Abstract
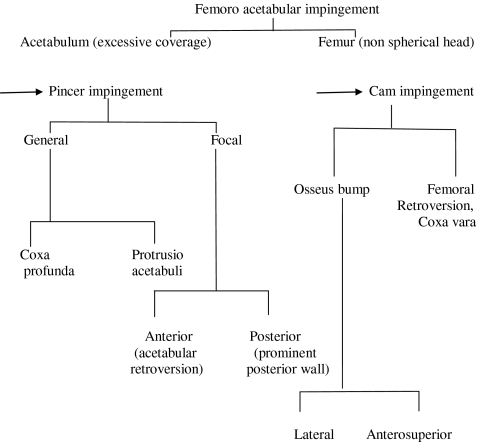
Hip pain in adults has traditionally been associated with osteoarthritis in the joint. However, many young patients with hip pain do get referred to orthopaedic surgeons without arthritis. Subtle bony and soft tissues abnormalities can present with hip pain in the active young adult. These abnormalities can lead to premature arthritis. With the improvements in clinical examination for hip impingement, radiological imaging using magnetic resonance arthrography (MRA) and or computed tomograms (CT) Scans, these lesions are being detected early. Though the cause of primary osteoarthritis is unknown, it is suggested that femoro-acetabular impingement (FAI) may be responsible for the progression of the disease in these patients. FAI is a pathological condition leading to abutment between the proximal femur and the acetabular rim. Two different mechanisms are described, although a combination of both is seen in clinical practice. Cam impingement is a result of reduced anterior femoral head neck offset. Pincer lesion is caused by abnormalities on the acetabular side. FAI due to either mechanism can lead to chondral lesions and labral pathology. Patients present with groin pain and investigated with radiographs, CT and MRA. Surgery is the treatment of choice. Open or arthroscopic exploration of the hip is undertaken with bony resection to improve the femoral head neck junction with resection or repair of the damaged labrum. This may involve femoral osteochondroplasty for the cam lesion and acetabular rim resection for pincer lesion. There is no difference in outcome between open and arthroscopic surgery for FAI.
Keywords: Femoro-aecetabular, Impingement, Hip, Young adults, Cam, Pincer
Introduction
Hip pain in young adults can represent a diagnostic challenge. Important features to elicit from the history include developmental dysplasia, trauma or predisposing factors of avascular necrosis. Some individuals have morphological abnormalities in the shape of the femur or the acetabulum [1]. Over recent years, improvements and increasing availability of imaging modalities has led to a better understanding of hip pathologies. The use of magnetic resonance imaging has helped to improve the diagnosis of soft tissue causes of hip pain, such as labral pathology. Consequently, a host of morphological abnormalities to the femoral neck and acetabulum have been termed “femoro-acetabular impingement” (FAI). Femoro-acetabular impingement is defined as the abutment between the proximal femur and the acetabular rim [2]. Abnormal hip morphology has been recognised as an important cause of early osteoarthritis of the hip [3]. This review will discuss the anatomical perspectives, clinical presentations and the current treatment options of femoro-acetabular impingement.
Anatomical perspectives
Mayer et al. (1999) first described FAI as an entity while assessing a series of patients with progressive pain after peri-acetabular osteotomy for hip dysplasia [4]. Stulberg et al. (1975) was first to identify the fundamental association of an abnormal proximal hip morphology and subsequent idiopathic degenerative arthritis of the hip [5]. They described abnormal head and neck clearance in patients with primary osteoarthritis of the hip. Stulberg called this ‘pistol grip deformity’ (Fig. 1). His theory was supported by Harris (1986) who reported the presence of subclinical childhood disease and abnormal bony morphology in 90% patients with primary osteoarthritis of the hip [6]. Furthermore, Tanzer et al. (2004) and Bardakos et al. (2009) supported strong evidence linking FAI and osteoarthritis of the hip [7, 8].
Fig. 1.
Anteroposterior (AP) radiograph showing pistol grip deformity (arrow)
Morphological variations to the hip joint associated with Femoro-acetabular impingement [9, 10]
The normal anatomy of the hip joint consists of the following:
The femoral head is slightly more than half a sphere
The femoral neck is cylindrical, narrowest in the midpoint and widest laterally and attaches the head to the shaft
The acetabulum is cup shaped
The labrum is triangular in cross section with its base attached to the acetabular rim
Recognised anatomical variations are as follows:[10]
The femoral head is conchoid shape
The position of the head in relation to the neck may be central (along the geometric axis of the neck axis) or may be displaced (inferior and posterior to the neck axis)
The head neck junction is concave
This concavity ensures anterior superior head neck clearance without impingement
The articular cartilage is thickest antero superiorly in the acetabulum and antero laterally in the femoral head
The fibrocartilagenous labrum is triangular in cross section with its base attached to the acetabular rim and the free margin covering the femoral head
The central arm of the labrum is covered with articular cartilage which is continuous with that of the lunate surface in the acetabulum
- The role of the labrum is as follows:
- Shock absorber
- Fluid seal for the hip joint, which enhances joint stability Disruption of the fluid seal, can make the joint unstable
- Nociceptive and proprioceptive function
Pathogenesis of femoro-acetabular impingement
The hip joint is a ball and socket joint. The principle function of the hip is to enable weight bearing for locomotion. Despite normal bony geometry, impingement can occur at extremes of movement. Abnormal morphologies of the hip or increased level of activities can aggravate the situation, resulting in frequent and often symptomatic impingement in the hip joint [1].
Normally, space is maintained between the femoral head neck junction and the acetabular rim provides unhindered hip movement. This is achieved with an offset between the anterior and superior surface of the femoral neck and the corresponding surface of the femoral head. The normal head neck offset is 9 mm [1, 2].
A deviation from this anatomical relationship may predispose mechanical blockage at extremes of hip movement. Other factors which may influence impingement includes a pistol grip deformity with reduced femoral neck offset in antero lateral aspect of head neck junction, reduced femoral anteversion and loss of spherecity in the femoral head [1, 2].
On the other hand, excessive coverage or retroversion of the acetabulum will affect the normal spatial relationship between the femoral head and the acetabulum. Retroversion of the acetabulum causes over-coverage and restricts flexion of the femoral neck. Coxa profunda deformity (the floor of the acetabulum touches the ilio-ischial line) increases the relative depth of the acetabulum and may predispose to impingement. The site of the acetabular abnormality is in the supero medial area of the rim [11].
Patients with normal hip morphology can suffer from impingement due to extreme range of movement in their hip joint [12]. However, in patients with altered morphology of the femoral head or the acetabulum, less motion is required before abutment between the neck and acetabulum occurs [3]. Hence, FAI is essentially a dynamic problem (Table 1).
Table 1.
Pathogenesis of FAI
Spinal impact of hip joint pathology is well known. However, this has not always well analysed or taken into account while pathogenesis of FAI is considered. Legaye et al. [13] reported that anterior pelvic plane (APP) and acetabular orientation are influenced by the sagittal balance of the spine. The APP is defined by the line joining the both anterior superior iliac spines (ASIS) and the pubic symphysis. APP is normally assumed to be vertical. The authors compared validated radiographic angles including the sagittal anterior pelvic plane (SAPPA) which measures the angle between the vertical and the APP to analyse the sagittal balance of the spine in two groups with and without back pain. There was significant increase (P < 0.001) in the sagittal tilt of APP compared to normal subjects (the APP was almost vertical).There was a strict relation between the SAPPA and the disturbance of the sagittal balance of the spine. This study showed that a sagittal rotation of the pelvis and a consequent tilt of the APP can result from perturbations in the spinal stability. This in turn can cause acetabular mal rotation and result in femoro-acetabular impingement.
Acetabular version is known to be dependent on the sacral slope. Increase in the sacral slope is known to cause greater acetabular retroversion on the frontal radiographs. Husson et al. [14] investigated the role of abnormal sagittal pelvic balance in FAI using radiographs of standing lateral view of the pelvis. They failed to demonstrate any anatomic or static abnormality of the pelvic sagittal balance in standing position associated with FAI. Moreover, there was no correlation between the pelvic tilt or cam lesions as measured with alpha angles indicating pelvic balance takes precedence over anatomic abnormalities.
Natural history
FAI occurs as a result of contact between a widened femoral neck and a decreased offset at the head neck junction [15]. The repetitive contact between the femoral neck and the acetabular rim causes damage to acetabular cartilage leading to labral tears manifesting as anterior hip pain and progression to early osteoarthritis of the hip. Two main causes of FAI have been described cam and pincer lesions [2, 3].
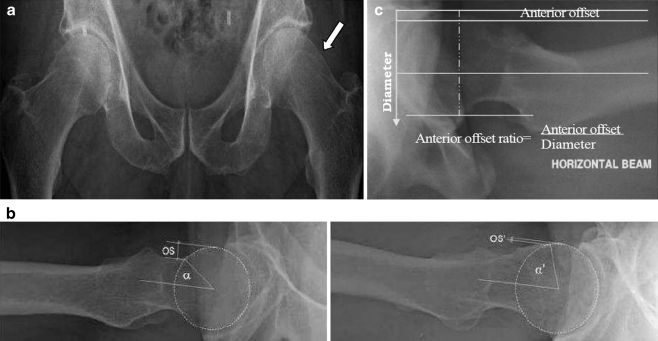
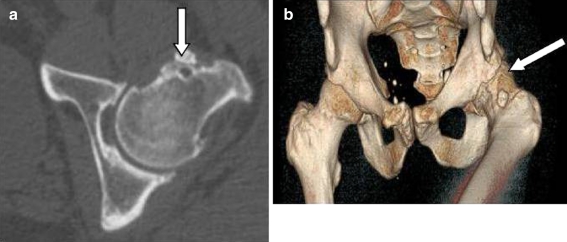
Cam lesions (Fig. 2)
Fig. 2.
(a) AP radiograph demonstrating cam lesion. (b) Cross table lateral radiograph showing normal alpha angle and normal head neck offset (left) and increased alpha angle with reduced head neck offset in cam lesion (right). (c) Cross table lateral view demonstrating calculation of the anterior offset ratio (AOR)
Cam lesions are more common in young active men. The cam is attributed to a nonspherical portion of the femoral head abutting against an acetabular rim. This abutment is most evident in flexion and internal rotation. This causes an outside-in abrasion of the acetabular cartilage with avulsion from the labrum and subchondral bone. This can lead to separation of the cartilage from the antero superior aspect of the labrum [11, 15].
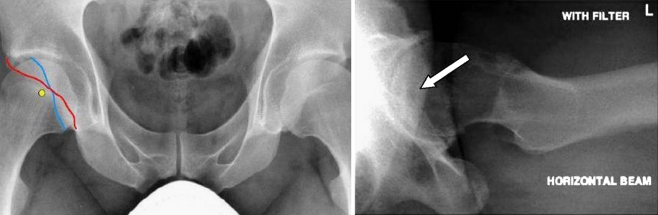
Pincer lesions (Fig. 3)
Fig. 3.
AP (left) and cross table lateral (right) radiographs in a hip with pincer lesion. Note the cross over sign in the AP (coloured lines) and lateral views (arrow). The ischeal spines are prominent in the AP radiograph
Pincer lesions are more common in middle-aged active women. They occur through repeated contact between a normal femoral head neck junction and an over covered acetabular rim. This results in labral degeneration, intra-substance ganglion formation, ossification of the acetabular rim, and deepening of the acetabulum. Unlike in cam lesions, the chondral damage is more circumferential [3, 16]. It is to be noted that spinal deformities like scoliosis or kyphosis can cause pelvic rotation and functional retroversion of the acetabulum which may act as a pincer lesion .Prior femoral neck fractures or pelvic osteotomy also cause impingement.
Cam and pincer lesions rarely occur in isolation. The most common type of FAI occurs from mixed cam and pincer pathology at the anterior femoral neck and anterior superior acetabular rim. Cobb et al. (2010) argued against this, after analyzing the morphology of 60 acetabula with CT scans. They reported that acetabula with cam hips were shallower than normal hips, which in turn were shallower than pincer hips (84° ± 5° versus 87° ± 4° versus 96° ± 5° respectively). Hence, they concluded, that cam and pincer lesions were different patho-anatomic entities with cam hips being shallow while the pincer hips are deeper than normal hips [17]. Allen et al. (2009) reported 113 (201 hips) patients with cam lesions of which 88(77.8%) had bilateral lesions [18].
Histologically, FAI is characterised by a chronic inflammation of the labrum located at the site of rupture and elicits a degenerative reaction. Ito et al. (2004) reported no histopathological difference in the labrum between cam and pincer lesion [19].
Risk factors
Cam lesions result from conditions that reduce the anterior head neck offset (Table 2) [3].
Table 2.
Causes of Cam lesions
| Idiopathic |
| Developmental |
| - Non spherical femoral head |
| - Coxa vara |
| Traumatic |
| - Malunited femoral neck fracture |
| - Post traumatic retro version of the femoral head |
| Childhood orthopaedic conditions |
| - Perthes disease |
| - Slipped capital femoral epiphysis |
| Iatrogenic |
| - Femoral osteotomy |
Pincer lesions may be due to acetabular retroversion where the antero lateral acetabular edge obstructs flexion or coxa profunda where the relative depth of the acetabulum is increased (Table 3) [2].
Table 3.
Causes of pincer lesion
| Idiopathic |
| Developmental |
| - Retroverted acetabulum |
| - Coxa profunda |
| - Os Acetabuli |
| - Protrusio acetabuli |
| - Chronic residual dysplasia of the acetabulum |
| Traumatic |
| - Post traumatic deformity of the acetabulum |
| Iatrogenic |
| - Over correction of retroversion in dysplastic hips |
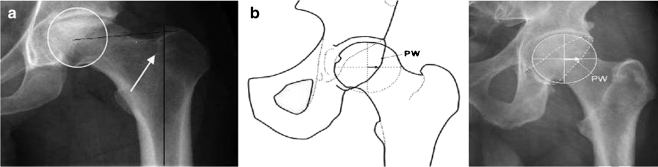
In demonstrating a link between FAI and hip osteoarthritis, Bardakos et al. (2009) identified two statistically significant predictive factors that influenced early progression to osteoarthritis [7].
Firstly, a reduced medial proximal femoral angle (MPFA) can be seen in the AP view radiographs (Fig. 4a). A varus deformity of the femoral neck is associated with a reduced medial proximal femoral angle, which was postulated to cause biomechanical imbalance, reduced abduction and early osteoarthritis.
Fig. 4 (a & b).
AP radiograph (left) demonstrating measurement of medial proximal femoral angle (MPFA) and the presence of posterior wall sign (middle schematic diagram and right radiograph)
Second is the presence of a posterior wall sign. This is defined as the centre of the femoral head being located lateral to the outline of the posterior acetabular rim on the AP view (Fig. 4b).
Of these two factors, they found the MPFA (odds ratio 18.7) to be more predictive for progression to osteoarthritis than the posterior wall sign, (odds ratio 10.2) with FAI.
Clinical symptoms and signs
Insidious onset of symptoms in active young and middle aged adults
Groin pain associated with activity and no prior history of trauma
Inability to perform activities such as high hip flexion or prolong sitting
Painful clicking, locking or instability from a labral tear secondary to undiagnosed FAI
Reduced range of motion especially flexion, adduction and internal rotation
Impingement tests
-
This test is positive if one elicits pain on adduction of a flexed, internally rotated hip with the patient supine.
-
Flexion Abduction External Rotation (FABER) provocation test [21]
With the hip in flexion, abduction and external rotation, abutment of the labrum and cartilage also can occur. The test is positive if it elicits similar pain as complained by the patient or if the distance between the lateral knee and the exam table differs between the symptomatic and contra lateral hip.
-
Posterior inferior impingement test [12]
With the hip in hyper extension, passively by hanging the leg over the end of the bed, the affected hip is passively externally rotated. The test is positive if it elicits similar pain as complained by the patient.
Investigations
Plain radiographs
Siebenrock et al. [22] described standardised radiograph criteria to obtain adequate anteroposterior (AP) radiographs in patients with suspected FAI. The coccyx should point directly over the symphysis pubis, documenting absence of rotation. The distance between the sacrococcygeal joint is on average 47 mm in women and 32 mm in men, denoting a neutrally rotated pelvis. The ideal distance between the tip of the coccyx and superior pubic symphysis should be 4 cm to 5 cm. This distance allows satisfactory assessment of anterior and posterior walls of the acetabulum, determining if a retroverted acetabulum is present or simply pincer-based impingement. Plain film radiographic studies indicated include AP pelvis view, as well as cross-table lateral view of the affected hip .It is beneficial to induce 10° to 15° of internal rotation into the lateral to compensate for femoral anteversion. Elimination of the anteversion provides optimal visualization of a cam impingement lesion.
The AP view should be assessed for evidence of the cam type deformity (flattened head–neck junction, pistol grip deformity), degenerative changes (Fig. 5a) and a profunda socket (Fig. 5b). A crossover sign may be observed indicating a prominent anterior acetabular wall, or acetabular retroversion.
Fig. 5.
(a & b) AP radiograph showing a cam deformity with degenerative changes in the hip (left) and coxa profanda socket in the acetabulum (right). (c) Cross table lateral radiographs showing fibrocystic changes at the head neck junction (arrow) indicating dynamic hip impingement (foot print of FAI)
The standard lateral view will reveal subchondral sclerosis and early subchondral cyst formation of the anterior acetabular rim and the cross-table true lateral will profile cam deformity or lack of concavity and reactive fibro cystic changes at the anterior head neck junction (Fig. 5c).
There may be signs of ossification of the acetabular rim or presence of os acetabulare. The general findings may include coxa vara, coxa valga, coxa profunda, and protrusio acetabulare or hip dysplasia.
Meyer et al. [23] compared different radiographic projections to assess femoral head neck aspherecity. The authors reported variations in the alpha angles according to the projection. They found that the Dunn view (AP of hip in neutral rotation, 45° of flexion and 20° of abduction) or a cross table projection in internal rotation is best to assess femoral head neck aspherecity while anteroposterior or externally rotated cross table views were least likely to detect these abnormalities.
Radiological measurements
Head neck offset (Fig. 2b)—the difference between the anterior radius of the femoral head and the anterior radius of the femoral neck on the lateral view. Values of less than 7 mm are considered abnormal. Clohisy et al. (2007) found a mean anterior offset of 6.6 mm for hips with impingement versus 9.3 mm for control [24].
-
Alpha Angles (Fig. 2b)—the angle the femoral neck axis and a line connecting the centre of the femoral head to the point of commencement of femoral head flattening. The average alpha angle in cam deformity is 65–70° compared to 42–47° in normal femur [8]. The alpha angle can also be measured in computed tomograms (CT) or magnetic resonance imaging (MRI) scans. Allen et al. (2009) reported a correlation between and the alpha angle and symptomatic cam lesions (Fig. 2) [18]. The alpha angle was significantly lower in females. The ratio of right to left side involvement in patients with unilateral was 2.5:1. Forty two percent patients with cam lesion had concomitant pincer lesion. Acetabular retroversion was present in 53 hips and coxa profunda in 45 hips. Barros et al. reported 82% patients with idiopathic osteoarthritis of the hip have larger alpha angles in the affected hip when compared to 30% those who do not [25].
The increased prevalence of cam in men and pincer in women (increased alpha angle in man) has also been shown by Ranawat et al. [26]. The authors found poor correlation between pain and radiographic finding of FAI.
Anterior offset ratio (AOR) (Fig. 2c)—is calculated by first drawing a line along the central axis of the neck, which does not necessarily pass through the centre of the femoral head [10]. Parallel lines are then drawn along the anterior cortex of the neck and along the anterior outer part of the femoral head. The perpendicular distance between these latter two lines is the anterior offset. The anterior offset ratio (AOR) is calculated by dividing the anterior offset by the diameter of the femoral head. The mean AOR was 0.19 with a 95% confidence interval of 0.18–0.20, suggesting a lower limit of the reference interval of 0.14 [27].
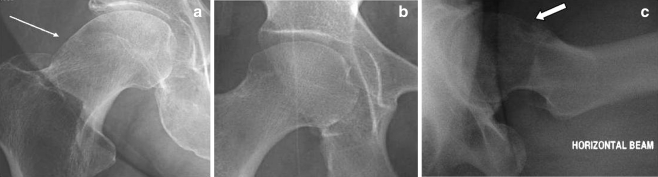
Magnetic resonance arthrography (MRA) (Fig. 6a and b)
Fig. 6.
(a) Coronal sections from magnetic resonance arthrogram (MRA) showing extrusion of radio opaque dye (arrow) at the site of labral tear. (b) Coronal section from magnetic resonance arthrogram (MRA) showing further extravasation of dye (arrow) through the torn labrum
If labral pathology is suspected, MR arthrography is the preferred investigation. Scans will show articular cartilage thinning, but the contrast medium will seldom penetrate beneath delaminating articular cartilage and the extent of peripheral articular cartilage instability may be underestimated.
Notzli et al. (2002) compared MR images in 39 patients with FAI with 35 asymptomatic control subjects [28]. They measured the non spherical shape of the femoral head–neck junction by measuring the alpha angle. The average alpha angle was 74° in patients with FAI and 42° in control subjects (P 0.001). They proposed an alpha angle of 55° or more was diagnostic of FAI.
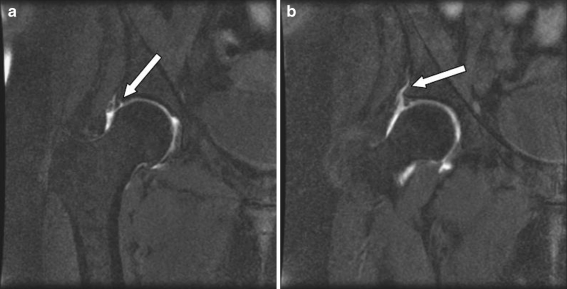
Position of discomfort (POD) Computer tomography (CT) scans (Singh et al. 2009) [29]
If the shape of the femoral head neck junction needs to be assessed for the presence of a Cam deformity, CT 3D surface reconstructions allow the lesion to be visualised and surgical resection planned (Fig. 7).
Fig. 7.
Three-dimensional reconstruction of Computed Tomography (CT) hip showing pre operative plan with marking of the area in the head neck junction (red circle) to be resected
A new CT view has been developed by Pritchard and O’Donnell to demonstrate FAI lesions. CT scanning in the position of discomfort (POD view) allows symptomatic cam deformity to be accurately mapped in a three dimensional reconstruction. This procedure helps in diagnosis of the problem by visualisation and subsequent planning for surgical resection.
Figure 8a shows an axial CT scan through the hip of a patient with a typical clinical signs of femoro-acetabular impingement. A fibrocystic impingement lesion of the anterior head neck junction is seen but no evidence of joint space compromise. In Fig. 8b, the same hip has been scanned in the POD position (patient supine with the hip flexed, adducted and internally rotated). The scan reveals the impingement lesions and narrowing if joint space indicating mechanical impingement.
Fig. 8 (a & b).
CT scans in position of discomfort (CT POD). Note the footprint of FAI in the coronal section with the hip in normal position (left) and dynamic impingement in position of discomfort best demonstrated with 3-D reconstruction of the CT images (right)
It is to note that CT scans in POD view best demonstrates a bony impingement lesion. To visualise labral pathology or other soft tissue injuries in the hip, an MRI or MR arthrogram is better suited.
Management options
Non operative management
Initial non-operative management such as modification of activities, avoiding excessive hip movement and regular non-steroidal anti-inflammatory agents can provide symptomatic relief. Discontinuation of sport or recreational activities is helpful; however, this is often unacceptable to young individuals.
Therefore, surgical intervention is a more realistic option. Physiotherapy has no role in management of FAI and hence not recommended [30].
Operative management
The aim of surgery is to remove the mechanical obstruction of the proximal femur against the acetabular rim [31]. It is important to address the associated labral tear and any other consequential articular damage. Both open surgical techniques and arthroscopic treatment have been described.
Open surgical procedures involve dislocating the hip anteriorly while taking care to minimise trauma to the blood supply to the femoral head. A trochanteric flip osteotomy is performed to improve the exposure. This enables a 360° view of the head neck junction. Any mechanical impingement of the head neck junction deemed to cause impingement is directly visualised and can be excised to restore the normal concave contour of the femoral neck junction. The complications include avascular necrosis of the femoral head and neck of femur fracture [32]. Mardones et al. suggested that the risk of femoral neck fracture was significantly high if more than 30% of the antero lateral quadrant of the head neck junction is resected [33].
Pronounced retroversion of the acetabulum can be dealt with by resection of the prominent anterior acetabular rim [4]. Alternatively, a peri-acetabular osteotomy to reorient the acetabulum has been published [34]. However, care should be taken to avoid over-correction as this may lead to iatrogenic impingement [35]. If there is adequate posterior cover, an excision osteoplasty may be preferred. Any labral tear should be treated with resection or repair as appropriate [12].
Combined arthroscopic examination and limited open procedures via Smith Peterson approach or Huetter anterior approach have been described Clohisy et al. 2005 [36]. Arthrotomy and debridement can be carried out in situ for a cam lesion. This is not a very popular approach at present.
An increasing number of surgeons are treating FAI arthroscopically. Arthroscopic management comprises of the examination of the central and peripheral compartments [37]. The central compartment refers to the structures medial to the labrum. All structures outside the labrum but inside the hip capsule fall in the peripheral zone. The procedure is performed with the patient in a supine or lateral decubitus position. A specialised traction device is used for arthroscopic procedures in the central zone. No traction is needed for lesions of the peripheral zone procedures. The joint is first filled with normal saline via a spinal needle inserted under image intensifier guidance. Two to three standard portals anterior, antero lateral or postero lateral can be used [38, 39].
The procedures achieved by hip arthroscopy at present include
Debridement of labral tear
Repair of torn labrum
Chondroplasty of acetabular lesions
Drilling or micro fracture of acetabular lesions
Acetabular rim excision
Debridement of acetabular chondral delamination
Capsular excision
Femoral osteochondroplasty
Outcome of surgical management
Bedi et al. published a systemic review on surgical outcome of operative management of FAI [40]. A review of patients suffering from FAI who were treated with open surgical procedures revealed 65% to 94% good to excellent outcomes (n = 194 and mean follow up was 40 months). These procedures included primarily labral debridement and osteoplasty. There was a good correlation between patient satisfaction and favorable outcome as defined by Harris hip scores or Merle d’Aubigne score. The failure rate, as defined by a dissatisfied patient and or conversion to total hip replacement ranged from 4% to 30% highest in patients with pre-existing ostearthritis.
The arthroscopic series collectively assessed 271 patients with a mean follow up of 26 months. A range of 67% to 93% good to excellent outcomes was reported. Arthroscopic labral tear repair combined with treatment for FAI proved very effective with 93% patients able to return to sports and 78% active at 1.5 years after surgery. The failure rate, as defined by a dissatisfied patient or conversion to total hip replacement, ranged from 1% to 33%.
However, of the 16 articles that were reviewed, none were level I or II studies. Only one study met the criteria for level III evidence. The rest were reported case series (level IV evidence). Nine out of the 16 studies used a validated outcome measure. The authors concluded that with this limited data, there was no clinical difference in the outcome after open or arthroscopic management of FAI. It is important to remember that associated problems in the hip such as untreated dysplasia, subluxation or arthritis render the outcome of FAI surgery less favourable [41]. Early failure, needing conversion to hip arthroplasty, is common in patients with extensive articular cartilage delamination at the time of the procedure. In hips with osteoarthritis of grade II or above, a debridement procedure has proved ineffective [42].
Byrd et al. reported 10 years follow up results in 29 patients (31 hips) that underwent arthroscopic resection of a labral tear [43]. Eighty three percent of patients without arthritis at the time of surgery had improved equal to or more than 18 points in Harris hip score at 10 years, whereas 88% patients who had arthritis at the time of surgery had to undergo a total hip replacement after mean duration of 63 months.
Conclusion
Awareness and understanding of FAI has become more widespread over recent years, with improvement in imaging modalities. This has led to the development of effective treatment of young active adults who were previously under diagnosed or in whom no effective treatment were available. Open or arthroscopic interventions are now relatively common enabling patients to get back to activities whilst minimising their predisposition to osteoarthritis.
Acknowledgments
Funding We did not receive any funding for writing this article.
Competing interests We are not aware of any conflict of interest on writing this article.
References
- 1.Hossain M, Andrew JG. Current management of femoroacetabular impingement. Curr Orthop. 2008;22:300–310. doi: 10.1016/j.cuor.2008.07.011. [DOI] [Google Scholar]
- 2.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Ortop. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage. J Bone Joint Surg Br. 2005;87-B:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 4.Mayers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Ortop. 1999;363:93–99. [PubMed] [Google Scholar]
- 5.Stulberg SD, Cordell LD, Harris WH, et al. Unrecognised childhood disease: a major cause of idiopathic osteoarthritis of the hip. The Proceedings of the Third Open Scientific Meeting of the Hip Society.St Louis, MO:CV Mosby;1975:212–2
- 6.Harris WH. Aetiology of osteoarthritis of the hip. Clin Orthop. 1986;213:20–33. [PubMed] [Google Scholar]
- 7.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91-B:162–169. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 8.Tanzer M, Noiseux N. Osseus abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop. 2004;429:170–177. doi: 10.1097/01.blo.0000150119.49983.ef. [DOI] [PubMed] [Google Scholar]
- 9.Crawford MJ, Dy CJ, Alexander JW, Thompson M, Schroder SJ, Vega CE, et al. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007;465:16–22. doi: 10.1097/BLO.0b013e31815b181f. [DOI] [PubMed] [Google Scholar]
- 10.Eijer H, Leunig M, Mohamed N, et al. Cross table lateral radiographs for screening of anterior femoral head neck offset in patients with femoro acetabular impingement. Hip Int. 2001;11:37–41. [Google Scholar]
- 11.Ito K, Minka II, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect: a MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint [Br] 2001;83-B:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 12.Crawford J, Villar R. Current concepts in the management of femoroacetabular impingement. J Bone Joint Surg Br. 2005;87-B:1459–1462. doi: 10.1302/0301-620X.87B11.16821. [DOI] [PubMed] [Google Scholar]
- 13.Legaye J. Int Orthop. 2009;33:1695–1700. doi: 10.1007/s00264-008-0702-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Husson JL, Mallet JF, Huten D, Odri GA, Morin C, Parent HF. The lumbar-pelvic-femoral complex:applications in hip pathology. Orthop Traumatol Surg Res. 2010;96S:S10–S16. doi: 10.1016/j.otsr.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Beaule PE, Zaragoza EJ, Motamedic K, Copelan N, Dorey J. Three dimensional computed tomography in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23:1286–1292. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 16.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The aetiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cobb J, Logishetty K, Davda K, Iranpour F. Cams and pincer impingement are distinct. Not mixed. The acetabular pathomorphology of femoroacetabular impingement. Clin Orthop Relat Res. 2010;468:2143–2151. doi: 10.1007/s11999-010-1347-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allen D, Beaulé P, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91-B:589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 19.Ito K, Kahlnor M, Leunig M, Ganz R. Hip morphology influences the pattern of femoro acetabular impingement. Clin Orthop. 2004;429:262–271. doi: 10.1097/01.blo.0000144861.11193.17. [DOI] [PubMed] [Google Scholar]
- 20.Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041–1047. doi: 10.1007/s00167-007-0348-2. [DOI] [PubMed] [Google Scholar]
- 21.Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25(2):299–308. doi: 10.1016/j.csm.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 23.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck aspherecity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 24.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog leg radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 25.Barros HJ, Camanho GL, Bernabé AC, Rodrigues MB, Leme LE. Femoral head–neck junction deformity is related to osteoarthritis of the hip. Clin Orthop Relat Res. 2010 Jul;468:1920–5. [DOI] [PMC free article] [PubMed]
- 26.Ranawat AS, Schulz B, Baumbach SF, Meftah M, Ganz R, Leunig M. Radiographic predictors of hip pain in femoroacetabular impingement. HSS Journal. Online First™, 10 January 2011 (in press). [DOI] [PMC free article] [PubMed]
- 27.Pollard T, Villar R, Norton M, Fern D, Williams M, Simpson D, et al. Femoroacetabular impingement and classification of the cam deformity: the reference interval in normal hips. Acta Orthop. 2010;81(1):134–141. doi: 10.3109/17453671003619011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head–neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 29.Singh PJ, Pritchard M, O’Donnell J. The POD CT scan—a better way to demonstrate FAI and early hip degeneration. Annual Scientific Meeting. International Society for Hip Arthroscopy; Oct 2009.
- 30.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. doi: 10.1097/00003086-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Byrd T, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739–746. doi: 10.1007/s11999-008-0659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 33.Mardones RM, Gonzalez C, Chen Q, Zobitz M, Kaufman KR, Trousdale RT. Surgical treatment of femoroacetabular impingement: evaluation of the effect of the size of the resection. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 1):84–91. doi: 10.2106/JBJS.E.01024. [DOI] [PubMed] [Google Scholar]
- 34.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85-A(2):278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Lever C, O’Hara J. Young adult hip disease: hip morphology and impingement. Curr Orthop. 2008;22:414–421. doi: 10.1016/j.cuor.2008.08.003. [DOI] [Google Scholar]
- 36.Clohisy JC, McClure JT. Treatment of anterior femoroacetabular impingement with combined hip arthroscopy and limited anterior decompression. Iowa Orthop J. 2005;25:164–171. [PMC free article] [PubMed] [Google Scholar]
- 37.Sampson TG. Arthroscopic treatment of femoroacetabular impingement. Tech Orthop. 2005;20:156–162. [PubMed] [Google Scholar]
- 38.Byrd JW. Hip arthroscopy by the supine approach. Instr Course Lect. 2006;55:325–336. [PubMed] [Google Scholar]
- 39.Smart LR, Oetgen M, Noonan B, Medvecky M. Beginning hip arthroscopy: indications, positioning, portals, basic techniques, and complications. Arthroscopy. 2007;23(12):1348–1353. doi: 10.1016/j.arthro.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 40.Bedi A, Chen N, Robertson W, Kelly B. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24:1135–1145. doi: 10.1016/j.arthro.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 41.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 42.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 43.Byrd JW, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25(4):365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]