Abstract
Background
Conducting longitudinal research studies with low-income and/or minority participants present a unique set of challenges and opportunities.
Purpose
To outline the specific strategies employed to successfully recruit and retain participants in a longitudinal study of nutritional anticipatory guidance during early childhood, conducted with a low-income, ethnically diverse, urban population of mothers.
Methods
We describe recruitment and retention efforts made by the research team for the ‘MOMS’ Study (Making Our Mealtimes Special). The ‘multilayered’ approach for recruitment and retention included commitment of research leadership, piloting procedures, frequent team reporting, emphasis on participant convenience, incentives, frequent contact with participants, expanded budget, clinical staff buy-in, a dedicated phone line, and the use of research project branding and logos.
Results
Barriers to enrollment were not encountered in this project, despite recruiting from a low-income population with a large proportion of African-American families. Process evaluation with clinic staff demonstrated the perception of the MOMS staff was very positive Participant retention rate was 75% and 64% at 6 months and 12 months post-recruitment, respectively. We attribute retention success largely to a coordinated effort between the research team and the infrastructure support at the clinical sites, as well as project branding and a dedicated phone line.
Conclusions
Successful participant recruitment and retention approaches need to be specific and consistent with clinical staff buy in throughout the project.
Keywords: recruitment, retention, longitudinal studies, low-income populations
1. Introduction
Although the National Institutes of Health Revitalization Act, issued over 15 years ago, requires the inclusion of “members of racial and ethnic minority groups” and women in clinical research [1], barriers to recruitment and retention remain for both the participant and the medical system. Racial and ethnic minorities report a general sense of distrust in the health care system and medical research [2,3]. This distrust, along with economic disadvantages, lack of awareness of available research studies, and communication barriers continue to impede recruitment and retention efforts [4]. Physician and staff resistance to conducting clinical research is an additional barrier [5]. Research designs need to better accommodate both stakeholder and service system characteristics; including aiming toward “interventions that clinicians can deliver, given the typical demands of practice in community settings…” [6].
Prior research has yielded some clues for establishing effective recruitment strategies. Flaskerud and Nyamathi [7] identified “cultural responsiveness” as an important factor in facilitating participation of minority persons, but also emphasize the need for resources to overcome problems of access and burden. Chang and colleagues [8] describe recruitment and retention strategies from “Moms in Motion,” a community-based trial among low-income overweight and obese mothers. The authors used cultural sensitivity in training for recruiters and suggest considering training peers as recruiters [8]. In addition to cultural sensitivity, interpersonal contacts and the power of face-to-face relationships have been shown to be important in both recruitment and retention of minority populations [5,9].
Previous studies have suggested that a combination of several strategies may improve retention of low-income populations [10]. Retention success has been attributed to consistent contact with study participants and maintenance of updated contact information [11]. In the Project DC-HOPE, a cohort of pregnant, inner-city African-American women, a 79% retention rate was achieved by using multiple strategies including consistent contact with the target population [12]. Moms In Motion yielded a 59% retention rate (at 10 weeks post-intervention) by focusing on multiple ways to maintain contact with highly mobile participants; requiring multiple phone numbers and addresses and providing small incentives for participants to update their contact information [8]. A similar technique requests complete contact information for at least two close family members or friends at the time of recruitment [13]. Other studies conducted in clinical settings suggest that interviews can be conducted when participants have scheduled other clinic visits [13] and that interventions should be offered at times and locations that are convenient for study participants [8,13,14]. Creating a project identity with the use of logos on all correspondence and advertisements can reinforce the participant’s bond with the study, reduce concerns regarding credibility and help the study become more easily recognizable [15].
The purpose of this paper is to detail specific recruitment and retention strategies used for a low-income, ethnically diverse group of mothers participating in longitudinal research. This study builds on previous work by discussing our success or barriers with common approaches to recruitment and retention and describing less well reported strategies such as budget, project identity, leadership, and clinical staff buy-in.
2. Methods
2.1 The project: Making our Mealtimes Special (MOMS)
The specific aims of the study were to develop, disseminate, monitor, and evaluate two new anticipatory guidance programs during the child’s first year of life to prevent childhood overweight and obesity for patients at the level of the clinical practice of these three low-income clinics.
The MOMS (Make Our Mealtimes Special) study was implemented in a low-income urban population in Columbus, Ohio. Primary care clinics in NCH Primary Care Network were chosen as the population of sites for this study. From the Network of 11 clinics in low-income neighborhood areas, we selected three clinical sites to participate in the MOMS study. We randomly allocated the two arms of the intervention and the control group to each of the three clinical sites (clusters). In our sample of clinics, the overall population is children and adolescents, aged 0–18 years with a racial/ethnic distribution of 50% African-American, 40% non-Hispanic White, and 10% Hispanic. Approximately 85% receive Medicaid for health care, which is available for children living in homes with family income below and up to 200% of the poverty level in Ohio.
The interventions took place as part of the routine anticipatory guidance given to parents by the clinical staff (pediatricians, nurses, and medical assistants) during their children’s regularly scheduled well-child visits; the research team was not responsible for intervention delivery at the clinical site. (A more detailed description of the study design is published elsewhere [16].) Briefly, the two intervention arms were a) an infant-focused nutritional educational protocol (referred to as “Ounce of Prevention”) and b) a mom-focused eating protocol promoting maternal consumption of the USDA food groups (referred to as “Maternal Focused Eating”). The control condition was the usual care condition, which was based on the Bright Futures Nutrition pocket guide [17]. The research team recruited participants and conducted follow-up interviews at the 6- and 12-month well-child visits. On most instances, the research interview, conducted by a member of the research team, and the intervention carried out by the clinical staff, occurred during the same office visit. In addition, the research team conducted a chart review to evaluate if all items of the anticipatory guidance were given.
The study inclusion criterion was biological mothers of healthy infants three months old or younger. Exclusion criteria included non-English speaking mothers, infants in foster care placement, infants hospitalized at birth for more than one week, and infants with gastrointestinal disease other than reflux, known congenital heart disease causing cyanosis and/or congestive heart failure, metabolic disorders, a genetic syndrome or born younger than 36 weeks gestation.
2.2 Overall approach to participant and staff recruitment and retention
The overarching goal of any clinical study is to optimize the type and number of participants recruited and retained in a study at minimal expense. However, we knew from the outset that successful recruitment and retention of low-income and/or minority participants present a unique set of challenges. Their lives are often very chaotic, often running out of money, food stamps, and bus passes by the end of the month. They relocate their residences often and without prior notice. Our overall approach to these challenges was to use multiple strategies for both recruitment and retention. We incorporated strategies that have been used successfully in previous studies, such as piloting, training, incentives, maintaining contact with participants, and keeping the process convenient for the participant [8,13,14]. We also employed less well discussed strategies including experienced involved leadership, establishing a project identity, clinical staff buy-in, an emphasis on personal contact, and increasing the proportion of the budget allocated for recruitment and retention by acquiring additional supplemental funding [15].
(1) Leadership
Leaders of the research team have a total of 30 years combined experience working with low-income, ethnically diverse families in hospital-affiliated clinical pediatric settings and have conducted longitudinal interventional research studies in maternal smoking reduction, which involved the same populations. Thus, project leadership had previous research experience with both recruitment and retention issues for difficult to reach populations. From the beginning stages, research staff was responsible for implementing recruitment and retention strategies during all stages of the project as well as reporting success and challenges of recruitment and retention to the entire research team during monthly meetings. This continued involvement allowed for quick and minor adjustments to be made to recruitment strategies.
(2) Staff
One of the co-investigators, a nurse, provided oversight of all three recruitment teams for each clinical site. This nurse also recruited and interviewed the participants at one of the clinics. The team leaders each have a Master’s degree or PhD in sociology and education. Because of these people oriented professions, they were able quickly to assess problems, suggest solutions, and form relationships easily with both clinical staff and participants. They also trained additional medical students and research assistants.
(3) Clinical staff recruitment or buy-in
Although the primary concern was the recruitment of suitable participants for the study, it was equally important to gain buy-in from the professional and support staff of the three study clinics. Prior to data collection, the research team held a meeting at each clinic to provide information about the study objectives and protocol and obtain suggestions from the clinical staff on successful project implementation. All staff members (physicians, nurses, medical assistants, registration specialists, social workers, and nutritionists) were invited to attend. The presentation, conducted by a principal investigator of the project along with research staff, emphasized the fact that customary clinic procedures would not be interrupted, nor would the intervention require any additional time or effort on the part of clinic staff. This message affirmed that study investigators were responsive to the realities of a busy clinic. Clinic staff provided the research team with information regarding the average wait time for patients in the waiting area as well as information regarding appointment schedules that was useful for recruitment and retention planning.
In addition, after one month of recruitment, a meeting was convened with staff at each clinic to inform them of study progress, provide a targeted time-frame for completion of the recruitment phase of the project, and receive feedback from the clinic staff. Surveys given to clinic staff during the second presentation (five months after the start of recruitment) revealed a positive perception of the research team. Most (86%) of clinical staff believed that the research team were personable and professional in their interactions.
(4) Budget
It was essential to create an ample budget that would allow for the research staff needed to ensure adequate participant recruitment and retention. The principal investigators recognized from the outset that this cost burden was unavoidable, and therefore supplemental funds in addition to the grant were sought from a hospital intramural grant and an external university summer grant. Some of these additional funds were used to pay medical students to assist research staff in recruitment of participants and for additional clerical staff to enhance retention capabilities throughout the study. The addition of the student recruiters allowed for a total of nine research staff working on recruitment simultaneously, thereby allowing for maximum recruitment in under a year. Part of the additional funding helped to maintain an intact research team to continue retention beyond the original end date of the grant. Including all three sources of funding, a total of 60% of the budget was used for recruitment and retention, 9% of which was spent on participant incentives and the remaining 51% on research staff working exclusively on recruitment and retention issues.
2.3 Specific recruitment strategies employed
(1) Piloting recruitment procedures
The recruitment strategy was field-tested in a two-month pilot project involving 26 mothers. The main goal of this pilot phase was for the research staff to learn how to ‘streamline’ study procedures into the busy clinic flow (i.e., introducing the project and the staff, obtaining informed consent, obtaining baseline data). Piloting these procedures was invaluable in avoiding conflicts between research staff and clinical staff once the project became operational.
(2) Personal approach
Research staff had access to clinic schedules so that recruiting efforts occurred only when patients of the appropriate age were scheduled for a clinic visit. The convenience sample was identified ‘in person’ by waiting room observation of incoming families with babies in their carriers. If the infant in the carrier was deemed a ‘likely candidate’—that is, apparently healthy and under three months of age—research staff would approach the parent(s), introduce themselves, briefly explain the study, and invite the mother to participate.
(3) Training research staff
A role modeling approach was used in training. New interviewers typically accompanied one of the leaders on three or four interview sessions. When the new interviewer felt comfortable with the process, s/he would take responsibility for two to three interviews accompanied by a team leader. Only then were the new interviewers permitted to conduct their own interviews independently. The interview team leaders also continued to conduct interviews in all three clinics in order to stay in touch with the clinic staff and the members of the interview team assigned to the clinic.
(4) Incentives
Part of our strategy for recruitment was to inform participants of the full project incentive structure verbally and in a written handout at enrollment. Participants were reminded of future incentives via a special ‘card’ listing each follow-up contact with the research team and the amount of the incentive offered for that interview. Original enrollment and continued participation in the project was encouraged by providing incentives of increasing amounts in the form of gift cards from a local grocery chain ($10 for the first visit, followed by $15 and $20).
2.4 Specific retention strategies employed
(1) Reporting progress and overcoming barriers
The research team met every other week during the entire project period. Each research team leader assigned to a particular clinical site was responsible for a detailed bi-monthly cohort retention report. This included information on the number of participants, duration of interview with each participant, unanticipated events, and any problems with the survey instrument or implementation. To assist with retention efforts, research staff kept detailed lists of contact information which was regularly checked against billing data records for accuracy and completeness. Research staff developed spreadsheets with expected dates of appointments, age of infant at time of visit, and visit type. All recruiting staff were trained in the existing computerized clinical scheduling system for each clinic that was also available centrally at the hospital so that they could both track participant well-child appointments and actually make these appointments. In addition, two clerical staff were trained in scheduling and portions of their salaries were paid from the project budget.
(2) Personal approach
For the follow-up interviews, efforts were made to provide consistent interviewers for each mother in order to maintain the mother–interviewer relationship.
(3) Phone line
A dedicated project phone line was established. At project enrollment, participants received a refrigerator magnet showing the dedicated telephone number. For maximum convenience to participants, they were instructed to use this dedicated phone line to make, change, or confirm well-child checks for their children. The phone was staffed during business hours by clerical staff trained in the study protocol. The clerical staff was trained to conduct follow-up calls to families who had missed appointments to get the child visit rescheduled. This increased the opportunities for research staff to meet with the mothers at well-child visits and to obtain survey data in accordance with the project protocol.
(4) Identity and logos
A project identity and corresponding logo, “MOMS - Making our Mealtimes Special”, was developed. This was used on all materials given to or mailed to the participants to maximize their identification with the project. Multiple mailings with the MOMS logo were sent out at regular intervals to the participants. These were a reminder postcard (4–5 months), a thank you note (after 6 months), and a newsletter (9 months, see appendix). All of these mailings emphasized the MOMs project identity for the families involved and also served as a project update to show participants of their important role in the project.
(5) Participant convenience
The follow-up interviews took place 6 and 12 months post enrollment, during the half hour prior to the well-child visit for these ages. This practice maximized convenience for the family, because the participants did not have to make an additional visit to the medical center or clinic for the research interview. It was a priority for research staff to be available to the participant. If an interview was not conducted at a well-child visit (if the participant missed the visit), then a phone interview was attempted. The mailed newsletter also provided information about transportation assistance for their next scheduled appointment. Most of our participants were insured by Caresource, a Medicaid provider for which provides free transportation for doctor visits, but may have forgotten about the availability of transportation assistance.
A minimum of five attempts were always made to meet the participant at the clinic, send a reminder notice in the mail, or arrange a phone interview. The scheduling system was routinely consulted to see if participants had an updated address or phone number and participants received incentives ($10.00 gift card) to call the dedicated phone line to update their contact information. Participants were considered lost to follow-up only after all means of contacting the participant had been exhausted.
(6) Repeated contact with participants
Reminder postcards (as mentioned above) were sent and follow-up phone calls prompted participants to schedule their child’s 6-month well-child visit, as this corresponded to a data collection point. Participants were able to schedule their appointments two weeks in advance via the hospital’s registration system. Research staff made a phone call the night before the appointment as an additional reminder. As previously mentioned, following the first 6 months of participation, MOMS participants received a personalized thank you letter for their assistance with the study. Additionally, the thank you note also served as a reminder of the upcoming 9-month well-child visit. If any appointment was missed at which data collection would take place, the participant would be contacted and the appointment rescheduled.
3.0 Results
3.1 Sample representation
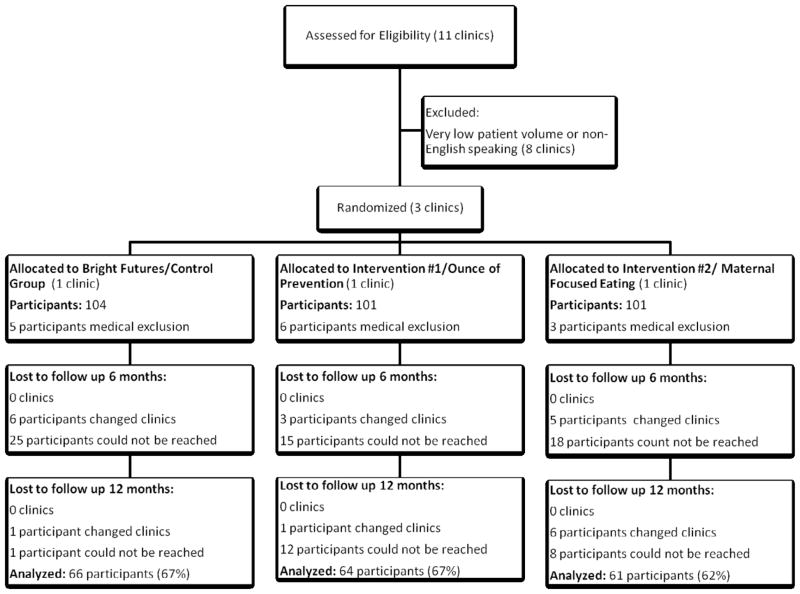
Figure 1 presents data on sample representation using a CONSORT chart for cluster randomized trials adapted from Thomas et al. [18]. The three clinics chosen for randomization were selected based on a high patient volume (60–90 patients per day, versus 30 in other sites), allowing for adequate patient recruitment and within a predominately English speaking patient population. The sites were also geographically far apart from each other, to minimize patients switching to other nearby clinics. All three clinics were located in low-income areas with a large population of minority women and children, who were the target population for this obesity intervention trial.
Figure 1.
Sample representation and retention: CONSORT Chart for cluster randomized trials.
3.2 Participant recruitment
Recruitment took place over a 9-month period. Although refusal rates were not formally tracked, research staff reported on these events during staff meetings and it was noted that refusals were very rare. There were instances when mothers felt rushed to get to their appointment or were busy managing several other children on their own and would decline to participate at that moment in time. However, it was common for a mother to ask to complete the initial questionnaire at a later well-child visit (such as a mother of a 6 week-old requesting to complete the questionnaire at the next well-child visit at 3 months of age). Recruitment of the full complement of 306 mother–infant dyads took place from June 2005 to March 2006; recruitment at one site was deliberately delayed as it underwent the conversion from paper to electronic medical records during the recruitment phase. During that transition, fewer patients were seen in that clinic site to allow for longer appointment times as the new electronic system was implemented. This factor decreased the recruitment rate at that site for about six weeks, but recruitment at this site was completed at approximately the same time as the other two sites.
3.3 Baseline characteristics of the MOMS study participants
The average maternal age for all three groups was 24 years (range 15–42 years) and 42% had a high school diploma or equivalent. The majority of participants received support from WIC (Women Infant Children formula and food supplements [94%]). Over half (53%) of mothers reported a family history of heart disease and/or diabetes in their parents’ generation. Maternal BMI by self-report ranged from 16 to 57, with a mean of 28; 62% of the mothers were overweight or obese (data not shown).
Table 1 presents baseline demographic characteristics of all study participants by arm of the intervention (Bright Futures [n=66], Ounce of Prevention [n=64], Maternal Focused Eating [n=61]) and was adapted from Feder et al. [19]. There were no significant differences in age, education, or support from WIC by arm of the intervention. Maternal Focused Eating reported significantly less food stamps use (45.9%), than either Bright Futures (62.5%) or Ounce of Prevention (68.3%). The racial distribution and martial status also differed by arm of the intervention. Again, Maternal Focused Eating was significantly different than Bright Futures and Ounce of Prevention. Specifically, the majority of the Maternal Focused Eating group was married (39.3%) and white (52.5%), whereas both the majority of the Bright Futures and Ounce of Prevention groups were single (51.6% and 53.3%) and Black (64.1% and 73.3%).
Table 1.
Baseline Characteristics by intervention cluster at 12 month (n=191, cluster=3)
| Bright Futures (n=64) | Ounce of Prevention (n=66) | Maternal Focused Eating (n=61) | p-value | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ANOVA | |
| Age (years) | 24.0 (5.7) | 23.8 (5.3) | 23.6 (4.7) | 0.85 |
| % | % | % | Chi-square | |
| Race | ||||
| White | 23.4 | 25.0 | 52.5 | .00 |
| Black | 64.1 | 73.3 | 21.3 | .00 |
| Hispanic/Other Race | 12.5 | 1.7 | 26.2 | .00 |
| Education | ||||
| < High School Diploma | 18.8 | 30.0 | 34.4 | .13 |
| High School Diploma | 48.4 | 38.3 | 47.5 | .46 |
| Some College | 32.8 | 31.6 | 18.0 | .13 |
| Relationship Status | ||||
| Single | 51.6 | 53.3 | 29.5 | .01 |
| Cohabiting | 34.4 | 28.3 | 31.1 | .77 |
| Married | 14.1 | 18.3 | 39.3 | .00 |
| WIC | ||||
| Yes | 90.1 | 95.0 | 91.8 | .64 |
| Food Stamps | ||||
| Yes | 62.5 | 68.3 | 45.9 | .03 |
3.4 Retention
Figure 1 presents sample retention by arm of intervention. The average retention rate was 75% at 6 months and 64% at 12 months post recruitment, with 57% of all participants having complete data at the three time points of baseline, 6 months, and 12 months. Analysis of retention rates by characteristics of the sample (Table 2) showed that at 6 months African-American mothers (82%) had higher retention rates than White women (70%) or women of Hispanic/Other race ethnicity (65); p<.05. Women aged 30–42 years (90%) also had a higher retention rate than women aged 20–29 (72%), or aged 15–19 (78%). However, at 12 months, there was no difference in retention rates by race or age. Similarly, there was no difference by race or age for those women who had follow-up data at both 6 and 12 months (data not shown). Additionally, no significant differences in retention were found by intervention arm.
Table 2.
Retention Rates by Characteristics at 6 and 12 months: The MOMS study
| 6 month (n=220) | Chi-Square p-value | 12 month (n=191) | Chi-Square p-value | |
|---|---|---|---|---|
| % | % | |||
| Clinic | ||||
| Maternal focused eating | 76.5 | .10 | 62.2 | .94 |
| Ounce of Prevention | 81.1 | 67.4 | ||
| Bright Futures | 68.7 | 66.7 | ||
| Participants | ||||
| Age | ||||
| 15–19 years | 77.8 | .05 | 65.1 | .13 |
| 20–29 years | 71.6 | 60.0 | ||
| 30–42 years | 89.7 | 76.9 | ||
| Race | ||||
| White | 69.6 | .02 | 60.8 | .76 |
| Black | 82.0 | 65.3 | ||
| Hispanic/Other Race | 65.0 | 62.5 | ||
| Education | ||||
| < High School Diploma | 83.7 | .07 | 59.3 | .44 |
| High School Diploma | 74.0 | 67.5 | ||
| Some College | 68.7 | 61.5 | ||
| Relationship Status | ||||
| Single | 78.0 | .56 | 62.9 | .96 |
| Cohabiting | 71.7 | 63.0 | ||
| Married | 75.0 | 64.7 | ||
| WIC | ||||
| No | 68.4 | .47 | 73.7 | .33 |
| Yes | 75.8 | 62.6 | ||
| Food Stamps | ||||
| No | 70.1 | .09 | 65.0 | .64 |
| Yes | 78.9 | 62.3 | ||
As noted in the flow chart, some participants were lost to follow-up due to switching from one clinic to another clinic in the primary care clinic network. Since the intervention was randomized to the clinic, any participant who changed clinics did not receive the correct intervention (or no intervention at all). Overall, Bright Futures lost 7 participants to other clinics, Ounce of Prevention lost four, and Maternal Focused Eating lost 11. In addition, 25% of the total sample was lost because of the inability to reach the mother for follow-up.
Those who were lost to follow-up were significantly younger (mean age 22.9 years) compared to those who remained in the study (mean age 24.0 years). No other significant differences were found in baseline characteristics.
4.0 Discussion
In this longitudinal project, a comprehensive approach was used for recruitment and retention. Despite recruiting from a low-income and minority population, few barriers to study enrollment were encountered in this clinic-based research study. This was most likely because the intervention itself was part of clinical care and was not perceived to be ‘experimental,’ although data were not specifically collected on this issue. Clinical staff buy-in appeared to be strong throughout the study. Furthermore, buy-in was likely achieved as the study design did not add any more tasks to the daily work-load in providing clinical care.
As noted by other studies in a similar population, recruitment and retention efforts were successful because of several strategies. Although not discussed previously in the literature as a recruitment or retention strategy, designating a nurse leader to oversee the leaders and interviewers at all three clinics provided excellent role modeling patient/health professional interactions and for integrating research processes into a clinical environment. Nurses are familiar with the clinic flow as well as the needs of the new mother. Clinic patients and parents seek guidance from the nurse as the person with the most time to devote to their needs. It is very likely that this bond helped initially form relationships between the research staff, clinical staff, and participants.
From the outset, retention was a priority of the research leadership. Our comprehensive approach to both recruitment and retention was selected based on the historical challenges faced in conducting prospective research within low-income and minority populations. Several of our strategies have been validated in previous studies and included face-to-face recruiting, consistent and repeated contact with the target population, financial incentives, participant tracking, and continuous monitoring. In addition, we developed a project logo and identity and used it on all mailings to participants and aided participant convenience with the use of a dedicated phone line. Despite the additional costs, we believe this investment of resources is essential for research projects attempting to follow a similar population. As such, all research staff, from the principal investigator to the data collection members of the team, must have the willingness to undertake a more involved protocol when working with a population which is often difficult to reach and retain.
The retention rate for this project was high at 6 months and fairly high at 12 months relative to other projects among low-income mothers. In their smoking cessation study, a different project with a similar population, French & Groner had an excellent retention rate at 3 months (over 75% depending on the group) but at 6 months only 60% of the cohort could be contacted [20] despite a planned, systematic approach of participant follow-up. Chang and colleagues [8] yielded a similar retention rate among low-income overweight and obese mothers. A parenting intervention study, which recruited women with inadequate prenatal care, similarly yielded a 59% retention rate at 12 months post intervention [21].
One factor that may contribute to reduced retention of low-income mothers is that an infant’s first two years of life is a very busy time for any mother. A study by Hambridge and colleagues examined if attendance at infant well-child visits could be increased if a stepped intervention of reminder, recall, and case management were employed [21]. In this urban population, those who received the stepped intervention were significantly more likely to have had ≥5 well-child visits by 15 months of age (65%), compared to those without the intervention (47%). The total cost per child for the intervention arm was $23.30 per child, per month [22]. This further emphasizes the logistical and cost challenges associated with retention of low-income mother-infant dyads during the first two years of life. To facilitate a similar retention plan, we had multiple team members in the clinics regularly to increase our visibility, with repeated efforts to call and contact mothers after missed appointments, and worked within the normal well-child visit schedule to reduce the burden on mothers.
Another factor that may influence participant retention may relate to the study topic. Senturia et al. [23] reported that 89% of participants completed 3-, 6-, and 9-month surveys in an inner-city pediatric asthma study. Asthma is a chronic disease that can have quite severe symptoms, and therefore missing clinic visits may be frightening for parents. In the MOMS study, one possible explanation for the drop in retention at 12 months may be related to the relatively benign topic of nutritional anticipatory guidance at a well-child visit. Because parents may have felt that they could ‘catch-up’ in their child’s immunization schedule and information several months later, adherence to the study protocol may not have been perceived as important. Likewise, more participants were lost in the Maternal Focused Eating group than the other two groups. This may reflect a lack of interest in establishing a healthy diet for themselves and the focus of the new mother on the dietary needs of her infant, which was more of the focus for the other groups.
A randomized clinical trial of diabetes self-management intervention at five community health centers in Massachusetts among low-income Latinos with type 2 diabetes retained 71% of the sample with all measures at both baseline and 12-month follow-up [24]. Similar to our study, researchers of this study attribute their retention success largely to a coordinated effort between the research team and the infrastructure support at the community health centers. What we term clinical staff buy-in in this manuscript includes the clinical infrastructure support we received from the three clinics. Having access to schedules and charts, being able to work with the nurses and doctors to finish surveys during down time in the well-child visits, use of desk space and chart areas in the clinics with assistance were essential elements of administrative support.
Our retention rates were analyzed by age, race, education, relationship status, use of WIC and food stamps to see if certain groups were inadvertently ‘selectively’ retained. When analyzing retention rates, we found that African-American women and those of older ages had higher retention at 6 months, but that there was no difference by race or age at 12 months and at both time points combined. There is no clear explanation for this finding, but we can state that our approach to recruitment and retention certainly did not select for non-minority or participants of older ages.
Failure to track refusals is a limitation of this study because future recruitment and retention strategies can be used that address these issues. For instance, parents who did not agree to their child’s participation in a school-based diabetes study cited that they did not understand the informed consent (37%), ran out of time to complete paper work (32%) and communication difficulties [25]. The parent’s suggestions for increasing recruitment include offering encouragement (53%), involving parents with previous experience in research (24%) and providing educational information (19%). Our study did offer encouragement through continued face-to-face and verbal communication. Involving previous research participants as recruiters is a novel idea that may be beneficial in these low-income, diverse populations because of the potential to decrease the distrust of health care providers and researchers.
5.0 Conclusion
In developing research projects with low-income populations and minorities, it is vital to have a clear plan for recruitment and retention strategies prior to implementing the project. Approaching this issue using a multiplicity of strategies simultaneously, and recognizing the significant monetary costs to provide for staff and incentives, is critical.
Supplementary Material
Acknowledgments
Acknowledgements of support: National Institutes of Health, NICHD R21-HD50944, The Research Institute at Nationwide Children’s Hospital, Columbus Ohio, and The Cristafi-Monte Fund of the Ohio State University College of Medicine
We would like to thank Anna Cunningham and Catherine Schroeder for their work on this project.
Abbreviations
- NCH
Nationwide Children’s Hospital
Footnotes
Conflicts of interest: None of the authors had any conflicts of interest; there was no corporate sponsorship of this research.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lisa Nicholson, School of Public Health, University of Illinois Chicago
Patricia M. Schwirian, The Ohio State University College of Nursing and Department of Family Medicine, Columbus, Ohio
Elizabeth G. Klein, Division of Health Behavior & Health Promotion, The Ohio State University College of Public Health, Columbus, Ohio.
Theresa Skybo, Mt. Carmel College of Nursing, Columbus, Ohio.
Lisa Murray-Johnson, The Ohio State University Medical Center, Columbus, Ohio.
Ihuoma Eneli, The Center for Healthy Weight and Nutrition, Nationwide Children’s Hospital, Columbus, Ohio
Bethany Boettner, Department of Sociology, The Ohio State University, Columbus, Ohio
Gina French, Community Pediatrics Division, University of Hawaii John A Burns School of Medicine, Honolulu, HI
Judith A. Groner, Section of Ambulatory Pediatrics, Nationwide Children’s Hospital, Columbus, Ohio
References
- 1.Office of Extramural Research NIH. 2001 http://grants.nih.gov/grants/funding/women_min/guidelines_amended_10_2001.htm.
- 2.Blumenthal DS, Sung J, Coates R, Williams J, Liff J. Recruitment and retention of subjects for a longitudinal cancer prevention study in an inner-city black community. Health Serv Res. 1995;30(1 Pt 2):197. [PMC free article] [PubMed] [Google Scholar]
- 3.Bonner GJ, Miles TP. Participation of African Americans in clinical research. Neuroepidemiology. 1997;16(6):281. doi: 10.1159/000109698. [DOI] [PubMed] [Google Scholar]
- 4.Gorelick PB, Harris Y, Burnett B, Bonecutter FJ. The recruitment triangle: reasons why African Americans enroll, refuse to enroll, or voluntarily withdraw from a clinical trial. An interim report from the African-American Antiplatelet Stroke Prevention Study (AAASPS) J Nat Med Assoc. 1998;90(3):141. [PMC free article] [PubMed] [Google Scholar]
- 5.Gilliss CL, Lee KA, Gutierrez Y, et al. Recruitment and retention of healthy minority women into community-based longitudinal research. J Womens Health Gend Based Med. 2001;10(1):77. doi: 10.1089/152460901750067142. [DOI] [PubMed] [Google Scholar]
- 6.Zayas LH, McKee MD, Jankowski KRB. Adapting psychosocial intervention research to urban primary care environments: A case example. Ann Fam Med. 2004;2(5):504–8. doi: 10.1370/afm.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flaskerud JH, Nyamathi AM. Attaining gender and ethnic diversity in health intervention research: cultural responsiveness versus resource provision. Adv Nurs Sci. 2000;22(4):1. doi: 10.1097/00012272-200006000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Chang M-W, Brown R, Nitzke S. Participant recruitment and retention in a pilot program to prevent weight gain in low-income overweight and obese mothers. BMC Public Health. 2009;9:424–34. doi: 10.1186/1471-2458-9-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Motzer SA, Moseley JR, Lewis FM. Recruitment and retention of families in clinical trials with longitudinal designs. West J Nurs Res. 1997;19(3):314. doi: 10.1177/019394599701900304. [DOI] [PubMed] [Google Scholar]
- 10.Davis LL, Broome ME, Cox RP. Maximizing retention in community-based clinical trials. J Nurs Scholarsh. 2002;34(1):47. doi: 10.1111/j.1547-5069.2002.00047.x. [DOI] [PubMed] [Google Scholar]
- 11.Bell LS, Butler TL, Herring RP, Yancey AK, Fraser GE. Recruiting blacks to the Adventist health study: Do follow-up phone calls increase response rates? Ann Epidemiol. 2005;15(9):667. doi: 10.1016/j.annepidem.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 12.El-Khorazaty MN, Johnson AA, Kiely M, et al. Recruitment and retention of low-income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC Public Health. 2007;7:233. doi: 10.1186/1471-2458-7-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosal MC, White MJ, Borg A, et al. Translational research at community health centers: challenges and successes in recruiting and retaining low-income Latino patients with type 2 diabetes into a randomized clinical trial. The Diabetes Educator. 2010;36(5):733–749. doi: 10.1177/0145721710380146. [DOI] [PubMed] [Google Scholar]
- 14.Deborah G, Wrenetha J, Louis F. What motivates participation and dropout among low-income urban families of color in a prevention intervention? Fam Relat. 2001;50(3):246–54. [Google Scholar]
- 15.Aitken L, Gallagher R, Madronio C. Principles of recruitment and retention in clinical trials. Int J Nurs Pract. 2003;9:338–46. doi: 10.1046/j.1440-172x.2003.00449.x. [DOI] [PubMed] [Google Scholar]
- 16.Groner JA, Skybo T, Murray-Johnson L, et al. Anticipatory guidance for prevention of childhood obesity: design of the MOMS project. Clin Pediatr (Phila) 2009;48(5):483–92. doi: 10.1177/0009922809331799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Green MPJ, Clark EM, Anatasi JM, Arlington VA, editors. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 2. Arlington, VA: National Center for Education in Maternal & Child Health; 2002. [Google Scholar]
- 18.Thomas RE, Grimshaw JM, Mollison J, et al. Cluster randomized trial of a guideline-based open access urological investigation service. Fam Pract. doi: 10.1093/fampra/cmg605. (in press) [DOI] [PubMed] [Google Scholar]
- 19.Feder G, Griffiths C, Eldridge S, Spence M. Effect of postal prompts to patients and general practioners on the quality of primary care after a coronary event (POST): a randomized trial. BMJ. 1999;318:1522–6. doi: 10.1136/bmj.318.7197.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.French GM, Groner JA, Wewers ME, Ahijevych K. Staying smoke free: An intervention to prevent postpartum relapse. Nicotine Tob Res. 2007;9(6):663–70. doi: 10.1080/14622200701365277. [DOI] [PubMed] [Google Scholar]
- 21.Katz KS, El-Mohandes A, Johnson DM, et al. Retention of low income mothers in a parenting intervention study. Journal of Community Health. 2001;26(3):203–218. doi: 10.1023/a:1010373113060. [DOI] [PubMed] [Google Scholar]
- 22.Hambridge SJ, Phibbs SL, Chandramouli V, et al. A stepped intervention increases well-child care and immunization rates in a disadvantaged population. Pediatrics. 2009;124:455–64. doi: 10.1542/peds.2008-0446. [DOI] [PubMed] [Google Scholar]
- 23.Senturia YD, McNiff Mortimer K, Baker D, et al. Successful techniques for retention of study participants in an inner-city population. Control Clin Trials. 1998;19(6):544. doi: 10.1016/s0197-2456(98)00032-4. [DOI] [PubMed] [Google Scholar]
- 24.Rosal MC, White MJ, Borg A, et al. Translational research at community health centers: Challenges and successes in recruiting and retaining low-income Latino patients with type 2 diabetes into a randomized clinical trial. The Diabetes Educator. 2010;36(5):733–49. doi: 10.1177/0145721710380146. [DOI] [PubMed] [Google Scholar]
- 25.Drews K, Harrell J, Thompson D, et al. Recruitment and retention strategies and methods in the HEALTHY study. Int J Obes. 2009;33:S21–28. doi: 10.1038/ijo.2009.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.