Abstract
AIM: To characterize the increasing incidence and geographic variation of acute diverticulitis.
METHODS: Using the nationwide inpatient sample (NIS) we identified a cohort who had been admitted with diverticulitis between 1998 and 2005. We calculated age-, sex-, and region-specific rates of hospitalizations for diverticulitis over time.
RESULTS: The age-adjusted hospitalization rate for diverticulitis increased from 61.8 per 100 000 to 75.5 per 100 000 between 1998 and 2005, and increased similarly in both sexes. Diverticulitis-associated admissions were male-predominant in those younger than age 45 years but were female-predominant thereafter. Admission rates increased the most among those < 45 years, while remaining unchanged for those ≥ 65 years. By 2005, the majority of hospitalized patients were < 65 years. Age-adjusted rates of diverticulitis-associated hospitalizations were lower in the West (50.4/100 000) compared to the Northeast (77.7/100 000), South (73.9/100 000), and Midwest (71.0/100 000).
CONCLUSION: Diverticulitis-associated hospitalizations have steeply risen, especially in young adults. These epidemiological trends vary by geographic region and warrant further investigation into potential dietary and environmental etiologies.
Keywords: Diverticulitis, Geographic variation, Hospitalization, Young adults
INTRODUCTION
Diverticular disease of the colon is among the most prevalent conditions in Western society and is among the leading conditions for outpatient visits and hospitalizations[1,2]. The prevalence of diverticular disease increases with age, occurring in less than 10% of those who are younger than 40 years and being as high as 66% in those older than 80 years[3]. Between 10%-25% of individuals with colonic diverticula will develop diverticulitis[4], of which a quarter can develop life threatening complications such as obstruction, perforation and intraperitoneal abscess formation[5].
There is significant geographic variation in the prevalence of diverticular disease, occurring much less commonly among Asians compared to western populations[4]. This observation has led to the theory that low-fibre diets may contribute to the development of colonic diverticula[6]. Additionally, there is emerging evidence that obesity and body mass index may also be predisposing factors[7,8].
Though diverticular disease is generally thought to be a disease of older adults, there are increasingly common reports of diverticulitis in individuals younger than 50 years[9]. Based on single-centre reports, these cases were often male-predominant[10] accompanied by a more aggressive disease course[8,11]. Using the nationwide inpatient sample (NIS), we sought to ascertain nationwide trends in hospitalizations for diverticulitis particularly among cases of younger onset and to evaluate for geographic variations in hospitalization rates within the US.
MATERIALS AND METHODS
Data source
All data were extracted from the NIS between 1998 and 2005. The NIS is maintained as part of the Healthcare cost and utilization project (HCUP) sponsored by the Agency for healthcare research and quality (AHRQ). These databases reflect a 20% stratified sample of non-federal, acute-care hospitals in the United States. The sampling frame includes community and general hospitals and academic medical centers comprising approximately 90% of all hospital discharges in the United States. Hospitals were grouped into 60 strata based on five hospital characteristics: US census region, location (urban versus rural), teaching versus non-teaching status, ownership (non-federal private or public), and bed-size (tertiles). Each data entry included a unique identifier, demographic variables (defined as age, gender, and race/ethnicity, median income for ZIP code), discharge disposition, primary and secondary diagnoses (up to 15), primary and secondary procedures (up to 15), primary insurance payers, total hospital charges, and length of stay. NIS data concurs with the National hospital discharge Survey, supporting data reliability[12].
Eligibility criteria
Our analysis included all hospital discharges between the years of 1998 and 2005 that were admitted with a primary or secondary diagnosis of diverticulitis as identified by Clinical Modification of the international classification of diseases, 9th revision (ICD-9-CM) codes (562.11, 562.13) and with a length of stay greater than 1 d.
Statistical analysis
Data were analyzed using the Stata 10.0 SE software package (Stata Corp LP, College Station, Texas). Analyses took into account the stratified two-stage cluster design using stata’s SVY (survey data) commands and incorporating individual discharge-level weights. Weighting functions using these hospital and discharge weights were applied to the 20% NIS sample to estimate the total number hospitalizations for diverticulitis throughout the US stratified. The primary outcome was rate of hospitalization for diverticulitis in the US population. We used the US resident population census from 1998 to 2005 published by the US Census Bureau as the denominator for rate calculations. We calculated age-adjusted rates with the direct standardization method using the US standard population from 2000. We also calculated age-specific and sex-specific rates of hospitalization for diverticulitis and then calculated the percent increase for each year of the study relative to the baseline rate in 1998 within each age group. These analyses were repeated stratified by the US geographic regions: the Northeast, West, South, and Midwest.
Ethical considerations
The analysis of the Nationwide inpatient sample uses completely unidentified data with no risk of loss of confidentiality and an initial expedited review by the Institutional Review Board of the Johns Hopkins Medical Institutions deemed it exempt from further ethical review.
RESULTS
Demographics of diverticulitis admissions
There were 323 097 hospital admissions for acute diverticulitis in the NIS database between 1998 and 2005. The demographic characteristics of the study population are shown in Table 1 stratified by geographic region. There was a greater proportion of diverticulitis admissions in patients who were 65 and older in the Midwest (50%) and the South (49%) compared to the Northeast (44%) and the West (46%). There was a greater percentage of minority Blacks and Hispanics in the South and the West (Table 1).
Table 1.
Demographics of admissions for acute colonic diverticulitis
|
Geographic region (%) |
||||
| Northeast | Midwest | South | West | |
| Age group | ||||
| 15-24 yr | < 1 | < 1 | < 1 | < 1 |
| 25-44 yr | 17 | 15 | 15 | 16 |
| 45-64 yr | 38 | 35 | 36 | 37 |
| ≥ 65 yr | 44 | 50 | 49 | 46 |
| Sex | ||||
| Male | 42 | 40 | 39 | 43 |
| Female | 58 | 60 | 61 | 57 |
| Race1 | ||||
| Non-hispanic white | 86 | 93 | 80 | 76 |
| Black | 6 | 5 | 9 | 4 |
| Hispanic | 6 | < 1 | 9 | 15 |
| Other | 2 | 2 | 2 | 3 |
Based on admissions with race data which was missing in 25%.
Epidemiological trends
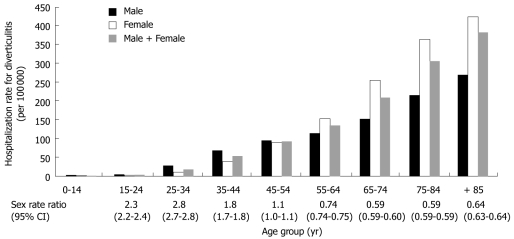
The rate of hospitalization increased with age in both males and females as shown in Figure 1. Diverticulitis admissions were male-predominant in those younger than 44 years with male-to-female ratio that is as high as 2.8 among those between those 25 and 34 years. For those between 45 and 54 years of age, hospitalizations for diverticulitis were similar between sexes, while after age 54 years, it became increasingly female-predominant.
Figure 1.
Age-specific hospitalization rates for diverticulitis stratified by sex in the US. Males are shown in black, females in white, and both sexes in gray. Male-to-female ratios with 95% confidence intervals (95% CI) are shown below each age subgroup.
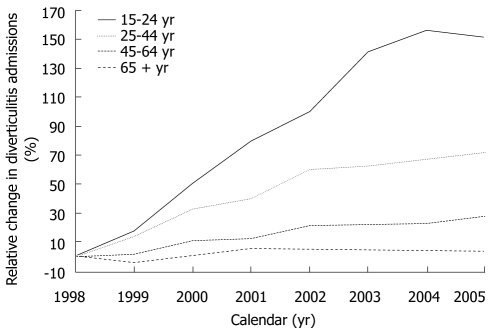
Table 2 shows the age- and sex-specific rates of hospitalization for acute diverticulitis during the 8 year study period. Age-adjusted diverticulitis-associated hospitalizations increased in both males (52.8 to 59.2 per 100 000) and females (67.3 to 79.6 per 100 000) and across all age groups. The overall age-adjusted hospitalization rate for diverticulitis increased from 61.8 per 100 000 to 75.5 per 100 000 during the study period. Figure 2 depicts the relative percentage increase in hospitalization rate for each age group relative to the baseline rate in 1998. This relative increase was inversely proportional with age, being sharpest in those between 15-24 years (150% overall increase), and gradually less with a 70% increase in those aged 25-44 years, 30% increase in those 45-64 years, and approaching 8% in those aged 65 years and older. In 1998, the proportion of admissions for diverticulitis in patients who were older than 65 years was 55%. Over the 8 year study period, that percentage decreased to 44%, with the majority of patients being under the age of 65 years by 2005. Those who were under the age of 45 years comprised 12.7% of all admissions for diverticulitis in 1998 and increased to 16.3% in 2005.
Table 2.
Age- and sex-specific time trends in hospitalization rates for colonic diverticulitis
|
Calendar year hospitalization rates for diverticulitis (per 100 000) |
||||||||
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | |
| 15-24 yr | ||||||||
| M | 1.4 | 1.7 | 1.8 | 2.2 | 2.6 | 3.2 | 3.4 | 3.2 |
| F | 0.5 | 0.6 | 0.9 | 1.1 | 1.3 | 1.3 | 1.4 | 1.6 |
| B | 1.0 | 1.1 | 1.3 | 1.6 | 1.9 | 2.3 | 2.5 | 2.4 |
| 25-44 yr | ||||||||
| M | 33.4 | 38.5 | 44.1 | 47.3 | 54.4 | 55.0 | 55.7 | 57.6 |
| F | 16.6 | 18.9 | 23.3 | 24.2 | 28.1 | 28.5 | 30.8 | 31.7 |
| B | 24.7 | 28.7 | 33.7 | 35.7 | 41.2 | 41.9 | 43.4 | 44.8 |
| 45-64 yr | ||||||||
| M | 84.4 | 90.1 | 98.9 | 97.9 | 107 | 109 | 108 | 117 |
| F | 99.7 | 99.3 | 110 | 114 | 125 | 122 | 126 | 132 |
| B | 92.3 | 94.9 | 105 | 106 | 116 | 116 | 117 | 125 |
| 65+ yr | ||||||||
| M | 181 | 178 | 180 | 189 | 187 | 187 | 182 | 191 |
| F | 322 | 298 | 317 | 329 | 331 | 331 | 323 | 330 |
| B | 264 | 249 | 261 | 271 | 272 | 271 | 265 | 272 |
M: Males; F: Females; B: Both sexes.
Figure 2.
Relative increase in hospitalization rates for diverticulitis in the US between 1998 and 2005, compared to the reference year (1998) stratified by age group.
Geographic variation in diverticulitis admissions
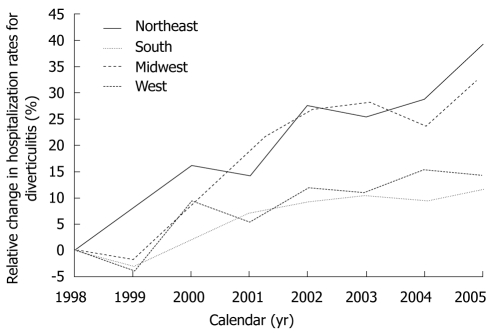
Table 3 shows age-specific and region-specific rates of admissions for diverticulitis. There was significant geographic variation in overall and age-specific growth rate of hospitalizations for acute diverticulitis. The overall age-adjusted rates of diverticulitis-related hospitalizations were 77.7 per 100 000 for the Northeast, 71.0 per 100 000 for the Midwest, 73.9 per 100 000 for the South, and 50.4 per 100 000 for the West. The age-adjusted incidence rate ratio for diverticulitis-associated admission in the West compared to the Northeast was 0.60 (95% CI, 0.59-0.60). There was significant variation in the region-specific proportional change in hospitalization rates relative to the baseline rate in 1998, as shown in Figure 3. The sharpest increases were observed in the Northeast (64.8 to 90.2 per 100 000; overall 39%) and the Midwest (60.5 to 74.8 per 100 000; overall 33%). The trends were more moderate in the South (69.9 to 76.5 per 100 000, overall 11%) and in the West (46.7 to 53.3 per 100 000, overall 14%).
Table 3.
Age- and region-specific time trends in rates of hospitalization for colonic diverticulitis
|
Calendar year rates of hospitalization for diverticulitis (per 100 000) |
||||||||
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | |
| 15-24 yr | ||||||||
| N | 1.4 | 1.8 | 1.6 | 1.8 | 2.2 | 2.7 | 2.9 | 2.9 |
| M | 0.6 | 0.9 | 1.2 | 1.7 | 1.9 | 2.1 | 2.1 | 2.7 |
| S | 1.0 | 0.9 | 1.2 | 1.8 | 2.1 | 2.4 | 2.6 | 2.3 |
| W | 0.9 | 1.2 | 1.6 | 1.2 | 1.4 | 1.9 | 2.2 | 2.0 |
| 25-44 yr | ||||||||
| N | 33.5 | 39.6 | 43.4 | 44.3 | 55.0 | 54.2 | 58.3 | 65.3 |
| M | 24.8 | 27.4 | 31.4 | 37.2 | 41.9 | 42.5 | 44.6 | 48.2 |
| S | 24.9 | 28.5 | 33.8 | 36.7 | 41.6 | 43.1 | 43.3 | 43.6 |
| W | 17.0 | 20.1 | 26.3 | 24.7 | 27.2 | 28.2 | 29.5 | 26.6 |
| 45-64 yr | ||||||||
| N | 106 | 114 | 125 | 126 | 138 | 137 | 147 | 155 |
| M | 85 | 86 | 102 | 108 | 119 | 123 | 115 | 130 |
| S | 105 | 107 | 111 | 113 | 122 | 122 | 119 | 128 |
| W | 66.8 | 67.3 | 78.2 | 73.3 | 83.1 | 81.4 | 89.7 | 87.6 |
| 65+ yr | ||||||||
| N | 245 | 256 | 275 | 260 | 283 | 276 | 267 | 291 |
| M | 271 | 254 | 265 | 298 | 299 | 299 | 285 | 296 |
| S | 304 | 277 | 284 | 302 | 288 | 292 | 290 | 286 |
| W | 206 | 184 | 200 | 199 | 200 | 198 | 196 | 203 |
N: Northeast; M: Midwest; S: South; W: West.
Figure 3.
Relative increase in hospitalization rates for diverticulitis in the US between 1998 and 2005, compared to the reference year (1998) stratified by geographic region.
There was also regional variation in rising incidence of hospitalizations for diverticulitis among those younger than age 45 years. Rates increased the most in the Northeast (from 24.2 to 44.7 per 100 000, overall 85%) and Midwest (from 17.2 to 32.6 per 100 000, overall 90%). The rise in hospitalizations in patients younger than 45 years was more moderate in the South (from 17.5 to 29.9 per 100 000, overall 71%) and was lowest in the West (from 12.1 to 18.4 per 100 000, overall 53%).
DISCUSSION
Our nationwide analysis has demonstrated geographic variations in the burden of diverticulitis and underscores rapidly increasing rates of diverticulitis-associated hospitalizations among individuals younger than age 45 years. These findings have implications for understanding the underlying etiology of diverticulitis as well as for the timely diagnosis of this condition in younger individuals. The rising epidemiological trends and geographic variations in diverticulitis-associated admissions, particularly among younger individuals, may correlate with observed temporal changes and regional differences in diet and obesity in America.
Diverticular disease is an age-related disorder of the large bowel affecting greater than half of the population over the age of 65 years[13]. Current evidence suggests that dietary deficiency (of fibre), colonic pressure, motility changes and colonic structural alterations may collectively contribute to diverticula formation[4]. Parallel epidemiological trends of decreasing dietary fibre and increasing diverticular disease have led to a hypothesized role of fibre deficiency in the pathogenesis of diverticular disease[6,14]. A large prospective study of 43 888 US male health care professionals[15] found that a decreased intake of insoluble dietary fibre, specifically fruits and vegetables, was associated with increased symptomatic diverticular disease. Similarly, obesity has also been linked to higher incidence of diverticulitis and diverticular bleeding[7,8]. It is hypothesized that adipose tissue secretes numerous cytokines that are known to participate in local and generalized inflammation and may play a role in the development of diverticulitis[16].
Our study showed that the overall rates of acute diverticulitis hospitalizations increased in the US in the last decade, which has been previously reported in the US[9] as well as in the UK[17] and Finland[18]. An epidemiological study of adults aged 40-74 years has also shown a rise in obesity, decreased physical activity, and decreased fibre intake which may all contribute to the increasing incidence of diverticular disease[19]. Similarly, a decline in fibre intake among children and 3-fold rise in childhood obesity in the US over the last 3 decades may also partially explain the sharp rise in admissions for diverticulitis among younger age groups[20,21].
The higher prevalence of obesity in the South and Midwest may correlate with our findings of higher rates of diverticulitis admissions in those regions compared to the West. Data from the Center for Disease Control showed that in 1991, the Midwest and the South had higher obesity rates compared to the Northeast and West, and this difference had persisted in the ensuing decade 2000[22]. Data from NHANES-III also showed that BMI was greater in the South and Midwest compared to the other regions[23]. Childhood obesity has been similarly shown to be most prevalent in the South ( ≥ 18%) while being least prevalent in the West (11.4%)[20].
Regional variation in diet may also contribute to geographic differences in diverticulitis admissions. Based on self-reported data, residents from the South consumed more fatty acids and the least amount of fibre, while those from the West consumed higher amounts of fibre than other regions[23]. One could hypothesize that there may be a protective association between higher fibre intake in the West and corresponding relatively lower age-adjusted rates of diverticulitis admissions. However, the roles of dietary fibre and obesity in geographic variations in diverticulitis remain speculative, and do not explain high rates of diverticulitis admissions in the Northeast. Thus, other environmental and health systems-based factors may be involved. Racial and ethnic differences in risk of diverticulitis may also contribute to geographic variations in hospital admissions for diverticulitis, particularly in the West, where there is a higher composition of Hispanics and Asians. There is evidence that these ethnic groups may be at lower risk for diverticulitis[24,25]. Unfortunately, because nearly 25% of racial and ethnic data is missing in the NIS database, we were not able to readily determine race- and ethnic-specific rates in diverticulitis admissions.
Our current study has several limitations inherent to administrative data analyses. The NIS data set does not contain personal identifiers, which does not allow linkage to medical records in order to validate ICD-9 codes for diverticulitis. However, we would not expect the degree of errors in administrative coding to be different with respect to time or age. Thus, this type of non-differential misclassification usually leads to conservative estimates of temporal trends. Additionally, this study evaluated only rates of hospitalization, and would not have included milder cases of diverticulitis managed in an outpatient setting. Furthermore, this is a cross-sectional study and we are unable to longitudinally follow patients after discharge to assess long-term mortality and morbidity such as recurrent diverticulitis or surgery.
Despite these limitations, this nationally representative analysis has demonstrated geographic variations in epidemiological trends in the burden of diverticulitis that will hopefully stimulate hypotheses into the aetiology of diverticular disease. Prospective studies are needed to determine if there is an association between diverticulitis and obesity, dietary intake, and other environmental factors, particularly among younger adults. From a clinical perspective, these findings drive the need for increased vigilance for diverticular disease among younger adults presenting with abdominal pain.
COMMENTS
Background
The incidence of diverticular disease increases with age. Between 10%-25% of individuals with colonic diverticula develop diverticulitis. Recent epidemiologic studies have shown a male predominant increase in diverticulitis in those under 45 years.
Research frontiers
The nationally representative analysis indicates that the burden of diverticulitis and the time trends in admissions vary by geographic region and may be associated with a decreased intake of insoluble dietary fibre and increasing obesity.
Innovations and breakthroughs
The steep rise in diverticulitis admissions among young adults is striking. From a clinical perspective, these findings drive the need for increased vigilance for diverticular disease among younger adults presenting with abdominal pain.
Applications
Prospective studies are needed to determine if there is an association between diverticulitis and obesity, dietary intake, and other environmental factors, particularly among younger adults.
Peer review
While this study is not entirely unique, it is well-written and would make a useful addition to the current literature on diverticular disease.
Footnotes
Supported by An AGA Research Scholar Award to Nguyen GC
Peer reviewer: Graham MacKay, MRCS (Glasgow), MBChB, MD, University Department of Surgery, Western Infirmary, Dumbarton Road, Glasgow, G11 6NT, United Kingdom
S- Editor Tian L L- Editor O’Neill M E- Editor Ma WH
References
- 1.Kozak LJ, DeFrances CJ, Hall MJ. National hospital discharge survey: 2004 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2006:1–209. [PubMed] [Google Scholar]
- 2.Papagrigoriadis S, Debrah S, Koreli A, Husain A. Impact of diverticular disease on hospital costs and activity. Colorectal Dis. 2004;6:81–84. doi: 10.1111/j.1463-1318.2004.00532.x. [DOI] [PubMed] [Google Scholar]
- 3.Aldoori W, Ryan-Harshman M. Preventing diverticular disease. Review of recent evidence on high-fibre diets. Can Fam Physician. 2002;48:1632–1637. [PMC free article] [PubMed] [Google Scholar]
- 4.Heise CP. Epidemiology and pathogenesis of diverticular disease. J Gastrointest Surg. 2008;12:1309–1311. doi: 10.1007/s11605-008-0492-0. [DOI] [PubMed] [Google Scholar]
- 5.Kang JY, Melville D, Maxwell JD. Epidemiology and management of diverticular disease of the colon. Drugs Aging. 2004;21:211–228. doi: 10.2165/00002512-200421040-00001. [DOI] [PubMed] [Google Scholar]
- 6.Korzenik JR. Case closed? Diverticulitis: epidemiology and fiber. J Clin Gastroenterol. 2006;40 Suppl 3:S112–S116. doi: 10.1097/01.mcg.0000225503.59923.6c. [DOI] [PubMed] [Google Scholar]
- 7.Strate LL, Liu YL, Aldoori WH, Syngal S, Giovannucci EL. Obesity increases the risks of diverticulitis and diverticular bleeding. Gastroenterology. 2009;136:115–122.e1. doi: 10.1053/j.gastro.2008.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schauer PR, Ramos R, Ghiatas AA, Sirinek KR. Virulent diverticular disease in young obese men. Am J Surg. 1992;164:443–446; discussion 446-448. doi: 10.1016/s0002-9610(05)81177-8. [DOI] [PubMed] [Google Scholar]
- 9.Etzioni DA, Mack TM, Beart RW Jr, Kaiser AM. Diverticulitis in the United States: 1998-2005: changing patterns of disease and treatment. Ann Surg. 2009;249:210–217. doi: 10.1097/SLA.0b013e3181952888. [DOI] [PubMed] [Google Scholar]
- 10.Marinella MA, Mustafa M. Acute diverticulitis in patients 40 years of age and younger. Am J Emerg Med. 2000;18:140–142. doi: 10.1016/s0735-6757(00)90004-4. [DOI] [PubMed] [Google Scholar]
- 11.Acosta JA, Grebenc ML, Doberneck RC, McCarthy JD, Fry DE. Colonic diverticular disease in patients 40 years old or younger. Am Surg. 1992;58:605–607. [PubMed] [Google Scholar]
- 12.Whalen D, Houchens R, ELixhauser A. 2002 HCUP nationwide Inpatient Sample (NIS) comparison report #2005-03 ed. Rockville, MD: US. Agency for Healthcare Research and Quality; 2005. pp. 1–89. [Google Scholar]
- 13.Commane DM, Arasaradnam RP, Mills S, Mathers JC, Bradburn M. Diet, ageing and genetic factors in the pathogenesis of diverticular disease. World J Gastroenterol. 2009;15:2479–2488. doi: 10.3748/wjg.15.2479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization. Br Med J. 1971;2:450–454. doi: 10.1136/bmj.2.5759.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aldoori WH, Giovannucci EL, Rockett HR, Sampson L, Rimm EB, Willett WC. A prospective study of dietary fiber types and symptomatic diverticular disease in men. J Nutr. 1998;128:714–719. doi: 10.1093/jn/128.4.714. [DOI] [PubMed] [Google Scholar]
- 16.Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. Gastroenterology. 2007;132:2169–2180. doi: 10.1053/j.gastro.2007.03.059. [DOI] [PubMed] [Google Scholar]
- 17.Kang JY, Hoare J, Tinto A, Subramanian S, Ellis C, Majeed A, Melville D, Maxwell JD. Diverticular disease of the colon--on the rise: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003;17:1189–1195. doi: 10.1046/j.1365-2036.2003.01551.x. [DOI] [PubMed] [Google Scholar]
- 18.Mäkelä J, Kiviniemi H, Laitinen S. Prevalence of perforated sigmoid diverticulitis is increasing. Dis Colon Rectum. 2002;45:955–961. doi: 10.1007/s10350-004-6335-5. [DOI] [PubMed] [Google Scholar]
- 19.King DE, Mainous AG 3rd, Carnemolla M, Everett CJ. Adherence to healthy lifestyle habits in US adults, 1988-2006. Am J Med. 2009;122:528–534. doi: 10.1016/j.amjmed.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Singh GK, Kogan MD, van Dyck PC. A multilevel analysis of state and regional disparities in childhood and adolescent obesity in the United States. J Community Health. 2008;33:90–102. doi: 10.1007/s10900-007-9071-7. [DOI] [PubMed] [Google Scholar]
- 21.Saldanha LG. Fiber in the diet of US children: results of national surveys. Pediatrics. 1995;96:994–997. [PubMed] [Google Scholar]
- 22. Available from: http://obesity1.tempdomainname.com/subs/fastfacts/obesity_US.shtml.
- 23.Hajjar I, Kotchen T. Regional variations of blood pressure in the United States are associated with regional variations in dietary intakes: the NHANES-III data. J Nutr. 2003;133:211–214. doi: 10.1093/jn/133.1.211. [DOI] [PubMed] [Google Scholar]
- 24.Martel J, Raskin JB. History, incidence, and epidemiology of diverticulosis. J Clin Gastroenterol. 2008;42:1125–1127. doi: 10.1097/MCG.0b013e3181865f18. [DOI] [PubMed] [Google Scholar]
- 25.Hjern F, Johansson C, Mellgren A, Baxter NN, Hjern A. Diverticular disease and migration--the influence of acculturation to a Western lifestyle on diverticular disease. Aliment Pharmacol Ther. 2006;23:797–805. doi: 10.1111/j.1365-2036.2006.02805.x. [DOI] [PubMed] [Google Scholar]