Abstract
Goal: To study the interaction of obesity and age in patients with multiple spine surgeries.
Methods: Data on the body mass index (BMI) of 956 patients were collected and classified into four groups: non-obese (BMI <30 kg/m2), obese-class I (BMI ≥30 kg/m2), obese-class II (BMI ≥35 kg/m2) and obese-class III (BMI ≥40 kg/m2). Patients' age was categorized into the following age groups: ≤40, 41–65 and ≥66. T-test and Chi-square test were applied using SPSS v16.
Results: In lumbar patients aged ≥66 years with previous spine surgery, the average number of previous spine surgeries significantly increased with increasing obesity from 1.4 in nonobese patients to 1.7, 2.5 and 3.5 in obese class I, II and III patients.
In lumbar decompression and fusion patients aged ≥66 years with previous spine surgery, the average number of previous spine surgeries signifi-cantly increased with increasing obesity from 1.7 in nonobese patients to 1.6, 2.0 and 3.5 in obese class I, II and III patients. A similar trend was noted in lumbar microdiskectomy patients aged ≥66 years but it was statistically nonsignificant due probably to small numbers.
Conclusion: Obesity is associated with an increased number of previous spine surgeries in patients over 65 years of age undergoing lumbar surgery.
Keywords: multiple spine surgery, age, obesity
Abstract
Ziel: Die Untersuchung der Beziehung zwischen Alter/Adipositas und mehrfachen Wirbelsäulenoperationen.
Methode: 956 Patienten wurden auf der Grundlage des Körpergewichtes (BMI) und des Lebensalters in vier Gruppen und Altersklassen eingeteilt: normalgewichtige Patienten (BMI <30 kg/m2); Adipositas-Gruppe I (BMI ≥30 kg/m2); Adipositas-Gruppe II (BMI ≥35 kg/m2); Adipositas-Gruppe III (BMI ≥40 kg/m2). Die untersuchten Altersklassen waren: ≤40 Jahre; 41–65 Jahre; ≥66 Jahre. Die Daten wurden mit t-Test und Chiquadrat-Test unter Anwendung des SPSS V 16 Programms ausgewertet.
Ergebnis: Bei Patienten im Alter von ≥66 Jahren, die an der Lendenwirbelsäule operiert werden sollten, stieg die Zahl der vorausgegangenen Wirbelsäulenoperationen signifikant mit zunehmender Adipositas von 1,4 bei normalgewichtigen Patienten auf 1,7, 2,5 und 3,5 in den Adipositas-Gruppen I bis III an.
Bei lumbalen Dekompressionen und Fusionen in Patienten der gleichen Altersgruppe stieg die Zahl der vorausgegangenen Operationen mit zunehmender Adipositas von 1,7 bei normalgewichtigen Patienten auf 1,6, 2,0 bzw. 3,5 in den Adipositas-Gruppen I bis III an. Ein ähnlicher Trend wurde bei Patienten (Alter ≥66 Jahre) mit lumbalen Mikrodissektionen beobachtet, die Unterschiede waren wahrscheinlich aufgrund der kleinen Fallzahlen statistisch nicht signifikant.
Schlussfolgerung: Adipositas ist bei älteren Patienten (über 65 Jahre), die sich einer Lumbalwirbelsäulenoperation unterziehen mussten, mit einer erhöhten Zahl vorausgegangener Eingriffe an der Wirbelsäule korreliert.
Introduction
Spine surgery is an important therapeutic modality for intractable back pain caused by evident abnormalities on vertebral column imaging. Surgical intervention on the spine is not the initial treatment for back pain and usually is reserved for patients who exhaust conservative methods of treatment starting from over-the-counter analgesics to nonsteroidal anti-inflammatory drugs to physiotherapy to nerve blocks without achieving a satisfying level of pain alleviation. Despite this, the number of spine surgeries nowadays is steadily increasing. Lumbar disc excisions account for most of spine surgical operations, while the remaining one-quarter represents spinal fusions and other procedures [1].
The rate of spine surgery in the United States is now at least 40% higher than in any other country and is more than five times the numbers in England and Scotland [2]. This seems to be related to differences in the culture and practice guidelines in those countries with some connection to the aging of the population and the obesity epidemic in our country [3]. In light of this, we aimed to study history of spine surgery in spine surgery candidates with regard to age and obesity factors.
Methods
The medical charts of 956 spine surgery candidates (45.9% males and 54.1% females) were retrospectively reviewed and the number of previous spine surgeries (PSS) prior to the index surgery was determined from the history of each patient. Patients were operated between 2005 and 2008 in a tertiary care center in Central Georgia. The index surgery was lumbar microdiskectomy (LMD), anterior cervical decompression and fusion (ACDF) or lumbar decompression and fusion (LDF). Patients were categorized as cervical (ACDF) or lumbar (LMD or LDF), de novo (no PSS) or recurrent (with a history of PSS).
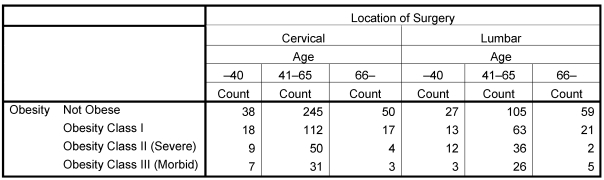
Data on the body mass index (BMI) were collected and patients were categorized into four groups: non-obese (BMI <30 kg/m2), obese-class I (BMI ≥30 kg/m2), obese-class II (BMI ≥35 kg/m2) and obese-class III (BMI ≥40 kg/m2). Age was categorized as ≤40, 41–65 and ≥66. T-test was used to compare scale variables (averages) while Chi-square test was used to compare categorical variables (percentages) with the help of the SPSS v16. Table 1 (Tab. 1) shows the distribution of patients in the study cohort per age, obesity and location of surgery.
Table 1. Distribution of patients per age, obesity and location of spine surgery.
Results
Prevalence of obesity in age groups
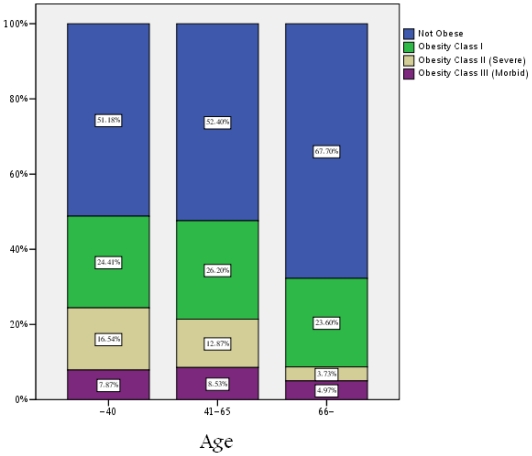
Over half of the patients (54.8%) were under the obesity threshold, 25.5% were obese-class I, 11.8% obese-class II and 7.8% obese-class III. Obesity was least prevalent in the oldest age group with 32.3% compared to 47.6% and 48.8% in the younger and youngest age groups (P<.01, Figure 1 (Fig. 1)). The percentage of patients with severe (3.7% vs. 12.9% and 16.5%) and morbid obesity (5% vs. 8.5% and 7.9%) in the oldest age group was the least compared with other age groups.
Figure 1. Prevalence of obesity per age group in spine surgery patients.
Prevalence of recurrent patients in age-obesity groups
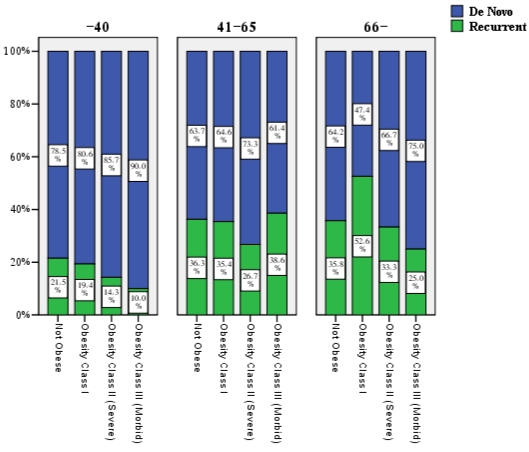
No significant differences in the percentage of recurrent patients among age-obesity groups were recorded. The highest percentage of recurrent patients (52.6%) was noted in the >65 years obesity class I group (P>.05, Figure 2 (Fig. 2)).
Figure 2. Prevalence of recurrent patients per age and obesity.
Differences in number of previous spine surgeries between age-obesity groups
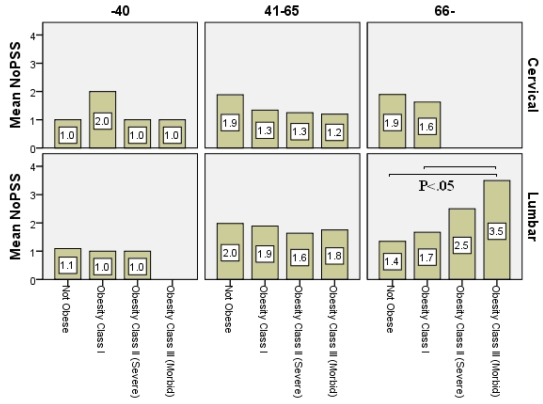
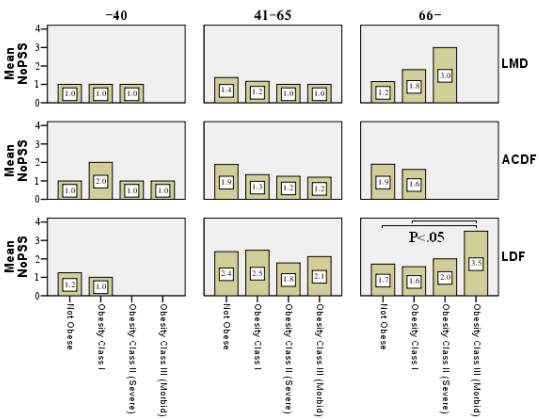
An increasing trend in the average number of previous spine surgeries was noticed in recurrent older patients undergoing lumbar surgery. In lumbar patients aged ≥66 age years with previous spine surgery (recurrent), the average number of previous spine surgeries significantly increased with increasing obesity from 1.4 in nonobese patients to 1.7, 2.5 and 3.5 in obese class I, II and III patients (Figure 3 (Fig. 3)).
Figure 3. The average number of previous spine surgeries (NoPSS) in recurrent patients (i.e. excluding those with 0 PSS) crossgraphed by age, surgery location and obesity groups.
Dividing the lumbar group per index surgery to LMD and LDF patients the trends were preserved. In LDFpatients aged ≥66 years with previous spine surgery (recurrent), the average number of previous spine surgeries significantly increased with increasing obesity from 1.7 in nonobese patients to 1.6, 2.0 and 3.5 in obese class I, II and III patients (Figure 4 (Fig. 4)). A similar trend was evident in LMD ≥66 years patients as well but it was statistically insignificant probably due to small numbers.
Figure 4. The average number of previous spine surgeries (NoPSS) in recurrent patients crossgraphed by age, surgery type and obesity groups.
Discussion
According to the American Obesity Association, 64.5% of adult Americans are considered overweight or obese [4]. We investigated obesity as an age-related factor that might have a causal relationship with degenerative spine disease. The paper addressed the question whether obese patients admitted for a spinal procedure had more previous spinal operations than nonobese patients. For the whole cohort this was denied as the percentage of recurrent patients was not statistically different between the age-obesity groups. A significant relationship between obesity and the number of previous operations was however recorded in older patients undergoing spine surgery despite the fact that obesity rate and severity decreases in the oldest age-group. This occurs because longer life span offers more opportunities to accumulate surgical spinal procedures in obese patients.
We used the number of previous spine surgeries instead of reoperation rate as a marker of multiple surgical interventions. Our finding represents an opposite reflection of the discovery of Hue et al., 1997, that age <65 is a risk factor for reoperation after spine surgery [5]. Our study specifically shows a significant relationship between the number of previous operations and obese classes in the age group >65. This finding may be an indirect argument for the hypothesis that obesity is a risk factor for spinal degeneration and multiple spine surgery. When excess weight is carried, the spine is forced to assimilate the burden, which may lead to structural compromise that accelerates degenerative disease especially in the lower (lumbar) section of the spine. Degenerative disc disease in the cervical spine is much less common than disc degeneration in the lumbar spine because the neck carries less weight and is generally subjected to far less torque and force. The medical literature seems to be more on the side of a positive relationship between obesity and degenerative spine disease [6], [7], [8]. Obesity has recently been shown to be “a strong and independent predictor” of recurrent herniation of nucleus pulposus and reoperation after lumbar microdiscectomy [9].
Some surgeons hesitate about operating on older obese patients because of the reportedly increased risk of perioperative complications [10], [11]. This has been contradicted in other studies [12], [13], [14]. Some recommend a less invasive spine approach in obese patients [15]. Nevertheless, with preoperative screening a high body mass index should not preclude access to surgery if proper indications exist [6], [15].
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Frymoyer JW. Are we performing too much spinal surgery? Iowa Orthop J. 1989;9:32–36. [Google Scholar]
- 2.Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine (Phila Pa 1976) 1994;19(11):1201–1206. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 3.Walid MS, Sanoufa M, Robinson JS. The effect of age and body mass index on cost of spinal surgery. J Clin Neurosci. 2011 doi: 10.1016/j.jocn.2010.07.132. Available from: http://dx.doi.org/10.1016/j.jocn.2010.07.132. [DOI] [PubMed] [Google Scholar]
- 4.American Obesity Association. AOA Fact Sheets. 2002. Available from: http://www.obesity.org/resources-for/fact-sheets.htm.
- 5.Hu RW, Jaglal S, Axcell T, Anderson G. A population-based study of reoperations after back surgery. Spine (Phila Pa 1976) 1997;22(19):2265–2270. doi: 10.1097/00007632-199710010-00013. [DOI] [PubMed] [Google Scholar]
- 6.Andreshak TG, An HS, Hall J, Stein B. Lumbar spine surgery in the obese patient. J Spinal Disord. 1997;10(5):376–379. doi: 10.1097/00002517-199710000-00003. Available from: http://dx.doi.org/10.1097/00002517-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Silveri CP, Spinasanta S. Back Pain and Obesity Connection to Back Pain and Development of Obesity. Montclair, NJ: SpineUniverse; ©1999-2011. Available from: http://www.spineuniverse.com/conditions/back-pain/back-pain-obesity. [Google Scholar]
- 8.Mirtz TA, Greene L. Is obesity a risk factor for low back pain? An example of using the evidence to answer a clinical question. Chiropr Osteopat. 2005;13(1):2. doi: 10.1186/1746-1340-13-2. Available from: http://dx.doi.org/10.1186/1746-1340-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meredith DS, Huang RC, Nguyen J, Lyman S. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J. 2010;10(7):575–580. doi: 10.1016/j.spinee.2010.02.021. Available from: http://dx.doi.org/10.1016/j.spinee.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 10.Patel N, Bradley B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro A, Harrop J, Sharan A, Ratliff JK. Obesity and spine surgery: relation to perioperative Complications. J Neurosurg Spine. 2007;6(4):291–297. doi: 10.3171/spi.2007.6.4.1. Available from: http://dx.doi.org/10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 11.Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976) 2009;34(5):495–500. doi: 10.1097/BRS.0b013e318198c5f2. Available from: http://dx.doi.org/10.1097/BRS.0b013e318198c5f2. [DOI] [PubMed] [Google Scholar]
- 12.Yadla S, Malone J, Campbell PG, Maltenfort MG, Harrop JS, Sharan AD, Vaccaro AR, Ratliff JK. Obesity and spine surgery: reassessment based on a prospective evaluation of perioperative complications in elective degenerative thoracolumbar procedures. Spine J. 2010;10(7):581–587. doi: 10.1016/j.spinee.2010.03.001. Available from: http://dx.doi.org/10.1016/j.spinee.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Watanabe M, Sakai D, Matsuyama D, Yamamoto Y, Sato M, Mochida J. Risk factors for surgical site infection following spine surgery: efficacy of intraoperative saline irrigation. J Neurosurg Spine. 2010;12(5):540–546. doi: 10.3171/2009.11.SPINE09308. Available from: http://dx.doi.org/10.3171/2009.11.SPINE09308. [DOI] [PubMed] [Google Scholar]
- 14.Park P, Upadhyaya C, Garton HJ, Foley KT. The impact of minimally invasive spine surgery on perioperative complications in overweight or obese patients. Neurosurgery. 2008;62(3):693–699. doi: 10.1227/01.neu.0000317318.33365.f1. Available from: http://dx.doi.org/10.1227/01.neu.0000317318.33365.f1. [DOI] [PubMed] [Google Scholar]
- 15.Singh AK, Ramappa M, Bhatia CK, Krishna M. Less invasive posterior lumbar interbody fusion and obesity: clinical outcomes and return to work. Spine (Phila Pa 1976) 2010;35(24):2116–2120. doi: 10.1097/BRS.0b013e3181cf0980. Available from: http://dx.doi.org/10.1097/BRS.0b013e3181cf0980. [DOI] [PubMed] [Google Scholar]