared with low lumbar and high sacral lesions, the low sacral lesion presents with variable muscle weakness of the foot/ankle complex but relative sparing of hip and knee motor function. As a result of the high level of variability of muscle strength, assessment should focus on prolonged walking, because this appears to be a good indicator of the person’s actual gait pattern and function [23].
Varying degrees of crouch gait [16] present as a collective pattern of rotational deformities or Internal Rotary Deformity/Pathway (IRD/IRP). An IRD is the biomechanical skeletal realignment of a limb in stance phase in response to internal moments and muscle activity under full weightbearing [5]. The crouch gait pattern for a child with spina bifida typifies an IRD and includes: forefoot abduction, midfoot pronation, hindfoot valgus, ankle dorsiflexion, medial rotation of the tibia–fibula unit, valgus stress at the knee, knee flexion, medial femoral rotation, and hip flexion.
The varying degrees of a crouch pattern of gait are typically caused when the weakened or absent soleus muscle is unable to oppose an external dorsiflexion moment, which leads to a persistent incline of the tibia during stance phase of gait. When the soleus is weakened, the results are continuous ankle dorsiflexion, concomitant hip and knee flexion, and a 60% decrease in walking velocity compared with normal [24]. This invariably leads to further malalignment of the foot/ankle.
Hyperpronation is one component of the crouch pattern of gait and associated IRD. It is important to consider because many children with spina bifida have calcaneovalgus foot/ankle deformities [6]. Hyperpronation of the foot collectively presents as hindfoot valgus, midfoot pronation, and forefoot abduction. As a result of this malalignment, the foot is unable to attain an adequate lever arm to support the body, causing further hyperpronation and an increased crouch pattern of gait.
In addition to hyperpronation, the crouch pattern of gait and associated IRD can lead to a persistent valgus stress at the knee. Knowing how the valgus stress is caused is important because many adults with spina bifida have knee problems [8, 14, 25]. According to Ounpuu et al. [16], valgus stress across the knee is more a result of coronal trunk motion than tibial torsion. However, it was noted in this same study that increased transverse plane range of motion in the knee was most related to transverse plane trunk motion. This increase in transverse motion may be a contributing factor to the valgus stress. Other investigations have had similar findings and indicate that when plantar flexors are absent and dorsiflexion increases, there is a concomitant increase in medial tibial and knee rotation [22, 23] that may contribute to the valgus stress. Furthermore, individuals with lumbosacral myelomeningocele exhibit an increasing valgus stress at the knee as the thigh–foot angle increases and knee flexion appears related to the valgus stress if the thigh–foot angle is at 10° to 20° [11].
Variables That Influence the Ability of an AFO to Improve Function
When a child with spina bifida presents with functional deficits, the ability of an AFO to address these deficits largely depends on the variables that influence the alignment and design of the AFO. These variables include acquisition of measurements/impression, sagittal alignment of the AFO–footwear combination, footplate length of the AFO, lateral/medial trim lines of the AFO, and posting considerations. One must also consider data acquisition and impression technique process. Many data acquisition methods and impression techniques have been described in the literature [5, 17, 19], but few have examined their influence on the ability of an AFO to improve function.
An impression for rotational deformities such as an IRD should be preceded with full and semiweightbearing assessment to determine how much of the transverse deformity can be reduced by manual manipulation of the patient’s limb. Without this type of assessment the AFO design is at risk for “under” correction, in which the deformity still persists, or “over” correction of the deformity, in which the patient is unable to tolerate the corrective forces.
Although the data acquisition and impression technique provides information necessary to properly align the AFO, the alignment of the AFO on the patient and in the shoe has the greatest impact. Proper alignment requires a clear distinction between a patient’s existing ankle angle compared with the AFO alignment in the shoe and the alignment of the tibia relative to the floor. The former can be determined during the impression technique phase, whereas the latter can only be assessed when the patient is wearing the AFO.
The sagittal alignment, particularly the shank angle to the floor (SAF) (Fig. 1), is largely dependent on how the AFO interfaces with the footwear. The type of footwear can affect how stable an AFO is inside the shoe. The combined effects of the shoe and the AFO are referred to as the AFO–footwear combination (AFOFC) and can impact sagittal alignment and influence shank kinematics of the tibia.
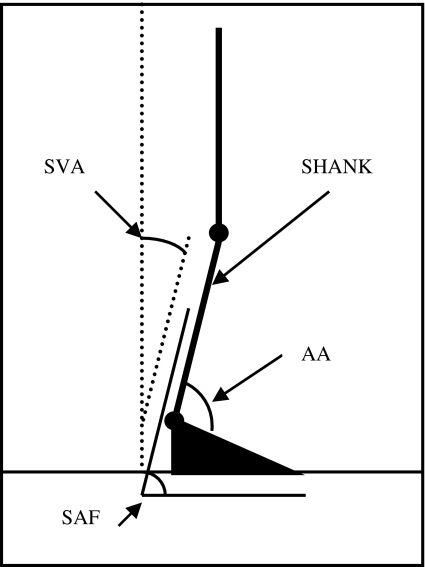
Fig. 1.
A diagram shows relative tibial shank alignment. The ankle angle of the AFO (AAAFO) is the relationship between the tibial section and footplate of the AFO. The shank angle to vertical (SVA) is the position of the tibial shank relative to the force of gravity acting vertically. The shank angle to the floor (SAF) is the position of the tibial shank relative to the floor.
For sagittal alignment variables of an AFO to have value, the clinical application must be apparent to the medical team. Once the patient is wearing the AFO, the focus should be on the SAF, because this is the primary determinant for proper standing and gait alignment. The SAF can be manipulated by using footwear with a heel–sole differential or by placing heel wedges between the inside of the shoe and the plantar aspect of the AFO. The initial alignment should focus on stabilizing the proximal joints of the lower limb and ensuring proper postural alignment. This is often between 10º and 12º of a forward incline of the SAF; however, it may lie in a broader range (7º to 15º) [13] depending on the clinical presentation.
The effects of AFO sagittal alignment can be impacted by selection of the proper footplate length. Based on the clinical presentation, the footplate length can limit or preserve joint motion to facilitate function and increase walking stability. We found that a full-length footplate can increase stance phase dorsiflexion and plantarflexion moments around the ankle when compared with no AFOs [4]. Based on these observations, the full footplate length of a solid AFO design not only provides stability around the ankle, but can indirectly stabilize the knee and influence the alignment of the hip during walking.
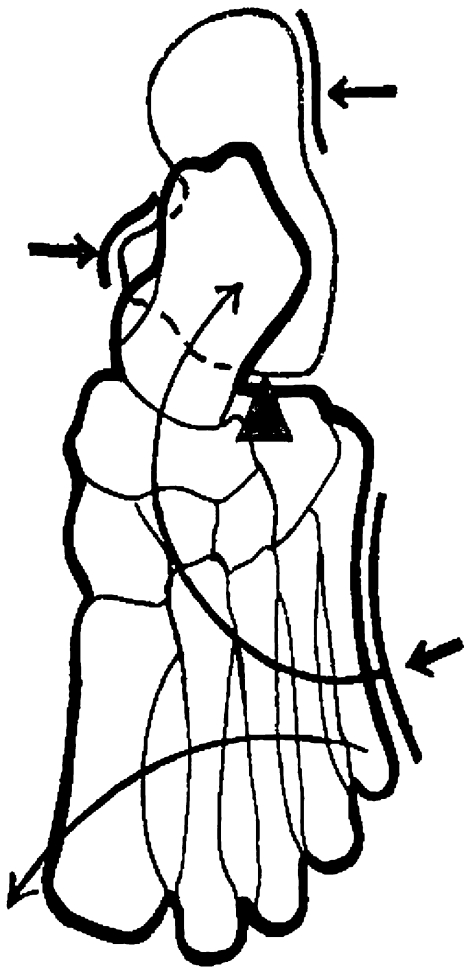
While the footplate length of an AFO preserves or limits joint motion, the function of the lateral and medial trim lines (walls) of the AFO is intended to provide appropriate alignment of the foot. The lateral and medial walls are most effective at maintaining alignment of the foot by providing a three-point force system represented by two forces laterally and one force medially (Fig. 2).
Fig. 2.
A diagram shows the appropriate three-point force system provided by an AFO to reduce hyperpronation.
When the lateral and medial walls of the AFO are not able to provide sufficient alignment of the foot, the addition of “external posting,” or sustentaculum tali modifications, can help improve alignment of the foot. This modification provides an external shelf in the AFO, positioned underneath the sustentaculum tali to prevent valgus and improve joint congruency between the calcaneus and talus when hyperpronation is present [3].
Indications for an AFO in Children With SB
An AFO and the variables associated with design and alignment can be indicated for various functional deficits associated with spina bifida. Each indication requires consideration to ensure that AFO design and alignment selection is appropriate, given the patient’s functional deficits. The three indications considered include excessive knee flexion during stance phase, hyperpronation, and valgus stress at the knee.
To reduce excessive knee flexion during stance phase, the AFO design and associated variables must be appropriately selected to make the orthosis effective. The goal is to prevent unwanted forward tibial translation during stance phase to improve the sagittal kinematics of the knee. An AFO design incapable of preventing unwanted forward tibial translation during the stance phase of gait is unlikely to stop excessive knee flexion. AFO design options that can prevent excessive knee flexion during stance phase include solid thermoplastic AFO, solid thermoplastic AFO with carbon fiber reinforcement, thermoset AFO, and energy storing thermoplastic designs or a dynamic assist carbon fiber AFO [15, 26]. Selection of the AFO design will likely dictate which associated variables require the most attention in limiting tibial translation.
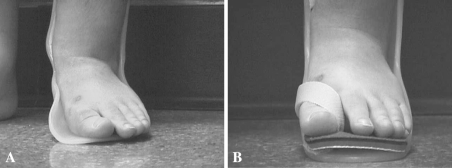
Many patients with excessive knee flexion will have hyperpronation as a secondary component of a crouch gait pattern, and that can also be managed with an AFO. Protecting the foot, ankle, and skin as well as restoration of (functional) alignment and proper gait mechanics are important considerations when designing an AFO for hyperpronation. AFO design considerations include long lateral wall, medial posting of the hindfoot/forefoot, and limitation of dorsiflexion. Of particular importance when managing hyperpronation with an AFO is the distal aspect of the lateral wall and its affect on forefoot abduction. The lateral wall of the AFO can prevent forefoot abduction, but when it is compromised to fit the AFO into the shoe, the hyperpronation is likely to persist. This can result in increased pressure and erythema across the midfoot, navicular or head of the talus medially, and be of particular concern in the presence of impaired sensation (Fig. 3A). When preserved, the lateral wall can improve alignment and weight distribution across the foot (Fig. 3B).
Fig. 3A–B.
(A) A photograph shows a patient in whom the lateral wall of the AFO has been removed. The result is increased pressure across the midfoot and medial malleolus. (B) A photograph shows a patient in whom the lateral wall has been restored with a different AFO. Note improved foot and ankle alignment and improved subtalar alignment.
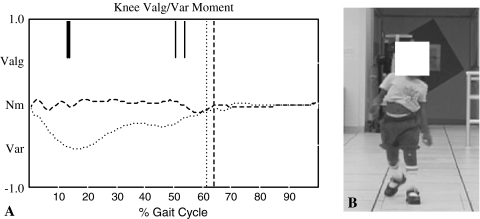
An AFO that helps hyperpronation may simultaneously be required to limit a valgus stress at the knee. Valgus stress is frequently seen in the presence of crouch gait and hyperpronation, and an AFO can reduce the deformity [11, 21]. If the valgus stress is a component of an IRD and crouch gait pattern, the deformity is likely to respond well to an AFO. If a true genu valgum is present, the use of an AFO may create discomfort across the knee. For an AFO to reduce the valgus stress, it will limit excessive dorsiflexion in stance phase and increase coronal diameter of footwear [10] and orthosis. When designing an AFO to reduce or limit dorsiflexion the trim lines, carbon fiber reinforcement, plastic corrugation, and material selection are all factors that should be considered to limit valgus stress. If the valgus stress persists at the knee, a medial buttress can be added to the external portion of the AFO in the location of the heel. This will increase the coronal diameter of the orthosis and limit movement of the orthosis in the shoe. An example of the AFO’s ability to reduce the valgus stress at the knee is illustrated with the results of gait analysis performed on a child with and without an AFO. The patient presented with a crouch gait and IRD that was managed with solid AFOs and shoes that included a wider coronal diameter of the sole. Without bilateral solid AFOs, this patient exhibited an internal varus moment at the knee, but with the AFOs, the valgus stress was reduced (Fig. 4). Because a likely contributing factor to the valgus stress is the crouch gait and IRD, the AFOs are able to limit excessive dorsiflexion. As a result, the AFOs were able to normalize elements of gait and provide better upright stability for the patient.
Fig. 4A–B.
(A) A graph shows the knee valgus/varus moment. The dotted line represents a patient walking barefoot and shows an internal varus moment at the knee. The dashed line represents the same patient wearing bilateral solid AFOs and as a result the internal varus moment has been reduced. (B) A photo of a patient with spina bifida. Although there is a persistent lateral trunk lean, the valgus thrust has been reduced. An external medial buttress was added to the AFO and shoe selection included a wider sole base to address the valgus thrust at the knee.
Discussion
AFOs are frequently used to manage functional deficits of the lower limbs for children with spina bifida. Although there is evidence describing the benefits of AFOs, it is difficult to determine what factors influence their ability to improve function and when these factors are indicated. Therefore, our purposes were to: (1) describe the functional deficits based on lesion levels; (2) identify and describe variables that influence the ability of an AFO to improve function; and (3) describe what variables manage excessive knee flexion, hyperpronation, and valgus stress at the knee.
A literature review included a search of MEDLINE, Cochrane, and Journal of Prosthetics and Orthotics databases, but is subject to a number of limitations. First, a review was performed using two conventional databases, but did not include a review of CINAHL or RECAL, nor were specific search inclusion/exclusion criteria established. As a result of these limitations, this article should be considered a selective, rather than systematic, review and the reader should be aware the selection of articles reflects the opinions of the author, not necessarily the literature. Second, this review describes variables that can assist in clinical decision-making, but offers no conclusive evidence about efficacy and is based on clinical experience and gait analysis data. Third, the literature review did not include a search of the “variables” themselves, but was limited to “orthoses” and “spina bifida” terms. Although this survey does reflect the opinions of this author, the literature review suggests these variables have not been sufficiently addressed. In a systematic review of literature between 1974 and 2003 regarding the efficacy of orthotic management for the lower limbs in children with myelomeningocele [12], the authors found studies specific to AFOs reflected level II and level IV levels of evidence. This author reviewed these same papers and, with the exception of one paper [9], found those studies did not identify or control for the variables described in this discussion. That systematic review found agreement about the ability of an AFO to control sagittal deformity, but it was unclear which variables make an AFO effective for this purpose. This was true of deformities in the coronal and transverse planes, with no clear indication of a relationship between variables, AFO design, and deformity. Finally, previous investigations about AFOs address the material and type of orthosis, but little is mentioned about design. Absent from these studies was discussion about alignment, footwear, trim lines, and posting considerations. As a result, it is difficult to know which variables make an AFO improve function. Furthermore, it would be difficult to reproduce these studies because they neglected to describe the design and variables of the AFO and control for the variables described in this discussion to determine the effects of the AFO.
For children with spina bifida, the neurologic level of lesion can lead to functional deficits characterized by skeletal malalignment that, if allowed to persist, can make ambulation difficult and cause joint pain later in life. For this reason, functional deficits require orthotic treatment to improve alignment and protect the lower limbs from pathologic forces that can limit mobility. To address functional deficits, specific variables were identified and described as necessary for an AFO to improve function. A review of the literature found one reference to sagittal alignment of the AFO–footwear combination, footplate length, and shoe modifications, but did not measure its effects [9]. Material selection and configuration were noted in several studies [17] and provide some application strategies for AFOs. There were no studies related to how data acquisition and impression techniques might influence the effectiveness of an AFO to restore function.
Use of an AFO for excessive knee flexion in crouch gait for children with spina bifida can improve sagittal knee alignment during gait [8, 21]. Some literature and kinematic data suggest the following strategies be considered when using an AFO: (1) using materials such as carbon-fiber or polypropylene to increase stiffness of the AFO; (2) AFO trim line configurations that stiffen the AFO and prevent forward tibial movement (rigid AFO) or resist forward tibial motion (carbon fiber spring AFO); and (3) the structural stiffness of the AFO footplate length and structural stiffness to resist external dorsiflexion moments.
Management of hyperpronation with an AFO has been described in several studies [17], but the effects on alignment and function are unclear. The impact of the AFO to reduce hyperpronation in the spina bifida population was not measured, but correction is consistent with the biomechanical principles of three-point force systems, total contact [5], and the relationship to the lateral and medial wall of the AFO. It is important to remember that the sustentaculum modification [3] can prevent hindfoot valgus, and preservation of the lateral wall of the AFO can prevent forefoot abduction.
Several studies [9, 12, 21] and the gait analysis data presented indicate that an AFO can reduce valgus stress at the knee. What remains unclear from previous investigations are variables of an AFO that have the greatest effect on the valgus stress at the knee.
Providing an appropriate AFO for a child with spina bifida requires a thorough evaluation of the patient and understanding of the functional deficits associated with each lesion level. Although there is evidence that AFOs can address specific deformities and can improve specific attributes of gait, it is difficult to determine what variables can influence the effectiveness of the AFO for specific clinical indications.
Acknowledgement
I thank Kevin Meade, PhD, for his feedback.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Asher M, Loson J. Factors affecting the ambulatory status of patients with spina bifida cystic. J Bone Joint Surg Am. 1983;65:350–356. [PubMed] [Google Scholar]
- 2.Banta JV, Lin R, Peterson M, Dagenais T. The team approach in the care of the child with myelomeningocele. J Prosthet Orthot. 1990;2:263–271. doi: 10.1097/00008526-199000240-00006. [DOI] [Google Scholar]
- 3.Carlson JM, Berglund G. An effective orthotic design for controlling the unstable subtalar joint. Orthotics and Prosthetics. 1979;33:39–49. [Google Scholar]
- 4.Fatone S, Gard SA, Malas BS. Effects of ankle–foot orthosis alignment and foot-plate length on the gait of adults with poststroke hemiplegia. Arch Phys Med Rehabil. 2009;90:810–818. doi: 10.1016/j.apmr.2008.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Fish DJ, Nielsen JP. Clinical assessment of human gait. J Prosthet Orthot. 1993;5:39–50. doi: 10.1097/00008526-199304000-00005. [DOI] [Google Scholar]
- 6.Fraser RK, Hoffman EB. Calcaneus deformity in the ambulant patient with myelomeningocele. J Bone Joint Surg Br. 1991;73:994–997. doi: 10.1302/0301-620X.73B6.1955450. [DOI] [PubMed] [Google Scholar]
- 7.Graham HK, Harvey A, Rodda J, Nattrass GR, Pirpiris M. The functional mobility scale. J Pediatr Orthop. 2004;24:514–520. doi: 10.1097/01241398-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Haskell A, Mann RA. Biomechanics of the foot. In: Hsu JD, Michael JW, Fisk JR, editors. AAOS Atlas of Orthoses and Assistive Devices. 4. Philadelphia, PA: Mosby; 2008. pp. 311–324. [Google Scholar]
- 9.Hullin MG, Robb JE, Loudon IR. Ankle–foot orthosis function in low-level myelomeningocele. J Pediatr Orthop. 1992;12:518–521. [PubMed] [Google Scholar]
- 10.Janisse DJ. Shoes and shoe modifications. In: Hsu JD, Michael JW, Fisk JR, eds. AAOS Atlas of Orthoses and Assistive Devices, 4th ed. Philadelphia, PA: Mosby; 2008:325–333.
- 11.Lim R, Dias L, Vankowski S, Moore C, Marinello M, Sarwark J. Valgus knee stress in lumbosacral myelomeningocele: a gait-analysis evaluation. J Pediatric Orthop. 1998;18:428–433. [PubMed] [Google Scholar]
- 12.Mazur JM, Kyle S. Efficacy of bracing the lower limbs and ambulation training in children with myelomeningocele. Dev Med Child Neurol. 2004;46:352–356. doi: 10.1111/j.1469-8749.2004.tb00497.x. [DOI] [PubMed] [Google Scholar]
- 13.Meadows B, Bowers RJ, Owen E. Biomechanics of the hip, knee, and ankle. In: Hsu JD, Michael JW, Fisk JR, editors. AAOS Atlas of Orthoses and Assistive Devices. 4. Philadelphia, PA: Mosby; 2008. pp. 299–309. [Google Scholar]
- 14.Menelaus MB. The knee. In: Broughton NS, Menelaus MB, editors. The Orthopaedic Management in Spina Bifida Cystica. Philadelphia, PA:: Saunders; 1998. pp. 129–134. [Google Scholar]
- 15.Novacheck TF, Beattie C, Rozumalski A, Gent G, Kroll G. Quantifying the spring-like properties of ankle–foot-orthoses (AFO’s) J Prosthet Orthot. 2007;19:98–108. doi: 10.1097/JPO.0b013e31812e555e. [DOI] [Google Scholar]
- 16.Õunpuu S, Thompson JD, Davis RB, Luca PA. An examination of the knee function during gait in children with myelomeningocele. J Pediatric Orthop. 2000;20:629–635. doi: 10.1097/01241398-200009000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Polliack AA, Elliot S, Landsberger SE, McNeal DR, Caves C. Lower extremity orthoses for children with myelomeningocele: user and orthotist perspectives. J Prosthet Orthot. 2001;13:123–133. doi: 10.1097/00008526-200112000-00012. [DOI] [Google Scholar]
- 18.Stillwell A, Menelaus MB. Walking ability in mature patients with spina bifida. J Pediatr Orthop. 1983;3:184–190. doi: 10.1097/01241398-198305000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Supan TJ. Principles of fabrication. In: Hsu JD, Michael JW, Fisk JR, editors. AAOS Atlas of Orthoses and Assistive Devices . 4. Philadelphia, PA: Mosby; 2008. pp. 53–60. [Google Scholar]
- 20.Thomas SS, Buckon CE, Melchionni J, Magnusson M, Aiona MD. Longitudinal assessment of oxygen cost and velocity in children with myelomeningocele: comparison of the hip–knee–ankle–foot orthosis and the reciprocating gait orthosis. J Pediatr Orthop. 2001;21:798–803. doi: 10.1097/00004694-200111000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Thompson JD, Ounpuu S, Davis RB, Luca PA. The effects of ankle–foot-orthoses on the ankle and knee in persons with myelomeningocele: an evaluation using three-dimensional gait analysis. J Pediatr Orthop. 1999;19:27–33. doi: 10.1097/00004694-199901000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Vankowski SJ, Dias LS. Clinical gait analysis in myeolomeningocele: motion in the sagittal, coronal, and transverse planes. In: Sarwark JF, Lubicky JP, editors. Caring for the Child With Spina Bifida. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2001. pp. 283–297. [Google Scholar]
- 23.Vankowski SJ, Michaud S, Dias L. External tibial torsion and the effectiveness of the solid ankle-foot orthosis. J Pediatric Orthop. 2000;20:349–355. [PubMed] [Google Scholar]
- 24.Vankoski SJ, Sarwark JF, Moore C, Dias L. Characteristic pelvic, hip, and knee kinematic patterns in children with lumbosacral myelomeningocele. Gait Posture. 1995;3:51–57. doi: 10.1016/0966-6362(95)90809-7. [DOI] [Google Scholar]
- 25.Williams JJ, Graham GP, Dunne KB, Menelaus MB. Late knee problems in myelomeningocele. J Pediatric Orthop. 1993;13:701–705. doi: 10.1097/01241398-199311000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Wolf SI, Alimusaj M, Rettig O, Döderlein L. Dynamic assist by carbon fiber spring AFOs for patients with myelomeningocele. Gait Posture. 2008;28:175–177. doi: 10.1016/j.gaitpost.2007.11.012. [DOI] [PubMed] [Google Scholar]