Abstract
Sporotrichosis is a subacute or chronic infection caused by Sporothrix schenckii. It is a primary cutaneous infection and it has different clinical forms: disseminated by lymphatic vessels (75%), localised cutaneous form (20%), disseminated cutaneous and extracuteus rarely. The systemic disseminated sporotrichosis is considered a severe opportunistic infection. The best diagnostic test is the culture. The authors report a case of a 36-year-old man, originally from Puebla, Mexico, with a diagnosis of disseminated sporotrichosis. Differential diagnosis with other pathologies includes leishmaniasis, chromoblastomycosis, tuberculosis verrucose and lymphangitis. The development of unusual presentations in immunocompromised patients has been reported.
Background
Sporotrichosis is a subacute or chronic infection caused by Sporothrix schenckii; it is a cosmopolitan disease, showing high incidence levels in Brazil, Central America, Colombia and Mexico.1 It affects both sexes and all ages, with prevalence highest among farmers, gardeners, florists and carpenters between 16 and 30 years of age.2 It is a primary skin infection that spreads mainly through the lymph (75%); there is also a fixed localised skin form (20%) and, in a lesser proportion, disseminated and extracutaneous varieties.3 The extent of the disease varies according to immune status; it is believed that T cell-mediated immunity limits its extent.4 Systemic disseminated sporotrichosis is considered a serious opportunistic infection that affects the internal organs and can produce fungemia,3 accompanied by fever, pain, malaise and weight loss.3
Culture is the diagnostic method of choice; pigment production is considered a virulence factor; in the microscopic study, thin, septate and branching hyphae are looked for with pyriform conidia of the radulospore or sympodial type. The intradermal reaction test with sporotrichin is the fastest method in the diagnosis of sporotrichosis.3 For its treatment, potassium iodide is used changing to itraconazole, fluconazole, terbinafine or amphotericin B for resistant or disseminated forms.3
Case presentation
A 36-year-old male patient, originally from Puebla, Mexico, presented. A farmer from age 5 years, his condition began at age 20 with a papular lesion on the dorsum of the left foot, which ulcerated on several occasions. Two months later he was treated with unspecified systemic and topical antifungal agents. The treatment was suspended after 3 months, the lesions grew and new ones appeared in the left thigh. From 1995 to 1997 the patient applied homemade remedies. Three years after the first symptoms appeared he attended the Hospital General de México where he was diagnosed.
Investigations
Direct examination and staining (Wright and Giemsa) was negative. Intradermal reaction (mycelial sporotrichin dilution 1:200) was positive with induration and erythema (8×8 cm). Cultures were done in Sabouraud dextrose agar (SDA) and SDA supplemented with antibiotics. An obtained isolated wet membranous colony, brown with a beige halo, was identified by morphology as S schenckii. The strain was studied by molecular biology methods corroborating the identification as S schenckii (sensu estricto).
Treatment
The infection was treated with itraconazole for 6 months with good results, but the patient discontinued the treatment and the lesions were reactivated and spread to his right leg and thigh. He did not receive any treatment and 2 years afterwards lesions began to appear on the buttocks. The patient took potassium iodide irregularly for 2 years; lesions appeared on the face, wrists, arms and abdomen.
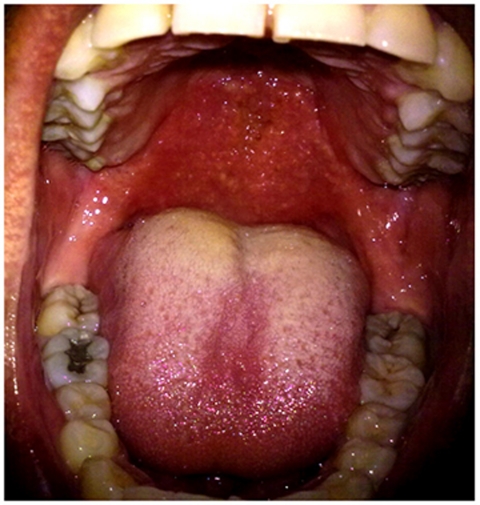
In the past 9 months the patient lost 11 kg, presented pharyngeal pain, hematic rhinorrhoea, fever and dysphagia. Physical examination made evident generalised dermatosis with nodular lesions, ulcers, gums and scabs on face, chest, legs and buttocks (figures 1 and 2); he showed retractile scar tissue in the extremities (figure 3)and retropharyngeal haematic yellow discharge was evident in the oral cavity as well as mouth breathing, nasal speech, oedematous, erythematous and granulose (cobblestone appearance) mucosa both on the palate and pharynx (figure 4).
Figure 1.
Lesions in the right thigh.
Figure 2.
Lesions in the right hand.
Figure 3.
Multiple lesions in the back, buttocks and thighs.
Figure 4.
Lesions in the pharynx.
The patient was admitted to the dermatology department at the Hospital General de México and was treated with 0.5 mg/kg/day amphotericin B to a total accumulated dose (TAD) of 1500 mg. The lesions in the oropharyngeal mucosa disappeared and 60% of the skin lesions healed (figure 5): 90% with a 900 mg TAD and 98% with a 1300 mg TAD. A total of 400 mg/day of itraconazole were added. At 1500 mg TAD, amphotericin B treatment was discontinued and all the lesions healed except three (wrist and left forearm). The patient was discharged and he continued with itraconazole (figures 6, 7 and 8).
Figure 5.
Pharynx after treatment.
Figure 6.
Residual lesions in the forehead.
Figure 7.
Multiple scars.
Figure 8.
Old lesions in the left leg and buttock.
Discussion
Sporotrichosis is considered an occupational disease (farmers, gardeners, florists and carpenters).2 The disseminated and extracutaneous forms are rare; in a series of 304 cases in Brazil, only 4 corresponded to this form.5 6 Other publications reported similar percentages ranging from 0.5–9%.7 8 Due to the atypical and complex characteristics of this form, a differential diagnosis should be made in relation to other diseases such as leishmaniasis, chromoblastomycosis, tuberculosis verrucosa and lymphangitis, among others.9 The development of unusual presentations has been reported in immunocompromised patients (both clinical and histological), which can delay diagnosis for months. Diabetes, HIV, chronic obstructive pulmonary disease, alcoholism and chronic use of steroids appear to be factors in the development of extracutaneous or disseminated forms according to reports of alcoholic and cirrhotic patients.5 7 9 Other studies report infection of the airway with odynophagia and dysphonia;10 a presentation that is rarely seen in patients with or without skin lesions, but not so in severe immunocompromised patients or those using inhaled corticosteroids.9 11
Our patient presents factors for infection such as living in an endemic area (where he probably acquired the fungus) and working as a farmer in such an area for 20 years. The disease progression was unusual; he developed the disseminated form although no factor related to immunosuppression was documented (he is a non-alcoholic, does not use steroids, HIV negative, etc) and immune function tests were normal. So it was an atypical presentation with cutaneous and mucosal dissemination.
The evolution of the disease with treatment was good; lesions showed almost a 100% remission with the 1500 mg TAD of amphotericin B. Itraconazole was added in pulses (7–21 days rest) for residual lesions and in order to avoid symptom reappearance. This patient represented a complex case, which was diagnosed several years ago. We believe that the spread of the infection was due to the erratic behaviour of the patient in relation to his treatment. Probably the initial treatment of the disease should have been more aggressive and carried out for a longer period of time.
Learning points.
-
▶
This is a very rare presentation form of this mycosis.
-
▶
There are so many differential diagnosis for this disease.
-
▶
The diagnosis is not easy and we had to follow a guide to reach the right diagnosis.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Chávez FI, Cabada BJ, Uribe JE, et al. Esporotricosis sistémica: comunicación de un caso y revisión bibliográfica. Med Int Mex 2007;23:87–90 [Google Scholar]
- 2.Arenas R. Esporotricosis. Una micosis cosmopolita. Mas Dermatol 2010;10:22–5 [Google Scholar]
- 3.Rodríguez GH, Magaña RM, Juárez L, et al. Esporotricosis cutánea diseminada: comunicación de un caso. Dermatología Rev Mex 2008;52:228–30 [Google Scholar]
- 4.Fernandez K, Helal NE, Brito M, et al. Detrimental role of endogenous nitric oxide in host defence against Sporothrix schenckii. Immunology 2008;123:469–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michel da Rosa A, Scroferneker M, Vettoraro R, et al. Epidemiology of sporotricosis: A study of 304 cases in Brazil. J Am Acad Dermatol 2005;52:451–9 [DOI] [PubMed] [Google Scholar]
- 6.Laniado-Laborín R. Coccidioidomycosis and other endemic mycoses in Mexico. Rev Iberoam Micol 2007;24:249–58 [DOI] [PubMed] [Google Scholar]
- 7.Itoh M, Okamoto S, Kariya H. Survey of 200 cases of sporotrichosis. Dermatologica 1986;172:209–13 [DOI] [PubMed] [Google Scholar]
- 8.Pappas PG, Tellez I, Deep AE, et al. Sporotrichosis in Peru: description of an area of hyperendemicity. Clin Infect Dis 2000;30:65–70 [DOI] [PubMed] [Google Scholar]
- 9.Fonseca-Reyes S, López Maldonado FJ, Miranda-Ackerman RC, et al. Extracutaneous sporotrichosis in a patient with liver cirrhosis. Rev Iberoam Micol 2007;24:41–3 [DOI] [PubMed] [Google Scholar]
- 10.Madrid H, Cano J, Gené J, et al. Sporothrix globosa, a pathogenic fungus with widespread geographical distribution. Rev Iberoam Micol 2009;26:218–22 [DOI] [PubMed] [Google Scholar]
- 11.Orofino CR, Celso MK, Damasco P, et al. Infectious arthritis s the single manifestation of sporotrichosis: serology from serum and synovial fluid samples as an aid to diagnosis. Rev Iberoam Micol 2008;25:54–6 [DOI] [PubMed] [Google Scholar]