Abstract
Objective
To evaluate patterns of antipsychotic use.
Design, setting, and measurements
We used nationally representative data from the IMS Health National Disease and Therapeutic Index to describe outpatient antipsychotic use. The primary outcome was the volume of visits where antipsychotics were used for specific indications (treatment visits). We also quantified use without U.S. Food and Drug Administration approval (off-label use) and off-label use with compendium data suggesting an uncertain evidence base.
Results
Antipsychotic use increased from 6.2 million (M) treatment visits (95% CI, 5.4-7.0) in 1995 to 16.7M visits (15.5-18.2) in 2006, then declined to 14.3M visits (13.0-15.6) by 2008. A shift occurred from typical agents in 1995 (84% of all antipsychotic visits) to atypical agents by 2008 (93%). As they declined, typical medications shifted towards use in schizophrenia (30% in 1995 to 48% 2008). In contrast, use of atypical agents expanded for bipolar affective disorder (10% to 34%), remained stable for depression (12% to 14%), and declined for schizophrenia (56% to 23%). Overall, antipsychotic use for indications without FDA approval increased from 4.4M visits in 1995 to 9.0M in 2008. The estimated cost associated with off-label use in 2008 was US$6.0 billion.
Conclusions
Atypical use has grown far beyond substitution for the now infrequently used typical agents. Antipsychotics are increasingly used for conditions where FDA approval and associated clinical evidence is less certain. Despite the value of innovation, the benefits of widening atypical antipsychotic use should be weighed against their cost, regulatory status, and incomplete nature of available evidence.
BACKGROUND
With their availability a half-century ago, antipsychotic medications revolutionized the treatment of psychiatric disease. Over the last two-decades, first generation or “typical” agents introduced in the late 1950s and 1960s have largely been replaced by a second generation of “atypical” antipsychotics. Recently, considerable attention has focused on atypical antipsychotics due to their increasingly prevalent use and high cost (1), as well as concerns regarding their safety (2), comparative efficacy (3), and off-label use in the absence of strong evidence (4). Atypical antipsychotics accounted for more than $13 billion dollars in U.S. prescription drug costs in 2007, nearly 5% of all U.S. drug expenditures (5). Among them, quetiapine, aripiprazole, olanzapine, and risperidone, each had annual U.S. sales exceeding $1 billion (6,7).
The shift towards atypical use has been partly driven by their lower risk of extrapyramidal (motor) adverse effects compared to typicals. As long-term experience has accrued, however, serious and distinct adverse effects of atypicals have emerged. Atypical antipsychotics cause weight gain and lead to a higher risk of diabetes and other metabolic sequelae than their typical counterparts (8). Compared to nonusers, there is an increased risk of mortality and cardiovascular events in elderly patients with dementia on atypicals (9). In addition, current comparative evidence suggests no definitive differences in efficacy or net adverse effect profiles between these two drug classes (10). Although approved initially for schizophrenia, antipsychotic medications also are used for numerous other conditions, including other psychoses, bipolar disorder, delirium, depression, personality disorders, dementia, and autism (11,12). While some atypical drugs have received FDA approval for limited aspects of these conditions, the evidence base for many off-label uses remains less certain than for those drugs with regulatory approval.
We examined long-term U.S. trends in physician use and costs of antipsychotics with focus on the clinical divergence of typical and atypical medications over the past fifteen years. Using nationally representative data on office-based visits from 1995 through 2008, we tested the hypothesis that with the shift to atypical agents, costly antipsychotic use is increasingly occurring in clinical situations lacking FDA approval and where evidence is less certain.
METHODS
Data source
We used physician survey data from the IMS Health National Diagnostic and Therapeutic Index (13) (NDTI). NDTI selects a random sample of office-based, patient-care physicians through stratified sampling by specialty and geographic region. Approximately 4,800 physicians participate each calendar quarter and each physician is randomly assigned two consecutive workdays per quarter for data collection. For each encounter, physicians complete an encounter form that captures a listing of the patients’ diagnoses and, for each diagnosis, a listing of associated medications that are newly prescribed or to be continued at the visit's conclusion. Although the majority of encounters take place in the outpatient office setting, the NDTI also captures phone-based encounters and those taking place in long-term care institutions (approximately 3-5% of encounters) or hospitals (approximately 10%).
Trends in antipsychotic medication use
We queried these data for patient visits where a typical or atypical antipsychotic drug was reported (referred to as a treatment visit). We report national estimates that were extrapolated from the sample data for visits by patients of all ages. For each estimate, 95% confidence intervals (CI) were available via estimates of the relative standard error. Analyses comparing NDTI with the U.S. National Center for Health Statistics’ National Ambulatory Care Medical Survey (NAMCS) suggest consistency in assessing patterns of outpatient care (14,15).
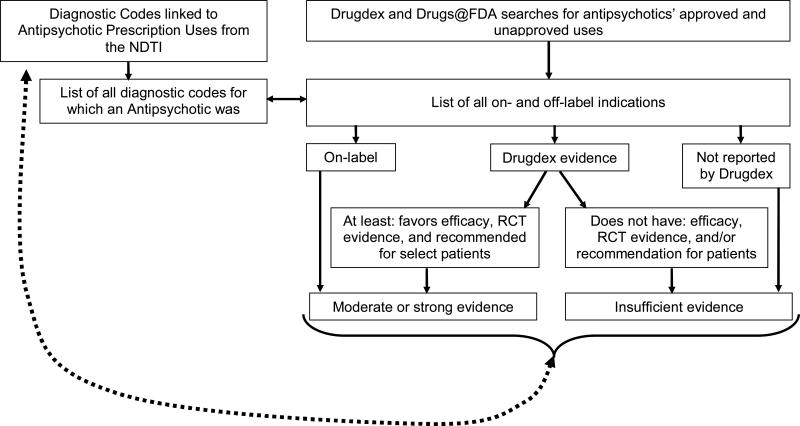
Classifying prescription use based on FDA labeling and available evidence
Based on the physician-reported diagnostic codes associated with each antipsychotic medication treatment visit, we searched the FDA website (16) to determine whether the reported indication had obtained FDA approval. We conservatively defined off-label use as lack of FDA approval through 2008, even when assessing use in earlier years. For these off-label indications, we used a widely referenced drug compendium, Drugdex® (12), to obtain summary information on the evidence base supporting each indication. We analyzed evidence at a drug, rather than class, level. We did so both because of the difficulty defining class effects for the chemically and clinically heterogeneous antipsychotics (17,18), and because the FDA approaches drug approval at the level of individual drugs. We characterized the evidence base for an off-label use as either “moderate or strong” or “uncertain.” “Moderate or strong” includes only those indications where Drugdex efficacy was “effective” or “favors efficacy,” the strength of evidence rating indicated RCT-derived evidence (“A” or “B”), and the strength of recommendation rating was “recommended,” “recommended for most patients,” or “recommended for some patients.” All indications not meeting these criteria were classified as having uncertain evidence.
Prescription expenditures
We obtained information on prescription expenditures from IMS Health National Sales Perspective and the IMS National Prescription Audit. We derived information on the mean price per day of therapy, as well as aggregate annual expenditures. These costs reflect funds paid for prescriptions by both health insurance and the patient.
Role of the funding source and institutional review
The study was supported by awards from the U.S. Agency for Healthcare Research and Quality, the Robert Wood Johnson Foundation, and the National Heart, Lung and Blood Institute, while the data were obtained under licensed agreement with IMS Health. These sources of funding and data had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript for publication. The study was determined to be exempt from Institutional Review Board review at the University of Chicago.
RESULTS
Overall trends for typical and atypical use
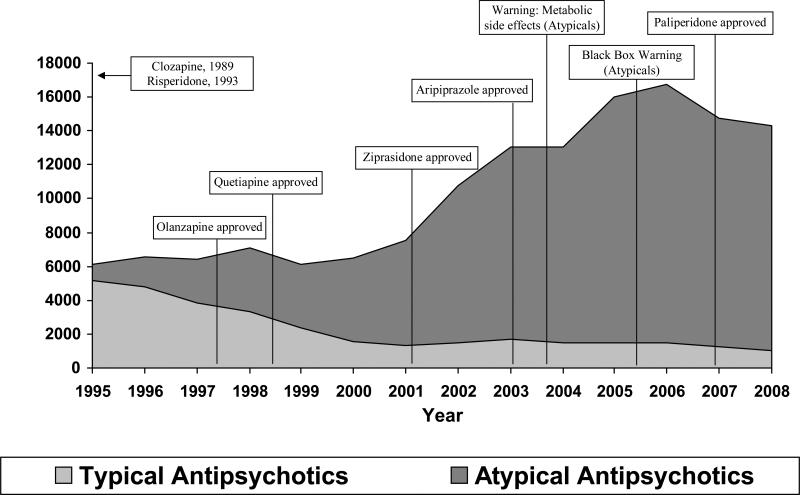
Annual antipsychotic treatment visits nearly tripled from 6.2 million (M) treatment visits (95% confidence interval, 5.4-7.0) in 1995 to 16.7 M (15.5-18.2) in 2006, but then declined to 14.3 M (13.0-15.6) by 2008. Typical antipsychotics decreased from 5.2 M (4.5-5.9) visits in 1995 to 1.0 M (0.8-1.3) visits in 2008, while atypical antipsychotics increased from 1.0 M (0.8-1.2) to 13.3 M (12.0-14.5) visits. This shift from typical agents (84% of antipsychotics in 1995) to atypical agents (93% in 2008) occurred in two phases (Figure 1). First, from 1995 through 2001, atypical antipsychotics increased primarily as they substituted for typical agents without change in the overall volume of antipsychotic use. Second, from 2002 through 2006, atypical antipsychotic prescribing increased more substantially, with only modest further reductions in the use of typical agents. More recently, there have been declines in the use of both typical and atypical antipsychotics.
APPENDIX FIGURE 1.
ASSESSMENT OF SCIENTIFIC SUPPORT FOR EACH DRUG-USE COMBINATION.
Most common antipsychotic medications
In 1995, the most commonly reported antipsychotic medications were the typical agents haloperidol (1.2 M treatment visits), thioridazine (1.0 M), and perphenazine (0.8 M). The two available atypical antipsychotics in 1995 were clozapine (0.2 M) and risperidone (0.8 M). In 2008, the most commonly reported atypical agents were quetiapine (16.7 M) risperidone (12.0 M), aripiprazole (6.7 M) and olanzapine (6.2 M). Among typical agents, haloperidol was most widely used (2.5 M, Table 1).
TABLE 1.
ANTIPSYCHOTIC MEDICATIONS BY TREATMENT SUBCLASS.*
| Total prescriptions 2008 (M) | 95% confidence intervals (M) | Cost per prescription 2008 ($) | Generic available | FDA approval date | |
|---|---|---|---|---|---|
| Typical antipsychotics | |||||
| Perphenazine (Trilafon®) | 0.80 | 0.6-1.0 | 12 | Yes | 02/57 |
| Chlorpromazine (Thorazine®) | 0.62 | 0.4-0.8 | 9 | Yes | 10/57 |
| Trifluoperazine (Stelazine®) | 0.26 | 0.2-0.4 | 26 | Yes | 04/59 |
| Fluphenazine (Permitil®) | 0.64 | 0.5-0.8 | 9 | Yes | 09/59 |
| Thioridazine (Mellaril®) | 0.35 | 0.2-0.5 | 11 | Yes | 03/62 |
| Haloperidol (Haldol®) | 2.48 | 2.1-2.9 | 13 | Yes | 04/67 |
| Thiothixene (Navane®) | 0.31 | 0.2-0.4 | 12 | Yes | 07/67 |
| Molindone (Moban®) | - | - | - | Yes | 01/74 |
| Loxapine (Loxitane®) | - | - | - | Yes | 02/75 |
| Atypical antipsychotics | |||||
| Clozapine (Clozaril®) | 1.56 | 1.2-1.9 | 85 | Yes | 09/89 |
| Risperidone (Risperdal®) | 12.02 | 10.8-13.2 | 200 | Yes | 12/93 |
| Olanzapine (Zyprexa®) | 6.15 | 5.4-6.9 | 406 | No | 09/96 |
| Quetiapine (Seroquel®) | 16.67 | 15.2-18.1 | 227 | No | 09/97 |
| Ziprasidone (Geodon®) | 2.96 | 2.5-3.4 | 308 | No | 02/01 |
| Aripiprazole (Abilify®) | 6.66 | 5.8-7.5 | 421 | No | 11/02 |
| Paliperidone (Invega®) | 0.78 | 0.6-1.0 | 345 | No | 12/06 |
Name represents original brand name first approved by the FDA, which may differ from current most frequently reported drug name (generic or brand); missing values denote products with minimal usage in 2008; analyses excluded Symbyax; values for total prescriptions derived from the IMS Health National Disease and Therapeutic Index™, 2008; values for total prescriptions and cost per prescription derived from the IMS Health National Prescription Audit™
Relative growth among children, non-elderly adults, and the elderly
Patterns of increasing antipsychotic use varied by patient age. The largest changes occurred among adults, ages 18-64 years old. In this age group, antipsychotic use (atypical and typical) was stable between 1995 (4.1 M treatment visits, 95% confidence intervals [CI], 3.5-4.7) and 2001 (5.1 M treatment visits, CI 4.4-5.8) and then increased markedly to 11.9 (CI 10.7-13.1 M treatment visits by 2006. Similarly, the number of treatment visits among those 65 years and older were constant between 1995 (1.4 M visits, CI 1.1-1.7) and 2000 (1.3 M visits, CI 1.0-1.6) after which they increased to a maximum of 2.2 M (CI, 1.8-2.6) in 2003 with modest decline to 1.6 M, CI 1.2-2.0 by 2008. The number of treatment visits among children increased eight-fold from 1995 (0.3 M CI 0.2-0.4) to 2005 (2.4 M CI 2.0-2.8).
Changes in clinical uses of typical and atypical antipsychotics
A substantial shift occurred in the clinical uses of antipsychotics between 1995 and 2008 (Table 2). The fraction of all typical antipsychotic used for patients with schizophrenia increased from 32% of typical treatment visits in 1995 to 53% in 2007 and decreased to 48% in 2008. In contrast, for schizophrenia declined from 56% of all atypical agent treatment visits in 1995 to 23% in 2008, while there was a substantial increase in use for bipolar affective disorder (10% to 34%). Atypical antipsychotic use for depression increased from 12% of all atypical treatment visits in 1995 to 18% in 2003 and then dropped to 14% of uses by 2008. The proportion of atypical use for other disorders (e.g., dementia, anxiety disorders) was stable during this period.
TABLE 2.
TYPICAL AND ATYPICAL ANTIPSYCHOTIC USE STRATIFIED BY CLINICAL INDICATION.*
| 1995-1996 | 1997-1998 | 1999-2000 | 2001-2002 | 2003-2004 | 2005-2006 | 2007-2008 | |
|---|---|---|---|---|---|---|---|
| TYPICAL ANTIPSYCHOTICS | |||||||
| Schizophrenia, % | 32 | 36 | 39 | 45 | 48 | 50 | 51 |
| Bipolar affective disorder, % | 12 | 11 | 11 | 13 | 13 | 18 | 17 |
| Depression/Reaction, % | 16 | 14 | 14 | 14 | 12 | 7 | 7 |
| Anxiety, % | 4 | 5 | 3 | 3 | 4 | 3 | 3 |
| ADHD/Conduct, % | 2 | 2 | 2 | 2 | 1 | 1 | 1 |
| Dementia, % | 8 | 6 | 6 | 4 | 4 | 2 | 4 |
| Other psychosis, % | 9 | 11 | 10 | 8 | 9 | 9 | 4 |
| All others, % | 17 | 15 | 15 | 11 | 9 | 10 | 12 |
| Total visits (thousands) | 9,992 | 7,107 | 3,941 | 2,781 | 3,110 | 2,916 | 2,253 |
| ATYPICAL | |||||||
| Schizophrenia, % | 51 | 37 | 32 | 29 | 24 | 24 | 24 |
| Bipolar affective disorder, % | 11 | 16 | 18 | 21 | 24 | 30 | 34 |
| Depression/Reaction, % | 15 | 13 | 18 | 18 | 17 | 15 | 14 |
| Anxiety, % | 3 | 4 | 4 | 5 | 6 | 5 | 4 |
| ADHD/Conduct, % | 2 | 2 | 3 | 3 | 5 | 5 | 5 |
| Dementia, % | 5 | 7 | 7 | 7 | 7 | 4 | 3 |
| Other psychosis, % | 8 | 13 | 11 | 11 | 10 | 10 | 9 |
| All others, % | 7 | 8 | 7 | 7 | 8 | 7 | 7 |
| Total visits (thousands) | 2,699 | 6,383 | 8,723 | 15,560 | 22,987 | 29,846 | 26,801 |
Source: IMS Health National Disease and Therapeutic Index™, 1995-2008
Changes in Off-label Use
In 1995, 74% of all antipsychotic treatment visits (or 4.4 M visits) were for conditions that were not approved by the FDA by 2008. By 2008, 60% (or 9.0 M visits) were off-label. For atypical antipsychotics, off-label uses increased from 50% in 1995 to 66% in 2003, before declining to 60% in 2008. For typical agents, off-label use declined from 78% in 1995 to 67% in 2008.
Exploratory analyses of use by levels of evidence
Among the 4.4 M antipsychotic off label uses in 1995, 4.2 M (97%) had a compendium summary suggesting an uncertain evidence base. In 2002, among the 6.8 M off-label use visits, 5.5 M (81%) had uncertain evidence. By 2008, 8.2 M (91%) of the 9.0 M off-label visits had uncertain evidence. Among atypical agents, off-label use with uncertain evidence increased from 0.44 M visits (45% of atypical off-label use) in 1995 to 6.9 M visits (54% of atypical off-label use) in 2008. Among typical antipsychotics, 3.6 M visits (76% of typical off-label uses) in 1995 were with uncertain evidence, compared to 0.8 M visits (65% of typical off-label uses) in 2008. The majority of increases in off-label use were due to increasing use among adults younger than 65 years for indications with uncertain evidence, rather than among children or the elderly.
Antipsychotic medication costs
From 2004 to 2008, the mean cost of typical antipsychotic prescription increased 8% from $38 to $41, while the cost of an atypical prescription increased by 43% from $226 to $323. In 2008, US$0.06 billion was spent on typical agents and $9.9 billion spent on atypical agents in the United States. Given these costs, we estimate that in 2008 $6.0 billion was expended on off-label use of antipsychotic medications, of which $5.4 billion was for uses with uncertain evidence.
DISCUSSION
From 1995 to 2008, there was a pronounced shift in the use of atypical antipsychotic drugs. Based on nationally representative serial, cross-sectional data from U.S. outpatient physician practices, we found a 45% decrease in the proportion of use for schizophrenia, for which most drugs were initially labeled, and a nearly seven-fold increase in use for bipolar affective disorder, representing a third of all uses with atypical agents in 2008. Rates of atypical use for depression did not change substantially over the period examined. Significant divergence in the application of typical and atypical agents was evident, with the small residual use of typical agents concentrated in prescribing for schizophrenia.
Antipsychotic medications are one of the most common and costly classes of prescription drugs in the U.S. While their increasing use has been widely reported, far less is known regarding the evolution of their clinical uses. While others have noted the shift towards antipsychotic use for mood disorders (19,20), our report reinforces the magnitude of this shift using with national U.S. data collected over an extended observation period with clinician-reported diagnoses.
Previous studies have demonstrated a substantial replacement of typical antipsychotics with their newer counterparts following the market release of the first atypical agent in 1989. This increase has occurred despite a lack of definitive advantages of the atypical agents over their typical predecessors in their efficacy and adverse effect profiles. Recent trials (22,23) failing to demonstrate clinically significant differences in the effectiveness of these two classes in schizophrenia raise the question of whether typical antipsychotics should be reconsidered as a first line therapy, given that the superiority of atypical agents has yet to be established. Such a shift in practice, however, is unlikely given the potency of a variety of non-clinical factors that shape prescribing, including clinical inertia and the continued marketing of atypical agents. This is especially important given the small share of all antipsychotic use accounted for by typical agents, as well as the divergence in the use of typical and atypical antipsychotic medications.
Prescription drugs vary in their clinical and biochemical innovation, and in many cases important discoveries regarding therapies are made only after market release, often to treat conditions distinct from those initially targeted. The effectiveness of selective serotonin reuptake inhibitors (SSRIs) to treat anxiety, and the use of angiotensin converting enzyme-inhibitors (ACE inhibitors) in congestive heart failure, are but two examples where drugs approved for one use were subsequently found to have other important clinical applications. Although typical and atypical antipsychotics were not initially developed for use in bipolar affective disorder, subsequent evidence suggests their efficacy in treating mania associated with this disease (24). While increasing antipsychotic use since 1995 reflects clinical innovation and other factors, it has led to clinical use where regulatory scrutiny has not occurred and where the supporting evidence is less certain.
Innovation in clinical practice necessarily involves the use of therapies that are not well studied. When the application of therapies for new and largely untested clinical indications reaches a substantial volume, however, there should be a corresponding obligation to generate evidence that demonstrates the safety and efficacy of the new uses. This is especially important in clinical settings where alternatives to the innovative therapies are already available, as with mood stabilizers (e.g., divalproex) for bipolar affective disorder and antidepressants (e.g., selective serotonin reuptake inhibitors) for the treatment of depression. Further scrutiny of widespread psychotropic medication use for scientifically unsupported off-label indications is needed, especially among those patient subpopulations and clinical applications where such uses are most common.
Our study has several important limitations. First, because the NDTI is a visit-based sample of outpatient office practices, it oversamples those with greater comorbid illness compared with population-based samples. Nevertheless, visit-based samples are commonly used for this type of analysis, and the NDTI provides data congruent with the National Ambulatory Medical Care Survey conducted by the U.S. government (14,15). Second, as with many other data sources, NDTI lacks information that would be useful in understanding the choice of off-label use, such as data regarding patient non-response to FDA approved therapies and detailed comorbid histories. Third, since there is no single source that includes summary information on drug safety and effectiveness, drug compendia vary in their assessments of the levels of evidence supporting different clinical applications (25). Despite its limitations, Drugdex® serves as a key source of information that is updated regularly, commonly used in clinical practice, and recognized in U.S. reimbursement regulations, including Medicaid evaluation of coverage for off-label uses (26). As with any method of determining levels of evidence, our estimates are subject to imprecision due to these limitations of drug compendium data and NDTI's sparse clinical detail. Even if significant misclassification were to have occurred, however, our results would still suggest a substantial exposure to therapies for clinical indications that have not received regulatory scrutiny and where the evidence base is uncertain. If only 30% of all atypical uses in 2008 were to have uncertain evidence (a conservative estimate compared with our derived estimate of 54%), this would translate into an estimated 3.8 M prescriptions at a cost of $3.0 billion.
Antipsychotic medications have important known benefits and risks. Our data suggest substantial growth of atypical antipsychotics beyond their substitution for older, typical antipsychotics. Patterns of clinical use have diverged for typical and atypical agents. The use of typical agents has declined, but continues predominantly for schizophrenia. In contrast, atypical agent use has dramatically increased, both substituting for typical agents and expanding into new indications, such as bipolar disorder and depression. Despite the value of innovation, expansion of clinical practice beyond FDA approved indications raises significant concerns. Further expansion of atypical antipsychotics should be approached with caution while awaiting new evidence evaluating their comparative benefits. This information is important not only for non-elderly adults who comprise the majority of atypical use, but also for children and the elderly, vulnerable populations where increasing rates of atypical use are also noted.
FIGURE 2.
AGGREGATE USE OF TYPICAL AND ATYPICAL ANTIPSYCHOTICS, 1995-2008.*
*Source: IMS Health National Disease and Therapeutic Index™, 1995-2008
TABLE 3.
ATYPICAL ANTIPSYCHOTIC USE STRATIFIED BY AGE AND FDA LABEL STATUS.*
| 1995-1996 | 1997-1998 | 1999-2000 | 2001-2002 | 2003-2004 | 2005-2006 | 2007-2008 | |
|---|---|---|---|---|---|---|---|
| Younger than 18 years | |||||||
| On-label, % | 12 | 12 | 21 | 23 | 24 | 26 | 24 |
| Off-label, moderate or good evidence, % | 33 | 27 | 24 | 18 | 12 | 8 | 9 |
| Off-label, uncertain evidence, % | 55 | 61 | 55 | 58 | 64 | 66 | 67 |
| Total for younger than 18, N (thousands) | 120 | 472 | 977 | 1774 | 3518 | 4520 | 4216 |
| | |||||||
| 18 to 64 years | |||||||
| On-label, % | 53 | 47 | 44 | 42 | 42 | 41 | 46 |
| Off-label, moderate or good evidence, % | 2 | 7 | 9 | 10 | 6 | 5 | 4 |
| Off-label, uncertain evidence, % | 44 | 46 | 47 | 47 | 52 | 55 | 50 |
| Total for 18-64, N (thousands) | 2099 | 4553 | 5787 | 10422 | 15053 | 20569 | 18634 |
| | |||||||
| 65 years and older | |||||||
| On-label, % | 18 | 17 | 15 | 16 | 15 | 21 | 25 |
| Off-label, moderate or good evidence, % | 1 | 20 | 22 | 26 | 20 | 17 | 12 |
| Off-label, uncertain evidence, % | 80 | 63 | 62 | 57 | 65 | 63 | 63 |
| Total for 65 and older, N (thousands) | 358 | 1116 | 1689 | 2849 | 3517 | 3543 | 2989 |
| | |||||||
| All ATYPICAL visits | |||||||
| On-label, % | 47 | 39 | 35 | 35 | 35 | 36 | 40 |
| Off-label, moderate or good evidence, % | 4 | 10 | 13 | 14 | 9 | 7 | 6 |
| Off-label, uncertain evidence, % | 50 | 51 | 51 | 51 | 56 | 57 | 54 |
| Total visits, N (thousands) | 2577 | 6141 | 8453 | 15045 | 22088 | 28632 | 25839 |
Values and column percents exclude the approximate 1%-2% of subjects whose age was not specified; Source: IMS National Disease and Therapeutic Index™, 1995-2008 and DrugDex™
TABLE 4.
TYPICAL ANTIPSYCHOTIC USE STRATIFIED BY AGE AND FDA LABEL STATUS.*
| 1995-1996 | 1997-1998 | 1999-2000 | 2001-2002 | 2003-2004 | 2005-2006 | 2007-2008 | |
|---|---|---|---|---|---|---|---|
| Younger than 18 years | |||||||
| On-label, % | 14 | 15 | 16 | 9 | 44 | 55 | 45 |
| Off-label, moderate or good evidence, % | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Off label, uncertain evidence, % | 85 | 85 | 84 | 91 | 56 | 45 | 55 |
| Total for younger than 18, N (thousands) | 608 | 441 | 232 | 81 | 77 | 67 | 31 |
| | |||||||
| 18 to 64 years | |||||||
| On-label, % | 26 | 28 | 32 | 34 | 38 | 41 | 38 |
| Off-label, moderate or good evidence, % | 2 | 1 | 1 | 1 | 1 | 1 | 2 |
| Off-label, uncertain evidence, % | 73 | 71 | 67 | 66 | 61 | 58 | 61 |
| Total for 18-64, N (thousands) | 6543 | 4996 | 2601 | 2055 | 2300 | 2227 | 1675 |
| | |||||||
| 65 years and older | |||||||
| On-label, % | 12 | 17 | 22 | 21 | 28 | 36 | 32 |
| Off-label, moderate or good evidence, % | 2 | 3 | 3 | 1 | 2 | 2 | 1 |
| Off-label, uncertain evidence, % | 86 | 80 | 75 | 79 | 69 | 62 | 67 |
| Total for 65 and older, N (thousands) | 2493 | 1472 | 938 | 565 | 641 | 495 | 486 |
| | |||||||
| All TYPICAL visits | |||||||
| On-label, % | 21 | 25 | 29 | 30 | 36 | 40 | 36 |
| Off-label, moderate or good evidence, % | 2 | 1 | 1 | 1 | 1 | 1 | 2 |
| Off-label, uncertain evidence, % | 77 | 73 | 70 | 69 | 63 | 58 | 62 |
| Total visits, N (thousands) | 9644 | 6909 | 3771 | 2701 | 3018 | 2789 | 2192 |
Values and column percents exclude the approximate 1%-2% of subjects whose age was not specified; Source: IMS National Disease and Therapeutic Index™, 1995-2008 and DrugDex™
Acknowledgements
The authors gratefully acknowledge analytic assistance from Shu Zhu, MPH, in preparing the manuscript. The statements, findings, conclusions, views, and opinions contained and expressed in this article are based in part on data obtained under license from the following IMS Health Incorporated information service(s): National Disease and Therapeutic Index™ (1995-2008); Integrated Promotional Services™ (2001-2008), National Prescription Audit™ (2001-2008), IMS Health Incorporated. All Rights Reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IMS Health Incorporated or any of its affiliated or subsidiary entities.
Funding
Dr. Alexander has career development awards from the Agency for Healthcare Research and Quality (K08 HS15699; RO1 HS0189960) and the Robert Wood Johnson Physician Faculty Scholars Program. Dr. Stafford has a mid-career development award from the National Heart, Lung and Blood Institute (K24 HL086703). The funding sources had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript for publication.
Footnotes
Disclosures
Dr. Alexander is a consultant for IMS Health.
REFERENCES
- 1.Prescription Drug Trends [February 3, 2009];The Kaiser Family Foundation, 2007. 2007 Available at: http://www.kff.org/rxdrugs/upload/3057_06.pdf.
- 2.Ray WA, Chung CP, Murray KT, et al. Atypical antipsychotic drugs and the risk of sudden cardiac death. New England Journal of Medicine. 2009;360:225–235. doi: 10.1056/NEJMoa0806994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McDonagh MS, Peterson K, Carson S, Chan B, Thakurta S. Drug class review on atypical antipsychotic drugs. [March 24, 2010];Update #2 final report. http://www.ohsu.edu/drugeffectiveness/reports/final.cfm. [PubMed]
- 4.Briesacher BA, Limcangco MR, Simoni-Wastila L, et al. The quality of antipsychotic prescribing in nursing homes. Archives of Internal Medicine. 2005;165:1280–1285. doi: 10.1001/archinte.165.11.1280. [DOI] [PubMed] [Google Scholar]
- 5.Zuvekas SH. Prescription drugs and the changing patterns of treatment for mental disorders, 1996-2001. Health Affairs. 2005;24:195–205. doi: 10.1377/hlthaff.24.1.195. [DOI] [PubMed] [Google Scholar]
- 6.Lamb E. Top 200 Prescription Drugs of 2007. [March 24, 2010];Pharmacy Times. 2008 May; Available at: http://www.pharmacytimes.com/issues/articles/2008-05_003.asp.
- 7. [10/20/2009];Drug Topics, 2009; 153: Online Edition. 2009 May 26; Available at: http://drugtopics.modernmedicine.com/drugtopics/data/articlestandard//drugtopics/222009/599845/article.pdf.
- 8.Smith M, Hopkins D, et al. First- v. second-generation antipsychotics and risk for diabetes in schizophrenia: systematic review and meta-analysis. The British Journal of Psychiatry. 2008;192:406–411. doi: 10.1192/bjp.bp.107.037184. [DOI] [PubMed] [Google Scholar]
- 9.Gill SS, Bronskill SE, Normand ST, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med. 2007;146:775–786. doi: 10.7326/0003-4819-146-11-200706050-00006. [DOI] [PubMed] [Google Scholar]
- 10.Shekelle P, Maglione M, Bagley S, et al. Comparative effectiveness of off-label use of atypical antipsychotics: comparative effectiveness review no 6. Prepared by the Southern California/RAND Evidence-based Practice Center under contract no 290-02-0003. Agency for Healthcare Research and Quality; Rockville, Md: Jan, 2007. [March 24, 2010]. Available at www.effectivehealthcare.ahrq.gov/reports/final.cfm. [PubMed] [Google Scholar]
- 11.Domino ME, Swartz MS. Who are the new users of antipsychotic medications? Psychiatric Services. 2007;59:507–514. doi: 10.1176/appi.ps.59.5.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomson Micromedex. Greenwood Village, Colorado: [Google Scholar]
- 13.IMS Health National Disease and Therapeutic Index, Plymouth Meeting; Pennsylvania. [Google Scholar]
- 14.Stafford RS, Radley DC. The underutilization of cardiacmedications of proven benefit, 1990 to 2002. Journal of the American College of Cardiology. 2003;41:56–61. doi: 10.1016/s0735-1097(02)02670-0. [DOI] [PubMed] [Google Scholar]
- 15.Zell ER, McCaig LF, Kupronis BA, Besser RE, Schuchat A. Proceedings of the section on survey research methods, American Statistical Association. American Statistical Association; Alexandria, VA: 2000. A comparison of the national disease and therapeutic index and the national ambulatory medical care survey to evaluate antibiotic usage. pp. 840–5. [Google Scholar]
- 16.Drugs@FDA [Nov. 15, 2007]; Available at: http://www.accessdata.fda.gov/Scripts/cder/DrugsatFDA/index.cfm.
- 17.Furberg CD, Herrington DM, Psaty BM. Are drugs within a class interchangeable? Lancet. 1999;354:1202–1204. doi: 10.1016/S0140-6736(99)03190-6. [DOI] [PubMed] [Google Scholar]
- 18.Rummel-Kluge CK, Komossa K, Schwartz S, et al. Second-Generation Antipsychotic Drugs and Extrapyramidal Side Effects: A Systematic Review and Meta-analysis of Head-to-Head Comparisons. Schizophrenia Bulletin. 2010 doi: 10.1093/schbul/sbq042. Advanced access published May 31, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ray WA, Chung CP, Murray KT, Hall K, Stein CM. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med. 2009;360:225–235. doi: 10.1056/NEJMoa0806994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crystal S, Olfson M, Huang C, Pincus H, Gerhard T. Broadened use of atypical antipsychotics: safety, effectiveness, and policy challenges. Health Aff. 2009;28:w770–w781. doi: 10.1377/hlthaff.28.5.w770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morena C, Laje G, Blanco C, Jiang H, Schmidt AB, Olfson M. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psych. 2007;64:1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- 22.McEvoy JP, Lieberman JA, Stroup TS, Davis SM, Meltzer HY, Rosenheck RA, Swartz MS, Perkins DO, Keefe RSE, Davis CE, Severe J, Hsiao JK, the CATIE Investigators Effectiveness of Clozapine Versus Olanzapine, Quetiapine, and Risperidone in Patients With Chronic Schizophrenia Who Did Not Respond to Prior Atypical Antipsychotic Treatment. Am J Psychiatry. 2006;163:600–610. doi: 10.1176/ajp.2006.163.4.600. [DOI] [PubMed] [Google Scholar]
- 23.Sikich L, Frazier JA, McClellan J, et al. Double-blind comparison of first- and second-generation antipsychotics in early-onset schizophrenia and schizoaffective disorder: findings from the Treatment of Early-onset Schizophrenia Spectrum Disorders (TEOSS) Study. Am J Psychiatry. 2008;165:1420–1431. doi: 10.1176/appi.ajp.2008.08050756. [DOI] [PubMed] [Google Scholar]
- 24.Geddes JR, Briess D. Bipolar disorder. [September 30, 2010];Clin Evid (Online) 2007 August 1; 2007. PMC2943789. Available at: http://www.ncbi.nlm.nih.gov/pubmed/19454110?dopt=Citation. [PMC free article] [PubMed]
- 25.Abarca J, Malone DC, Armstrong EP, Grizzle AJ, Hasten PD, Van Bergen RC, Lipton RB. Concordance of severity ratings provided in four drug interaction compendia. J Am Pharm Assoc. 2004;44:136–141. doi: 10.1331/154434504773062582. [DOI] [PubMed] [Google Scholar]
- 26. [August 13, 2008];Thomson Micromedex DrugDex ® Compendium Revision Request - CAG-00391. Centers for Medicare and Medicaid Services 2008. http://www.cms.hhs.gov/mcd/ncpc_view_document.asp?id=16.