Abstract
Objective
To investigate the prevalence and correlates of intimate partner violence (IPV) among women at an HIV voluntary counseling and testing (VCT) center in northern Tanzania.
Methods
In a cross-sectional study, the lifetime history of IPV experienced by women attending an HIV VCT center in Moshi, Tanzania, from June 2005 to January 2008 was assessed. Bivariate and ordered logistic regression analyses were performed to identify risk factors for IPV.
Results
Of 2436 enrolled women, 432 (17.7%) reported IPV during their lifetime. Older, unemployed, and less-educated women, and those with children were more likely to have experienced IPV (P<0.05). IPV exposure differed by marital status (P<0.001). Adjusting for sociodemographics, the odds ratio of IPV was 1.51 (95% confidence interval [CI] 1.10–2.07) for married women and 2.25 (95% CI 1.63–3.10) for divorced women, compared with single women. HIV prevalence did not differ by IPV exposure or severity; however, 22.4% of single women who had experienced IPV were HIV seropositive, compared with 15.1% of women with no experience of IPV (P=0.041).
Conclusion
Given that IPV represents both a risk factor for and a consequence of HIV infection, VCT sites are an appropriate and accessible venue for IPV screening and counseling in resource-poor settings.
Keywords: Counseling, Domestic violence, HIV infection, Tanzania
1. Introduction
Intimate partner violence (IPV), also known as domestic violence, is emotional, physical, or sexual violence, and is usually perpetrated against women by their intimate male partners. IPV is a violation of basic human rights and places an increasingly recognized burden on women’s health and public health worldwide [1,2]. Although most studies on IPV arise from the West, recent studies across the African continent have yielded prevalence estimates of either physical or sexual IPV ranging from 18% in the past year to 71% in a lifetime [3–7]. The accuracy of these widely ranging estimates is uncertain, given both the underreporting of IPV and a lack of consistent research methodologies.
There are few data on the prevalence and severity of IPV in Tanzania. In the World Health Organization (WHO) Multi-Country Study on Women’s Health and Domestic Violence, 56% of rural and 41% of urban Tanzanian women reported some experience of IPV [3]. A population-based study in Moshi, Tanzania, reported a past-year prevalence of 21% and a lifetime prevalence of 26% of physical or sexual violence; verbal or emotional abuse was not assessed in that study and has rarely been investigated in the sub-Saharan Africa setting [4].
The characteristics associated with IPV vary. The following risk factors have been cited: age, either younger or older [3,6,8]; lower level of education [3,4,9]; divorce, separation, or cohabitation with a partner outside marriage [3]; income inequality between partners [4,5]; lack of fidelity [9]; and more than 5 children [4]. IPV has also been linked to HIV, especially in regions with a high prevalence of seropositivity [8,10–12]. In a sample of 245 women presenting for voluntary counseling and testing (VCT) in Dar es Salaam, Tanzania, those found to be infected with HIV were 65% more likely to have been in a physically abusive relationship in their lifetime, and more than twice as likely to be in a currently abusive relationship [8].
Given the high prevalence of IPV in Tanzania, its impact on women’s health, and its relationship with HIV infection, the aim of the present study was to investigate the correlates associated with the prevalence and severity of IPV by screening a large sample of women presenting to an HIV VCT center in the Kilimanjaro Region of Tanzania.
2. Materials and methods
In the present cross-sectional study, subjects were recruited between 1 June 2005 and 31 January 2008 at an HIV VCT center in Moshi, Tanzania, operated by Kikundi cha Wanawake Kilimanjaro Kupambana na Ukimwi (KIWAKKUKI; Women Against AIDS in Kilimanjaro). KIWAKKUKI, a women-led HIV/AIDS advocacy, education, and home-care organization, was selected as the site for the present study because of its local and national reputation as a holistic, community-based AIDS service organization with the capacity to accommodate research activities. With the exception of those attending during a 3-week national VCT campaign in October 2007, all female clients aged 18 years or older were approached consecutively for study participation; refusal rates were less than 5% [13].
The study protocol was approved by institutional review boards at Kilimanjaro Christian Medical Centre, the Tanzania National Institute for Medical Research, and Duke University Medical Center. All participants provided written, informed consent before data collection. Participants who reported IPV were referred for counseling services within KIWAKKUKI. Participant confidentiality was maintained during the interview, in case of referral, and with data storage and entry.
After giving informed consent, clients presenting for VCT were interviewed in Kiswahili by trained counselors in a private location using a standardized 44-item questionnaire. The questionnaire covered sociodemographic information, reasons for testing, sexual behavior, and symptoms associated with HIV infection. It also included the following IPV-related questions modeled after questions from the WHO Multi-Country Study on Women’s Health and Domestic Violence [14]: “has your current husband/partner, or any other partner, ever done something physically to hurt you?” and “has your current husband/partner, or any other partner, ever physically forced you to have sexual intercourse when you did not want to?” The answer choices to each question were “frequently,” “sometimes,” and “never.” Data were entered by using Teleform 9.0 (Cardiff, Vista, CA, USA), and unique records of all female clients aged 18 and older with at least 1 lifetime sexual partner were analyzed by using Stata 11 (StataCorp, College Station, TX, USA).
“Frequently” and “sometimes” responses to either question regarding IPV were aggregated into 1 binary variable describing lifetime prevalence of any IPV. A second variable comprised of mutually exclusive groups was created to describe the severity of IPV; the first group comprised those who responded “never” to both IPV questions; the second group comprised those who responded “sometimes” to at least 1 IPV question; and the third group comprised those who responded “frequently” to at least 1 IPV question. Marital status was based on self-report of being married (including monogamous and polygamous relationships, and cohabiting and engaged partners), single, widowed, or divorced. Fifty women with missing data on either IPV or marital status were excluded.
Differences in client characteristics were assessed via Pearson χ2 test and Mantel–Haenszel odds ratio (OR). Nonparametric trend tests were used to assess changes in IPV prevalence with increasing age. After the identification of significant variables by bivariate analysis, a logistic regression was modeled to quantify the effect of sociodemographic factors (P<0.10 in bivariate analysis) and HIV serostatus on IPV prevalence. By using parameter estimates from this model, the marginal effect of marriage on the probability of IPV among married women as compared with single women was calculated. The size of the sample selected for the present study was sufficient to afford a precision within 2.9 percentage points for estimates of IPV prevalence as low as 18% (the lowest documented value in literature from Africa [5]). Our sample of 2436 women implied a power of 95% to identify an OR of 1.19 or above.
3. Results
Of the 2436 female VCT clients who enrolled in the present study, 432 (17.7%) reported experiencing either physical or sexual violence perpetrated by a partner during their lifetime (Table 1). As compared with women without IPV, those who had experienced IPV were more likely to be older (OR 1.32, 95% confidence interval [CI] 1.20–1.44), unemployed (OR 1.76, 95% CI 1.28–2.44), and have children (OR 4.14, 95% CI 2.88–5.96), and were less likely to be educated (OR 0.64, 95% CI 0.49–0.83).
Table 1.
Characteristics of study participants with and without a history of IPV a
| No history of IPV (n=2004) | Any history of IPV (n=432) | |
|---|---|---|
| Age category, years * | ||
| 18–24 | 605 (30.2) | 71 (16.4) |
| 25–30 | 360 (18.0) | 69 (16.0) |
| 30–39 | 513 (25.6) | 145 (33.6) |
| 40+ | 526 (26.3) | 147 (34.0) |
| Marital status b | ||
| Single | 955 (47.7) | 116 (26.9) |
| Married | 462 (23.1) | 131 (30.3) |
| Divorced | 277 (13.8) | 118 (27.3) |
| Widowed | 310 (15.5) | 67 (15.5) |
| Number of lifetime partners | ||
| 1 | 754 (37.7) | 149 (34.7) |
| 2–4 | 1059 (52.9) | 238 (55.4) |
| 5+ | 186 (9.3) | 43 (10.0) |
| Urban residence | 1001 (50.1) | 209 (48.4) |
| Education lower than secondary level b | 1470 (73.4) | 351 (81.3) |
| Any children b | 1468 (73.3) | 397 (91.9) |
| Employed b | 1845 (92.1) | 375 (86.8) |
| % HIV seropositive | 387 (19.3) | 96 (22.2) |
| Reasons for VCT | ||
| Illness b | 372 (18.6) | 125 (29.0) |
| New sexual partner | 180 (14.4) | 41 (11.8) |
| Suspect sexual partner unfaithful b | 1008 (50.5) | 294 (68.1) |
| Sexual partner died | 280 (14.0) | 74 (17.1) |
| Pre-marriage b,c | 297 (19.3) | 27 (9.0) |
| Pre-conception | 134 (6.7) | 19 (4.4) |
| Received gifts/money for sexual intercourse b | 176 (8.8) | 22 (5.1) |
| Sexual partner has other partners b | 460 (35.1) | 180 (62.9) |
| Suspect any partner has ever had HIV b | 255 (12.7) | 85 (19.7) |
Values are expressed as number (percentage).
P<0.05.
n=1838; the number did not include those currently married.
The prevalence of IPV differed by marital status (P<0.001): 10.8% of single women, 17.8% of widowed women, 22.1% of married women, and 29.9% of divorced women reported any lifetime IPV. There were no differences in the number of lifetime partners or the prevalence of HIV seropositivity rate according to history of IPV; however, women with IPV were more likely to have sexual partners with other partners (OR 3.14, 95% CI 2.39–4.12), to suspect HIV in a current or past sexual partner (OR 1.68, 95% CI 1.28–2.21), and to present for VCT owing to illness (OR 1.79, 95% CI 1.41–2.27) and/or suspicion of an unfaithful sexual partner (OR 2.09, 95% CI 1.67–2.61). They were also less likely to receive gifts or money in exchange for sexual intercourse (OR 0.56, 95% CI 0.35–0.88).
Among those with a history of IPV, 338 (78.2%) women reported any physical violence, 265 (61.3%) reported any sexual violence, and 171 (39.6%) reported both physical and sexual violence. Most women experienced physical violence “sometimes” without any sexual violence, with 44 (10.2%) “frequently” experiencing both physical and sexual violence (Table 2). The differences in sociodemographics according to severity of IPV exposure were similar to those according to IPV exposure alone (data not shown).
Table 2.
Severity of IPV among study participants a
| Sexual violence | |||||
|---|---|---|---|---|---|
| Never | Sometimes | Frequently | Total | ||
| Physical violence | Never | 2004 (82.3) | 76 (3.1) | 18 (0.7) | 2098 (86.1) |
| Sometimes | 115 (4.7) | 79 (3.2) | 19 (0.8) | 213 (8.7) | |
| Frequently | 52 (2.1) | 29 (1.2) | 44 (1.8) | 125 (5.1) | |
| Total | 2171 (89.1) | 184 (7.6) | 81 (3.3) | 2436 (100.0) | |
Values are expressed as number (percentage).
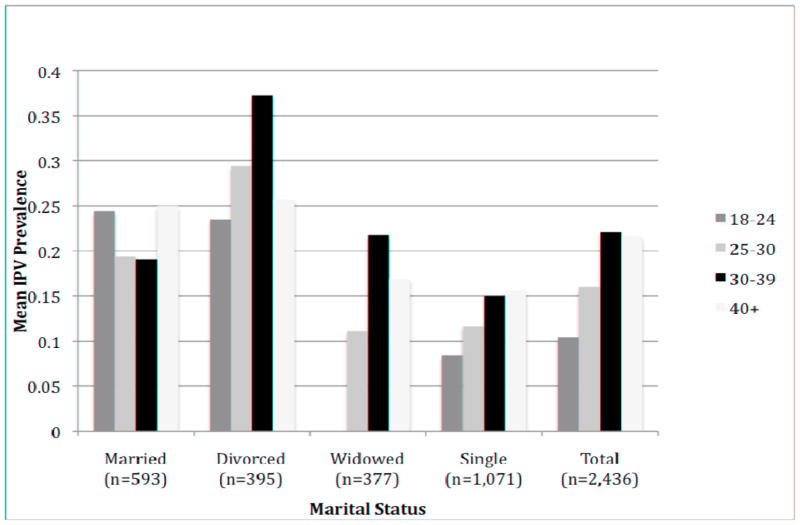
The prevalence of IPV increased with age: 10.5% of 18–24-year-olds, 16.1% of 25–30-year-olds, 22.0% of 30–39-year-olds, and 21.8% of women older than 40 years reported any IPV (trend test, P<0.001; Figure 1). The trend persisted when stratifying by IPV severity: 7.1% of 18–24-year-olds, 11.7% of 25–30-year-olds, 12.8% of 30–39-year-olds, and 13.1% of women older than 40 years reported sometimes experiencing IPV (P<0.001), and 3.4% of 18–24-year-olds, 4.4% of 25–30-year-olds, 9.3% of 30–39-year-olds, and 8.8% of women older than 40 years reported frequently experiencing IPV (P<0.001). Figure 1 also shows the difference in the relationship between IPV prevalence and age when stratified by marital status. Patterns of IPV appeared to differ among each marital category, with the prevalence of IPV increasing with age among single women (trend test, P<0.001).
Figure 1.
Mean prevalence of IPV by age and marital status among study participants (n=2436).
The OR of IPV was 1.51 (95% CI 1.10–2.07) among married women, and 2.25 (95% CI 1.63–3.10) among divorced women when compared with single women and when age, education, employment, presence of children, urban residence, and HIV serostatus were held constant (Table 3). The predicted probability of IPV was 22.1% among married women as compared with 16.2% among otherwise identical single women (P<0.001). There was no difference in the regression model using IPV severity as the predicted outcome.
Table 3.
Multivariate analysis assessing the impact of HIV and sociodemographics on IPV among study participants
| Odds ratio | 95% CI | ||
|---|---|---|---|
| Marital status | |||
| Single | (ref) | ||
| Married | 1.51 | 1.10 | 2.07 |
| Divorced | 2.25 | 1.63 | 3.10 |
| Widowed | 1.13 | 0.78 | 1.65 |
| Age category, years | |||
| 18–24 | (ref) | ||
| 25–29 | 1.08 | 0.74 | 1.59 |
| 30–39 | 1.33 | 0.92 | 1.91 |
| 40+ | 1.28 | 0.88 | 1.87 |
| Education level | |||
| Less than secondary | (ref) | ||
| Secondary or higher | 1.02 | 0.77 | 1.36 |
| Employment status | |||
| Employed | (ref) | ||
| Unemployed | 1.80 | 1.28 | 2.52 |
| Any children | |||
| 0 | (ref) | ||
| ≥1 | 2.81 | 1.82 | 4.33 |
| Rural versus urban | |||
| Rural | (ref) | ||
| Urban | 1.25 | 1.00 | 1.57 |
| HIV status | |||
| HIV-seronegative | (ref) | ||
| HIV-seropositive | 0.98 | 0.75 | 1.28 |
Abbreviation: ref, reference category.
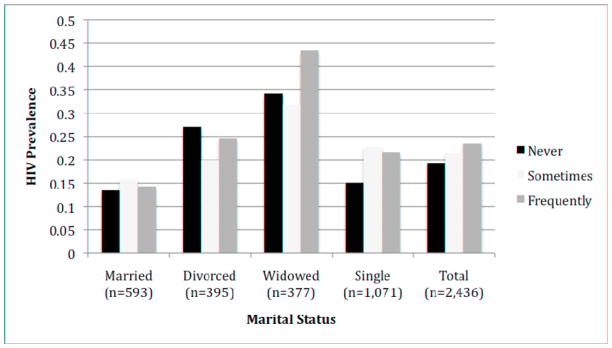
HIV seropositivity did not differ according to IPV exposure in univariate or multivariate analysis. When stratified by marital status, 22.4% of single women with a history of IPV were infected with HIV as compared with 15.1% without a history of IPV (P=0.041), resulting in 63% greater odds of HIV infection as compared with their unexposed counterparts (OR 1.63, 95% CI 1.01–2.61). The mean frequency of HIV seropositivity was 19.3% among those never having experienced IPV, 21.5% among those sometimes experiencing IPV, and 23.5% among those frequently experiencing IPV, although differences were not significant (Figure 2). When stratified by marital status, 43.5% of widowed women with the greatest severity of IPV were infected with HIV.
Figure 2.
Mean HIV prevalence by IPV severity and marital status among study participants (n=2436).
4. Discussion
In the present study of more than 2000 women presenting for HIV VCT in Moshi, Tanzania, nearly 1 in 5 women reported a lifetime occurrence of physical or sexual IPV, and over one-third of those affected frequently experienced violence. The prevalence of IPV varied significantly by marital status: married and divorced women reported the highest frequency and severity of IPV. Single women with a history of IPV were more likely to be infected with HIV than those without a history of IPV. Given that IPV has been linked with significant health consequences, VCT sites represent a unique opportunity to screen, counsel, and refer women who experience IPV.
The prevalence of lifetime IPV reported in the present study was lower than that reported elsewhere [3–6,8–10]. The use of general screening questions might have contributed to this result. Delineating specific examples of IPV might prompt respondents who otherwise do not consider their partner to be violent to answer in the affirmative. Moreover, women who have not previously been asked such questions might feel uncomfortable reporting IPV initially, but might feel more comfortable disclosing this history over time, particularly as individuals often present for repeat HIV testing at VCT centers. Lastly, underreporting of IPV is well known, and it is the sociocultural norm to accept IPV as part of a relationship in some African cultures [5,15,16].
The spectrum of risk factors for IPV reported so far suggests that, ultimately, every woman is at risk for IPV, and the sociodemographic risk factors that we identified contribute additional data characterizing the most vulnerable population of women. Marriage represents a significant risk factor for IPV and might represent an important risk stratifier for IPV screening. Differences in the predicted probabilities of IPV between married women and single women suggested that there is a 36.2% higher probability of IPV among married women, with as much as a quarter of IPV potentially occurring during marriage. Because IPV may be more common in married relationships, couples-based HIV VCT must be approached with care, because women might be at increased risk for IPV, both emotional and physical, around the time of testing and disclosure of serostatus to their partner [17–21]. Nevertheless, couples-based services also offer a unique opportunity for initial IPV counseling.
Several studies have described an association between IPV and HIV [8,10–12]. Violence can increase the risk of HIV transmission via coercion into sexual intercourse, decreased ability to negotiate the use of condoms, and increased sexual risk-taking behaviors [10–12,19,22]. Although we found an association between HIV seropositivity and IPV among single women, this relationship did not hold across all women. The high prevalences of HIV seropositivity and IPV in the community emphasize the importance for all women to be screened and considered at risk for both HIV and IPV.
As mentioned above, VCT centers represent an ideal setting for screening, counseling, and referring victims of IPV to support services, especially given the penetration of HIV testing in low-income countries [19]. Because VCT counselors gain the trust of their clients and ensure confidentiality, and because many women have little access to other avenues addressing IPV, screening for IPV would be appropriate and effective in this setting. VCT centers, many of which have strong ties to their community, can become prime locations for counseling women and can serve as a central point to connect victims of IPV to available medical, legal, and support services within the community. In addition, decreased adherence to antiretroviral treatment has been reported among HIV-infected women who have been victims of abuse [23]. As HIV prevention, care, and treatment venues in resource-poor settings expand to include other services, integration of screening, support, and services for IPV among HIV-infected women might prove important in ensuring better adherence to HIV care and treatment.
There are several limitations to the present study. First, because this was a cross-sectional analysis designed to gather information about risk factors for HIV, we were unable to determine whether IPV occurred in the current or prior relationship, marital status at the time of IPV, or the temporal relationship between IPV and HIV seroconversion. Second, we did not assess emotional abuse, which is intrinsic to the complex set of interactions surrounding IPV and which may be linked to HIV risk [11]. Third, because the study population comprised VCT clients at a women’s organization, where individuals might feel more comfortable reporting IPV, the results cannot be generalized to all women of northern Tanzania. Many of the same factors that are associated with IPV are also associated with HIV infection; therefore, it is likely that women presenting for HIV testing are those who are at higher risk for IPV and are more likely to report it.
Further studies at VCT centers should investigate the impact of screening and counseling victims of IPV with more detailed questions to establish the effectiveness of VCT as a site for routine screening [24]. Additional work to investigate the relationship between IPV and HIV testing or serostatus disclosure to the partner would greatly inform appropriate counseling strategies. VCT counselors would also require training in counseling victims of IPV and referring them to appropriate local support groups.
In the present study, 17.7% of women presenting for HIV VCT services reported a history of IPV. Violence against women is a violation of women’s basic rights, and screening for its occurrence is an important initial step in improving the health and lives of women. Because IPV is a common occurrence, and is both a risk factor for and a consequence of HIV, the ongoing expansion of HIV-testing services represents an ideal opportunity for screening, counseling, and referring women who are at risk for and victims of IPV.
Acknowledgments
The Duke VCT study was supported in part by the NIH Fogarty International Center through the International Clinical Research Fellows Program at Vanderbilt University (R24 TW007988; for MP, BM), the Fogarty International Center AIDS International Training and Research Program (D43 TW006732; for FM, BN, NT), the Duke Clinical Trials Unit and Clinical Research Sites (U01 AI06984; for NT), the International Studies on AIDS Associated Coinfections award (ISAAC; U01 AI-03-036; for FM, NT), and the Hubert-Yeargan Center for Global Health. The KIWAKKUKI–Duke VCT Study Group comprises the following additional individuals: John Bartlett (Duke Global Health Institute, Duke University, Durham, North Carolina, USA), John A. Crump (Duke Global Health Institute, Duke University, Durham, North Carolina, USA), Keren Landmann (Duke University Medical Center, Durham, North Carolina, USA), Anna Mgonja (KIWAKKUKI, Moshi, Tanzania), Antipas Mtalo (KIWAKKUKI, Moshi, Tanzania), Florida Muro (Kilimanjaro Christian Medical Centre, Moshi, Tanzania), Sabina Mtweve (Kilimanjaro Christian Medical Centre, Moshi, Tanzania), and Jeffrey Wilkinson (Duke University Medical Center, Durham, North Carolina, USA).
Footnotes
Conflict of interest
The authors have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Heise L, Ellsberg M, Gottmoeller M. A global overview of gender-based violence. Int J Gynaecol Obstet. 2002;78 (Suppl 1):S5–14. doi: 10.1016/S0020-7292(02)00038-3. [DOI] [PubMed] [Google Scholar]
- 2.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331–6. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO multi-country study on women’s health and domestic violence against women: summary report of initial results on prevalence, health outcomes and women’s responses. 2005 http://www.who.int/gender/violence/who_multicountry_study/en/. Published.
- 4.McCloskey LA, Williams C, Larsen U. Gender inequality and intimate partner violence among women in Moshi, Tanzania. Int Fam Plan Perspect. 2005;31(3):124–30. doi: 10.1363/3112405. [DOI] [PubMed] [Google Scholar]
- 5.Andersson N, Ho-Foster A, Mitchell S, Scheepers E, Goldstein S. Risk factors for domestic physical violence: national cross-sectional household surveys in eight southern African countries. BMC Womens Health. 2007;7:11. doi: 10.1186/1472-6874-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jewkes R, Levin J, Penn-Kekana L. Risk factors for domestic violence: findings from a South African cross-sectional study. Soc Sci Med. 2002;55(9):1603–17. doi: 10.1016/s0277-9536(01)00294-5. [DOI] [PubMed] [Google Scholar]
- 7.Borwankar R, Diallo R, Sommerfelt AE. Gender-based violence in sub-Saharan Africa: a review of Demographic and Health Survey findings and their use in National Planning. 2008 http://www.wilsoncenter.org/index.cfm?fuseaction=events.event_summary&event_id=517332.
- 8.Maman S, Mbwambo JK, Hogan NM, Kilonzo GP, Campbell JC, Weiss E, et al. HIV-positive women report more lifetime partner violence: findings from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. Am J Public Health. 2002;92(8):1331–7. doi: 10.2105/ajph.92.8.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karamagi CA, Tumwine JK, Tylleskar T, Heggenhougen K. Intimate partner violence against women in eastern Uganda: Implications for HIV prevention. BMC Public Health. 2006;6:284. doi: 10.1186/1471-2458-6-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lary H, Maman S, Katebalila M, McCauley A, Mbwambo J. Exploring the association between HIV and violence: young people’s experiences with infidelity, violence and forced sex in Dar es Salaam, Tanzania. Int Fam Plan Perspect. 2004;30(4):200–6. doi: 10.1363/3020004. [DOI] [PubMed] [Google Scholar]
- 11.Andersson N, Cockcroft A, Shea B. Gender-based violence and HIV: relevance for HIV prevention in hyperendemic countries of southern Africa. AIDS. 2008;22 (Suppl 4):S73–86. doi: 10.1097/01.aids.0000341778.73038.86. [DOI] [PubMed] [Google Scholar]
- 12.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–8. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 13.Chu HY, Crump JA, Ostermann J, Oenga RB, Itemba DK, Mgonja A, et al. Sociodemographic and clinical characteristics of clients presenting for HIV voluntary counselling and testing in Moshi, Tanzania. Int J STD AIDS. 2005;16(10):691–6. doi: 10.1258/095646205774357307. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. WHO Multi-Country Study on Women’s Health and Life Experiences: Core Questionnaire (Version 10) Geneva, Switzerland: World Health Organization; 2003. http://whqlibdoc.who.int/publications/2005/924159358X_annex3-4_eng.pdf. [Google Scholar]
- 15.Speizer IS. Intimate partner violence attitudes and experience among women and men in Uganda. J Interpers Violence. 2010;25(7):1224–41. doi: 10.1177/0886260509340550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Bureau of Statistics. Tanzania: DHS, 2004–05 – Final Report (English) 2005 http://www.measuredhs.com/pubs/pub_details.cfm?ID=566. Published.
- 17.Becker S, Mlay R, Schwandt HM, Lyamuya E. Comparing couples’ and individual voluntary counseling and testing for HIV at antenatal clinics in Tanzania: a randomized trial. AIDS Behav. 2010;14(3):558–66. doi: 10.1007/s10461-009-9607-1. [DOI] [PubMed] [Google Scholar]
- 18.Allen S, Karita E, Chomba E, Roth DL, Telfair J, Zulu I, et al. Promotion of couples’ voluntary counseling and testing for HIV through influential networks in two African capital cities. BMC Public Health. 2007;7:349. doi: 10.1186/1471-2458-7-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med. 2000;50(4):459–78. doi: 10.1016/s0277-9536(99)00270-1. [DOI] [PubMed] [Google Scholar]
- 20.Kiarie JN, Farquhar C, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Domestic violence and prevention of mother-to-child transmission of HIV-1. AIDS. 2006;20(13):1763–9. doi: 10.1097/01.aids.0000242823.51754.0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gielen AC, McDonnell KA, Burke JG, O’Campo P. Women’s lives after an HIV-positive diagnosis: disclosure and violence. Matern Child Health J. 2000;4(2):111–20. doi: 10.1023/a:1009522321240. [DOI] [PubMed] [Google Scholar]
- 22.van der Straten A, King R, Grinstead O, Vittinghoff E, Serufilira A, Allen S. Sexual coercion, physical violence and HIV infection among women in steady relationships in Kigali, Rwanda. AIDS Behav. 1998;2(1):61–73. [Google Scholar]
- 23.Cohen MH, Cook JA, Grey D, Young M, Hanau LH, Tien P, et al. Medically eligible women who do not use HAART: the importance of abuse, drug use, and race. Am J Public Health. 2004;94(7):1147–51. doi: 10.2105/ajph.94.7.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization. Putting women first: ethical and safety recommendations for research on domestic violence against women. 1999 http://www.who.int/gender/violence/womenfirtseng.pdf. Published.