Abstract
From a young age, males are at higher cardiovascular risk than females. Dyslipidemia, including a higher burden related to small low-density lipoproteins (LDL), plays an important role in precipitating atherosclerosis in both males and females. We investigated sex differences in atherogenic lipoprotein burden and the independent predictors of LDL particle size in children and adolescents. We measured the concentrations of total testosterone, sex hormone-binding globulin, estradiol, total cholesterol, triglyceride, LDL cholesterol, HDL cholesterol, and LDL particle size in 135 children and adolescents (67 boys, 68 girls). The free androgen index was significantly and negatively correlated with LDL particle size (r = -0.273, P = 0.026) in boys, but estrogen and LDL particle size were not related. In a stepwise multiple regression analysis adjusted for body mass index, age, and homeostasis model assessment for insulin resistance, free androgen index was still an independent predictor of LDL particle size in boys (R2 = 0.075, P = 0.026). The prominent decrease in LDL particle size along with increased testosterone concentrations in males might explain why they are more likely to display atherogenic dyslipidemia from adolescence.
Keywords: Adolescent, Small dense LDL, Testosterone
INTRODUCTION
Plasma low-density lipoprotein cholesterol (LDL-C) is associated with an increased risk of coronary heart disease (CHD) (1, 2); however, more than 30% of patients with CHD events have normal LDL-C level (3, 4). LDL particles are heterogeneous and can be divided into two subclasses based on variations in density, size, and chemical composition: large buoyant LDL (lb-LDL, pattern A) and small dense LDL (sd-LDL, pattern B) (5). Studies have shown that sd-LDL has greater atherogenic potential than lb-LDL in various ethnic groups (6-9).
Several studies have reported that LDL particle size tends to be smaller in both young and adult males compared to females (10-12). Hormonal differences have been hypothesized to account for these sex differences, but few studies have examined the association between sex steroid hormones and LDL particle size in young people. A recent clinical trial showed that hormone replacement therapy (HT) does not reduce the risk of coronary disease in postmenopausal women (13). Furthermore, HT users reportedly do not have a better LDL subclass distribution, which may explain the failure of HT to reduce the incidence of heart disease events (14). These results suggest that estrogens might not be the key determinant of this sex difference.
Children and adolescents experience profound changes in sex steroid hormones during puberty. Moreover, adverse patterns of atherosclerosis begin during childhood (15). Therefore, children and adolescents are appropriate candidates to study the relationship between sex steroid hormones and LDL size.
The purpose of this study was to compare LDL particle size in boys and girls, and to investigate whether changes in male sex hormone concentrations are related to LDL particle size in children and adolescents.
MATERIALS AND METHODS
A detailed description of the study design and methods is outlined in a previous report (16). Briefly, 135 children and adolescents (67 boys, 68 girls; mean age, 11.6 ± 2.0 yr) participated after guardians' permission in this study from January to February in 2004; their ages ranged from 7 to 16 yr. The subjects were recruited through newspaper advertisements in Suwon, Korea. Pubertal stage was assessed by physical examination, which was performed by a pediatrician at our institute, according to the Tanner criteria. We assigned 33 boys and 19 girls to the child group (Tanner stage = 1) and 34 boys and 49 girls to the adolescent group (Tanner stage ≥ 2).
Anthropometric and body fat measurements
We measured the weight and height of all subjects in the morning after minimum 8-hr fasting while they were wearing light clothing. Body mass index (BMI) was calculated as weight (kg)/height (m2). Blood pressure was measured twice in the sitting position at 3-min intervals using a standard sphygmomanometer.
To assess the distribution of body fat in the abdomen, we performed computed tomography (High Speed Advantage; General Electric Co., Fairfield, CT, USA) at the umbilical level and measured the total abdominal fat area (cm2) equivalent to a Hounsfield unit range of -50 to -250. We identified the visceral fat area and subcutaneous fat area by applying the peritoneum as a boundary. The clinical status of the participants was made unknown to the investigator who collected and analyzed these data.
Laboratory measurements
After fasting for 8 hr or more, all subjects visited laboratory between 08:00 and 10:00, and a blood sample was drawn from the antecubital vein. Plasma was separated from the collected blood and stored at -70℃ until analyzed. Glucose, insulin, total cholesterol, triglyceride (TG), and high-density lipoprotein (HDL)-cholesterol concentrations were measured by standard methods. LDL-C concentration was calculated using the Friedewald equation. As a marker of insulin resistance, a homeostasis model assessment (HOMA) index was calculated from the fasting insulin and glucose concentrations as (insulin [µIU/mL] × glucose [mM/L])/22.5.
Estradiol (E2) and total testosterone concentrations were measured with commercial solid-phase radioimmunoassays (Diagnostic Products Corp., Los Angeles, CA, USA). Sex hormone-binding globulin (SHBG) concentrations were measured using a commercial immunoradiometric assay (Diagnostic Products Corp.). The free androgen index (FAI) was used to estimate the amount of testosterone unbound by SHBG and thus, immediately biologically active. FAI was calculated as (100 Total testosterone/SHBG). To convert testosterone to nM, the ng per mL value was multiplied by 3.467.
LDL particles were isolated by sequential flotation ultracentrifugation, and LDL particle size distribution (d 1.019-1.063 g/mL) was examined using a pore gradient lipoprotein system (CBS Scientific, Del Mar, CA, USA) with commercially available non-denaturing polyacrylamide slab gels containing a linear gradient of 2% to 16% acrylamide (Alamo Gels Inc., San Antonio, TX, USA). Standards, including latex beads (34 nm), thyroglobulin (17 nm), apoferritin (12.2 nm), and catalase (10.4 nm), were used to estimate the relative migration (Rf) rates of each band. The gels were scanned using a GS-800 Calibrated Imaging Densitometer (Bio-Rad Laboratories, Graz, Austria). LDL particle size was calculated with reference to the Rf value of the standards. LDL subclasses were classified as sd-LDL (pattern B; diameter < 25.5 nm) and lb-LDL (pattern A; diameter < 25.5 nm) (5).
Statistical analysis
The subjects were divided into two groups based on the Tanner stage: children (Tanner stage = 1) and adolescents (Tanner stage ≥ 2). In each group, boys and girls were analyzed separately to better understand the association between LDL particle size and sex steroid hormone concentrations. All data are presented as means ± standard deviation and number. Since HOMA for insulin resistance (IR) and concentrations of insulin, TG, testosterone, SHBG, FAI, and E2 were not normally distributed, these variables were log-transformed prior to analysis.
The clinical characteristics and laboratory findings were compared for boys and girls using Student's t test. Because BMI and age differed significantly between boys and girls in both children and adolescents, each factor was compared using an ANCOVA after adjusting for BMI and age. We used correlation analyses to examine the relationship between LDL particle size and each factor in boys and girls, separately. Multiple stepwise regression analysis was performed to investigate whether the FAI was related to LDL particle size in boys, after adjusting for age, BMI, and HOMA-IR.
Statistical analyses were performed using PASW for Windows (v. 18.0; SPSS Inc., Chicago, IL, USA), and P < 0.05 was considered significant.
Ethics statement
This study was conducted according to the ethical guidelines of Ajou University Hospital and Ajou University School of Medicine and written informed consent was obtained from all guardians of the participants.
RESULTS
Sex differences in baseline characteristics and LDL particle size in children and adolescents
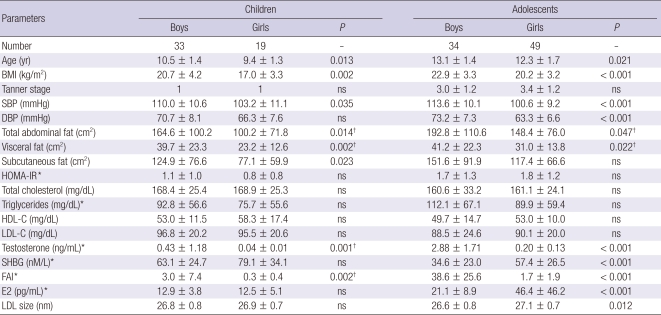
Table 1 shows the data for clinical and biochemical parameters and LDL particle size grouped by sex in children and adolescents. Boys were older than girls in both the child (P = 0.013) and adolescent groups (P = 0.021). No significant sex difference in Tanner stage existed within adolescents. Systolic blood pressure (SBP) was significantly higher in boys for both children (P = 0.035) and adolescents (P < 0.001). BMI differed significantly between boys and girls, and was higher in both groups of boys (P = 0.002 for children, P < 0.001 for adolescents). Visceral fat area was significantly higher in boys of both groups (P = 0.002 for children, P = 0.022 for adolescents), although the subcutaneous fat area was significantly higher only in male children (P = 0.023). FAI and serum testosterone concentrations were significantly higher in boys for both children (P = 0.002) and adolescents (P < 0.001). SHBG and E2 concentrations were significantly higher in girls than in boys, but only for adolescents (P < 0.001).
Table 1.
Comparison of clinical and biochemical parameters and LDL particle size by sex in children and adolescents
Data are presented as means ± SD; P values by Student's t-test for continuous variables and χ2 tests for categorical variables are given. *log-transformed; †not significant after adjustment for BMI and age by ANCOVA. BMI, body mass index; HOMA-IR, homeostasis model assessment for insulin resistance; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure; SHBG, sex hormone-binding globulin; FAI, free androgen index; E2, estradiol; LDL, low density lipoprotein; ns, not significant.
The concentrations of total cholesterol, HDL-C, LDL-C, and TG did not differ significantly between boys and girls in either age group. Of note, LDL particle size did not differ between the sexes in children, but was significantly smaller in male adolescents as compared to female adolescents (P = 0.012). After adjusting for BMI and age, the difference between sexes was still significant for SBP in both age groups (P < 0.05). In adolescents, the serum concentrations of testosterone, SHBG, and E2, and LDL particle size remained significantly different after adjustment (P < 0.05). However, FAI and serum testosterone concentrations were not significantly different in children after adjustment.
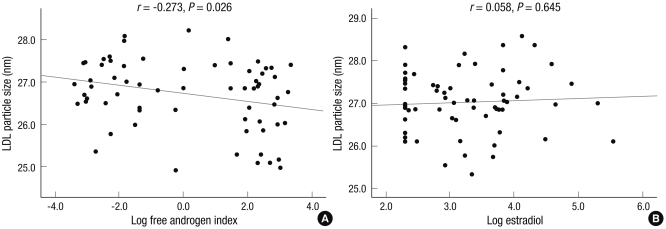
Correlation between sex hormones and LDL particle size in boys and girls
In boys, univariate analysis showed significant associations between LDL particle size and BMI, SBP, DBP, TG, HDL-C, testosterone, SHBG, and FAI (P < 0.05). In girls, only TG and HDL-C were significantly associated with LDL particle size (P < 0.05); none of sex hormones were associated with LDL particle size. The relationships between LDL size and sex hormones in boys and girls are shown in Fig. 1.
Fig. 1.
Correlation between low density lipoprotein (LDL) particle size and sex hormones in children (A) and adolescents (B).
Because LDL particle size was significantly associated with FAI only in boys, we performed the stepwise multivariable regression analysis in boys only. Since age, BMI, and HOMA-IR were significantly associated with FAI (data not shown), these parameters were defined as confounding variables in the analysis. As a result, FAI remained an independent predictor of LDL particle size in boys (R2 = 0.075, P = 0.026).
LDL particle size before and after puberty in relation to sex hormone concentrations
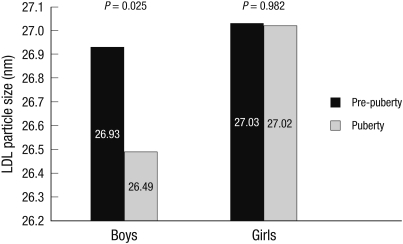
LDL particle size was significantly different only in adolescents, not in children (Table 1), and FAI was independently correlated with LDL particle size only in boys. E2 concentration and LDL particle size were not significantly correlated in either age group (Table 2). We hypothesized that LDL particle size is affected by more profound changes in testosterone concentrations. To test this hypothesis, we categorized individuals as either before or after puberty in both boys and girls according to their testosterone and E2 concentrations, respectively. We arbitrarily determined a cutoff level as the prepubertal upper normal values of testosterone (0.8 nM/L) and E2 (10 pg/mL) concentrations and lower normal value of SHBG (62.4 nM/L) concentrations (17). We also calculated the FAI cutoff value (1.28) using the arbitrarily determined testosterone and SHBG concentrations. The analysis showed that LDL particle size differed significantly before and after puberty (P = 0.025) in boys, but not in girls (P = 0.982) (Fig. 2).
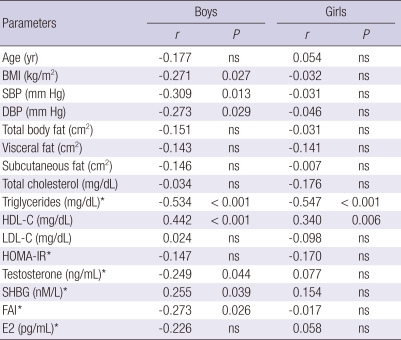
Table 2.
Anthropometric and biochemical parameters associated with LDL particle size in boys and girls
*log-transformed. r, correlation coefficient; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; HOMA-IR, homeostasis model assessment for insulin resistance; SHBG, sex hormone-binding globulin; FAI, free androgen index; E2, estradiol; ns, not significant.
Fig. 2.
Mean low density lipoprotein (LDL) particle size before and after mid-puberty in boys and girls according to testosterone and estrogen levels, respectively.
DISCUSSION
In this study, we showed that LDL particle size was significantly smaller only in adolescents, and that the particle size decreases as FAI increases in boys. Even though LDL-C concentrations were within the normal range and did not differ between boys and girls in children and adolescents, the higher burden of small dense LDL during puberty in boys could imply a higher cardiovascular risk in males starting at a young age.
The factors affecting LDL particle size have been studied widely in adults, but few studies have included children (12, 18-20). Among these factors, sex has been suggested to be important, although few studies have found sex differences in LDL size in children (12, 21). In contrast, some investigations of adults have reported significant sex differences in LDL size (10, 11). These studies found larger LDL particle sizes in women, and our results extend this previously reported sex difference to include children and adolescents.
The mechanisms responsible for the sex differences in LDL particle size remain unclear. Studies have suggested that differences in visceral fat accumulation and TG metabolism between men and women are responsible for this sex difference (10-12). However, we found no sex differences in visceral fat or TG concentrations in either age group. In addition, we found no association between visceral fat and LDL particle size in boys and girls.
The relationship between testosterone concentrations and the lipid profile is controversial. Few studies have examined the association between LDL particle size and testosterone concentration. In one adult study, low levels of SHBG and testosterone were associated with small dense LDL in normoglycemic middle-aged men (22). These data are inconsistent with our results. However, testosterone administration in men decreased LDL size in other studies (23, 24). In vivo studies found that testosterone administration increases the activity of hepatic lipase, which hydrolyzes TG in LDL and produces small dense LDL particles. This mechanism may explain why testosterone is associated with smaller LDL particle size (23-25).
In this study, we found a difference in LDL particle size only in adolescents and not in children. Moreover, FAI was associated with LDL particle size only in boys. This led us to hypothesize that some threshold in testosterone concentration must be reached for this association. To test this hypothesis, we compared LDL particle size before and after puberty according to sex hormone concentrations and found a significant difference between the two groups, but only in boys. These results were consistent with the hypothesis that testosterone had a more potent effect on LDL particle size than estrogen, and that profound changes in testosterone concentration were involved in the regulation of LDL particle size.
In general, estrogen has been regarded as a favorable factor on lipid profiles and anti-atherogenic effects, and is one of the factors responsible for the sex difference in cardiovascular risk (26). However, the Women's Health Initiative clinical trial failed to find a reduction in coronary heart disease events among estrogen HT users (13). They also found that HT users did not have a better LDL subclass distribution, which may explain the failure of HT to reduce the incidence of heart disease events (14). Furthermore, the SWAN study reported that FAI was related to cardiovascular risk factors, including unfavorable lipid profiles in multiethnic premenopausal and perimenopausal women (27). Based on our results and the reasons cited above, we suggest that testosterone might have a greater effect on LDL particle size than estrogen. More studies are required to confirm this conclusion.
This study has several limitations. First, the study was performed on a small number of subjects and thus did not represent all children and adolescents in the population. In addition, the study design was cross-sectional, and therefore, we cannot speculate on the association between LDL particle size and serial changes in FAI. Specifically, we cannot evaluate the longitudinal association between testosterone concentrations and LDL particle size before and after puberty in the same individuals. However, we could estimate longitudinal associations from this study, including a broad spectrum of ages from prepuberty to late puberty. In this study, we could not measure free testosterone, which is more informative as a male sex hormone. FAI is also known to have a poor correlation with actual free testosterone concentrations in male adults (28, 29). However, free testosterone can be approximated by FAI if, and only if, the total testosterone concentration is negligible in relation to the concentrations of SHBG-binding sites (28). For that reason, this is a reasonable approximation for samples from children in whom blood testosterone concentrations are rarely above 10% of the SHBG concentration (29). In addition, we could not draw blood at the same point in the menstrual cycle in girls. Given the variation in serum estradiol concentrations over the menstrual cycle, whether estradiol concentrations are associated with LDL particle size is not clear. Further studies are required to elucidate the association between estrogen and LDL particle size in children and adolescents.
Our study, however, is the first to show that FAI is significantly related to LDL particle size in boys, and our findings suggest that testosterone might contribute to higher cardiovascular risk in males by lowering LDL particle size. Further prospective studies should focus on the effects of sex hormones on the lipid profile and the associated development of atherosclerosis.
Footnotes
This study was supported by a grant from the Korean Health 21 R&D Project, Ministry of Health and Welfare, Korea (A050463), and a 2004 grant from Ajou University School of Medicine. There is no conflict of interests with these financial supports relating to publishing this article.
AUTHOR SUMMARY
A Higher Burden of Small Low-density Lipoprotein Particles is Associated with Profound Changes in the Free Androgen Index in Male Adolescents
Yong Jun Choi, Sung Hee Choi, Hae Jin Kim, Seung Jin Han, Jin Soon Hwang, Yoon-Sok Chung, Kwan Woo Lee, Hong Keun Cho, and Dae Jung Kim
Even from a young age, males are known to have higher cardiovascular risk than females. Dyslipidemia, including a higher burden related to small low-density lipoproteins (LDL), plays an important role in precipitating atherosclerosis. Here we investigate sex differences in atherogenic lipoprotein burden and the LDL particle size in 135 children and adolescents. LDL particle size is significantly smaller in male than female. The free androgen index (FAI) (100 Total testosterone/sex hormone binding globulin [SHBG]) is negatively correlated with LDL particle size in boys whereas estrogen and LDL particle size are not related with each other. After puberty, LDL particle size declines markedly in male adolescents. The prominent decrease in LDL particle size associated with an increase in testosterone concentrations might underlie the risk of atherogenic dyslipidemia in males from adolescence.
References
- 1.Castelli WP, Garrison RJ, Wilson PW, Abbott RD, Kalousdian S, Kannel WB. Incidence of coronary heart disease and lipoprotein cholesterol levels. The Framingham Study. JAMA. 1986;256:2835–2838. [PubMed] [Google Scholar]
- 2.Kwon SW, Yoon SJ, Kang TS, Kwon HM, Kim JH, Rhee J, Lee SJ, Park JK, Lim JY, Yoon YW, Hong BK. Significance of small dense low-density lipoprotein as a risk factor for coronary artery disease and acute coronary syndrome. Yonsei Med J. 2006;47:405–414. doi: 10.3349/ymj.2006.47.3.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Genest JJ, McNamara JR, Salem DN, Schaefer EJ. Prevalence of risk factors in men with premature coronary artery disease. Am J Cardiol. 1991;67:1185–1189. doi: 10.1016/0002-9149(91)90924-a. [DOI] [PubMed] [Google Scholar]
- 4.Hamsten A, Walldius G, Szamosi A, Dahlen G, de Faire U. Relationship of angiographically defined coronary artery disease to serum lipoproteins and apolipoproteins in young survivors of myocardial infarction. Circulation. 1986;73:1097–1110. doi: 10.1161/01.cir.73.6.1097. [DOI] [PubMed] [Google Scholar]
- 5.Austin MA, King MC, Vranizan KM, Krauss RM. Atherogenic lipoprotein phenotype. A proposed genetic marker for coronary heart disease risk. Circulation. 1990;82:495–506. doi: 10.1161/01.cir.82.2.495. [DOI] [PubMed] [Google Scholar]
- 6.Gardner CD, Fortmann SP, Krauss RM. Association of small low-density lipoprotein particles with the incidence of coronary artery disease in men and women. JAMA. 1996;276:875–881. [PubMed] [Google Scholar]
- 7.Krauss RM. Dense low density lipoproteins and coronary artery disease. Am J Cardiol. 1995;75:53B–57B. doi: 10.1016/0002-9149(95)80012-h. [DOI] [PubMed] [Google Scholar]
- 8.Lamarche B, Tchernof A, Moorjani S, Cantin B, Dagenais GR, Lupien PJ, Després JP. Small, dense low-density lipoprotein particles as a predictor of the risk of ischemic heart disease in men. Prospective results from the Quebec Cardiovascular Study. Circulation. 1997;95:69–75. doi: 10.1161/01.cir.95.1.69. [DOI] [PubMed] [Google Scholar]
- 9.Slyper AH. Low-density lipoprotein density and atherosclerosis. Unraveling the connection. JAMA. 1994;272:305–308. [PubMed] [Google Scholar]
- 10.Carr MC, Hokanson JE, Zambon A, Deeb SS, Barrett PH, Purnell JQ, Brunzell JD. The contribution of intraabdominal fat to gender differences in hepatic lipase activity and low/high density lipoprotein heterogeneity. J Clin Endocrinol Metab. 2001;86:2831–2837. doi: 10.1210/jcem.86.6.7586. [DOI] [PubMed] [Google Scholar]
- 11.McNamara JR, Campos H, Ordovas JM, Peterson J, Wilson PW, Schaefer EJ. Effect of gender, age, and lipid status on low density lipoprotein subfraction distribution. Results from the Framingham Offspring Study. Arteriosclerosis. 1987;7:483–490. doi: 10.1161/01.atv.7.5.483. [DOI] [PubMed] [Google Scholar]
- 12.Shimabukuro T, Sunagawa M, Ohta T. Low-density lipoprotein particle size and its regulatory factors in school children. J Clin Endocrinol Metab. 2004;89:2923–2927. doi: 10.1210/jc.2003-031818. [DOI] [PubMed] [Google Scholar]
- 13.Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, Bonds D, Brunner R, Brzyski R, Caan B, Chlebowski R, Curb D, Gass M, Hays J, Heiss G, Hendrix S, Howard BV, Hsia J, Hubbell A, Jackson R, Johnson KC, Judd H, Kotchen JM, Kuller L, LaCroix AZ, Lane D, Langer RD, Lasser N, Lewis CE, Manson J, Margolis K, Ockene J, O'Sullivan MJ, Phillips L, Prentice RL, Ritenbaugh C, Robbins J, Rossouw JE, Sarto G, Stefanick ML, Van Horn L, Wactawski-Wende J, Wallace R, Wassertheil-Smoller S Women's Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: The Women's Health Initiative Randomized Controlled Trial. JAMA. 2004;291:1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 14.Mackey RH, Kuller LH, Sutton-Tyrrell K, Evans RW, Holubkov R, Matthews KA. Hormone therapy, lipoprotein subclasses, and coronary calcification: the Healthy Women Study. Arch Intern Med. 2005;165:510–515. doi: 10.1001/archinte.165.5.510. [DOI] [PubMed] [Google Scholar]
- 15.Reinehr T, Kiess W, de Sousa G, Stoffel-Wagner B, Wunsch R. Intima media thickness in childhood obesity: relations to inflammatory marker, glucose metabolism, and blood pressure. Metabolism. 2006;55:113–118. doi: 10.1016/j.metabol.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 16.Choi YJ, Jo YE, Kim YK, Ahn SM, Jung SH, Kim HJ, Chung YS, Lee KW, Kim DJ. High plasma concentration of remnant lipoprotein cholesterol in obese children and adolescents. Diabetes Care. 2006;29:2305–2310. doi: 10.2337/dc06-0938. [DOI] [PubMed] [Google Scholar]
- 17.Alan HB. Tietz clinical guide to laboratory tests. 4th ed. St. Louis, MO: Saunders; 2006. [Google Scholar]
- 18.Miyashita M, Okada T, Kuromori Y, Harada K. LDL particle size, fat distribution and insulin resistance in obese children. Eur J Clin Nutr. 2006;60:416–420. doi: 10.1038/sj.ejcn.1602333. [DOI] [PubMed] [Google Scholar]
- 19.Stan S, Levy E, Delvin EE, Hanley JA, Lamarche B, O'Loughlin J, Paradis G, Lambert M. Distribution of LDL particle size in a population-based sample of children and adolescents and relationship with other cardiovascular risk factors. Clin Chem. 2005;51:1192–1200. doi: 10.1373/clinchem.2004.046771. [DOI] [PubMed] [Google Scholar]
- 20.Steinbeck KS, Bermingham MA, Mahajan D, Baur LA. Low-density lipoprotein subclasses in children under 10 years of age. J Paediatr Child Health. 2001;37:550–553. doi: 10.1046/j.1440-1754.2001.00753.x. [DOI] [PubMed] [Google Scholar]
- 21.Freedman DS, Bowman BA, Otvos JD, Srinivasan SR, Berenson GS. Levels and correlates of LDL and VLDL particle sizes among children: the Bogalusa heart study. Atherosclerosis. 2000;152:441–449. doi: 10.1016/s0021-9150(99)00495-5. [DOI] [PubMed] [Google Scholar]
- 22.Haffner SM, Laakso M, Miettinen H, Mykkänen L, Karhapää P, Rainwater DL. Low levels of sex hormone-binding globulin and testosterone are associated with smaller, denser low density lipoprotein in normoglycemic men. J Clin Endocrinol Metab. 1996;81:3697–3701. doi: 10.1210/jcem.81.10.8855825. [DOI] [PubMed] [Google Scholar]
- 23.Herbst KL, Amory JK, Brunzell JD, Chansky HA, Bremner WJ. Testosterone administration to men increases hepatic lipase activity and decreases HDL and LDL size in 3 wk. Am J Physiol Endocrinol Metab. 2003;284:E1112–E1118. doi: 10.1152/ajpendo.00524.2002. [DOI] [PubMed] [Google Scholar]
- 24.Tan KC, Shiu SW, Kung AW. Alterations in hepatic lipase and lipoprotein subfractions with transdermal testosterone replacement therapy. Clin Endocrinol (Oxf) 1999;51:765–769. doi: 10.1046/j.1365-2265.1999.00882.x. [DOI] [PubMed] [Google Scholar]
- 25.Berg G, Schreier L, Geloso G, Otero P, Nagelberg A, Levalle O. Impact on lipoprotein profile after long-term testosterone replacement in hypogonadal men. Horm Metab Res. 2002;34:87–92. doi: 10.1055/s-2002-20521. [DOI] [PubMed] [Google Scholar]
- 26.Pérez-López FR, Larrad-Mur L, Kallen A, Chedraui P, Taylor HS. Gender differences in cardiovascular disease: hormonal and biochemical influences. Reprod Sci. 2010;17:511–531. doi: 10.1177/1933719110367829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sutton-Tyrrell K, Wildman RP, Matthews KA, Chae C, Lasley BL, Brockwell S, Pasternak RC, Lloyd-Jones D, Sowers MF, Torréns JI SWAN Investigators. Sex-hormone-binding globulin and the free androgen index are related to cardiovascular risk factors in multiethnic premenopausal and perimenopausal women enrolled in the Study of Women Across the Nation (SWAN) Circulation. 2005;111:1242–1249. doi: 10.1161/01.CIR.0000157697.54255.CE. [DOI] [PubMed] [Google Scholar]
- 28.Kapoor P, Luttrell BM, Williams D. The free androgen index is not valid for adult males. J Steroid Biochem Mol Biol. 1993;45:325–326. doi: 10.1016/0960-0760(93)90350-6. [DOI] [PubMed] [Google Scholar]
- 29.Ly LP, Handelsman DJ. Empirical estimation of free testosterone from testosterone and sex hormone-binding globulin immunoassays. Eur J Endocrinol. 2005;152:471–478. doi: 10.1530/eje.1.01844. [DOI] [PubMed] [Google Scholar]