Summary
Background and objectives
Acute infusion of the potent V2 receptor agonist 1-desamino-8-d-arginine vasopressin (dDAVP) reduces sodium excretion in humans, through an effect attributed to the stimulation of the amiloride sensitive epithelial sodium channel, ENaC, in ex vivo/in vivo experiments. We investigated in humans whether the antinatriuretic effect of dDAVP is sensitive to amiloride, a specific blocker of ENaC.
Design, setting, participants, & measurements
Forty-eight healthy normotensive adult men were assigned to a high Na/low K (250/40 mmol/d) diet, to suppress aldosterone secretion. dDAVP (4-μg intravenous bolus followed by 4 μg over 2 hours) was administrated before and after a 7-day administration of 20 mg/d amiloride. Urine and blood samples were collected before and at the end of the dDAVP infusion, to measure Na, K, creatinine, and osmolality concentrations.
Results
dDAVP alone decreased the urinary flow rate by 75% and the sodium excretion rate by 19% despite an increase in creatinine clearance by 38 ml/min. Potassium excretion rate was unchanged and the urinary Na/K ratio decreased by 18%. Seven-day amiloride administration had no effect on the dDAVP-induced decrease in the urinary flow rate (−71%) nor on the dDAVP-induced increase in creatinine clearance (+35 ml/min), but it fully prevented the dDAVP-induced decrease in both urinary sodium excretion (+1%) and urinary Na/K ratio (+21%).
Conclusions
The antinatriuretic effect of dDAVP in humans is amiloride sensitive, and thus is related to the stimulatory effect on ENaC-mediated sodium reabsorption. This test provides a new tool to investigate ENaC function in a clinical setting.
Introduction
Vasopressin (AVP), secreted in response to increases in plasma osmolality, plays a key role in water metabolism by stimulating renal water conservation. Vasopressin leads to a rapid increase in solute-free water reabsorption, by increasing water permeability of principal cells of the collecting ducts (CD) via a V2 receptor–mediated (V2R-mediated) translocation of aquaporin 2 water channels to the apical cell membrane (1). Water reabsorption then occurs through osmotic equilibration between the hypo-osmotic tubular fluid delivered at the end of the diluting segment and, successively, the iso-osmotic cortical and hyperosmotic medullary interstitial fluids (1). Thereafter, water reabsorption in the outer medulla is enhanced by the acute increase in osmolality of the medullary interstitium, which occurs secondary to V2R-mediated translocation of UT-A1 and/or UT-A3 urea channels to the apical membrane of inner medullary CDs (2).
In addition to its effect on water permeability, vasopressin influences renal sodium handling. Conflicting results on the vasopressin effects on sodium reabsorption have been reported depending on the experimental setting (isolated collecting duct cell lines, isolated kidney, or in vivo), the concentration/dose administered, and the hydration status (3–5). These differences have been resolved by Perucca et al., who showed in rats that vasopressin at physiologic doses promotes distal sodium reabsorption in vivo via a V2R-mediated effect, whereas at supraphysiologic concentrations, it induces a natriuretic effect via a V1aR-mediated effect (6). Moreover, acute infusion of 1-desamino-8-d-arginine-vasopressin (dDAVP), a potent V2R agonist, was shown in healthy humans to reduce sodium excretion along with its antiaquaretic effect, without affecting potassium secretion (7). The V2R-mediated antinatriuretic effect of vasopressin has been attributed, in ex vivo/in vitro experiments on isolated CDs and various cell lines, to the stimulation of the activity and expression of the amiloride sensitive epithelial sodium channel (ENaC) of the principal CD cells (8–14). However, that AVP may influence ENaC activity has not been evaluated in humans.
The aim of this clinical investigation was thus to investigate whether the ENaC blocker, amiloride, can fully or partially block the antinatriuretic effects of the V2R agonist dDAVP. We studied the effects on urine flow rate, osmolality, and Na and K excretion of acute V2R stimulation by dDAVP before and after 7-day oral administration of 20 mg oral daily (o.d.) amiloride. The patients were subjected to a high sodium (Na)/low potassium (K) diet to suppress endogenous aldosterone secretion, as aldosterone also influences ENaC-mediated sodium reabsorption.
Materials and Methods
Participants
Forty-eight healthy normotensive white male, nonsmoking patients (age, 23.2 ± 3.9 years; body mass index, 23.0 ± 2.3 kg/m2) were enrolled in the study after providing written and informed consent. Data from one patient was excluded from analysis because of inadequate urinary collection.
The protocol (ClinicalTrials.gov: NCT2006-005056-32) was approved by the Comité de Protection des Personnes Paris, Ile de France III (France), and all procedures were in accordance with the Declaration of Helsinki.
Study Protocol
Participants were assigned to a high Na/low K (250/40 mmol/d) diet for 14 days with protein, caloric, and water intake kept constant. All meals were provided by the metabolic kitchen of the hospital and were taken in the unit.
On day 3 of the diet, patients completed a 24-hour urine collection. On day 4 at 9:00 a.m., after a 12-hour overnight fast, patients ingested 10 ml/kg body wt of water to achieve a hyperhydration state. After a 1-hour period of rest in a semirecumbent position, patients received a single intravenous dose of dDAVP (4 μg injected over 30 seconds) followed by a 2-hour continuous infusion of 4 μg of dDAVP in 50 ml of isotonic glucose solution (33 ng/min, 0.42 ml/min). Blood samples were taken before and at the end of the dDAVP infusion, for the measurement of plasma Na, K, creatinine, active renin, and aldosterone concentrations and plasma osmolality. BP was measured before and during the dDAVP infusion with an automated validated BP recorder (Press Mate BP 8800; Colin, Komaki-City, Japan). Urine samples were collected before dDAVP infusion (from 10:00 to 11:00 a.m.) and during the 2-hour dDAVP infusion (11:00 a.m. to 1:00 p.m.), for the measurement of urinary Na, K, and creatinine concentrations and osmolality. After each urine collection, water intake was matched to diuresis. Patients were discharged at the end of the dDAVP infusion and continued the same high Na/low K diet from day 4 to day 14. Amiloride (20 mg o.d.) was then orally administered for 1 week from day 7 to day 14 and was taken everyday in the unit.
On day 13, patients again completed a 24-hour urine collection. On day 14, they were given the last 20-mg amiloride dose at 7:00 a.m. after an overnight fast. At 9:00 a.m., they ingested 10 ml/kg body wt of water and underwent the second dDAVP test, as on day 4.
Laboratory Methods
Plasma and urine osmolality was measured by cryoscopy (Fiske Mark3 osmometer; Norwood, MA). The methods used for collecting blood samples and for quantifying plasma AVP (RIA), renin (immunoradiometric assay), and aldosterone (RIA) were those as described previously (15).
Calculations
Creatinine clearance (Ccreat), osmotic clearance (Cosm), and free water clearance (CH2O) were calculated as
and
where Pcreat and Ucreat are plasma and urinary concentrations of creatinine, respectively, Posm and Uosm are plasma and urinary osmolality, respectively, and V is urinary flow.
The transtubular potassium gradient (TTKG) was calculated as follows: TTKG = (UK × Posm)/(PK × Uosm), where PK and UK are the plasma and urinary concentrations of potassium, respectively (16).
Statistical Analyses
Data were analyzed using ANOVA for repeated measurements over time, taking into account amiloride administration, dDAVP infusion, and their interaction (amiloride × dDAVP) as the fixed effects and a modeling covariance structure within patients. Unadjusted pairwise comparisons between days (amiloride versus control period), and time points (before and after dDAVP), were done when the ANOVA was significant. A nonparametric Wilcoxon test was used for clearance parameters. Correlations between variables were estimated using analysis of covariance after withdrawal of the subject effect. Data are expressed as mean ± SD for normally distributed data, median [interquartile range, IQR], or geometric mean (95% confidence interval, CI) unless otherwise specified. Relative changes from baseline are expressed as the ratio of geometric means (95% CI). P < 0.05 was considered to be significant except for the interaction between dDAVP and amiloride effects that was considered significant for P < 0.10. SAS statistical software version 8.2 (Cary, NC) was used for statistical analyses.
Results
Effect of dDAVP Infusion Alone, on the Fourth Day of a High Na/Low K Diet
After 4 days on the high Na/low K diet, sodium and potassium balances were achieved, as reflected by the 24-hour urinary Na and K excretion rates (303 ± 50 and 56 ± 12 mmol/24 h, respectively). Plasma renin and aldosterone concentrations were low and plasma osmolality, plasma Na, plasma K, and creatinine values were within the physiologic range (Table 1).
Table 1.
Biochemical and hormonal changes in response to dDAVP administered alone (control period, day 4) or after 7-day pretreatment with amiloride (amiloride period, day 14) in 47 healthy patients on a high Na/low K diet
| Control Period (Day 4) | Amiloride (Day 14) | ||
|---|---|---|---|
| Plasma osmolality (mosmol/kg H2O) | Before dDAVP | 284 ± 4 | 283 ± 3 |
| After dDAVP | 285 ± 4 | 282 ± 4 | |
| Plasma sodium (mmol/L) | Before dDAVP | 139 ± 2 | 137 ± 2 |
| After dDAVP | 139 ± 3 | 137 ± 2 | |
| Plasma potassium (mmol/L) | Before dDAVP | 3.6 ± 0.2 | 4.1 ± 0.3 |
| After dDAVP | 3.6 ± 0.2 | 4.1 ± 0.3 | |
| Plasma creatinine (μmol/L) | Before dDAVP | 81 ± 10 | 81 ± 10 |
| After dDAVP | 81 ± 11 | 80 ± 10 | |
| Plasma active renin (pg/ml) | Before dDAVP | 13 (12, 15) | 43 (39, 48) |
| After dDAVP | 15 (14, 17)a | 51 (46, 57)a | |
| Plasma aldosterone (pg/ml) | Before dDAVP | 20 (16, 25) | 180 (159, 203) |
| After dDAVP | 16 (13, 19)a | 183 (165, 204) |
Data are mean ± SD or geometric mean (95% CI).
P < 0.001 after versus before dDAVP.
As expected, dDAVP led to a significant decrease in the urinary flow rate by 75% (95% CI: 68 to 81%, P < 0.0001 versus baseline; Table 2). Urine osmolality was low before dDAVP infusion because of the water load, and increased by 246% (199 to 301%, P < 0.0001 versus baseline; Table 2) at the end of the infusion. Free water clearance decreased by 4.4 ml/min (95% CI: 3.2 to 5.2 ml/min, P < 0.0001 versus baseline; Table 2), and osmotic clearance decreased by 0.8 ml/min (0.5 to 1.1 ml/min, P = 0.0004 versus baseline; Table 2).
Table 2.
Changes in urine in response to dDAVP in response to dDAVP administered alone (control period, day 4) or after 7-day pretreatment with amiloride (amiloride period, day 14) in 47 healthy subjects on a high Na/low K diet
| Control Period (Day 4) | Amiloride (Day 14) | ||
|---|---|---|---|
| Flow rate (ml/min) | Before dDAVP | 5.9 [4.1, 8.0] | 5.6 [3.9, 7.0] |
| After dDAVP | 1.2 [1.1, 1.6]b | 1.3 [1.0, 1.7]b | |
| Uosm (mosmol/kg H2O) | Before dDAVP | 137 [117, 211] | 165 [126, 222] |
| After dDAVP | 588 [487, 636]b | 630 [545, 723]b | |
| UcreatV (μmol/min) | Before dDAVP | 9.5 [8.0, 10.7] | 9.2 [7.7, 10.6] |
| After dDAVP | 12.1 [10.9, 14.0]b | 11.6 [10.7, 13.1]b | |
| UNaV (μmol/min) | Before dDAVP | 249 [186, 308] | 254 [194, 343] |
| After dDAVP | 193 [139, 236]a | 234 [190, 300] | |
| UKV (μmol/min) | Before dDAVP | 75 [62, 90] | 61 [46, 76] |
| After dDAVP | 70 [60, 87] | 53 [39, 75] | |
| UNa/UK (mmol/mmol) | Before dDAVP | 3.2 [2.7, 3.9] | 4.1 [3.3, 5.2] |
| After dDAVP | 2.5 [2.2, 3.2]b | 4.4 [3.3, 6.2] | |
| Ccreat (ml/min) | Before dDAVP | 118 [98, 138] | 113 [94, 134] |
| After dDAVP | 153 [138, 178]b | 144 [136, 165]b | |
| Cosm (ml/min) | Before dDAVP | 3.1 [2.5, 3.8] | 3.5 [2.6, 3.8] |
| After dDAVP | 2.6 [2.2, 3.0]b | 2.9 [2.6, 3.5]a | |
| CH2O (ml/min) | Before dDAVP | 3.0 [0.9, 4.4] | 2.4 [0.4, 3.3] |
| After dDAVP | −1.3 [−1.5, −1.0]b | −1.6 [−1.9, −1.2]b | |
| TTKG | Before dDAVP | 6.6 [5.3, 7.6] | 4.5 [3.7, 5.7] |
| After dDAVP | 7.8 [6.3, 8.9]b | 4.2 [3.4, 5.7] |
Uosm, urinary osmolality; UNaV, urinary sodium excretions; UKV, urinary potassium excretions; UcreatV, urinary creatinine excretions; Ccreat, creatinine clearances, Cosm, osmolar clearances; CH2O, free water clearances; TTKG, transtubular potassium gradient (see Materials and Methods section). Data are median [IQR].
P < 0.05 after versus before dDAVP.
P < 0.001 after versus before dDAVP.
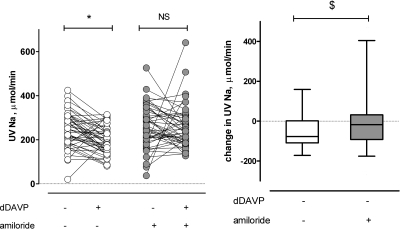
In addition to its effects on urinary flow rate and osmolality, dDAVP infusion was associated with a significant decrease in urine sodium excretion by 18.9% (4.5 to 31.1%, P = 0.0124; Table 2 and Figure 1) and a significant increase in creatinine clearance by 38 ml/min (31 to 48 ml/min, P < 0.0001; Table 2). At the end of the dDAVP infusion, there was a slight increase in the plasma renin concentration (Table 1), and a slight decrease in the plasma aldosterone concentration (Table 1) and in the systolic BP (−2.1 mmHg, 95% CI: −3.9 to −0.3, P = 0.0228, not shown). Changes in urine sodium excretion were correlated with changes in the urine flow rate (r = 0.62, n = 47, P < 0.0001), but not with changes in BP (not shown).
Figure 1.
Interaction between amiloride and the dDAVP effects on urinary sodium excretion. Forty-seven patients received twice a single intravenous dose of dDAVP (4 μg injected over 30 seconds) followed by a 2-hour continuous infusion of 4 μg of dDAVP in 50 ml isotonic saline solution alone (day 4) or after a 7-day administration of 20 mg o.d. amiloride (day 14). The left panel shows the individual UNaV. The box plot in right panel shows changes from baseline in UNaV (box, median and IQR; whiskers, 95% CI). UNaV, urine sodium excretion rate; *P < 0.05; $, significant interaction between amiloride and dDAVP effects (P < 0.10).
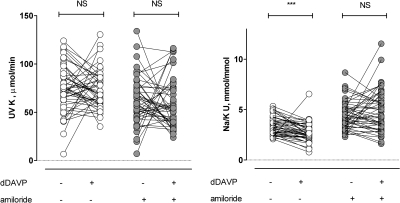
Despite the decrease in sodium and water excretion, potassium excretion remained unaffected (Table 2). The urinary Na/K ratio decreased by 18% (7 to 27%, P < 0.0001; Table 2 and Figure 2) and TTKG increased by +21% (9 to 34%, P = 0.0004; Table 2), suggesting that potassium secretion at the distal nephron was stimulated.
Figure 2.
Effect of dDAVP on urine potassium excretion rate (1) and (2) urinary Na/K ratio in the presence or absence of amiloride pretreatment (individual data of the 47 patients). ***P < 0.0001 dDAVP versus baseline.
Effect of dDAVP Infusion After a 7-Day Administration of 20 mg o.d. Amiloride (Day 14 of the High Na/Low K Diet)
The 7-day administration of amiloride led to a 1.6-kg (95% CI: 1.0 to 2.2 kg) decrease in body weight (P < 0.0001, day 14 versus day 4) and to a significant increase in plasma renin and aldosterone concentrations (Table 1), reflecting the net negative sodium balance. Twenty-four-hour Na and K excretion rates (246 ± 72 and 45 ± 16 mmol/24 h, respectively) matched Na and K intakes, suggesting that a new steady state was reached. Systolic/diastolic BP did not significantly change with amiloride (122 ± 10/66 ± 9 versus 120 ± 9/62 ± 7 mmHg, P = NS day 14 versus day 4). Amiloride increased the plasma potassium concentration by 0.50 mmol/L (0.40 to 0.59 mmol/L, P < 0.0001), reflecting its potassium sparing effect. The plasma sodium concentration was 2.2 mmol/L (1.5 to 2.9 mmol/L, P < 0.0001) lower, without any change either in plasma creatinine concentration or in osmolality (Table 1).
Amiloride pretreatment did not influence the dDAVP effects on urine flow rate, free water clearance, urinary osmolarity, and creatinine clearance (Table 2): dDAVP decreased urinary flow rate by 71% (63 to 77%, P < 0.0001 dDAVP versus baseline and P = 0.41 for amiloride × dDAVP interaction) and increased creatinine clearance by 35 ml/min (23 to 43 ml/min, P < 0.0001 versus baseline and P = 0.37 for amiloride × dDAVP interaction). These figures were similar to those observed on day 4.
In contrast, the antinatriuretic effect of dDAVP was almost abolished by amiloride pretreatment (Table 2 and Figure 1), as shown by the nonsignificant dDAVP-induced change in sodium excretion (+1%, 95% CI: −14.3 to +18.9%, P = 0.91 dDAVP versus baseline and P = 0.0626 for amiloride × dDAVP interaction). The dDAVP-induced decrease in osmolar clearance was significantly smaller than that on day 4 (−0.43 ml/min, 95% CI: −0.74 to −0.10 ml/min, P = 0.0268 dDAVP versus baseline and P = 0.0487 for amiloride × dDAVP interaction).
As on day 4, potassium excretion did not significantly change after dDAVP infusion (−4.2%, 95% CI: −20.5 to +15.5%, P = 0.65 dDAVP versus baseline and P = 0.57 for amiloride × dDAVP interaction; Table 2 and Figure 2). Amiloride prevented dDAVP effects on TTGK (−2.7%, 95% CI: −12.4 to +8.0%, P = 0.60 dDAVP versus baseline and P = 0.004 for amiloride × dDAVP interaction) and on urinary Na/K ratio (21%, 95% CI: −11 to +52%, P = 0.81 dDAVP versus baseline and P = 0.004 for amiloride × dDAVP interaction; Table 2 and Figure 2).
Finally, the plasma renin concentration increased slightly, as on day 4 (Table 1), but the plasma aldosterone concentration (Table 1) and systolic BP (−0.7 mmHg, 95% CI: −2.5 to 1.1 mmHg, P = 0.44, not shown) showed no change.
Discussion
We showed that the acute antinatriuretic effect of the V2R agonist dDAVP was fully prevented by a 7-day administration of 20 mg o.d. amiloride, a selective ENaC inhibitor. However, dDAVP-induced antidiuretic effects were maintained. We also showed that the stimulatory effect of dDAVP on distal potassium secretion in humans was amiloride sensitive. These data confirm the major physiologic role of ENaC in the V2R-mediated antinatriuretic effect of vasopressin in humans, a phenomenon currently described only in vitro.
We compared renal responses to dDAVP before and after a 7-day administration of a high dose of amiloride (20 mg o.d.). We selected this dose of amiloride because it was previously shown to be more potent than 100 mg of spironolactone, the mineralocorticoid receptor antagonist, for reversing hydrochlorothiazide-induced hypokalemia in healthy patients (17). We studied the effects of dDAVP on a high Na and low K diet, to suppress endogenous aldosterone secretion, the main stimulus of ENaC activity and expression, and induced water diuresis, before dDAVP infusion, to decrease endogenous vasopressin secretion. To minimize the hemodynamic effects of supraphysiologic doses of the V2R agonist, we selected lower doses of dDAVP than those previously used (7). Indeed, we observed only a small nonsignificant decrease in BP, a marginal increase in plasma renin concentrations without any change in the plasma aldosterone concentration.
Under these experimental conditions, infusion of dDAVP induced a marked decrease in urinary flow rate. This was associated with a decrease in urine sodium excretion in healthy patients, consistent with results obtained previously under different experimental conditions (7,18). The antinatriuretic effect of dDAVP was associated with a significant decrease in osmolar clearance. The magnitude of the decrease in sodium excretion in our study was smaller than those previously reported by Bankir et al. (−20% versus −60%, respectively) (7), probably because of the lower dose of dDAVP used in our study and/or of the initial washout of the medullary osmotic gradient due to the water load (19–21). In both studies, individual changes in the urine flow rate were significantly correlated with simultaneous individual changes in urine sodium excretion but not with those in BP, illustrating the dependence of the urinary flow rate on the change in “effective” solute excretion rates.
The decrease in the urinary sodium excretion rate with dDAVP alone occurred despite an increase in the filtered load of sodium, demonstrating that dDAVP has a potent stimulatory effect on renal tubular sodium reabsorption. Indeed, creatinine clearance, a GFR index, increased by approximately 30% after dDAVP infusion independently of amiloride administration. Although the mechanism of such V2R-induced rise in GFR has not yet been elucidated, a similar effect was previously reported in rats (19,22) as in water-loaded patients (5,23). Accordingly, GFR was shown to be significantly higher during low-hydration regimes than during high-hydration regimens in healthy patients (5). In the presence of amiloride, the dDAVP-induced increase in the filtered load of sodium without a change in sodium excretion suggests that sodium overload has been compensated in amiloride-insensitive segments. The mechanism of this adaptation is however beyond the scope of our study.
Amiloride pretreatment did not affect the antidiuretic effect of dDAVP (decrease in urinary flow rate) nor its antiaquaretic effect (decrease in water clearance), but fully prevented its antinatriuretic effect and blunted the decrease in osmolar clearance. This effect was independent of aldosterone that was suppressed by the high Na/low K diet. Altogether, these results suggest that dDAVP increases sodium reabsorption in a nephron segment that expresses V2R and is permeable to water in the presence of vasopressin, that is, in the CD, and are in agreement with the results of ex vivo/in vitro experiments (for review, see reference 11). Several studies have been published on vasopressin and its effects on tubular sodium reabsorption with conflicting results (3,4,7,11,24,25). Actually, vasopressin displays biphasic effects on sodium excretion in rats, resulting from a balance between the V2R-mediated antinatriuretic effect of lower concentrations and the V1aR-mediated natriuretic effect achieved at higher concentrations, which overrides the sustained action on V2R (6). Acute V2R activation stimulates the activity of ENaC in CD by inducing translocation of ENaC from intracellular storage vesicles to the apical membrane, by increasing its open probability, and by enhancing its stability, increasing in turn the number of functional ENaCs at that membrane (13,26). In addition, chronic treatment with dDAVP in rats also leads to a large increase in the expression of both the β- and γ-ENaC subunits in the kidney (for review, see references 11,27). This effect is different from that of aldosterone, which induces only a modest increase in α-ENaC and no change in β- and γ-ENaC expression (28). However, in addition to its effect on ENaC, acute administration of dDAVP has been shown in rats to induce translocation of the Na-K-2Cl cotransporter (NKCC2) to the apical membrane in the thick ascending limb via a V2R-mediated effect (29), whereas chronic administration of dDAVP to Brattleboro rats (genetically devoid of vasopressin) increased protein abundance of both the NKCC2 and the thiazide-sensitive NCC cotransporter (30). Moreover, if no stimulation of adenylate cyclase production by vasopressin in Thick Ascending Limb (TAL) was initially observed, suggesting no V2R expression in this segment in humans (31,32), a recent study demonstrated the presence of significant amounts of V2R mRNA and protein along the human nephron (from medullary TAL to CDs) (33). Altogether, these data suggest that transporters other than ENaC may also contribute to the V2R-mediated antinatriuresis in humans, but the importance of their contribution in vivo is not known. Nevertheless, our results suggest that the ENaC-dependent mechanisms may be predominant because the dDAVP-induced antinatriuretic effect was reversed by amiloride. However, as in all human studies, it is not possible to affirm that the amiloride-sensitive decrease in sodium excretion results from a direct action of vasopressin on ENaC activity or is a consequence of an indirect mechanism. Recent patch clamp studies on the luminal membrane of collecting duct principal cells in vitro bring support for a direct action of vasopressin on ENaC (14).
As in previous studies in humans (7), potassium excretion rate did not change with dDAVP infusion despite a marked decrease in the urinary flow rate and sodium excretion. This suggests that distal potassium excretion was maintained by compensatory mechanisms. Accordingly, two clinical indices of distal potassium secretion (TTKG and urinary Na/K ratio) were both significantly increased by dDAVP, confirming the known stimulatory effect of V2R agonists on distal potassium secretion (6,8,34). These effects were prevented by amiloride, suggesting the indirect involvement of an ENaC-dependent mechanism.
This study has some limitations including the use of an asymmetrical sequential design instead of a randomized crossover design and the absence of time control experiments before each dDAVP infusion due to blood volume constraints, time constraints, and cost limitations. The fact that each subject was studied twice and was its own control can partially compensate for this lack of control study. Despite these limitations, our study design allowed us to show neutralization by amiloride of the antinatriuretic effects of dDAVP, which was the primary objective of the study. Finally, we used dDAVP, a selective V2 agonist, and not the natural hormone AVP, which acts on several receptor subtypes. Indeed, it has been shown that V1aR-mediated effects may partially blunt the renal V2R-mediated effects of vasopressin in rats, however, only at higher concentrations of the hormone (6,27). Therefore, there is likely a certain range of vasopressin concentrations in which an antinatriuretic effect will occur along with the antidiuretic action of the hormone.
In conclusion, this study shows that, in addition to its well-known effect on water reabsorption, vasopressin significantly reduces urinary sodium excretion in humans by stimulating ENaC-mediated sodium reabsorption. It may thus be assumed that ENaC stimulation by vasopressin might induce, along with many other factors, some degree of sodium retention (27). The contribution of this effect to pathophysiologic variations in BP and to the pathophysiology of edematous states, in which vasopressin secretion can be significantly stimulated, remains to be addressed (27).
Disclosures
None.
Acknowledgments
This work was supported by the “Programme Hospitalier de Recherche Clinique from the Assistance Publique des Hôpitaux de Paris” (Grant: AOR0641). Dr. A. Blanchard is a recipient of a “Contrat d'Interface” grant from INSERM.
We thank the nursing staff of the Clinical Investigation Center who ran the protocol and Mrs. Christiane Dollin who performed the renin and the aldosterone measurements.
This work was previously reported in abstract form (Blanchard et al. J Hypertens 27: S374, 2009).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Access to UpToDate on-line is available for additional clinical information at www.cjasn.org.
References
- 1. Nielsen S, Kwon TH, Christensen BM, Promeneur D, Frokiaer J, Marples D: Physiology and pathophysiology of renal aquaporins. J Am Soc Nephrol 10: 647–663, 1999 [DOI] [PubMed] [Google Scholar]
- 2. Fenton RA, Knepper MA: Urea and renal function in the 21st century: Insights from knockout mice. J Am Soc Nephrol 18: 679–688, 2007 [DOI] [PubMed] [Google Scholar]
- 3. Balment RJ, Brimble MJ, Forsling ML, Musabayane CT: Natriuretic response of the rat to plasma concentrations of arginine vasopressin within the physiological range. J Physiol 352: 517–526, 1984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Leaf A, Bartter FC, Santos RF, Wrong O: Evidence in man that urinary electrolyte loss induced by pitressin is a function of water retention. J Clin Invest 32: 868–878, 1953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anastasio P, Cirillo M, Spitali L, Frangiosa A, Pollastro RM, De Santo NG: Level of hydration and renal function in healthy humans. Kidney Int 60: 748–756, 2001 [DOI] [PubMed] [Google Scholar]
- 6. Perucca J, Bichet DG, Bardoux P, Bouby N, Bankir L: Sodium excretion in response to vasopressin and selective vasopressin receptor antagonists. J Am Soc Nephrol 19: 1721–1731, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bankir L, Fernandes S, Bardoux P, Bouby N, Bichet DG: Vasopressin-V2 receptor stimulation reduces sodium excretion in healthy humans. J Am Soc Nephrol 16: 1920–1928, 2005 [DOI] [PubMed] [Google Scholar]
- 8. Tomita K, Pisano JJ, Knepper MA: Control of sodium and potassium transport in the cortical collecting duct of the rat. Effects of bradykinin, vasopressin, and deoxycorticosterone. J Clin Invest 76: 132–136, 1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nicco C, Wittner M, DiStefano A, Jounier S, Bankir L, Bouby N: Chronic exposure to vasopressin upregulates ENaC and sodium transport in the rat renal collecting duct and lung. Hypertension 38: 1143–1149, 2001 [DOI] [PubMed] [Google Scholar]
- 10. Morris RG, Schafer JA: cAMP increases density of ENaC subunits in the apical membrane of MDCK cells in direct proportion to amiloride-sensitive Na(+) transport. J Gen Physiol 120: 71–85, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schafer JA: Abnormal regulation of ENaC: Syndromes of salt retention and salt wasting by the collecting duct. Am J Physiol Renal Physiol 283: F221–F235, 2002 [DOI] [PubMed] [Google Scholar]
- 12. Sauter D, Fernandes S, Goncalves-Mendes N, Boulkroun S, Bankir L, Loffing J, Bouby N: Long-term effects of vasopressin on the subcellular localization of ENaC in the renal collecting system. Kidney Int 69: 1024–1032, 2006 [DOI] [PubMed] [Google Scholar]
- 13. Boulkroun S, Ruffieux-Daidie D, Vitagliano JJ, Poirot O, Charles RP, Lagnaz D, Firsov D, Kellenberger S, Staub O: Vasopressin-inducible ubiquitin-specific protease 10 increases ENaC cell surface expression by deubiquitylating and stabilizing sorting nexin 3. Am J Physiol Renal Physiol 295: F889–F900, 2008 [DOI] [PubMed] [Google Scholar]
- 14. Bugaj V, Pochynyuk O, Stockand JD: Activation of the epithelial Na+ channel in the collecting duct by vasopressin contributes to water reabsorption. Am J Physiol Renal Physiol 297: F1411–F1418, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Azizi M, Iturrioz X, Blanchard A, Peyrard S, De Mota N, Chartrel N, Vaudry H, Corvol P, Llorens-Cortes C: Reciprocal regulation of plasma apelin and vasopressin by osmotic stimuli. J Am Soc Nephrol 19: 1015–1024, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ethier JH, Kamel KS, Magner PO, Lemann J, Jr., Halperin ML: The transtubular potassium concentration in patients with hypokalemia and hyperkalemia. Am J Kidney Dis 15: 309–315, 1990 [DOI] [PubMed] [Google Scholar]
- 17. Murdoch DL, Forrest G, Davies DL, McInnes GT: A comparison of the potassium and magnesium-sparing properties of amiloride and spironolactone in diuretic-treated normal subjects. Br J Clin Pharmacol 35: 373–378, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Agnoli GC, Borgatti R, Cacciari M, Lenzi P, Marinelli M, Stipo L: Low-dose desmopressin infusion: Renal action in healthy women in moderate salt retention and depletion, and interactions with prostanoids. Prostaglandins Leukot Essent Fatty Acids 67: 263–273, 2002 [DOI] [PubMed] [Google Scholar]
- 19. Capasso G, Saviano C, Ciani F, Lang F, Russo F, De Santo NG: A decrease in renal medullary tonicity stimulates anion transport in Henle's loop of rat kidneys. Am J Physiol 274: F693–F699, 1998 [DOI] [PubMed] [Google Scholar]
- 20. De Wardener HE, Herxheimer A: The effect of a high water intake on the kidney's ability to concentrate the urine in man. 1957. J Am Soc Nephrol 11: 980–987, 2000 [DOI] [PubMed] [Google Scholar]
- 21. Gottschalk CW: Osmotic concentration and dilution of the urine. Am J Med 36: 670–685, 1964 [DOI] [PubMed] [Google Scholar]
- 22. Bouby N, Ahloulay M, Nsegbe E, Dechaux M, Schmitt F, Bankir L: Vasopressin increases glomerular filtration rate in conscious rats through its antidiuretic action. J Am Soc Nephrol 7: 842–851, 1996 [DOI] [PubMed] [Google Scholar]
- 23. Andersen LJ, Andersen JL, Schutten HJ, Warberg J, Bie P: Antidiuretic effect of subnormal levels of arginine vasopressin in normal humans. Am J Physiol 259: R53–R60, 1990 [DOI] [PubMed] [Google Scholar]
- 24. Humphreys MH, Friedler RM, Earley LE: Natriuresis produced by vasopressin or hemorrhage during water diuresis in the dog. Am J Physiol 219: 658–665, 1970 [DOI] [PubMed] [Google Scholar]
- 25. Kompanowska-Jezierska E, Emmeluth C, Grove L, Christensen P, Sadowski J, Bie P: Mechanism of vasopressin natriuresis in the dog: Role of vasopressin receptors and prostaglandins. Am J Physiol 274: R1619–R1625, 1998 [DOI] [PubMed] [Google Scholar]
- 26. Butterworth MB, Edinger RS, Frizzell RA, Johnson JP: Regulation of the epithelial sodium channel by membrane trafficking. Am J Physiol Renal Physiol 296: F10–F24, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bankir L, Bichet DG, Bouby N: Vasopressin V2 Receptors, ENaC and sodium reabsorption: A risk factor for hypertension? Am J Physiol Renal Physiol 299: F917–F28, 2010 [DOI] [PubMed] [Google Scholar]
- 28. Loffing J, Zecevic M, Feraille E, Kaissling B, Asher C, Rossier BC, Firestone GL, Pearce D, Verrey F: Aldosterone induces rapid apical translocation of ENaC in early portion of renal collecting system: Possible role of SGK. Am J Physiol Renal Physiol 280: F675–F682, 2001 [DOI] [PubMed] [Google Scholar]
- 29. Gimenez I, Forbush B: Short-term stimulation of the renal Na-K-Cl cotransporter (NKCC2) by vasopressin involves phosphorylation and membrane translocation of the protein. J Biol Chem 278: 26946–26951, 2003 [DOI] [PubMed] [Google Scholar]
- 30. Ecelbarger CA, Kim GH, Wade JB, Knepper MA: Regulation of the abundance of renal sodium transporters and channels by vasopressin. Exp Neurol 171: 227–234, 2001 [DOI] [PubMed] [Google Scholar]
- 31. Chabardes D, Gagnan-Brunette M, Imbert-Teboul M, Gontcharevskaia O, Montegut M, Clique A, Morel F: Adenylate cyclase responsiveness to hormones in various portions of the human nephron. J Clin Invest 65: 439–448, 1980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ruggles BT, Murayama N, Werness JL, Gapstur SM, Bentley MD, Dousa TP: The vasopressin-sensitive adenylate cyclase in collecting tubules and in thick ascending limb of Henle's loop of human and canine kidney. J Clin Endocrinol Metab 60: 914–921, 1985 [DOI] [PubMed] [Google Scholar]
- 33. Mutig K, Paliege A, Kahl T, Jons T, Muller-Esterl W, Bachmann S: Vasopressin V2 receptor expression along rat, mouse, and human renal epithelia with focus on TAL. Am J Physiol Renal Physiol 293: F1166–F1177, 2007 [DOI] [PubMed] [Google Scholar]
- 34. Giebisch G, Krapf R, Wagner C: Renal and extrarenal regulation of potassium. Kidney Int 72: 397–410, 2007 [DOI] [PubMed] [Google Scholar]