Abstract
Background
Patients with spina bifida potentially experience social isolation with limited employment opportunities and restriction of independent living, neurologic and intellectual impairment, and orthopaedic and urologic consequences of their condition. However, the degree of disability as these individuals age into adulthood has not been completely delineated.
Questions/purpose
In adults with spina bifida we determined the cause of death for those who had died, IQ, level of education, work history, independent living status, physical disabilities, and urologic status; we then identified surgical procedures that led to better adult function.
Methods
We retrospectively reviewed 84 individuals with myelomeningocele, examining social, cognitive, and physical disabilities. The minimum age at followup was 20 years (mean, 31 years; range, 20–64 years).
Results
Forty-two percent had normal IQs. Seventy percent never needed a neurosurgical shunt and those without shunts had higher IQs. Forty-four percent had regular education and 8% achieved college degrees. Fifty-six percent were unemployed. Thirty percent lived independently. Twenty-three percent were either married or divorced with nine normal offspring. Eighty-five percent dressed themselves, 65% shopped independently, 54% drove. Thirty-one percent were at the thoracic neurologic level (all used wheelchairs), 12% were at L1–L3 (all used a wheelchair except one), 33% were at L4–L5 (78% used a wheelchair at least part-time), and 24% were at S1 and below (all walked). Fifty-four percent experienced decubiti and as a consequence, four required major extremity amputations. Spinal fusions protected sitting balance, but hip surgery did not produce congruent hips and occasionally resulted in debilitating stiffness. Pressure sores resulted in partial foot amputations despite plantigrade feet.
Conclusions
Our observations confirm the consequences associated with the physical and cognitive disabilities of patients with spina bifida. Many of these consequences can likely be mitigated by modern multidisciplinary care and special education to increase independence.
Level of Evidence
Level IV, observational study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Individuals born with spina bifida (myelomeningocele) face serious physical and social consequences, including paralysis, insensate skin, and potential social ostracism associated with loss of bowel and bladder control. Over time, muscle paralysis can produce contractures, joint dislocations, and spinal deformity. Loss of protective skin sensation may result in pressure sores. Urinary incontinence with attendant frequent bladder infections can produce eventual renal failure.
Medical and surgical interventions (including early closure of the neural tube defect, neurosurgical treatment of associated hydrocephalus, prevention of contractures and joint dislocations, and clean intermittent catheterization [5]) decrease the likelihood of mortality and the severity of related physical deformities. Nevertheless, patients with spina bifida have medical and social problems throughout their lives. Varying degrees of cognitive impairment often accompany the spina bifida. Numerous studies [2, 6, 8, 14, 15, 18, 21, 22] have examined the short-term effectiveness of surgical treatment and several have investigated the physical, neurologic, and social issues associated with spina bifida. Orthopaedic deformities, bowel and bladder incontinence, and reduced cognitive functioning [10] result in a lower self-concept [19] compared with healthy children. The need for catheterization and the presence of physical abnormalities may create insecurities in affected teenagers and young adults that prevent them from developing intimate relationships [14, 22]. Although the literature has documented the physical and cognitive disabilities of patients with spina bifida, we are not confident that substantial improvements in the multidisciplinary care of individuals with spina bifida have occurred. Unfortunately the outcomes of individuals with spina bifida who have received more modern treatments may not be better than those in the past. A report of patients with spina bifida treated on average 16 years after our individuals demonstrated essentially equivalent outcomes [16].
In adults with spina bifida we determined the cause of death for those who had died, IQ, education and work histories, independent living status, physical disabilities, and urologic status were study variables. We also identified surgical procedures that subsequently led to better adult function.
Patients and Methods
Between 1941 and 1964, 221 patients with spina bifida were seen at Texas Scottish Rite Hospital (TSRH). From 1985 to 1987, we attempted to examine all prior patients but could locate only 149 of them with 72 lost to followup. Forty-five of the 149 had died, 12 refused to participate in the study, and eight lived in state schools; permission was denied for their participation. The remaining 84 former patients whose average age was 31 years (range, 20–58 years) constitute this study.
We evaluated the current social situation of our cohort using parameters of IQ, education and employment, living arrangements and marriage, and other markers of independence. We ascertained intellectual function with IQ testing and information about physical problems such as limited ambulation, hydrocephalus, joint contractures, spine deformities, pressure sores, and urinary incontinence with a physical examination and activities of daily living test. This work was performed in the 1980s with the verbal permission of the research participants and the institution. At that time, there was no Institutional Review Board to consider the proposal.
Data collection included physical assessment and a questionnaire; 59 were able to return to TSRH to complete both aspects of the study and 25 completed only the questionnaire. The physical assessment included an examination administered by one of the authors (JWR); an evaluation of the ability to perform activities of daily living administered by a TSRH occupational therapist (AS); pertinent radiographs; photographs; and laboratory measurements of blood urea nitrogen (BUN) and creatinine.
One of the authors (BFS) read aloud a written questionnaire to patients and recorded their answers. We used medical charts and the questionnaire to collect data including histories of patients’ neurosurgical procedures; orthopaedic procedures; highest level of education achieved; current employment status as well as whether this employment provided sufficient income to be independent; ambulatory status; and method of urinary control.
Although the questionnaire included questions relating to bowel and bladder control, in determining function, we only used data from subjects who completed both the questionnaire and physical assessment. This was done because the term “control” proved ambiguous (eg, some patients who wore diapers considered themselves to have bowel and bladder control) and we wanted to determine with the examination the type of control and whether the patient was judged by us (JWR, BFS) to have socially acceptable control of bowel and bladder.
Wechsler Adult Intelligence Scale-Revised (WAIS-R) IQ tests [24] were administered by a TSRH psychologist (AM) who recommended that for the psychometric test administered to this group, an IQ of 90 would be considered average intelligence (normal WAIS-R IQ is 90 to 110). We acknowledge this mark may be lower than standards used in other situations.
Results
Forty-five individuals died before the review. The age range and cause of death are described (Table 1).
Table 1.
Cause of death of 45 individuals
| Cause of death | Died before age 10 | Died after age 10 |
|---|---|---|
| General infection | 10 | 5 |
| Hydrocephalus | 6 | 1 |
| Heart failure | 2 | 3 |
| Kidney failure | 1 | 3 |
| Unknown | 8 | 6 |
| Total | 27 | 18 |
The majority of individuals in our group (58%) had an IQ less than 90; the remaining 42% scored more than 90 (Table 2). Twenty-five subjects (30%) had a ventriculoperitoneal shunt and had required between one and 25 revisions and 59 patients (70%) never needed a shunt. Requirement for a shunt correlated with neurologic level (Table 3).
Table 2.
IQ testing
| Category | Percent |
|---|---|
| Intellectually disabled (IQ of < 60) | 9% |
| Borderline intellectually disabled (IQ of 60–70) | 26% |
| Low intelligence (IQ of 80–90) | 23% |
| Normal (IQ of > 90) | 42% |
Table 3.
IQ versus shunt and neurologic level
| Shunt and neurologic level | IQ > 90 |
|---|---|
| Shunt | 53% |
| No shunt | 65% |
| Thoracic/upper lumbar | 57% |
| Lower lumbar/sacral | 69% |
All but 2% of the study individuals received some type of education. The majority (54%) received special education, and the remaining 44% received regular education. Only 8% of patients achieved college degrees.
At the time of the followup, 56% of the individuals were unemployed and 36% worked full-time. Employment was related to IQ (Table 4).
Table 4.
Employment versus IQ
| Employment status | Entire group | IQ > 90 | IQ < 70 |
|---|---|---|---|
| Full-time/part-time | 36% | 52% | 15% |
| Unemployed | 56% | 38% | 75% |
| College | 2% | 5% | 0% |
| Sheltered workshop | 4% | 0% | 10% |
| Retired | 2% | 5% | 0% |
Seventy percent of the individuals lived with their parents or in an institution; 30% lived independently at the time of followup. At the time of our study, 76% of the individuals were not married or in intimate relationships. Fifteen percent were married (12 female and one male) with seven children among them, and 8% were divorced (six female and one male) with two children. All nine children were born without spina bifida and in each instance the mother had spina bifida and the father did not. One female was widowed and had not remarried.
Study individuals experienced varying degrees of independence in their everyday lives. The majority (85%) dressed themselves. Sixty-five percent shopped independently, and 54% could drive. Seventy-six percent had their own bank accounts, and 57% were receiving government aid.
Neurologic level correlated with ambulation (Table 5).
Table 5.
Ambulation status
| Neurologic level and percent of entire group | Ambulation status | ||||
|---|---|---|---|---|---|
| Full-time wheelchair | Part-time wheelchair | Walk full-time with crutches | Walk part-time without crutches | Walk full-time without crutches | |
| Thoracic (31%) | 100% | ||||
| L1-L3 (12%) | 86% | 14% | |||
| L4-L5 (33%) | 78% | 22% | |||
| Sacral (24%) | 100% | ||||
Fifty-four percent of the 59 examined individuals experienced pressure sores (decubiti) during their lifetime. None of the current sores dated from childhood. However, surgical treatment had required major amputations, including a hemipelvectomy in one individual and a hip disarticulation in another. At the time of examination, 44% had active pressure sores in the pelvic area or lower extremities. Pelvic decubiti did not correlate well with pelvic obliquity because 38% of the individuals with pelvic obliquity never had decubiti. Several others had decubiti on the high side of their pelvic obliquity and many had an ischial decubitus with a level pelvis (Table 6). Ten L5 or sacral-level patients had active pressure foot sores. Four sacral-level patients had required amputations of or within the foot as a result of pressure sores, one Symes and three ray resections. At the time of followup, one of the foot ray amputations and both the hip disarticulation and the hemipelvectomy still had active ulcers. The amputations were performed during débridement for osteomyelitis and an attempt was made to maintain maximal length of the limb; thus, the amputation level was often still in an area of insensate skin. Because pressure sores were observed on the high side of pelvic obliquity and on plantigrade feet, the sores were attributed to loss of sensation and/or inability of the individual to care for their skin. One individual with a Symes amputation walked with a prosthesis.
Table 6.
Pelvic pressure sores
| Pelvic obliquity | Decubiti |
|---|---|
| Decubitus on the low side of obliquity | 47% |
| Decubitus on the high side of obliquity | 13% |
| Midline decubitus | 4% |
| Prior hip disarticulation and hemipelvectomy | 8% |
| No pelvic obliquity | 28% |
Half of the examined individuals with thoracic level lesions and 27% of patients with L3 and below had scoliosis of greater than 20°. Twenty percent of patients had spinal fusions. Although pelvic obliquity persisted in many patients, the fusions often decreased the severity of the obliquity and improved sitting balance.
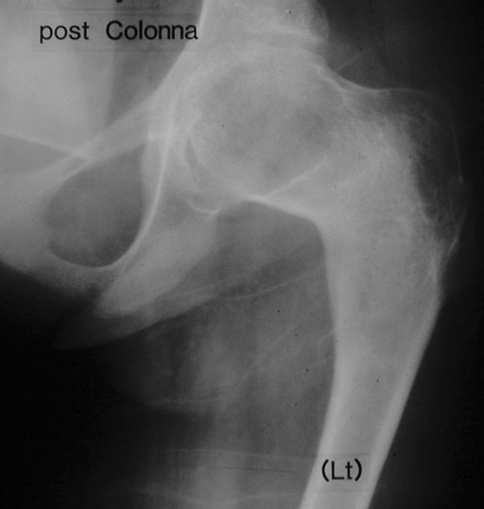
Hip dislocations commonly occurred when neurologic levels were L4 and above. Hip reduction surgery often failed and postoperative stiffness in several individuals substantially decreased function (Fig. 1). All of the hips that underwent surgical reductions either redislocated or settled into varying degrees of subluxation.
Fig. 1.
This radiograph demonstrates the adult outcome of a Colonna arthroplasty performed on a 9-year-old L3-level patient with a dislocated hip. The hip is ankylosed.
Among examined individuals, there were 37 tendon transfers in the foot, which included lateral transfers of the anterior tibialis tendon, transfers of the anterior tibialis tendon to the heel, and transfers of the posterior tibialis tendon to the dorsum of the foot. Eleven of these tendon transfers were functional, 22 were inactive, and it was impossible to determine whether the remaining four were truly functional because severe joint stiffness precluded active movement.
There had been 13 Grice procedures; from this group, 10 remained plantigrade and three required conversion to triple arthrodeses. Of the 27 triple arthrodeses 22 remained plantigrade, four developed recurrent deformities, and one developed pressure sores requiring amputation. All four patients with recurrent deformity underwent revisions: three pantalar arthrodeses and one talectomy. All four of these attempts at revision failed and the feet developed severe recurrent deformities.
Seven percent of those examined were in active renal failure with BUN levels of greater than 40 and creatinine levels above 3 (Table 7). Twenty-nine percent of the examined individuals had inadequate bowel or bladder control.
Table 7.
Urologic status
| Individual’s techniques for urinary control | Socially acceptable | Renal failure |
|---|---|---|
| Intact urinary control (14) | 14 | |
| Clean intermittent catheterization (6) | 6 | |
| Indwelling Foley catheters (3) | 3 | 2 |
| Ilioconduits (18) | 15 | 1 |
| Wore diapers (12) | 0 | |
| Condom catheters (6) | 4 | 1 |
Discussion
Patients with spina bifida frequently experience social isolation with limited employment opportunities and restriction of independent living, neurologic and intellectual impairment, and orthopaedic and urologic consequences of their condition. The previous literature, however, does not clearly define the rates at which these consequences occur. We therefore determined the physical and social condition of adults with spina bifida. The study variables included the cause of death for those who had died, IQ, education and work histories, independent living status, physical disabilities, any beneficial orthopaedic surgeries, and urologic status.
We acknowledge limitations to our study. First, we lost data that compromised the depth of analysis. The data in this report are means and ranges because after these computations were made, the individual study participants’ research charts were accidentally destroyed. The loss of data prevented detailed correlation between physical disabilities and function. However, the remaining data still provide valuable information about the cohort. Second, the patients in our cohort were treated 48 to 68 years ago; current treatment might create different findings with less intellectual impairment and hip stiffness. As an example, the small number of shunted patients in our study likely reflects a selection process because in the years 1941 to 1961, many patients with severe hydrocephalus died and thus never came to our tertiary orthopaedic hospital. Contemporary neurosurgical care has focused on providing prompt venticuloperitoneal shunting to diminish impairment from hydrocephalus [13]. Current orthopaedic care has been directed toward the spine to improve sitting balance with fewer surgical procedures to maintain hip reductions [7]. Third, 25 patients completed the questionnaire but were not able to return to the hospital for an examination. Some of the 25 questionnaire-only patients undoubtedly had important sequelae of their condition that were not counted. Nevertheless, our data document much of the adult consequences of spina bifida, including the social implications of disabilities such as reduced cognitive capabilities, limited ambulation, and urinary incontinence.
Adults typically die from sepsis or renal failure [15]. In our study, the majority of individuals younger than age 10 died from generalized infection and older than age 10 infection and renal failure were the most common reasons for death.
Several followup studies found a correlation similar to ours between the requirement for a shunt and low IQs [9, 16, 17]. Although IQ cannot be dramatically changed, an individual’s independence is a result of not only inherent cognitive abilities, but also environmental factors. In a past study, a group of adolescents with spina bifida participated in a 2-week camp that involved activities and counseling to improve their self-esteem, independence, and employability [3]. Campers demonstrated both immediate and long-term improvements, including increased socialization with friends, learning to drive a car with handicap controls, and seeking summer employment, when compared with a control group of patients with spina bifida who did not attend the camp. We predict enrolling children with myelomeningocele in special education programs that focus on realistic capabilities would engender similar results as the described camp experience.
Our study correlated IQ, level of education, history of employment, and ability to live independently. Only 42% of our patients had an IQ above 90 and of those, only 52% worked full- or part-time. Comparing our results with recent literature raises questions regarding whether outcomes have improved. A study evaluating adults with spina bifida whose treatment occurred an average of 16 years after our patients [16] reflected a similar experience regarding successful independent living (37% versus our 30%) and driving (39% versus our 54%). Seventy percent of their individuals had IQs greater than 80 compared with our study in which 42% had IQs greater than 90. Nevertheless, only 26% of their subjects were regularly employed compared with 36% of our individuals. The majority of individuals in our cohort received special education, but the special education programs of 30 to 70 years ago were much less focused on the patients’ specific problems and may have been less effective in helping them become educated and independent. Modern special education programs, specifically designed to help children with spina bifida transition to adulthood, should greatly improve the futures of children with the condition. A publication in 2001 described a 20- to 25-year followup of 71 adults with spina bifida and found 85% were attending or had graduated from high school or college [4]. Only 8% of our group achieved a college degree. Perhaps the modern availability of focused, special education classes in the early years of school helped those individuals achieve the skills necessary to succeed in college. In addition, online curricula, diversity programs, and the increased variety of degree choices currently offered in college allow for a larger group of handicapped people to attend. Architectural barriers limiting access to buildings for handicapped people were also more common in the past and modern building design may account for the apparent increase in college attendance for wheelchair-dependent people with spina bifida.
The results of the followup physical examination suggest several possible improvements in orthopaedic care for patients with spina bifida. Many of the orthopaedic surgeries performed for these children did not improve their function and, in several instances, seemed detrimental. Common procedures such as hip reduction surgery often failed with the hip remaining subluxated at followup. A few of the postoperative hips were stiff and resulted in loss of ambulatory function. Hip reduction surgery has been advocated for L4–L5 level patients to help maintain their walking capabilities, because walking with a reduced hip consumes less energy compared with walking with a substantial Trendelenburg gait. Nevertheless, 78% of the L4–L5 level individuals used a wheelchair at least part-time. Individuals’ global function depended more on the ROM of the hip than on whether it was located or dislocated. Because better lower extremity ROM benefitted function, contracture releases were probably helpful. However, these surgeries were performed in the distant past and the amount of permanent contracture improvement was difficult to determine because many of the charts did not document the preoperative degree of contracture.
Individuals with spinal fusions had better postoperative sitting balance and therefore needed less upper extremity support to sit. This probably allowed them to use their hands more as compared with individuals with severe untreated spinal curves. However, there were several individuals who had untreated severe spinal curves and who also functioned at a very high level. Our impression that spinal deformity surgery improved sitting balance but did not dramatically improve physical function was also described in a recent paper [23]. Orthopaedic surgery performed to maintain plantigrade feet was helpful. Individuals with feet that were substantially deformed had trouble with ambulation even if their neurologic level was low and their muscle strength good. However, plantigrade feet still had high rates of pressure sores and many low-level patients needed partial foot amputations.
Medical problems that affect children with spina bifida continue and become increasingly difficult to manage throughout adulthood [25], and patients’ physical and neurologic conditions hinder their ability to function as independent individuals. Our study subjects were in need of good general medical care, occasional general orthopaedic care, and treatment of pressure sores.
Despite the physical disabilities, we speculate the right type of education and family environment can help diminish the negative social consequences associated with spina bifida. Encouraging and guiding parents to cultivate early independence in their children will impact their success as adults [12, 20]. Multidisciplinary spina bifida clinics have been effective in providing treatment for these children’s complex medical and orthopaedic problems. Likewise, the closure of a multidisciplinary spina bifida clinic has been demonstrated to have a deleterious effect on the patient’s subsequent treatment [11]. Multidisciplinary clinics that focus on treating children with spina bifida should include social and psychological assessment of the child and the parents. Some multidisciplinary spina bifida clinics only involve social workers and psychologists on an “as-needed” basis [1]. Unfortunately, managing children with spina bifida with a multidisciplinary clinic that evaluates only the patient’s medical and orthopaedic needs will ignore the issues that become crucial in adulthood: developing independence, employment, and social acceptance. Our study suggests the potential benefit of individualized educational programs focused on goals judged to be achievable by each participant. Our study also suggests orthopedic surgery should be very selective and focused on achieving a straight spine with a level pelvis, supple joints, and plantigrade feet.
Acknowledgments
We thank Adenia Spencer, OTR, for her assistance in assessing the study subjects’ activities of daily living and Anne Morton, PhD, for the psychologic testing.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Texas Scottish Rite Hospital (data collection) and the University of Utah/Shriners Hospitals for Children (data analysis).
References
- 1.Asher M, Olson J, Weigel J, Morantz R, Harris J, Leiberman B, Whitney W (1979) The myelomeningocele patient. A multidisciplinary approach to care. J Kans Med Soc. 80:403–408, 413 [PubMed]
- 2.Bier JA, Prince A, Tremont M, Msall M. Medical, functional, and social determinants of health-related quality of life in individuals with myelomeningocele. Dev Med Child Neurol. 2005;47:609–612. doi: 10.1017/S0012162205001209. [DOI] [PubMed] [Google Scholar]
- 3.Bodzioch J, Roach JW, Schkade J. Promoting independence in adolescent paraplegics: a 2-week ‘camping’ experience. J Pediatr Orthop. 1986;6:198–201. doi: 10.1097/01241398-198603000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg. 2001;34:114–120. doi: 10.1159/000056005. [DOI] [PubMed] [Google Scholar]
- 5.Danielsson AJ, Bartonek A, Levey E, McHale K, Sponseller P, Saraste H. Associations between orthopaedic findings, ambulation and health-related quality of life in children with myelomeningocele. J Child Orthop. 2008;2:45–54. doi: 10.1007/s11832-007-0069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dillon CM, Davis BE, Duguay S, Seidel KD, Shurtleff DB. Longevity of patients born with myelomeningocele. Eur J Pediatr Surg. 2000;10(Suppl 1):33–34. doi: 10.1055/s-2008-1072412. [DOI] [PubMed] [Google Scholar]
- 7.Heeg M, Broughton NS, Menelaus MB. Bilateral dislocation of the hip in spina bifida: a long-term follow-up study. J Pediatr Orthop. 1998;18:434–436. doi: 10.1097/00004694-199807000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Hunt GM. Open spina bifida: outcome for a complete cohort treated unselectively and followed into adulthood. Dev Med Child Neurol. 1990;32:108–118. doi: 10.1111/j.1469-8749.1990.tb16910.x. [DOI] [PubMed] [Google Scholar]
- 9.Hunt GM. The Casey Holter lecture. Non-selective intervention in newborn babies with open spina bifida: the outcome 30 years on for the complete cohort. Eur J Pediatr Surg. 1999;9(Suppl 1):5–8. doi: 10.1055/s-2008-1072302. [DOI] [PubMed] [Google Scholar]
- 10.Iddon JL, Morgan DJ, Loveday C, Sahakian BJ, Pickard JD. Neuropsychological profile of young adults with spina bifida with or without hydrocephalus. J Neurol Neurosurg Psychiatry. 2004;75:1112–1118. doi: 10.1136/jnnp.2003.029058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaufman BA, Terbrock A, Winters N, Ito J, Klosterman A, Park TS. Disbanding a multidisciplinary clinic: effects on the health care of myelomeningocele patients. Pediatr Neurosurg. 1994;21:36–44. doi: 10.1159/000120812. [DOI] [PubMed] [Google Scholar]
- 12.Kirpalani HM, Parkin PC, Willan AR, Fehlings DL, Rosenbaum PL, King D, Nie AJ. Quality of life in spina bifida: importance of parental hope. Arch Dis Child. 2000;83:293–297. doi: 10.1136/adc.83.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lacy M, Pyykkonen BA, Hunter SJ, Do T, Oliveira M, Austria E, Mottlow D, Larson E, Frim D. Intellectual functioning in children with early shunted posthemorrhagic hydrocephalus. Pediatr Neurosurg. 2008;44:376–381. doi: 10.1159/000149904. [DOI] [PubMed] [Google Scholar]
- 14.Lindehall B, Moller A, Hjalmas K, Jodal U, Abrahamsson K. Psychosocial factors in teenagers and young adults with myelomeningocele and clean intermittent catheterization. Scand J Urol Nephrol. 2008;42:539–544. doi: 10.1080/00365590802273218. [DOI] [PubMed] [Google Scholar]
- 15.McDonnell GV, McCann JP. Why do adults with spina bifida and hydrocephalus die? A clinic-based study. Eur J Pediatr Surg. 2000;10(Suppl 1):31–32. doi: 10.1055/s-2008-1072411. [DOI] [PubMed] [Google Scholar]
- 16.Oakeshott P, Hunt GM. Long-term outcome in open spina bifida. Br J Gen Pract. 2003;53:632–636. [PMC free article] [PubMed] [Google Scholar]
- 17.Oi S, Sato O, Matsumoto S. Neurological and medico-social problems of spina bifida patients in adolescence and adulthood. Childs Nerv Syst. 1996;12:181–187. doi: 10.1007/BF00301248. [DOI] [PubMed] [Google Scholar]
- 18.Peeker R, Damber JE, Hjalmas K, Sjodin JG, Zweigbergk M. The urological fate of young adults with myelomeningocele: a three decade follow-up study. Eur Urol. 1997;32:213–217. [PubMed] [Google Scholar]
- 19.Shields N, Taylor NF, Dodd KJ. Self-concept in children with spina bifida compared with typically developing children. Dev Med Child Neurol. 2008;50:733–743. doi: 10.1111/j.1469-8749.2008.03096.x. [DOI] [PubMed] [Google Scholar]
- 20.Vachha B, Adams R. Influence of family environment on language outcomes in children with myelomeningocele. Child Care Health Dev. 2005;31:589–596. doi: 10.1111/j.1365-2214.2005.00542.x. [DOI] [PubMed] [Google Scholar]
- 21.Mechelen MC, Verhoef M, Asbeck FW, Post MW. Work participation among young adults with spina bifida in the Netherlands. Dev Med Child Neurol. 2008;50:772–777. doi: 10.1111/j.1469-8749.2008.03020.x. [DOI] [PubMed] [Google Scholar]
- 22.Verhoef M, Barf HA, Post MW, Asbeck FW, Gooskens RH, Prevo AJ. Secondary impairments in young adults with spina bifida. Dev Med Child Neurol. 2004;46:420–427. doi: 10.1017/S0012162204000684. [DOI] [PubMed] [Google Scholar]
- 23.Wai EK, Young NL, Feldman BM, Badley EM, Wright JG. The relationship between function, self-perception, and spinal deformity: implications for treatment of scoliosis in children with spina bifida. J Pediatr Orthop. 2005;25:64–69. doi: 10.1097/00004694-200501000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Wechsler D. WAIS-R: Manual: Wechsler Adult Intelligence Scale–Revised. New York, NY: Psychological Corporation; 1981. [Google Scholar]
- 25.Woodhouse CR. Myelomeningocele in young adults. BJU Int. 2005;95:223–230. doi: 10.1111/j.1464-410X.2005.05374.x. [DOI] [PubMed] [Google Scholar]