Abstract
Background
Cardio-pulmonary interactions play an important role in the pathophysiology of hypoplastic left heart syndrome (HLHS). Pulmonary vasculopathy has been identified, especially in those with restrictive/intact atrial septum (R/IAS). Responsiveness of the pulmonary vasculature to maternal hyperoxygenation (MH) may provide a tool to assess the degree of pulmonary vasculopathy present prior to birth.
Methods and Results
Doppler echocardiography was performed in 27 normal and 43 HLHS fetuses. In HLHS, sampling was repeated after 10 minutes of MH with 60% FiO2, and after 5 minutes of recovery. Sampling was performed in the proximal, mid-portion, and distal branch pulmonary artery (PA). Pulsatility index (PI) was used as a measure of vascular impedance. Of the HLHS fetuses, 34 had an open inter-atrial septum and 9 had a R/IAS. At birth, 5 fetuses underwent immediate intervention on the inter-atrial septum. Middle cerebral artery PI was lower in HLHS vs. normals (p<0.001). There was no difference in umbilical artery, ductus arteriosus, or branch PA PI between normals and HLHS. MH led to a significant decrease in PI at each of the PA sites sampled in fetuses with an open atrial septum (p<0.001); however, there no was significant change in the PI in fetuses that required immediate intervention on the atrial septum at birth. Using a cutoff value of <10% vasoreactivity, the sensitivity of MH testing for determining need for immediate intervention at birth is 100% [0.46-1.0], specificity 94% [0.78-.99], positive predictive value 71% [0.30-0.95], and negative predictive value 100% [0.86-1.0]. No untoward effects were seen with MH.
Conclusions
PA vasoreactivity to MH occurs in the fetus with HLHS. MH testing accurately identifies fetuses requiring urgent postnatal intervention at birth and may be used to select candidates for fetal atrial septoplasty.
Keywords: congenital heart defects, fetal echocardiography, oxygen, hypoplastic left heart syndrome
Introduction
Hypoplastic left heart syndrome (HLHS) is one of the most challenging forms of congenital heart disease to treat, however survival in the current era continues to improve1. Paralleling the improvement in operative outcome is the increased frequency of prenatal diagnosis of HLHS2. Fetal echocardiography allows for an early and accurate diagnosis of this anomaly, allows for the opportunity to investigate the unique cardiovascular physiology of this anomaly in the 2nd and 3rd trimesters of pregnancy, and facilitates the ability to implement immediate management at birth3-5. Understanding the developmental aspects of HLHS prior to birth can provide new knowledge and the potential for new treatment strategies that may contribute to improved outcomes in the future.
Critical to a successful postnatal strategy for HLHS is the status of the pulmonary vasculature, of which little is known prior to birth. While only a small proportion of the overall fetal cardiac output is normally directed into the pulmonary vasculature, this flow is critical for healthy pulmonary vascular development6-9. In the fetus with HLHS, the entire cardiac output must traverse the main pulmonary artery and the quantity of blood flow directed into the branch pulmonary arteries may differ from normal. In addition, blood returning from the pulmonary vasculature via the pulmonary veins must cross the atrial septum from left atrium to right; hence, the degree of patency of the atrial septum influences the capacity for pulmonary venous drainage from the lungs.
Infants with HLHS and a restrictive (RAS) or intact atrial septum (IAS) have a particularly poor prognosis4, 10, 11. Obstruction to left atrial egress leads to marked changes in the pulmonary vasculature, which may persist despite successful opening of the atrial septum and decompression of the left atrium after birth4, 10, 11. Postnatal autopsy studies have demonstrated “arterialization” of the pulmonary veins and dilation of the lymphatics12-14. A mechanism for evaluating the prenatal status of the pulmonary vasculature in the fetus with HLHS would be of great value as it could identify the fetus that could benefit from either prenatal intervention or immediate, urgent postnatal care.
In our study, we sought to investigate the pulmonary vasculature in the fetus with HLHS by assessing for changes in the Doppler derived pulsatility index (PI), a surrogate measure of vascular impedance, within the branch pulmonary arteries in response to maternal hyperoxygenation (MH). In normal fetuses, a decrease in vascular impedance in response to MH occurs after 31 weeks gestation, termed pulmonary vasoreactivity.15 Lack of vasoreactivity in response to MH has served as a useful clinical tool in predicting lethal pulmonary hypoplasia in conditions such as congenital diaphragmatic hernia, renal abnormalities, or chronic premature rupture of membranes16. We hypothesized that fetuses with HLHS and an abnormal pulmonary vascular bed due to atrial septal restriction would not demonstrate normal vasoreactivity in response to MH, thereby accurately identifying fetuses at risk.
The purpose of our study was to 1) establish a protocol and determine the safety of MH in the fetus with HLHS, 2) describe the response of the pulmonary vasculature to MH in the fetus with an open atrial septum, and 3) determine whether the response of the pulmonary vasculature to MH could correctly discriminate between the well newborn with HLHS and the one who will need immediate, urgent left atrial decompression at birth.
Methods
Study Population
A cross-sectional, prospective investigation was undertaken. The study population consisted of pregnant women referred for fetal echocardiography to the Fetal Heart Program at the Children's Hospital of Philadelphia from January 2004 to September 2008. Inclusion criteria consisted of singleton fetuses with HLHS and no extracardiac anatomic abnormalities and normal utero-placental function. As controls for comparison, fetuses with normal cardiovascular anatomy, normal utero-placental function, and no extra-cardiac anatomic abnormalities of hemodynamic significance were recruited. Fetuses were excluded for gestational age < 18 weeks or > 40 weeks, persistent non-sinus rhythm, or a maternal condition potentially affecting fetal hemodynamics, such as gestational diabetes, thyroid disease, or pre-eclampsia. Institutional Review Board permission for the study was granted (CHOP IRB #2004-10-3948).
Fetal Echocardiography
A complete standard-of-care fetal echocardiogram was performed in room air (baseline study). For each study, multiple tomographic views of the fetal heart were obtained17 using a Siemens Sequoia 512 coupled with a 6C2 transducer. After confirming the presence of either normal or HLHS anatomy, informed consent for study participation was obtained. In normal and HLHS fetuses, vascular impedance was measured using the pulsatility index [PI = (peak systolic velocity – end-diastolic velocity)/ mean velocity]. PI values were measured in the umbilical artery, middle cerebral artery, and ductus arteriosus. As previous investigators have demonstrated, Doppler signals vary based on location of sampling within the pulmonary vasculature18-22. In order to standardize a MH protocol for future studies, we chose to obtain PI values from three specific sites within the pulmonary artery – the proximal, mid, and distal branch pulmonary artery locations. The proximal branch pulmonary artery was defined as the first segment just distal to the take-off from the patent ductus arteriosus (PA 1); mid branch pulmonary artery was the most distal aspect of the pulmonary artery in the extra-parenchymal segment, just before the vessel enters the lung parenchyma (PA 2); and distal branch pulmonary artery was defined as the intra-parenchymal segment at the first branching point within the lung (PA 3) (see figure 1). Either the right or left pulmonary artery was selected for analysis based upon the position of the fetus with an angle of interrogation < 10 degrees. The right, left, and combined ventricular cardiac outputs indexed to estimated gestational weight were recorded as previously described23. Qualitative assessments of right ventricular function and degree of tricuspid regurgitation were made. In HLHS fetuses, the right ventricular cardiac output was recorded alone, as the left ventricular cardiac output was assumed to be negligible. For all parameters, 3 measurements were made at the time of examination and the results were averaged for further analysis.
Figure 1.
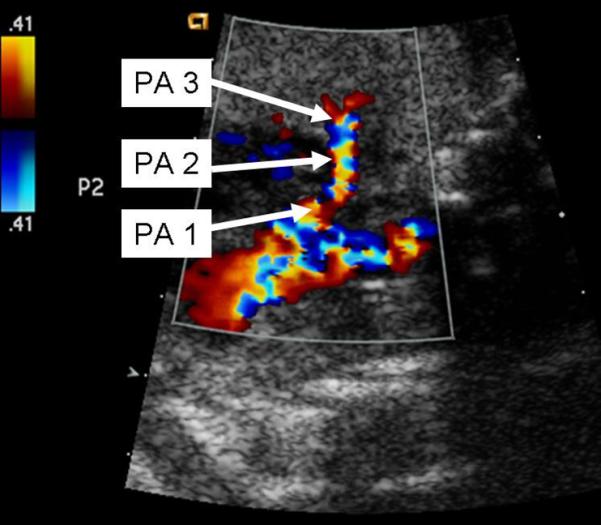
Sites of branch pulmonary artery sampling via Doppler echocardiography.
Normal fetuses (n=27) were scanned only once while the mother was breathing room air. HLHS fetuses (n=43) were scanned according to a three-phase protocol—room air, MH, and recovery. During MH, the mother was administered 100% FiO2 via a non-rebreather face mask at 8L of flow—effectively providing a FiO2 of 60% for 10 minutes. This protocol for MH has been previously established as an effective means for delivering supplemental oxygen to the fetus15. The fetal echocardiogram was repeated while the mother was breathing 60% oxygen and the study parameters listed above were recorded. Oxygen was then discontinued for at least 5 minutes and follow-up imaging performed while the mother was now breathing room air (recovery phase). During this recovery phase, qualitative assessments of right ventricular function, graded as either normal or depressed, and degree of tricuspid regurgitation, graded as either none, trivial or mild; moderate; or severe, were made to ensure that MH did not cause any harmful changes in these parameters. In addition, the ductus arteriosus and umbilical artery were reimaged to ensure that MH did not cause either ductal constriction, as previously defined as a pulsatility index in the ductus arteriosus < 1.924, or placental insufficiency. Fetuses with HLHS underwent one or more examinations during gestation according to the protocol outlined above.
In HLHS fetuses, an assessment of the inter-atrial communication was performed. The atrial septum was considered intact if there was no opening seen on 2-dimensional imaging and no flow across seen on color Doppler flow mapping. The inter-atrial communication was considered restrictive if the 2-dimensional measurement was < 3mm, if there was flow acceleration across the patent foramen ovale > 1m/s with no return to baseline, and if the pulmonary venous Doppler flow pattern revealed significant reversal in the pulmonary veins with atrial contraction, as previously described3, 25-28. In all fetuses deemed to have a restrictive inter-atrial communication, the last examination performed prior to delivery was after 32.9 weeks gestation.
Postnatal data
Postnatal data was obtained on each HLHS fetus that underwent care at our institution. Postnatal data included oxygen saturation at birth, pH, PaO2, and PaCO2 from initial arterial blood gas, weight at birth, the inspired oxygen content and requirement for mechanical ventilation at birth, and the need for urgent intervention to open the atrial septum due to hypoxemia.
Statistical Analysis
All continuous variables were normally distributed. Consequently, for each parameter, the mean and standard deviations were calculated. For the purposes of statistical analysis, only the first scan of each HLHS fetus during the phase I baseline, room air study was compared to the frequency matched normal control population via unpaired student's t-tests. HLHS fetuses were subdivided into groups depending upon whether there was an open (n=34) vs. restrictive/intact atrial septum (n=9). Paired student's t-tests were used to compare HLHS phase I baseline room air studies to HLHS phase II MH studies. For the purposes of statistical analysis, only the last scan prior to delivery of each HLHS fetus was included in this phase of the analysis since vasoreactivity in response to MH has only been reported in normal fetuses after 31 weeks gestation. Analysis was performed for the entire HLHS cohort as well as the subgroups with an open and with a restrictive/intact inter-atrial communication. Within the subgroup analysis, adjustments for multiple comparisons were made with the Bonferroni correction. To assess safety of MH for HLHS fetuses, the ductus arteriosus and umbilical artery were compared via repeated measures ANOVA analysis at baseline, during MH, and during recovery. Qualitative right ventricular function was assessed with McNemar's test at baseline and after MH, while the degree of tricuspid regurgitation was analyzed with the Wilcoxon signed rank test at baseline and after MH. Pulmonary vasoreactivity was reported as the percent change in PI at MH relative to baseline. Trends in pulmonary vasoreactivity over the course of gestation were assessed for the open atrial septum subgroup (n=34) and the restrictive atrial septum group (n=9) via linear regression analysis. The coefficient of determination, R2, was calculated for each model. In this regression analysis, only the maximal vasoreactivity data from the last scan prior to delivery was included. All values were considered statistically significant at a p<0.05. Finally, the sensitivity, specificity, positive predictive value, and negative predictive value of MH testing, with 95% confidence intervals, for predicting the need for urgent intervention on the inter-atrial septum at birth were determined.
Results
Study Population
There were 27 normal control and 43 HLHS fetuses enrolled in the study. Each HLHS fetus underwent one or more evaluations over the course of gestation for a total of 68 echocardiographic evaluations. Of the HLHS fetuses, 9 had a restrictive/intact inter-atrial communication and 34 HLHS fetuses had an open inter-atrial communication.
Comparison of Normal fetuses to HLHS fetuses During Room Air
Table 1 summarizes the results for the normal control population compared to the first scan of the HLHS population during the room air phase of the study. There were no significant differences in gestational age, estimated fetal weight, umbilical artery PI, ductus arteriosus PI, mid branch pulmonary artery PI, or distal branch pulmonary artery PI. MCA PI was significantly lower in the HLHS group than in the normal control group. In addition, the indexed right ventricular cardiac output for the HLHS population was lower than the indexed combined cardiac output for the normal control population, as we have previously reported29. The proximal branch pulmonary artery PI trended lower in the normal control population compared to the HLHS population, although it did not meet statistical significance (p=0.053).
Table 1.
Room Air—Normal vs. HLHS
| Normal (n=27) | HLHS-RA (n=43) | P-value* | |
|---|---|---|---|
| GA (weeks) | 30.1 ± 4.5 | 29.6 ± 5.0 | 0.72 |
| Fetal weight (kg) | 1.66 ± 0.76 | 1.59 ± 0.91 | 0.76 |
| UA PI | 1.15 ± 0.21 | 1.18 ± 0.23 | 0.59 |
| MCA PI | 2.17 ± 0.40 | 1.76 ± 0.31 | <0.001* |
| DA PI | 2.85 ± 0.29 | 2.94 ± 0.32 | 0.24 |
| PA 1 PI | 3.16 ± 0.49 | 3.42 ± 0.54 | 0.053 |
| PA 2 PI | 3.44 ± 0.53 | 3.60 ± 0.58 | 0.29 |
| PA 3 PI | 3.93 ± 0.72 | 4.07 ± 0.69 | 0.42 |
| CCO or RVCO (cc/kg/min) | 457 ± 71 | 414 ± 89 | 0.047* |
Results are expressed as mean ± standard deviation.
P-value has been calculated using independent sample t-test.
Comparison of Room Air HLHS fetuses to MH HLHS fetuses
Table 2 illustrates the comparison between the HLHS cohort during the room air phase of the study to the HLHS cohort during MH. With MH, there was no significant change in the indexed right ventricular cardiac output. There was a trend toward an increase in the MCA PI with MH, although it did not meet statistical significance. There was a statistically significant decrease in the proximal (PA1), mid (PA2), and distal (PA3) pulmonary artery PI during MH, with the greatest degree of change taking place at PA3.
Table 2.
Comparison of HLHS conditions (RA vs. MH)
| HLHS condition(n=43) |
P-value* | ||
|---|---|---|---|
| RA | MH | ||
| MCA PI | 1.59 ± 0.36 | 1.67 ± 0.29 | 0.059 |
| PA 1 PI | 3.2 ± 0.59 | 2.85 ± 0.43 | <0.001* |
| PA 2 PI | 3.53 ± 0.59 | 3.1 ± 0.48 | <0.001* |
| PA 3 PI | 4.1 ± 0.68 | 3.35 ± 0.52 | <0.001* |
| RVCO (cc/kg/min) | 414.6 ± 96.2 | 419.4 ± 103.7 | 0.625 |
Results are expressed as mean ± standard deviation.
P-value has been calculated using Paired t-test
Comparison of HLHS fetuses during Room Air, MH, and Recovery
There was no significant difference in the PI of the ductus arteriosus or in the umbilical artery in the baseline room air study compared to MH study or to the recovery study (Table 3). The PI in the ductus arteriosus increased slightly in response to MH, although it did not reach statistical significance. Importantly, no significant ductal constriction was noted with MH. There was no significant change in the degree of tricuspid regurgitation between the phases of the study. In the baseline studies, there were 36 fetuses with trivial or mild tricuspid regurgitation, 5 with moderate regurgitation, and 1 with severe regurgitation. In the MH and recovery phases, there were 39 fetuses with trivial or mild regurgitation, 3 with moderate regurgitation, and none with severe regurgitation (p = 0.10). Similarly, there were no significant changes in qualitative right ventricular function between the phases of the studies. In the baseline studies, there were 42 fetuses with good function and 1 fetus with depressed function. In the MH and recovery phases, there were 43 fetuses with good function and no fetuses with depressed function (p = 1.0).
Table 3.
Comparison of HLHS conditions (RA vs. MH vs. Recovery)
| HLHS condition (n=43) |
P-value* | |||
|---|---|---|---|---|
| RA | MH | Recovery | ||
| UA PI | 1.15 ± 0.22 | 1.18 ± 0.25 | 1.15 ± 0.43 | 0.689 |
| DA PI | 2.84 ± 0.34 | 2.98 ± 0.31 | 2.97 ± 0.33 | 0.084 |
Results are expressed as mean ± standard deviation.
P-value has been calculated using repeated measure of ANOVA.
Differences in response to MH between the fetuses with HLHS - open atrial septum versus HLHS - restrictive/intact atrial septum
Tables 4 and 5 list the change in response to MH in HLHS fetuses with an open (n=34) compared to a restrictive/intact atrial septum (n=9), respectively. There was a significant decrease in PI for all three PA sites in the HLHS – open atrial septum group. However, there was no significant decrease in PI for all three PA sites in the HLHS – restrictive/intact atrial septum group.
Table 4.
HLHS-RA (open septum) vs. HLHS-MH (open septum)
| HLHS condition(n=34) |
P-value* | ||
|---|---|---|---|
| RA | MH | ||
| UA PI | 1.16 ± 0.23 | 1.18 ± 0.25 | 0.588 |
| MCA PI | 1.61 ± 0.38 | 1.68 ± 0.32 | 0.186 |
| DA PI | 2.84 ± 0.36 | 2.94 ± 0.29 | 0.193 |
| PA 1 PI | 3.3 ± 0.61 | 2.82 ± 0.45 | <0.001§ |
| PA 2 PI | 3.59 ± 0.60 | 3.02 ± 0.43 | <0.001§ |
| PA 3 PI | 4.05 ± 0.69 | 3.27 ± 0.44 | <0.001§ |
| RVCO (cc/kg/min) | 409.3 ± 91.5 | 415.1 ± 94.26 | 0.614 |
Results are expressed as mean ± standard deviation.
P-value has been calculated using Paired t-test.
P-value indicates significant difference between RA and MH based on Bonferroni correction (α/2=0.05/2=0.025).
Table 5.
HLHS-RA (R/IAS) vs. HLHS-MH (R/IAS)
| HLHS condition(n=9) |
P-value* | ||
|---|---|---|---|
| RA | MH | ||
| UA PI | 1.15 ± 0.24 | 1.21 ± 0.23 | 0.447 |
| MCA PI | 1.53 ± 0.30 | 1.64 ± 0.22 | 0.110 |
| DA PI | 2.80 ± 0.31 | 3.03 ± 0.24 | 0.209 |
| PA 1 PI | 3.1 ± 0.49 | 2.95 ± 0.36 | 0.498 |
| PA 2 PI | 3.25 ± 0.48 | 3.39 ± 0.57 | 0.615 |
| PA 3 PI | 4.18 ± 0.68 | 3.67 ± 0.70 | 0.101 |
| RVCO (cc/kg/min) | 439.1 ± 122.5 | 439.6 ± 149.5 | 0.980 |
Results are expressed as mean ± standard deviation.
P-value has been calculated using Paired t-test and significance level has been identified based on Bonferroni correction (α/2=0.05/2=0.025).
Trends in pulmonary vasoreactivity according to gestational age in HLHS fetuses with open vs. restrictive/intact inter-atrial septum
Figure 2 demonstrates the scatterplot of the greatest percentage change in PI with MH at either the proximal (PA1), mid (PA2), or distal (PA3) pulmonary artery vs. gestational age in HLHS fetuses with an open (n=34) and with a restrictive inter-atrial (n=9) communication. Fetuses who required a postnatal intervention are labeled with a “1”, while fetuses who did not require a postnatal intervention at birth are labeled with a “0.” In fetuses with an open inter-atrial septum, vasoreactivity increased over the course of gestation. By regression analysis, the observed trend was statistically significant, F= 4.3, p = 0.046 according to the equation y = 0.179x +28.2. The R2 = 0.12, however, is low, suggesting significant variability in the acquisition of vasoreactivity in HLHS fetuses with an open inter-atrial communication. In contrast, in the 9 fetuses with a restrictive inter-atrial communication, there was no significant trend in vasoreactivity over the course of gestation, F= 0.48, p = 0.51 according to the equation y= -1.159x + 52.6.
Figure 2.
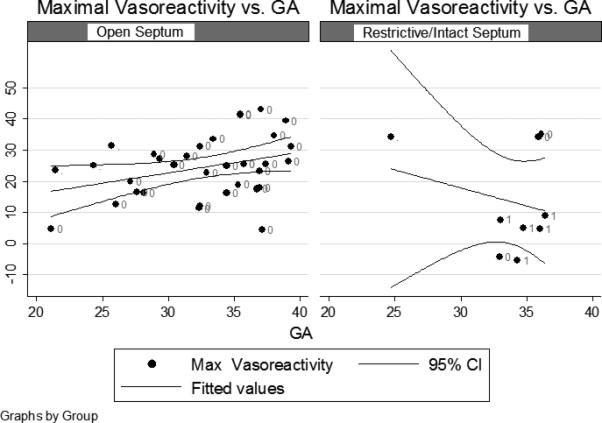
Maximal vasoreactivity at any pulmonary artery branch point versus gestational age for HLHS fetuses with an open inter-atrial septum (shown on the left) and HLHS fetuses with a restrictive/intact atrial septum (shown on the right). Fetuses not requiring an intervention on the inter-atrial septum are labeled with a “0”, while fetuses requiring intervention on the inter-atrial septum are labeled with a “1.” The linear regression and 95% confidence intervals are also illustrated for both groups.
Postnatal findings
Postnatal data was available for 38 of 43 HLHS fetuses. In our prenatal cohort, there were 2 terminations of pregnancy and 3 fetuses delivered at outside hospitals. Of the 5 fetuses with no postnatal data available, 4 had open inter-atrial communications and 1 had a restrictive inter-atrial communication. At birth, 9 neonates (24%) required supplemental oxygen, and 11 neonates (29%) required mechanical ventilation prior to surgery. Of those requiring supplemental oxygen, 6/9 (67%) were deemed to have a restrictive/intact atrial septum prenatally. Of the 30 fetuses deemed to have an open inter-atrial communication, none required an immediate intervention on the atrial septum postnatally. Of the 8 fetuses with a restrictive inter-atrial communication, 5 required an immediate intervention on the inter-atrial septum at birth. One had a surgical atrial septectomy and died prior to Stage 1. Four neonates had a stent placed across the atrial septum in the catheterization lab and 3 of these neonates survived to discharge from the hospital. All of these 5 fetuses who required immediate intervention of the inter-atrial septum had < 10% vasoreactivity on the last scan prior to delivery. Based upon the findings of this study, we defined a cutoff value for vasoreactivity in response to MH in HLHS fetuses of < 10% on the last scan prior to delivery. Using this cutoff value of < 10% vasoreactivity on the final scan performed after 31 weeks gestation, the sensitivity of MH vasoreactivity testing for determining the need for intervention on the atrial septum was 100% [0.46-1.0], the specificity was 94% [0.78-0.99], the positive predictive value was 71% [0.30-0.95], and the negative predictive value was 100% [0.86-1.0]. In our cohort, there were 2 false positive tests, defined as no need for urgent intervention on the inter-atrial septum with < 10% vasoreactivity on the last scan prior to delivery. One fetus, scanned at 37.1 weeks gestation had an open inter-atrial septum and did not require supplemental oxygen at birth. Conversely, the other fetus, scanned at 32.9 weeks gestation, had a restrictive inter-atrial septum prenatally. At birth, this baby required intubation with 25% FiO2 in the neonatal period and then proceeded non-urgently to a stage I reconstruction.
Discussion
MH testing is a safe and useful tool to assess the pulmonary vasculature in fetuses with HLHS. There were no adverse consequences associated with MH testing. Through all phases of testing, qualitative assessments of right ventricular function and degree of tricuspid regurgitation remained the same. Moreover, there was no significant change in right ventricular cardiac output with MH. Finally, there was no ductal constriction noted in during MH or during the recovery period.
MH testing correctly identified HLHS fetuses that required urgent intervention on the inter-atrial septum at birth. None of the HLHS fetuses with appropriate vasoreactivity on the last scan prior to delivery required an urgent intervention on the inter-atrial septum at birth. In fact, two fetuses deemed to have a restrictive inter-atrial communication by previously published criteria3, 26, 28 were vasoreactive in response to MH in late third-trimester testing. At birth, both babies had good oxygen saturations while breathing room air. Figure 3 illustrates the pulmonary venous Doppler flow patterns and vasoreactivity testing for one of these fetuses. Rasanen defined vasoreactivity as a decrease in the pulsatility index of the branch pulmonary artery > 20% after 31 weeks gestation in normal fetuses15. Based upon review of our results, however, we defined vasoreactivity in our HLHS cohort as a decline in the PI of greater than 10% at any branch point. HLHS fetuses with no decline in the PI at any branch point greater than 10% were considered to be non-vasoreactive in response to MH. Vasoreactivity was noted as early as 24 weeks gestation in one fetus with a restrictive inter-atrial communication. A second fetus with a restrictive inter-atrial communication demonstrated vasoreactivity at 26 weeks gestation, but lost vasoreactivity by 32 weeks gestation. Indeed, by providing a window for intervention, MH testing may prove useful when deciding upon a fetal intervention to open up a restrictive inter-atrial communication. We propose the routine incorporation of MH testing for late 3rd trimester HLHS fetuses to assess the health of the pulmonary vasculature and to identify fetuses at greatest risk for postnatal pulmonary venous obstruction.
Figure 3.
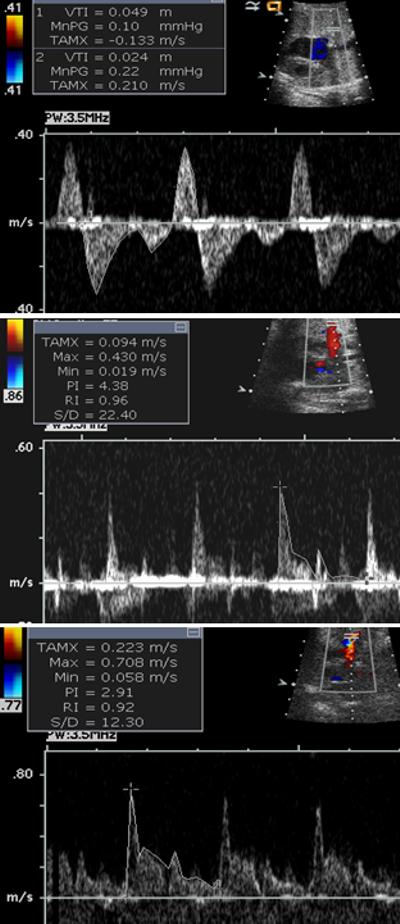
The top panel illustrates the pulmonary venous Doppler flow pattern in a fetus with HLHS and a restrictive inter-atrial communication. The bottom two panels demonstrate MH testing for this same fetus. The middle panel demonstrates the distal branch pulmonary artery Doppler flow pattern during the room air phase of the study while the bottom panel demonstrates this Doppler flow pattern during MH. Despite having a restrictive inter-atrial communication by previously reported criteria, there is significant vasoreactivity in response to MH. At birth, this fetus had adequate oxygen saturations while breathing room air.
Our study suggests that pulmonary vascular impedance is similar in HLHS fetuses compared to normal controls at baseline. The PI at the proximal, mid, and distal branch pulmonary artery was higher in our HLHS population compared to our normal control population at baseline; however, none met statistical significance (Table 1). Histopathologic changes within the pulmonary vasculature in HLHS fetuses have been well described in the postnatal literature12-14, 30, 31. It is conceivable that subtle changes within the pulmonary vasculature are present in HLHS fetuses in utero, accounting for the mildly elevated PI at each branch pulmonary artery site compared to normal controls. Alternatively, the mildly elevated PI seen within the pulmonary vasculature may simply reflect altered flow patterns within the HLHS fetus. As we have previously reported, fetuses with HLHS have statistically lower cardiac outputs compared to normal control fetuses29 (see Table 1). In the setting of a reduced cardiac output, blood may be preferentially shunted away from less vital organs, such as the lungs, and toward more vital structures, such as the brain, accounting for the overall mild increase in pulmonary vascular impedance and lower resistance in the cerebral vasculature compared to normal controls.
HLHS fetuses with an open inter-atrial communication acquire vasoreactivity over the course of gestation. However, fetuses with a restrictive inter-atrial septum did not demonstrate a significant change in vasoreactivity over the course of gestation (Figure 2). One fetus with a restrictive inter-atrial septum demonstrated vasoreactivity at 26 weeks gestation, but lost vasoreactivity by 32 weeks gestation. We hypothesize that HLHS fetuses with a restrictive inter-atrial communication have elevated pressures within the pulmonary vasculature at earlier gestational ages. These elevated pressures may be a trigger for the acquisition of a muscular adventitial coat, thereby enabling vasoreactivity in response to MH at an earlier gestational age compared to normal fetuses or compared to fetuses with HLHS and an open inter-atrial communication. With continued obstruction to pulmonary venous egress, we hypothesize that the pulmonary veins become “arterialized” over the course of gestation leading to marked hypoxemia and hypercarbia at birth. In the absence of elevated pressures within the pulmonary vasculature, fetuses with HLHS and an open inter-atrial communication may acquire a muscular adventitial coat at a similar gestational age as normal fetuses without HLHS.
In response to MH, the MCA PI increased, but did not meet statistical significance. A previous investigator proposed that the cerebrovasculature vasodilates in response to hypoxia32. If this explanation were true, one would expect the PI within the MCA to normalize in response to 10 minutes of MH, which raises the mixed venous oxygen content by approximately 10-15 torr. In fact, although the MCA PI increased with MH, it did not normalize, suggesting that the vasodilation of the cerebral vasculature may more related to flow than to hypoxemia.
Limitations
Our study is limited by the small number of HLHS fetuses with a restrictive inter-atrial communication within our study cohort. Consequently, we may have insufficient power to detect changes in our parameters with MH testing within our subgroup analysis. Similarly, we may be underpowered to detect a change in vasoreactivity over the course of gestation. Based upon the results of our MH testing, we defined a cutoff for lack of vasoreactivity as a change in PI of < 10% with MH. However, we did not confirm this finding in our normal control population. Finally, we did not invasively check to determine that MH testing raised the fetal oxygen content. As a result, we have failed to detect changes in our parameters with MH testing on account of inadequate oxygen delivery to the fetus.
Conclusions
Our study demonstrates that MH testing is a safe, useful clinical tool to assess the pulmonary vasculature in fetuses with HLHS. In response to MH, there was no change in either the MCA or UA PI. There was no increase in the degree of tricuspid regurgitation, although three different fetuses had a significant decrease in the degree of tricuspid regurgitation after the administration of MH. Qualitatively, there were no changes in right ventricular function in response to MH. The PI in the DA did increase in response to MH, likely reflecting increased flow into the pulmonary vascular bed and decreased flow across the ductus arteriosus. Importantly, no ductal constriction was observed with MH. In our study, MH was performed for approximately 30 minutes—10 minutes of MH and then 20 minutes for acquisition of images. Long-term MH therapy has been used safely in fetuses with IUGR to prolong pregnancy33, 34. Whether long-term MH therapy may be beneficial in fetuses with HLHS remains to be determined. We conclude that MH testing certainly has a role in identifying HLHS fetuses requiring urgent postnatal intervention on the inter-atrial septum. In addition, by providing a window to assess the pulmonary vasculature in the late second trimester fetus, MH testing may prove useful when considering a fetal intervention, such as a fetal atrial septoplasty, for those HLHS fetuses with a restrictive/intact atrial septum.
Infants with hypoplastic left heart syndrome (HLHS) and a restrictive or intact atrial septum have a particularly poor prognosis. Obstruction to left atrial egress leads to marked changes in the pulmonary vasculature, which may persist despite successful opening of the atrial septum after birth. A mechanism for evaluating the prenatal status of the pulmonary vasculature in the fetus with HLHS would be of great value as it could identify the fetus that could benefit from either prenatal intervention or immediate, urgent postnatal care. In this novel, prospective study, we sought to investigate the pulmonary vasculature in the fetus with HLHS by assessing for changes in the Doppler derived pulsatility index (PI), a surrogate measure of vascular impedance, within the branch pulmonary arteries in response to maternal hyperoxygenation (MH). In our HLHS cohort, MH led to a significant decrease in the PI within the branch pulmonary artery in fetuses with an open atrial septum (p<0.001); however, there no was significant change in the PI at any of the branch pulmonary artery sites in fetuses that required immediate intervention on the atrial septum at birth. Indeed, MH testing predicted the need for immediate intervention on the inter-atrial septum at birth with sensitivity 100% specificity 94%, positive predictive value 71%, and negative predictive value 100%. We conclude that MH testing accurately identifies HLHS fetuses requiring urgent postnatal intervention at birth and may be used to select candidates for fetal atrial septoplasty.
Funding Sources
Dr. Szwast was partially funded for this work by a NIH Training Grant, T32-HL007915.
Footnotes
Journal Subject Code: [31] Echocardiography; [41] Pediatric and congenital heart disease, including cardiovascular surgery
Conflict of Interests Disclosure: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Mahle WT, Spray TL, Wernovsky G, Gaynor JW, Clark BJ., III Survival after reconstructive surgery for hypoplastic left heart syndrome: A 15-year experience from a single institution. Circulation. 2000;102:III136–III141. doi: 10.1161/01.cir.102.suppl_3.iii-136. [DOI] [PubMed] [Google Scholar]
- 2.Khoshnood B, de VC, Vodovar V, Goujard J, Lhomme A, Bonnet D, Goffinet F. Trends in prenatal diagnosis, pregnancy termination, and perinatal mortality of newborns with congenital heart disease in France, 1983-2000: a population-based evaluation. Pediatrics. 2005;115:95–101. doi: 10.1542/peds.2004-0516. [DOI] [PubMed] [Google Scholar]
- 3.Michelfelder E, Gomez C, Border W, Gottliebson W, Franklin C. Predictive value of fetal pulmonary venous flow patterns in identifying the need for atrial septoplasty in the newborn with hypoplastic left ventricle. Circulation. 2005;112:2974–2979. doi: 10.1161/CIRCULATIONAHA.105.534180. [DOI] [PubMed] [Google Scholar]
- 4.Glatz JA, Tabbutt S, Gaynor JW, Rome JJ, Montenegro L, Spray TL, Rychik J. Hypoplastic left heart syndrome with atrial level restriction in the era of prenatal diagnosis. Ann Thorac Surg. 2007;84:1633–1638. doi: 10.1016/j.athoracsur.2007.06.061. [DOI] [PubMed] [Google Scholar]
- 5.Marshall AC, van d V, Tworetzky W, Gomez CA, Wilkins-Haug L, Benson CB, Jennings RW, Lock JE. Creation of an atrial septal defect in utero for fetuses with hypoplastic left heart syndrome and intact or highly restrictive atrial septum. Circulation. 2004;110:253–258. doi: 10.1161/01.CIR.0000135471.17922.17. [DOI] [PubMed] [Google Scholar]
- 6.Wallen LD, Perry SF, Alston JT, Maloney JE. Fetal lung growth. Influence of pulmonary arterial flow and surgery in sheep. Am J Respir Crit Care Med. 1994;149:1005–1011. doi: 10.1164/ajrccm.149.4.8143035. [DOI] [PubMed] [Google Scholar]
- 7.Wallen LD, Perry SF, Alston JT, Maloney JE. Morphometric study of the role of pulmonary arterial flow in fetal lung growth in sheep. Pediatr Res. 1990;27:122–127. doi: 10.1203/00006450-199002000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Rasanen J, Wood DC, Weiner S, Ludomirski A, Huhta JC. Role of the pulmonary circulation in the distribution of human fetal cardiac output during the second half of pregnancy. Circulation. 1996;94:1068–1073. doi: 10.1161/01.cir.94.5.1068. [DOI] [PubMed] [Google Scholar]
- 9.Rudolph AM, Heymann MA. Circulatory changes during growth in the fetal lamb. Circ Res. 1970;26:289–299. doi: 10.1161/01.res.26.3.289. [DOI] [PubMed] [Google Scholar]
- 10.Vida VL, Bacha EA, Larrazabal A, Gauvreau K, Thiagaragan R, Fynn-Thompson F, Pigula FA, Mayer JE, Jr., del Nido PJ, Tworetzky W, Lock JE, Marshall AC. Hypoplastic left heart syndrome with intact or highly restrictive atrial septum: surgical experience from a single center. Ann Thorac Surg. 2007;84:581–585. doi: 10.1016/j.athoracsur.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 11.Vlahos AP, Lock JE, McElhinney DB, van der Velde ME. Hypoplastic left heart syndrome with intact or highly restrictive atrial septum: outcome after neonatal transcatheter atrial septostomy. Circulation. 2004;109:2326–2330. doi: 10.1161/01.CIR.0000128690.35860.C5. [DOI] [PubMed] [Google Scholar]
- 12.Rychik J, Rome JJ, Collins MH, DeCampli WM, Spray TL. The hypoplastic left heart syndrome with intact atrial septum: atrial morphology, pulmonary vascular histopathology and outcome. J Am Coll Cardiol. 1999;34:554–560. doi: 10.1016/s0735-1097(99)00225-9. [DOI] [PubMed] [Google Scholar]
- 13.Haworth SG, Reid L. Quantitative structural study of pulmonary circulation in the newborn with aortic atresia, stenosis, or coarctation. Thorax. 1977;32:121–128. doi: 10.1136/thx.32.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Graziano JN, Heidelberger KP, Ensing GJ, Gomez CA, Ludomirsky A. The influence of a restrictive atrial septal defect on pulmonary vascular morphology in patients with hypoplastic left heart syndrome. Pediatr Cardiol. 2002;23:146–151. doi: 10.1007/s00246-001-0038-7. [DOI] [PubMed] [Google Scholar]
- 15.Rasanen J, Wood DC, Debbs RH, Cohen J, Weiner S, Huhta JC. Reactivity of the human fetal pulmonary circulation to maternal hyperoxygenation increases during the second half of pregnancy: a randomized study. Circulation. 1998;97:257–262. doi: 10.1161/01.cir.97.3.257. [DOI] [PubMed] [Google Scholar]
- 16.Broth RE, Wood DC, Rasanen J, Sabogal JC, Komwilaisak R, Weiner S, Berghella V. Prenatal prediction of lethal pulmonary hypoplasia: the hyperoxygenation test for pulmonary artery reactivity. Am J Obstet Gynecol. 2002;187:940–945. doi: 10.1067/mob.2002.127130. [DOI] [PubMed] [Google Scholar]
- 17.Rychik J, Ayres N, Cuneo B, Gotteiner N, Hornberger L, Spevak PJ, van d V. American Society of Echocardiography guidelines and standards for performance of the fetal echocardiogram. J Am Soc Echocardiogr. 2004;17:803–810. doi: 10.1016/j.echo.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Laudy JA. Doppler ultrasonography of the human fetal pulmonary circulation. Eur J Obstet Gynecol Reprod Biol. 2001;99:3–5. doi: 10.1016/s0301-2115(01)00368-2. [DOI] [PubMed] [Google Scholar]
- 19.Laudy JA, de Ridder MA, Wladimiroff JW. Human fetal pulmonary artery velocimetry: repeatability and normal values with emphasis on middle and distal pulmonary vessels. Ultrasound Obstet Gynecol. 2000;15:479–486. doi: 10.1046/j.1469-0705.2000.00134.x. [DOI] [PubMed] [Google Scholar]
- 20.Liang RI, Prapas N, Detti L, Cosmi E, Copel JA, Mari G. Assessment of blood flow velocity waveforms of the pulmonary circulation by multigate spectral Doppler scanning and traditional pulsed Doppler ultrasonography. J Ultrasound Med. 2002;21:31–37. doi: 10.7863/jum.2002.21.1.31. [DOI] [PubMed] [Google Scholar]
- 21.Sivan E, Rotstein Z, Lipitz S, Sevillia J, Achiron R. Segmentary fetal branch pulmonary artery blood flow velocimetry: in utero Doppler study. Ultrasound Obstet Gynecol. 2000;16:453–456. doi: 10.1046/j.1469-0705.2000.00268.x. [DOI] [PubMed] [Google Scholar]
- 22.Rasanen J, Huhta JC, Weiner S, Wood DC, Ludomirski A. Fetal branch pulmonary arterial vascular impedance during the second half of pregnancy. Am J Obstet Gynecol. 1996;174:1441–1449. doi: 10.1016/s0002-9378(96)70586-0. [DOI] [PubMed] [Google Scholar]
- 23.Dubin J, Wallerson DC, Cody RJ, Devereux RB. Comparative accuracy of Doppler echocardiographic methods for clinical stroke volume determination. Am Heart J. 1990;120:116–123. doi: 10.1016/0002-8703(90)90168-w. [DOI] [PubMed] [Google Scholar]
- 24.Tulzer G, Gudmundsson S, Sharkey AM, Wood DC, Cohen AW, Huhta JC. Doppler echocardiography of fetal ductus arteriosus constriction versus increased right ventricular output. J Am Coll Cardiol. 1991;18:532–536. doi: 10.1016/0735-1097(91)90611-c. [DOI] [PubMed] [Google Scholar]
- 25.Crowe DA, Allan LD. Patterns of pulmonary venous flow in the fetus with disease of the left heart. Cardiol Young. 2001;11:369–374. doi: 10.1017/s1047951101000464. [DOI] [PubMed] [Google Scholar]
- 26.Taketazu M, Barrea C, Smallhorn JF, Wilson GJ, Hornberger LK. Intrauterine pulmonary venous flow and restrictive foramen ovale in fetal hypoplastic left heart syndrome. J Am Coll Cardiol. 2004;43:1902–1907. doi: 10.1016/j.jacc.2004.01.033. [DOI] [PubMed] [Google Scholar]
- 27.Rychik J, Gullquist SD, Jacobs ML, Norwood WI. Doppler echocardiographic analysis of flow in the ductus arteriosus of infants with hypoplastic left heart syndrome: relationship of flow patterns to systemic oxygenation and size of interatrial communication. J Am Soc Echocardiogr. 1996;9:166–173. doi: 10.1016/s0894-7317(96)90024-3. [DOI] [PubMed] [Google Scholar]
- 28.Better DJ, Apfel HD, Zidere V, Allan LD. Pattern of pulmonary venous blood flow in the hypoplastic left heart syndrome in the fetus. Heart. 1999;81:646–649. doi: 10.1136/hrt.81.6.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Szwast A, Tian Z, McCann M, Donaghue D, Rychik J. Right ventricular performance in the fetus with hypoplastic left heart syndrome. Ann Thorac Surg. 2009;87:1214–1219. doi: 10.1016/j.athoracsur.2008.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wagenvoort C, EDWARDS JE. Pulmonary Arterial Tree in Aortic Atresia with Intact Ventricular Septum. Laboratory Investigation. 1961;10:924–&. [Google Scholar]
- 31.Maeda K, Yamaki S, Kado H, Asou T, Murakami A, Takamoto S. Hypoplasia of the small pulmonary arteries in hypoplastic left heart syndrome with restrictive atrial septal defect. Circulation. 2004;110:II139–II146. doi: 10.1161/01.CIR.0000138223.74524.4e. [DOI] [PubMed] [Google Scholar]
- 32.Donofrio MT, Bremer YA, Schieken RM, Gennings C, Morton LD, Eidem BW, Cetta F, Falkensammer CB, Huhta JC, Kleinman CS. Autoregulation of cerebral blood flow in fetuses with congenital heart disease: the brain sparing effect. Pediatr Cardiol. 2003;24:436–443. doi: 10.1007/s00246-002-0404-0. [DOI] [PubMed] [Google Scholar]
- 33.Battaglia C, Artini PG, D'Ambrogio G, Galli PA, Segre A, Genazzani AR. Maternal hyperoxygenation in the treatment of intrauterine growth retardation. Am J Obstet Gynecol. 1992;167:430–435. doi: 10.1016/s0002-9378(11)91424-0. [DOI] [PubMed] [Google Scholar]
- 34.Nicolaides KH, Campbell S, Bradley RJ, Bilardo CM, Soothill PW, Gibb D. Maternal oxygen therapy for intrauterine growth retardation. Lancet. 1987;1:942–945. doi: 10.1016/s0140-6736(87)90292-3. [DOI] [PubMed] [Google Scholar]


