Abstract
Lymphangioma of the colon is a relatively rare non-epithelial tumor and usually presents as a submucosal polypoid lesion. Many cases incidentally discovered are usually asymptomatic. However, they may present as abdominal pain or bleeding, and their resection is normally required. Lymphangioma itself is generally recognized as a benign tumor and no cases of malignant transformation have yet been reported, although its natural history is currently unknown. To the best of our knowledge, this study is the first to describe a case of spontaneous resolution in multiple colonic lymphangiomas without any specific treatment.
Keywords: Lymphangioma, Colon, Natural history
INTRODUCTION
Lymphangioma is a benign tumor commonly found in children. The majority of lymphangiomas are considered to be lymph vessel anomalies. The condition involves several expanded lymphatics surrounded by benign endothelial cells and usually occurs in the head, neck and axillary regions, and rarely in the gastrointestinal tract[1-3]. Recently, the number of case reports has been increasing with the increased use of endoscopic colon examination. Many lymphangiomas are asymptomatic and require no treatment, because the condition is considered absolutely benign. No cases, in which lymphangioma underwent malignant transformation, have been reported. However, some cases of lymphangioma accompany colon cancer[2]. When symptoms such as bleeding, intussusceptions or protein losing enteropathy are present, resection of lymphangioma is necessary[4-7]. Thus far, the natural history of colonic lymphangioma has remained unknown. Herein, we report the first case of spontaneous resolution of multiple colonic lymphangiomas during the follow-up.
CASE REPORT
A 54-year-old male patient suffered intermittently from blood-tinged stool with no personal or familial history of any specific disease. Physical examination showed no remarkable abdominal abnormality. Laboratory test or chest and abdominal radiography displayed no specific findings. Initial colonoscopy revealed numerous elevated lesions with smooth surfaces throughout the entire colon, which evidenced morphological changes as shown by endoscopy. In particular, the lesions on the left side of the colon evidenced surface petechiae (Figure 1). A diagnostic procedure and endoscopic mucosal resection were performed for the appropriate diagnosis and treatment of the lesions. Histopathological examination showed that the cystic lesion was lined with cuboid-shaped cells that were positive for CD68 histiocytic markers (Figure 2) but negative for CD34 and CK on immunohistochemical examination, the patient was thus diagnosed with colonic lymphangioma. Abdominal computed tomography showed no definite abnormalities, and the possibility of secondary events was excluded. The complaint of mild symptoms led to medical observation and use of stool softener.
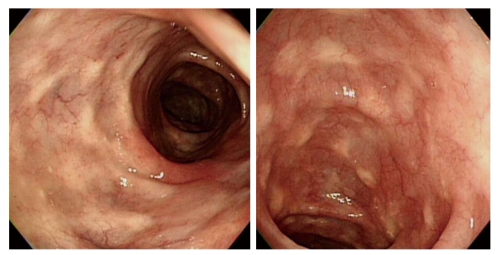
Figure 1.
Initial colonoscopy showing multiple elevated or protruding lesions with semi-transparant and smooth surfaces (A), and petechiae on the surfaces of lesions in the sigmoid colon (B).
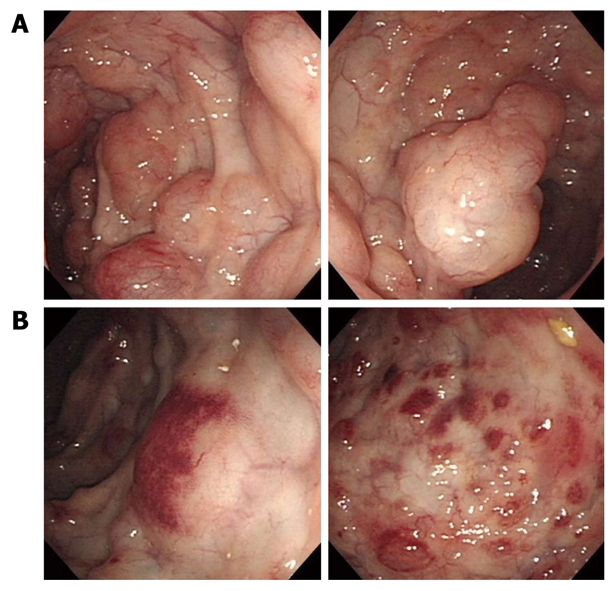
Figure 2.
Initial histopathological examination showing a submucosal cystic structure lined with cuboidal endothelial cells for the CD68 histiocystic marker (bottom) and a few giant cells (upper, HE stain, × 200).
After 12 mo, the patient visited our department for colonoscopy, which showed no more remarkable changes than the previous findings. Biopsy procedure was repeated, which demonstrated that the cystic lesion had no lining endothelium but was lined with focal multinucleated giant cells in the submucosa (Figure 3). After 24 mo, colonoscopy revealed complete resolution of colonic lymphangiomas without any specific treatment (Figure 4).
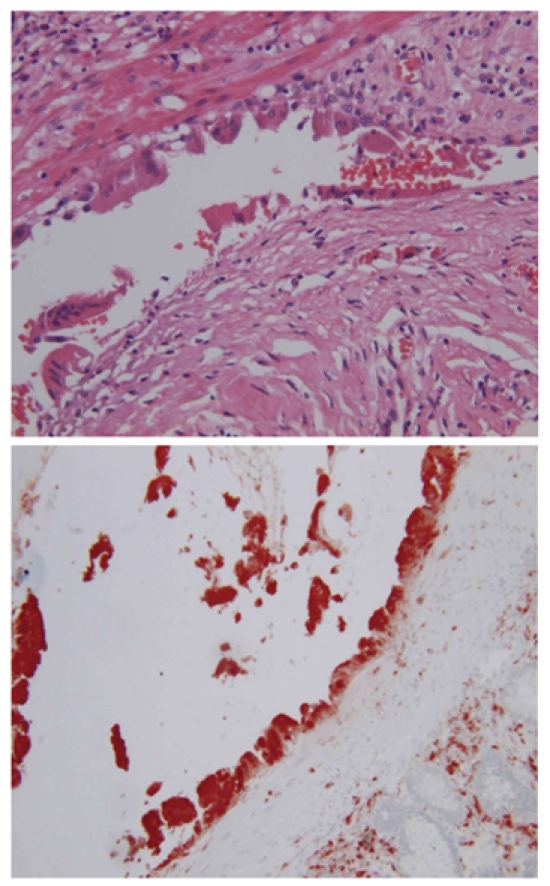
Figure 3.
Histopathological examination 12 mo after initial examination showing cystically dilated lesion lined with endothelium (upper, HE stain, × 40) and focal multinucleated giant cells (bottom, HE stain, × 100).
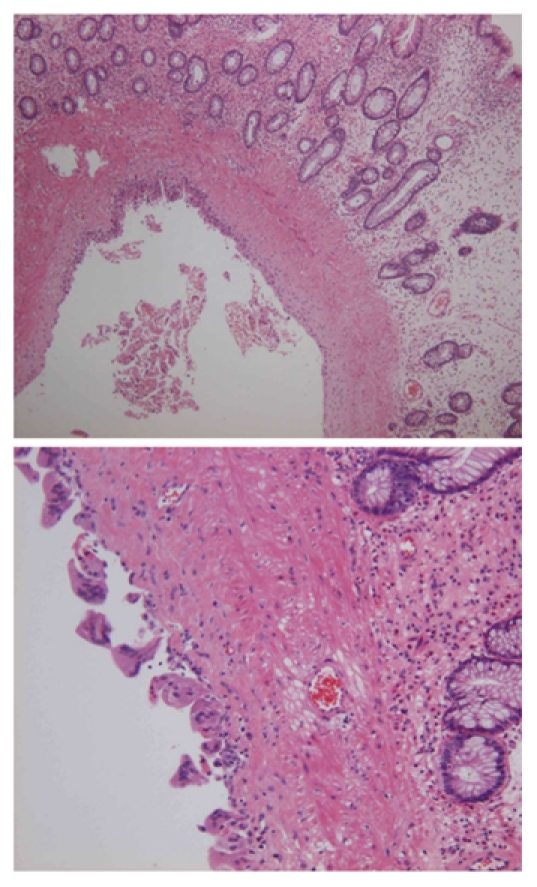
Figure 4.
Follow-up colonoscopy 24 mo after initial examination showing multiple whitish scars throughout the entire colonic mucosa and resolved lymphangioma without specific therapy.
DISCUSSION
In most reported cases of colonic lymphangioma, the condition is solitary. Only a few cases of multiple lymphangiomas of the colon, the so-called “colonic lymphangiomatosis”, have been reported so far[8,9]. Endoscopic findings of colonic lymphangioma are characterized by the presence of submucosal tumor properties covered with normal mucosa, round and soft surfaces, a wide base area, pink color and semi-transparency. Histological observations of lymph vascular dilation and outgrowth in the submucosal layer are important for its correct diagnosis in these cases. The condition is classified into capillary, cavernous, and cystic types[10]. The cystic type, as in our case, is also the most frequently reported and characterized by dilated lymphatic vessels surrounded by flat endothelial cells between fat, fibrotic and lymphatic structures. To the best of our knowledge, the formation of lymphangioma impedes lymph flow for a prolonged period, resulting in lymph vessel expansion or further progression and is generally perceived as a developmental malformation or agenesis of lymphatic tissue. Other causes such as abdominal trauma, lymphatic obstruction, inflammatory processes, cancer, surgery, or radiation may result in secondary lymphagioma formation[11-16]. In the case of lymphangioma appearing late in adulthood, the lesion may have developed secondarily from a local disturbance of the lymphatic circulation[2]. Therefore, the clinicians should look out for the causative condition, particularly in adults. Abdomen computed tomography showed no co-morbid disease in our case.
Although a definitive diagnosis of colonic lymphangioma requires complete excision including the submucosal layer, unnecessary surgery should be avoided. Moreover, as in our case, it is quite difficult to perform a total colectomy to remove lesions involving the entire colon. The spontaneous resolution of cystic hygromas originating in the neck or mediastinum has been reported[14,15]. Several investigators have suggested that increased pressure in the lymphatic system may overcome incomplete obstructions, which may explain why the lesions are spontaneously resolved. In contrast, spontaneous resolution presumably results from the establishment of alternative routes of lymphatic drainage in cases of septated lesions[16-18]. Although this hypothesis has been applied to cystic hygroma of the neck or the spleen, it may match well in our case. The mild leakage induced by increased pressure of the cyst may stimulate dendritic cells or macrophages in the stroma. In a prolonged state of lymphatic stagnation, CD68-positive cells, which can be dendritic cells or macrophages, might correspond to the cells equipped with phagosomes and lysosomes[19]. These stimulated cells would evidence phagocytic activity on the lining cells, which continues until the lymphangioma is resolved.
In conclusion, conservative management coupled with close surveillance may be an effective treatment strategy for lymphangioma, and resection of lymphangioma should be reserved in mild symptomatic or asymptomatic patients, because of its benign nature and possible spontaneous resolution.
Footnotes
Peer reviewers: A M El-Tawil, MSc, MRCS, PhD, Department of Surgery, University Hospital of Birmingham, East Corridor, Ground Floor, Birmingham, B15 2TH, United Kingdom; Antonio.Basoli, Professor, General Surgery “Paride Stefanini”, Università di Roma - Sapienza, Viale del Policlinico 155, Rome 00161, Italy
S- Editor Tian L L- Editor Wang XL E- Editor Zheng XM
References
- 1.Huguet KL, Metzger PP, Menke DM. Colorectal lymphangioma. Am Surg. 2007;73:414–416. [PubMed] [Google Scholar]
- 2.Matsuda T, Matsutani T, Tsuchiya Y, Okihama Y, Egami K, Yoshioka M, Maeda S, Onda M. A clinical evaluation of lymphangioma of the large intestine: a case presentation of lymphangioma of the descending colon and a review of 279 Japanese cases. J Nippon Med Sch. 2001;68:262–265. doi: 10.1272/jnms.68.262. [DOI] [PubMed] [Google Scholar]
- 3.Hilliard RI, McKendry JB, Phillips MJ. Congenital abnormalities of the lymphatic system: a new clinical classification. Pediatrics. 1990;86:988–994. [PubMed] [Google Scholar]
- 4.Zilko PJ, Laurence BH, Sheiner H, Pollard J. Cystic lymphangiomyoma of the colon causing protein-losing enteropathy. Am J Dig Dis. 1975;20:1076–1080. doi: 10.1007/BF01071198. [DOI] [PubMed] [Google Scholar]
- 5.Iwabuchi A, Otaka M, Okuyama A, Jin M, Otani S, Itoh S, Sasahara H, Odashima M, Kotanagi H, Satoh M, et al. Disseminated intra-abdominal cystic lymphangiomatosis with severe intestinal bleeding. A case report. J Clin Gastroenterol. 1997;25:383–386. doi: 10.1097/00004836-199707000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Kok KY, Mathew VV, Yapp SK. Lymphangioma of the small-bowel mesentery: unusual cause of intestinal obstruction. J Clin Gastroenterol. 1997;24:186–187. doi: 10.1097/00004836-199704000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Matsuba Y, Mizuiri H, Murata T, Niimi K. Adult intussusception due to lymphangioma of the colon. J Gastroenterol. 2003;38:181–185. doi: 10.1007/s005350300030. [DOI] [PubMed] [Google Scholar]
- 8.Kim J, Han D, Hong CH, Lee HL, Kim JP, Sohn JH, Hahm JS. Colonic lymphangiomatosis associated with protein-losing enteropathy. Dig Dis Sci. 2005;50:1747–1753. doi: 10.1007/s10620-005-2929-6. [DOI] [PubMed] [Google Scholar]
- 9.Watanabe T, Kato K, Sugitani M, Hasunuma O, Sawada T, Hoshino N, Kaneda N, Kawamura F, Arakawa Y, Hirota T. A case of multiple lymphangiomas of the colon suggesting colonic lymphangiomatosis. Gastrointest Endosc. 2000;52:781–784. doi: 10.1067/mge.2000.109714. [DOI] [PubMed] [Google Scholar]
- 10.Kim KM, Choi KY, Lee A, Kim BK. Lymphangioma of large intestine: report of ten cases with endoscopic and pathologic correlation. Gastrointest Endosc. 2000;52:255–259. doi: 10.1067/mge.2000.107710. [DOI] [PubMed] [Google Scholar]
- 11.Kim JH, Ryu WS, Min BW, Song TJ, Son GS, Kim SJ, Kim YS, Um JW. Acquired omental cystic lymphangioma after subtotal gastrectomy: a case report. J Korean Med Sci. 2009;24:1212–1215. doi: 10.3346/jkms.2009.24.6.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tezuka K, Ogawa Y, Satake K, Ohira M, Yamada S, Uno H, Wakasa K, Hirakawa K. Lymphangioma of the lesser omentum associated with abdominal esophageal carcinoma: report of a case. Surg Today. 2002;32:362–366. doi: 10.1007/s005950200053. [DOI] [PubMed] [Google Scholar]
- 13.Fisher D, Hiller N. Case report: giant tuberculous cystic lymphangioma of posterior mediastinum, retroperitoneum and groin. Clin Radiol. 1994;49:215–216. doi: 10.1016/s0009-9260(05)81782-9. [DOI] [PubMed] [Google Scholar]
- 14.Joo SH, Kim MJ, Kim KW, Lee WJ, Park MS, Lim JS. Spontaneous regression of a cystic tumor in a postpartum woman; is it a cystic lymphangioma? Yonsei Med J. 2007;48:715–718. doi: 10.3349/ymj.2007.48.4.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kiyota A, Tsukimori K, Yumoto Y, Hojo S, Morokuma S, Fukushima K, Takahata Y, Nakayama H, Wake N. Spontaneous resolution of cystic hygroma and hydrops in a fetus with Noonan's syndrome. Fetal Diagn Ther. 2008;24:499–502. doi: 10.1159/000193364. [DOI] [PubMed] [Google Scholar]
- 16.Brumfield CG, Wenstrom KD, Davis RO, Owen J, Cosper P. Second-trimester cystic hygroma: prognosis of septated and nonseptated lesions. Obstet Gynecol. 1996;88:979–982. doi: 10.1016/s0029-7844(96)00358-4. [DOI] [PubMed] [Google Scholar]
- 17.Bernstein HS, Filly RA, Goldberg JD, Golbus MS. Prognosis of fetuses with a cystic hygroma. Prenat Diagn. 1991;11:349–355. doi: 10.1002/pd.1970110603. [DOI] [PubMed] [Google Scholar]
- 18.Gallagher PG, Mahoney MJ, Gosche JR. Cystic hygroma in the fetus and newborn. Semin Perinatol. 1999;23:341–356. doi: 10.1016/s0146-0005(99)80042-1. [DOI] [PubMed] [Google Scholar]
- 19.Kishimoto K, Tate G, Kitamura T, Kojima M, Mitsuya T. Cytologic features and frequency of plasmacytoid dendritic cells in the lymph nodes of patients with histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease) Diagn Cytopathol. 2010;38:521–526. doi: 10.1002/dc.21265. [DOI] [PubMed] [Google Scholar]