Abstract
The objective of this study was to identify longitudinal patterns of injection drug use over 20 years in the AIDS Linked to the Intravenous Experience (ALIVE) Study, a community-based cohort of injection drug users (IDUs) in Baltimore, Maryland, with a focus on injection cessation. Starting in 1988, persons over 18 years of age with a history of injection drug use were recruited into the study. Participants provided information on their injection drug use semiannually through 2008. The analysis was restricted to 1,716 IDUs with at least 8 study visits. Finite mixture models were used to identify trajectories and predictors of injection patterns over time. The mean age of participants was 35 years; 75% were male, and 95% were African-American. Five distinct patterns were identified: 2 usage patterns (32% engaged in persistent injection and 16% had frequent relapse) and 3 cessation patterns (early cessation (19%), delayed cessation (16%), and late cessation (18%)). A history of drug treatment, no recent use of multiple substances, and less frequent injection distinguished the early cessation group from the other groups. This study demonstrated multiple trajectories of drug injection behaviors, with a substantial proportion of IDUs stopping injection over extended time frames. For maximum effectiveness, public health programs for IDUs should be long-term, comprehensive, and targeted toward individual patterns of use.
Keywords: behavior, HIV, longitudinal studies, substance abuse, intravenous
Injection drug use is associated with substantial mortality and morbidity, including infection with bloodborne pathogens, serious bacterial infections, and overdose. This public health burden highlights the need for a better understanding of the natural history of injection drug use in order to intervene most effectively. However, few longitudinal studies have followed heroin and/or cocaine users over long time periods to characterize natural history (1–6), with even fewer having focused explicitly on injectors (7–10). Most existing studies have focused on treatment-based samples, but the large majority of injection drug users (IDUs) do not seek formal treatment (2, 11), and a substantial number of IDUs quit using drugs without seeking treatment (12–14).
Of particular importance to public health efforts is the characterization of injection cessation and predictors among IDUs. However, previous research on injection cessation has focused primarily on short periods of cessation (e.g., 6 months to 1 year). Short-term behavior changes among IDUs are not always predictive of longer-term recovery. In fact, while the majority of studies have demonstrated that a significant proportion of IDUs reported ceasing injection for short periods of time (15–19), as many as 50%–75% of those who stopped had at least 1 subsequent relapse (19, 20), often within 1 year of cessation (17).
To better understand long-term injection cessation, it is critical to consider the full spectrum of injection behaviors over long time spans. In previous research from a community-based cohort study of IDUs in Baltimore City—the AIDS Linked to the Intravenous Experience (ALIVE) Study—Galai et al. (19) described patterns of injection drug use over 10 years based on the number of transitions into and out of injection. However, cessation was defined as no injection for at least 6 months and thus included both injectors who had stopped using for short periods of time and those who had stopped longer-term. In the current study, we characterized longitudinal trajectories of injection drug use in this same population over a period of 20 years, with an emphasis on distinguishing short-term cessation from long-term cessation. Baseline sociodemographic and behavioral predictors of long-term injection cessation were also determined.
MATERIALS AND METHODS
Study population
The ALIVE Study is a prospective community-based cohort study of IDUs in Baltimore, Maryland, and has been described previously (21). Briefly, 2,946 IDUs were recruited through community outreach in 1988–1989. An additional 682 participants were recruited during 2 additional recruitment periods in 1994–1995 and 1998. Persons were eligible for enrollment if they were aged 18 years or older, were free of acquired immunodeficiency syndrome, and had a history of injection drug use at baseline. In baseline and semiannual follow-up interviews, researchers collected information on sociodemographic characteristics, drug injection behaviors, medical history, human immunodeficiency virus (HIV) risk behaviors (sexual and drug-related), and drug treatment. The institutional review board at the Johns Hopkins Bloomberg School of Public Health reviewed and approved the study procedures, and all participants provided written informed consent.
Since the goal was to characterize long-term injection patterns among active drug injectors, participants were included if they reported injecting drugs at the first follow-up visit, had at least 1 additional visit at which they reported injecting, and participated in at least 6 subsequent follow-up visits (a minimum of 8 study visits). Participants who did not report injecting drugs at their first study visit (n = 400) were older and had a shorter average duration of follow-up, fewer visits of reporting injection, and fewer years of injecting at baseline than those who did report injecting at their first study visit. Those who did not report injection at an additional visit over the course of follow-up (n = 183) had shorter average follow-up times and fewer years of injecting at baseline than those with an additional injection visit. Finally, participants without 6 study visits following their second injection visit (n = 619) had fewer years of reporting injecting at baseline, had fewer visits at which they reported injecting, and were more likely to have died than those who did have 6 additional visits.
Statistical analysis
We used descriptive statistics to examine the proportion of the sample reporting injection drug use by year. To determine heterogeneous patterns of injection being masked in the aggregate, we employed semiparametric latent class growth modeling or finite mixture models, an extension of conventional maximum likelihood models (22). The goal of such methods is to identify membership in latent groups defined by distinctive longitudinal patterns (23). While the number of patterns can be hypothesized a priori, one aim of this method is to identify the number of latent groups in a sample. On the basis of prior research (19, 24), we hypothesized a priori that there would be a minimum of 3 patterns: persistent injection, relapse, and cessation. However, to allow for the possibility of additional patterns emerging, we examined up to 6 patterns.
The outcome in this analysis was self-reported injection of heroin, cocaine, and/or “speedball” (mixed heroin and cocaine) during the prior 6 months. The time scale was the time from study enrollment to censoring. Participants were censored either at the time of death, when they were lost to follow-up, or administratively at the end of 2008. To define the number of groups, we fitted an iterative series of models, varying the number of groups up to 6. Results were compared using 3 criteria: the Bayesian Information Criterion, the average posterior probabilities of groups, and the usefulness of the number of classes in practice (25). We chose the Bayesian Information Criterion because of its superior qualities for model selection, although use of other metrics is possible (26). We considered the usefulness of the number of groups by examining the shapes of the trajectories for similarity, the number of persons in each class, and the number of estimated parameters. Posterior probabilities for group membership were calculated, and participants were assigned to the group with the highest probability of membership. Backward selection of the parameters representing time (e.g., linear, quadratic, cubic) was used to determine trajectory shapes, and parameters were removed on the basis of statistical significance (P ≤ 0.05).
After the number and shapes of the trajectories had been identified, baseline sociodemographic and behavioral characteristics were included as time-fixed covariates. Predictors were selected on the basis of previous research on injection cessation. Behavioral predictors that were not statistically significant (P ≤ 0.05) in univariate models were excluded; however, all sociodemographic characteristics were retained in the final model. Injection behaviors were carried forward for gaps in follow-up that were short in duration. Data for gaps longer than 2 missed visits (<3% of visits) were not imputed and were considered missing for the purposes of this analysis. All analyses were conducted in SAS, version 9.1 (SAS Institute Inc., Cary, North Carolina).
RESULTS
Description of study population
A total of 1,716 persons with 38,718 observations were included. The median age of participants at baseline was 35 years; 75% were male, and 95% African-American (Table 1). The median number of follow-up visits was 20 (representing approximately 10 years), with a range of 8–42. The majority of participants had never married (66%) and had not completed high school (57%). At baseline, 29% were infected with HIV. The median age at injection initiation was 19 years, and participants had a median of 14 years of injection at study enrollment. Over half reported a history of ever receiving drug treatment at baseline. In the 6 months prior to the first follow-up visit, three-quarters of IDUs reported injecting both heroin and cocaine, and nearly half were injecting daily or more frequently. Approximately 20% reported having used crack, and a similar percentage used alcohol daily. Methadone maintenance therapy was reported by 10%. Over 40% reported having had sex with an IDU partner in the previous 6 months.
Table 1.
Baseline Demographic Characteristics and Behavioral Factors in the Prior 6 Months Among 1,716 Injection Drug Users in the ALIVE Study, Baltimore, Maryland, 1988–2008
| % | Median (IQR) or Mean (SD) | |
| Female sex | 25 | |
| Age, years | 35 (30–39) | |
| African-American race | 95 | |
| Marital status | ||
| Never married | 66 | |
| Married | 5 | |
| Widowed, divorced, or separated | 29 | |
| Educational attainment | ||
| Less than high school | 57 | |
| High school diploma | 31 | |
| More than high school | 13 | |
| Lived with children under age 18 years at baseline | 43 | |
| Currently employed at baseline | 19 | |
| Ever having received drug treatment at baseline | 59 | |
| Age at injection initiation, years | 19 (16–24) | |
| Duration of injection at baseline, years | 14 (7–20) | |
| HIV-infected at baseline | 29 | |
| No. of follow-up visits | 20 (13–28) | |
| Type of drug injected | ||
| Heroin only | 10 | |
| Cocaine only | 14 | |
| Mixed heroin and cocaine use | 77 | |
| Frequency of injection | ||
| Less than daily | 50 | |
| Daily or more often | 50 | |
| Frequency of alcohol use | ||
| None | 21 | |
| Less than daily | 58 | |
| Daily | 21 | |
| Methadone maintenance therapy | 10 | |
| Detoxification | 15 | |
| Sex with an IDU partner | 45 | |
| Sex with an anonymous partner | 19 | |
| No. of sex partners | 3 (8.5)a | |
| Incarcerated for ≥7 days | 16 | |
| Noninjecting drug use | ||
| Smoked marijuana | 48 | |
| Snorted cocaine | 20 | |
| Snorted heroin | 15 | |
| Smoked crack | 24 | |
| Smoked heroin | 1 |
Abbreviations: ALIVE, AIDS Linked to the Intravenous Experience; HIV, human immunodeficiency virus; IDU, injection drug user; IQR, interquartile range; SD, standard deviation.
Mean value (and SD).
Trajectories of injection drug use
The final model included 5 groups: early cessation, delayed cessation, late cessation, frequent relapse, and persistent injection. While the 6-class solution had the smallest Bayesian Information Criterion (i.e., the largest negative value), it was less useful in practice than the 5-class model, as it had multiple repetitive trajectory shapes requiring additional estimated parameters. The 5-group model had average posterior probabilities of group membership ranging from 0.81 to 0.93 across groups (Table 2), indicating good classification quality (25).
Table 2.
Average Posterior Probabilities and Prevalences of Injection Drug Use Group Membership Based on a 5-Group Solution Among 1,716 Injection Drug Users in the ALIVE Study, Baltimore, Maryland, 1988–2008a
| Injection Drug Use Group | Injection Drug Use Group |
Prevalence, % | ||||
| Early Cessation | Delayed Cessation | Late Cessation | Frequent Relapse | Persistent Injection | ||
| Early cessation | 0.93 | 0.04 | 0.03 | 0.00 | 0.00 | 18.7 |
| Delayed cessation | 0.03 | 0.87 | 0.06 | 0.03 | 0.02 | 15.7 |
| Late cessation | 0.03 | 0.05 | 0.87 | 0.04 | 0.02 | 17.5 |
| Frequent relapse | 0.00 | 0.02 | 0.05 | 0.85 | 0.09 | 16.2 |
| Persistent injection | 0.00 | 0.02 | 0.02 | 0.15 | 0.81 | 31.9 |
Abbreviation: ALIVE, AIDS Linked to the Intravenous Experience.
The probabilities on the diagonal are the average posterior probabilities of group membership among persons assigned to the group, while the off-diagonals show the average posterior probability of group membership among persons not assigned to the group. Probabilities do not sum to 1 because of rounding.
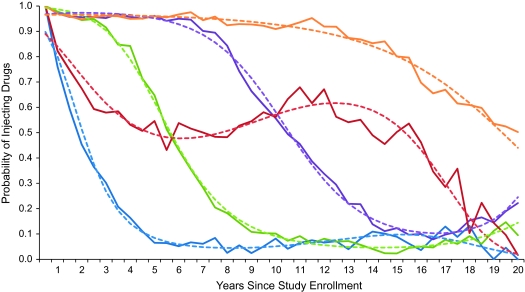
Figure 1 displays the trajectories of injection drug use over time based on the 5-class model. All groups were best represented by cubic trajectories (i.e., 2 shape changes), except the persistent injection group, which was best identified by a quadratic solution (i.e., 1 shape change). There were 3 trajectories associated with cessation. The early cessation group showed a sharp decline to very low injection levels during the first 5 years, while the delayed cessation and late cessation groups displayed less steeply declining injection levels after approximately 10 and 15 years, respectively. These groups represented 19%, 16%, and 18% of the sample, respectively. Because the early cessation group was characterized by the lowest levels of injection, sustained for the longest period of time, this group was identified as the long-term injection cessation group of interest and was used as the reference group in subsequent multivariate models. The frequent relapse group represented 16% of the sample and had fairly even drug use across the first 15 years of the study, with declining use thereafter. The probability of injection in this group vacillated around 0.50, suggesting that this group was characterized by frequent stops and relapses. The persistent injectors (32%) demonstrated high levels of injection throughout the course of the study.
Figure 1.
Trajectories of injection drug use among 1,716 injection drug users in the AIDS Linked to the Intravenous Experience (ALIVE) Study, Baltimore, Maryland, 1988–2008. The dotted lines represent the predicted probabilities of injection drug use conditional on membership in one of the 5 drug-use groups, while the solid lines represent the observed proportion of injection drug use given group membership. The y-axis represents the conditional probability of injection drug use, while the x-axis reflects time since study enrollment. The 5 groups (and prevalence of group within sample) are depicted with the following colors: blue, early cessation (19%); green, delayed cessation (16%); purple, late cessation (18%); red, frequent relapse (16%); orange, persistent injection (32%).
Predictors of injection drug use trajectories
In the adjusted model, several baseline factors were associated with the early cessation pattern as compared with the 2 other cessation groups (Table 3). Early cessation IDUs had injected drugs for fewer years at baseline than IDUs in the delayed cessation group. In addition, early cessation IDUs were more likely to be injecting heroin exclusively at the start of follow-up, were more likely to report less-than-daily injection, and were less likely to report having had sex with an IDU partner relative to the delayed cessation and late cessation groups. IDUs in the early cessation group were also more likely to engage in noninjection use of heroin and/or cocaine (snorting or smoking) than IDUs in the late cessation group. Finally, IDUs in the early cessation group were less likely to have had a recent incarceration at baseline than those in the late cessation group.
Table 3.
Injection Drug Use Group Membership Model Estimatesa (Relative to the Early Cessation Group) Based on Injection Drug Use Patterns, Adjustedb for Baseline Demographic Characteristics and Behavioral Factors in the Prior 6 Months, Among 1,716 Injection Drug Users From the ALIVE Study, Baltimore, Maryland, 1988–2008
| Injection Drug Use Group |
||||||||
| Delayed Cessation |
Late Cessation |
Frequent Relapse |
Persistent Injection |
|||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Constant | −1.360 | 0.96 | −2.052* | 0.98 | 2.012* | 0.89 | −0.272 | 0.82 |
| Age (per 10 years) | −0.149 | 0.20 | −0.011 | 0.20 | −0.286 | 0.21 | −0.109 | 0.18 |
| Duration of injecting drug use, years | ||||||||
| Quartile 1 (≤7) | 0.000 | 0.000 | 0.000 | 0.000 | ||||
| Quartile 2 (8–14) | 0.322 | 0.28 | 0.272 | 0.27 | 0.105 | 0.27 | 0.411 | 0.24 |
| Quartile 3 (15–20) | 0.692* | 0.30 | 0.133 | 0.31 | 0.420 | 0.30 | 0.617 | 0.27 |
| Quartile 4 (>20) | 0.911* | 0.37 | 0.329 | 0.37 | 0.010 | 0.40 | 0.635* | 0.33 |
| Ever having received drug treatment | −0.252 | 0.21 | 0.057 | 0.21 | −0.582* | 0.21 | −0.606* | 0.19 |
| HIV-infected at baseline | −0.189 | 0.22 | −0.148 | 0.23 | 0.265 | 0.22 | −0.137 | 0.20 |
| Type of drug injected | ||||||||
| Heroin | 0.000 | 0.000 | 0.000 | 0.000 | ||||
| Cocaine | 0.753 | 0.44 | 0.106 | 0.42 | −0.089 | 0.34 | 0.820* | 0.37 |
| Mixed heroin and cocaine use | 1.372* | 0.39 | 1.021* | 0.34 | 0.171 | 0.29 | 1.462* | 0.33 |
| Daily or more frequent injection | 0.578* | 0.21 | 0.736* | 0.21 | 0.301 | 0.22 | 0.855* | 0.19 |
| Daily alcohol use | −0.250 | 0.26 | 0.138 | 0.25 | 0.131 | 0.25 | 0.181 | 0.22 |
| Marijuana use | −0.204 | 0.20 | −0.021 | 0.21 | −0.200 | 0.21 | 0.354* | 0.18 |
| Noninjection heroin/cocaine use | −0.335 | 0.21 | −0.452* | 0.21 | −0.425* | 0.22 | −0.652* | 0.19 |
| Methadone maintenance therapy | −0.178 | 0.34 | −0.271 | 0.35 | −0.144 | 0.38 | −0.246 | 0.32 |
| Incarceration for ≥7 days | 0.270 | 0.29 | 0.533* | 0.27 | 0.543* | 0.27 | 0.152 | 0.26 |
| Sex with an IDU partner | 0.576* | 0.21 | 0.726* | 0.20 | 0.272 | 0.21 | 0.457* | 0.18 |
Abbreviations: ALIVE, AIDS Linked to the Intravenous Experience; HIV, human immunodeficiency virus; IDU, injection drug user; SE, standard error.
P ≤ 0.05.
The estimates shown are log odds ratios for a given characteristic/behavioral factor with membership in the specified group relative to the early cessation group.
Results were adjusted for length of time in follow-up, sex, race, educational attainment, marital status at baseline, and all of the characteristics listed in the table.
There were several differences between the early cessation group and the frequent relapse and persistent injection groups. Participants in the early cessation group had injected drugs for fewer years at baseline than the persistent injection group. Early cessation IDUs were more likely to have had a history of any drug treatment at baseline and were more likely to report noninjection heroin and/or cocaine use compared with the persistent and frequent relapse groups. IDUs in the early cessation group were less likely to report daily injection or more frequent injection at baseline compared with the persistent group. IDUs in the early cessation group were less likely to report a recent incarceration episode than the frequent relapse group. Several additional factors further differentiated the persistent injectors from the early cessation IDUs. The early cessation IDUs were less likely to report injecting mixed heroin/cocaine or cocaine exclusively, relative to heroin only, in comparison with the persistent injectors. Finally, IDUs in the early cessation group were less likely to report marijuana use and sex with an IDU partner compared with the persistent injectors.
Factors which were explored in univariate models and found not to be statistically significant at the P < 0.05 level and which therefore were not included in the final adjusted model included: history of employment at baseline, detoxification in the prior 6 months, sex with an anonymous partner in the previous 6 months, number of sexual partners in the previous 6 months, and the presence of any HIV-related physical illness symptom. HIV infection at baseline was not associated with drug-use trajectory.
DISCUSSION
The results of this study add to the existing evidence that addiction is a chronic condition characterized by distinct courses over time (24). While overall, injection drug use decreased in this community-based cohort from 1988 through 2008, the 5 longitudinal patterns identified confirm findings from previous research demonstrating that subgroups with varied trajectories of injection exist among IDUs (19). It was encouraging that nearly half of this cohort of IDUs demonstrated decreasing injection drug use over the 20 years of follow-up, with approximately 20% having stopped injecting for nearly 7 years. However, one-third of the sample represented persistent injectors. A number of factors distinguished the group that was abstinent for the longest period of time, highlighting potential points of intervention.
Some of the results were comparable to those of the prior analysis using the first 10 years of data from this cohort (19). Both analyses observed the same proportion of persistent injectors. However, the distribution across other groups was markedly different, likely partially reflecting the extended follow-up time, as well as methodological differences. For example, the frequent relapse pattern was twice as common in the earlier analysis. It is possible that some of the IDUs identified as frequent relapsers in the initial study transitioned to cessation during the 10 additional years of follow-up. However, some of the discrepancy may also be explained by the varying classification methods. In the initial analysis, group membership was highly dependent on injection behavior reported at the last available study visit. Because our focus was on distinguishing different cessation patterns, it was important to consider the full trajectory of injection behavior, which was possible via use of semiparametric models. This person-based approach is also objective in that the posterior probabilities of group membership provided a metric for assessing the appropriateness of classification (22). As a result, this analysis extended the prior analysis to identify several distinct patterns of injection cessation.
The identification of 3 distinct cessation patterns is further supported by the fact that they were differentiated by several behavioral characteristics. In the prior analysis, only history of incarceration distinguished the cessation group from the other groups (19). In our analysis, persons who stopped injecting for the longest period of time, compared with the 2 other cessation groups, were less likely to report mixed heroin and cocaine injection at baseline. These findings support a previous ALIVE analysis which demonstrated that injecting both heroin and cocaine was associated with longer time to short-term cessation (17). While medication-assisted therapy offers a pharmaceutical option for persons quitting heroin use, there is no such comparable treatment for cocaine users, potentially explaining the delayed time to cessation for those using mixed heroin/cocaine. Indeed, any history of drug treatment at baseline was also predictive of early injection cessation in comparison with not stopping. Cocaine users may have a riskier profile than heroin users; in previous analyses, they have tended to inject more frequently and to have riskier injection practices than persons using only heroin (27, 28). The positive relation between injecting cocaine only and persistent injection compared with long-term injection cessation remained after controlling for injection frequency, suggesting that the effects of cocaine use on drug-use trajectory may relate to the neurobiologic effects of cocaine in addition to the injection behaviors associated with its use.
IDUs who stopped injecting early also tended to be less severe injectors than participants in other groups. In general, IDUs injecting drugs less frequently than daily tend to have more favorable outcomes than daily injectors. Data from both community-based and treatment-based samples have also suggested a higher likelihood of short-term injection cessation among less frequent injectors, potentially suggesting a less severe addiction (15–17, 20, 29). In this analysis, heavier injection at baseline was not associated with the frequently relapsing injectors as compared with the early cessation group, suggesting that less severe use may be a predictor of both long-term and short-term cessation.
While heavier drug injection at baseline was associated with a lower likelihood of cessation, noninjection cocaine or heroin use had the opposite effect. Indeed, participants who reported noninjection heroin or cocaine use at baseline were more likely to stop injecting earlier. It is possible that some IDUs substituted noninjection drugs for injection drugs in their attempts to stop injecting. On the other hand, it is also possible that those who used noninjection drugs were less frequent injectors. While the data did not support the premise that noninjection drug use was more common among less frequent injectors than among daily injectors, data on frequency of noninjection drug use were not adequate to further substantiate drug preferences in this group.
While behavioral characteristics predicted drug-use trajectories in this analysis, no stable demographic factors at baseline, including age, were predictive of the patterns. In one of the first studies related to recovery from addiction, Winick (30) contended that aging drug users matured out of drug use. However, studies have increasingly supported the idea of multiple pathways of drug use, including those not related to aging, and while some aging drug users quit using because of exhaustion or changing life roles/increased responsibilities (such as parenting), others continually use drugs throughout the course of their lives (3, 31, 32). Our findings support the idea of multiple pathways of use, and while aging may be a factor for some IDUs who stop injecting, it appears that other factors may be more powerful predictors of injection cessation during adulthood.
There are several limitations of the current study that are important to consider in light of the results. First, latent class growth modeling has been criticized for potential overfitting of latent trajectory classes (33). While this is a valid concern, the selection of the final number of groups was based on prior research in similar populations (19, 24, 34). Growth mixture or general growth mixture models would allow for additional individual variation around the class mean and may be alternative models for validating the results obtained here (25). In addition, although the amount of time for which injectors reported having injected at baseline was included in the model, it was not incorporated into the shape of the trajectories. Behaviors engaged in prior to study enrollment may not have been reflective of behaviors observed after enrollment, resulting in misclassification of participants into pathways that did not reflect their entire drug-use history. Semiannual contact with study personnel may also have affected drug-use behaviors or the reporting of drug-use behaviors, and therefore the shapes of the trajectories; however, there was no evidence suggesting that this would have biased the groups differentially, and several studies in ALIVE and other cohorts have demonstrated validity and reliability of self-reported drug-use behaviors among IDUs (35–37).
Only time-fixed sociodemographic factors and behavioral variables were included. We did this intentionally in order to determine what stable factors predicted injection drug use pathways. However, drug-use behaviors are dynamic and highly susceptible to proximal factors. The inclusion of time-varying covariates in this model would have affected the shape of the trajectories rather than membership in the groups (22). An analysis of baseline factors in relation to drug-use trajectories is an important first step to clearly distinguish predictors, rather than consequences, of drug use over time. In future analyses, we plan to more closely examine long-term injection cessation in relation to time-varying predictors.
In addition, while the trajectories were based on injection drug use only, noninjection drug use may have influenced the shape and prevalence of the groups produced, particularly in light of research which suggests frequent transitions between differing routes of administration (17, 38, 39). While noninjection drug use (heroin, cocaine, crack, marijuana, and alcohol) was included in the final model, excluding this information from the trajectories limits the ability of the results to speak more generally to the course of addiction over time. Further, given that the level of noninjection drug use remained stable over time in the cohort, injection cessation does not necessarily signify recovery from addiction. However, sensitivity analyses displayed similar trajectories when noninjection drug use and injection drug use were included in the latent class models.
There is potential for survivor bias in that the persistent injectors were the most likely to die in comparison with the other groups. The potential for early censoring in the persistent group hampers the ability to determine whether there would be changes in the course of the trajectories with additional follow-up. However, the groups had similar median lengths of follow-up despite the higher mortality among the persistent users, suggesting that this bias may have had a limited impact on the study results.
The results of this study suggest that the prevention and treatment needs of IDUs are multidimensional and heterogeneous. Persistent injectors and those frequently stopping and relapsing to injection are the most in need of harm reduction, HIV prevention programs, and overdose prevention training, while IDUs in the cessation groups would benefit from support over longer time frames enabling them to fully transition out of injection. Additional research is still needed to develop and test interventions designed to target drug users’ individual trajectories and to determine the most effective timing for intervention. Although our results do not provide definitive information on when in the course of the trajectory intervention would be most successful, clinicians and counselors should consider IDUs’ patterns of use over time in tailoring treatment and care. For example, there is an urgent need for treatments designed to assist polydrug users, specifically those using cocaine along with heroin, since this leads to riskier behavioral patterns. Finally, programs should also consider the context in which people are using drugs (e.g., persons with an IDU partner); interventions and programs that are comprehensive in scope and are targeted not only toward individual drug-use patterns but also the context of drug use may be more successful in reducing injection drug use and its associated morbidity and mortality.
Acknowledgments
Author affiliations: Health Services, Policy and Practice Section, Department of Community Health, Brown University, Providence, Rhode Island (Becky L. Genberg); and Department of Epidemiology, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland (Becky L. Genberg, Stephen J. Gange, Vivian F. Go, David D. Celentano, Gregory D. Kirk, Shruti H. Mehta).
This study was supported by the National Institute on Drug Abuse at the National Institutes of Health (Dissertation Research Award R36DA025501 and grants R01DA012568 and R01DA004334).
Conflict of interest: none declared.
Glossary
Abbreviations
- ALIVE
AIDS Linked to the Intravenous Experience
- HIV
human immunodeficiency virus
- IDU
injection drug user
References
- 1.Hser YI, Hoffman V, Grella CE, et al. A 33-year follow-up of narcotics addicts. Arch Gen Psychiatry. 2001;58(5):503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- 2.Price RK, Risk NK, Spitznagel EL. Remission from drug abuse over a 25-year period: patterns of remission and treatment use. Am J Public Health. 2001;91(7):1107–1113. doi: 10.2105/ajph.91.7.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vaillant GE. A 20-year follow-up of New York narcotic addicts. Arch Gen Psychiatry. 1973;29(2):237–241. doi: 10.1001/archpsyc.1973.04200020065009. [DOI] [PubMed] [Google Scholar]
- 4.Robins LN, Slobodyan S. Post-Vietnam heroin use and injection by returning US veterans: clues to preventing injection today. Addiction. 2003;98(8):1053–1060. doi: 10.1046/j.1360-0443.2003.00436.x. [DOI] [PubMed] [Google Scholar]
- 5.Waldorf D. Life without heroin: some social adjustments during long-term periods of voluntary abstention. Soc Probl. 1970;18(2):228–243. [Google Scholar]
- 6.Haastrup S, Jepsen PW. Eleven year follow-up of 300 young opioid addicts. Acta Psychiatr Scand. 1988;77(1):22–26. doi: 10.1111/j.1600-0447.1988.tb05071.x. [DOI] [PubMed] [Google Scholar]
- 7.Van Ameijden EJ, Langendam MW, Notenboom J, et al. Continuing injecting risk behaviour: results from the Amsterdam Cohort Study of drug users. Addiction. 1999;94(7):1051–1061. doi: 10.1046/j.1360-0443.1999.947105110.x. [DOI] [PubMed] [Google Scholar]
- 8.Roy E, Haley N, Leclerc P, et al. HIV incidence among street youth in Montreal, Canada. AIDS. 2003;17(7):1071–1075. doi: 10.1097/00002030-200305020-00017. [DOI] [PubMed] [Google Scholar]
- 9.Gollub EL, Rey D, Obadia Y, et al. Gender differences in risk behaviors among HIV+ persons with an IDU history. The link between partner characteristics and women's higher drug-sex risks. The Manif 2000 Study Group. Sex Transm Dis. 1998;25(9):483–488. doi: 10.1097/00007435-199810000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Sibthorpe B, Lear B. Circumstances surrounding needle use transitions among injection drug users: implications for HIV intervention. Int J Addict. 1994;29(10):1245–1257. doi: 10.3109/10826089409047940. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham JA. Untreated remissions from drug use: the predominant pathway. Addict Behav. 1999;24(2):267–270. doi: 10.1016/s0306-4603(98)00045-8. [DOI] [PubMed] [Google Scholar]
- 13.Stall R, Biernacki P. Spontaneous remission from the problematic use of substances: an inductive model derived from a comparative analysis of the alcohol, opiate, tobacco, and food/obesity literatures. Int J Addict. 1986;21(1):1–23. doi: 10.3109/10826088609063434. [DOI] [PubMed] [Google Scholar]
- 14.Sobell LC, Ellingstad TP, Sobell MB. Natural recovery from alcohol and drug problems: methodological review of the research with suggestions for future directions. Addiction. 2000;95(5):749–764. doi: 10.1046/j.1360-0443.2000.95574911.x. [DOI] [PubMed] [Google Scholar]
- 15.Bruneau J, Brogly SB, Tyndall MW, et al. Intensity of drug injection as a determinant of sustained injection cessation among chronic drug users: the interface with social factors and service utilization. Addiction. 2004;99(6):727–737. doi: 10.1111/j.1360-0443.2004.00713.x. [DOI] [PubMed] [Google Scholar]
- 16.Langendam MW, van Brussel GH, Coutinho RA, et al. Methadone maintenance and cessation of injecting drug use: results from the Amsterdam Cohort Study. Addiction. 2000;95(4):591–600. doi: 10.1046/j.1360-0443.2000.95459110.x. [DOI] [PubMed] [Google Scholar]
- 17.Shah NG, Galai N, Celentano DD, et al. Longitudinal predictors of injection cessation and subsequent relapse among a cohort of injection drug users in Baltimore, MD, 1988–2000. Drug Alcohol Depend. 2006;83(2):147–156. doi: 10.1016/j.drugalcdep.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Saxon AJ, Calsyn DA, Jackson TR. Longitudinal changes in injection behaviors in a cohort of injection drug users. Addiction. 1994;89(2):191–202. doi: 10.1111/j.1360-0443.1994.tb00878.x. [DOI] [PubMed] [Google Scholar]
- 19.Galai N, Safaeian M, Vlahov D, et al. Longitudinal patterns of drug injection behavior in the ALIVE Study cohort, 1988–2000: description and determinants. Am J Epidemiol. 2003;158(7):695–704. doi: 10.1093/aje/kwg209. [DOI] [PubMed] [Google Scholar]
- 20.Termorshuizen F, Krol A, Prins M, et al. Long-term outcome of chronic drug use: the Amsterdam Cohort Study among drug users. Am J Epidemiol. 2005;161(3):271–279. doi: 10.1093/aje/kwi035. [DOI] [PubMed] [Google Scholar]
- 21.Vlahov D, Anthony JC, Munoz A, et al. The ALIVE Study, a longitudinal study of HIV-1 infection in intravenous drug users: description of methods and characteristics of participants. NIDA Res Monogr. 1991;109:75–100. [PubMed] [Google Scholar]
- 22.Nagin DS. Group-Based Modeling of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 23.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29(3):374–393. [Google Scholar]
- 24.Hser YI, Huang D, Chou CP, et al. Trajectories of heroin addiction: growth mixture modeling results based on a 33-year follow-up study. Eval Rev. 2007;31(6):548–563. doi: 10.1177/0193841X07307315. [DOI] [PubMed] [Google Scholar]
- 25.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–891. [PubMed] [Google Scholar]
- 26.Nylund KL, Asparouhov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–569. [Google Scholar]
- 27.Mehta SH, Galai N, Astemborski J, et al. HIV incidence among injection drug users in Baltimore, Maryland (1988–2004) J Acquir Immune Defic Syndr. 2006;43(3):368–372. doi: 10.1097/01.qai.0000243050.27580.1a. [DOI] [PubMed] [Google Scholar]
- 28.Nelson KE, Galai N, Safaeian M, et al. Temporal trends in the incidence of human immunodeficiency virus infection and risk behavior among injection drug users in Baltimore, Maryland, 1988–1998. Am J Epidemiol. 2002;156(7):641–653. doi: 10.1093/aje/kwf086. [DOI] [PubMed] [Google Scholar]
- 29.Termorshuizen F, Krol A, Prins M, et al. Prediction of relapse to frequent heroin use and the role of methadone prescription: an analysis of the Amsterdam Cohort Study among drug users. Drug Alcohol Depend. 2005;79(2):231–240. doi: 10.1016/j.drugalcdep.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 30.Winick C. Maturing out of narcotic addiction. Bull Narc. 1962;14(1):1–7. [Google Scholar]
- 31.Waldorf D. Natural recovery from opiate addiction: some social-psychological processes of untreated recovery. J Drug Issues. 1983;13(2):237–280. [Google Scholar]
- 32.Anglin MD, Brecht ML, Woodward JA, et al. An empirical study of maturing out: conditional factors. Int J Addict. 1986;21(2):233–246. doi: 10.3109/10826088609063452. [DOI] [PubMed] [Google Scholar]
- 33.Bauer DJ, Curran PJ. Distributional assumptions of growth mixture models: implications for overextraction of latent trajectory classes. Psychol Methods. 2003;8(3):338–363. doi: 10.1037/1082-989X.8.3.338. [DOI] [PubMed] [Google Scholar]
- 34.Xie H, Drake R, McHugo G. Are there distinctive trajectory groups in substance abuse remission over 10 years? An application of the group-based modeling approach. Adm Policy Ment Health. 2006;33(4):423–432. doi: 10.1007/s10488-006-0048-0. [DOI] [PubMed] [Google Scholar]
- 35.Latkin CA, Vlahov D, Anthony JC. Socially desirable responding and self-reported HIV infection risk behaviors among intravenous drug users. Addiction. 1993;88(4):517–526. doi: 10.1111/j.1360-0443.1993.tb02058.x. [DOI] [PubMed] [Google Scholar]
- 36.Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51(3):253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- 37.Macalino GE, Celentano DD, Latkin C, et al. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Educ Prev. 2002;14(5):367–378. doi: 10.1521/aeap.14.6.367.24075. [DOI] [PubMed] [Google Scholar]
- 38.Des Jarlais DC, Arasteh K, Perlis T, et al. The transition from injection to non-injection drug use: long-term outcomes among heroin and cocaine users in New York City. Addiction. 2007;102(5):778–785. doi: 10.1111/j.1360-0443.2007.01764.x. [DOI] [PubMed] [Google Scholar]
- 39.Neaigus A, Gyarmathy VA, Miller M, et al. Transitions to injecting drug use among noninjecting heroin users: social network influence and individual susceptibility. J Acquir Immune Defic Syndr. 2006;41(4):493–503. doi: 10.1097/01.qai.0000186391.49205.3b. [DOI] [PubMed] [Google Scholar]