Abstract
Context:
The Hertel model of chronic ankle instability (CAI) is commonly used in research but may not be sufficiently comprehensive. Mechanical instability and functional instability are considered part of a continuum, and recurrent sprain occurs when both conditions are present. A modification of the Hertel model is proposed whereby these 3 components can exist independently or in combination.
Objective:
To examine the fit of data from people with CAI to 2 CAI models and to explore whether the different subgroups display impairments when compared with a control group.
Design:
Cross-sectional study.
Patients or Other Participants:
Community-dwelling adults and adolescent dancers were recruited: 137 ankles with ankle sprain for objective 1 and 81 with CAI and 43 controls for objective 2.
Intervention(s):
Two balance tasks and time to recover from an inversion perturbation were assessed to determine if the subgroups demonstrated impairments when compared with a control group (objective 2).
Main Outcome Measure(s):
For objective 1 (fit to the 2 models), outcomes were Cumberland Ankle Instability Tool score, anterior drawer test results, and number of sprains. For objective 2, outcomes were 2 balance tasks (number of foot lifts in 30 seconds, ability to balance on the ball of the foot) and time to recover from an inversion perturbation. The Cohen d was calculated to compare each subgroup with the control group.
Results:
A total of 56.5% of ankles (n = 61) fit the Hertel model, whereas all ankles (n = 108) fit the proposed model. In the proposed model, 42.6% of ankles were classified as perceived instability, 30.5% as recurrent sprain and perceived instability, and 26.9% as among the remaining groups. All CAI subgroups performed more poorly on the balance and inversion-perturbation tasks than the control group. Subgroups with perceived instability had greater impairment in single-leg stance, whereas participants with recurrent sprain performed more poorly than the other subgroups when balancing on the ball of the foot. Only individuals with hypomobility appeared unimpaired when recovering from an inversion perturbation.
Conclusions:
The new model of CAI is supported by the available data. Perceived instability alone and in combination characterized the majority of participants. Several impairments distinguished the sprain groups from the control group.
Keywords: ankle injuries, joint instability, postural balance, recurrent ankle sprains
Key Points
The proposed new model of chronic ankle instability is supported by data from previous studies and the current study. More subgroups are identified than in previous models, with perceived instability as a common link.
On balance tests, all groups with chronic ankle instability performed more poorly than control groups.
The model will allow the development of specific injury-rehabilitation and injury-prevention programs for subgroups of chronic ankle instability.
Ankle sprains are very common not only in the sporting population1 but also in the general community.2 Although the acute symptoms of ankle sprain resolve quickly, many people report persisting problems, such as pain and instability.3 Chronic ankle instability (CAI) is one of the most common of these residual problems3 and has been defined as “repetitive bouts of lateral ankle instability resulting in numerous ankle sprains.”4 Despite the high prevalence of CAI, it remains a phenomenon that is poorly understood by researchers and clinicians alike. This has resulted in inconsistencies in terminology, definitions, and in hypotheses about impairments,4 relationships among the impairments,5 and the relative contributions of the impairments to activity limitations and participation restrictions.
The World Health Organization has classified the effects of disease in terms of impairments, which refer to problems in body structure or function; activity limitations, which refer to difficulties in execution of activities; and participation restrictions, which refer to changes in life situations, often involving a physical component (International Classification of Functioning, Disability, and Health).6 Impairments associated with CAI include increased ligamentous laxity and proprioceptive deficits. Activity limitations affect the execution of activities such as walking or jumping.7 Participation restrictions as a consequence of CAI can include cessation of sport or occupational involvement.
Inconsistencies in CAI research may be explained, in part, by the common assumption that CAI is a homogeneous condition. That is, it is often assumed that all cases of CAI arise from the same injury and develop the same impairments, leading to a consistent relationship between impairments and activity limitations. This assumption likely explains the conflicting results from investigations of CAI. If CAI is a heterogeneous condition that includes several homogeneous subgroups, conflicting reports of impairments, activity limitations, and participation restrictions may reflect researchers' recruitment of either an idiosyncratically determined subgroup or a heterogeneous population, thereby “washing out” significant findings.
The ability to define subgroups that constitute CAI would allow focused investigations of each of these homogeneous subgroups. Such a classification would aid the exploration of relationships among subgroups, including whether each subgroup is characterized by different impairments, activity limitations, and participation restrictions and, consequently, facilitate the development of targeted treatment and prevention strategies.
HISTORICAL BACKGROUND OF THE CONCEPT OF CAI
Historically, several terms have been used interchangeably to describe the phenomenon of ankle instability, including chronic ankle instability,8 chronic lateral ankle instability,9 ankle instability,10 residual ankle instability,11 chronic instability,12 recurrent instability,13 recurrent lateral ankle instability,14 and chronic ankle sprain.15 Although there is no consensus that these terms represent the same phenomenon, we consistently use the term chronic ankle instability (CAI) in this retrospective study.
The most commonly cited characteristics of CAI include giving way of the ankle,9,16–18 mechanical instability,9,18–20 pain and swelling,14,17,20,21 loss of strength,22 recurrent sprain,5,20,23–25 and functional instability.9,18,26 Residual problems can persist for decades,27 with up to 72% of people unable to return to their previous level of activity.28 Some residual problems, such as fear of the ankle giving way, have been reported to continue to worsen over time rather than improve.29 Additionally, the likely development of impairment and activity limitation is independent of the severity of the initial injury30–34 and is not confined to the injured limb; problems have been reported in the contralateral ankle of 85% of people who develop CAI after unilateral sprain.28 Reported participation restrictions include decreasing the level of exercise,28 change in type of sport,35 and withdrawing from occupational activity.29
The earliest investigators of CAI described 2 subgroups: those with patient-reported ankle symptoms and those with abnormal physical findings.36 Freeman37 subsequently termed these ankle symptoms functional instability. He defined functional instability as the tendency for the foot to give way. Thus, 2 main subgroups of CAI became widely accepted: those with mechanical instability and those with functional ankle instability.
Although the definition of mechanical instability is universally accepted as pathologic ligamentous laxity about the ankle-joint complex,4,12,18,19 no universally approved definition of functional ankle instability exists.38 Evans et al31 described functional instability as a subjective complaint of weakness; this description was expanded by Lentell et al16 to include pain and the perception that the ankle felt less functional than the other ankle and less functional than before the injury. Tropp et al39 distinguished functional instability from mechanical instability by defining it as joint motion that did not necessarily exceed normal physiologic limits but that was beyond voluntary control. Other proposed characteristics of functional ankle instability have included perceived or actual giving way of the ankle (or both)10,16,40 and other characteristics previously associated with CAI in general: pain and swelling30 and recurrent sprain.41,42 That is, various definitions of functional ankle instability have been used to determine eligibility criteria when recruiting participants to studies. Such differences in inclusion criteria may explain the inconsistent findings from CAI research to date.
The relationship between mechanical instability and functional instability has also been widely debated and variously described as “little or none,”9,20 “not constant,”43 and “commonly occurring.”44 The proposed temporal relationship between mechanical and functional instability also varies, with functional ankle instability inferred as either a direct consequence of mechanical instability34 or, conversely, a cause of mechanical instability.45 Recurrent sprain is further proposed to be an independent consequence of mechanical instability,46 functional instability,47 or both.45 Thus, little consensus exists in the literature as to the relationship among these variables.
Hertel4 proposed a model involving mechanical and functional instability that is widely accepted. In this model, mechanical and functional instability are not mutually exclusive but part of a continuum, and recurrent sprain occurs when both conditions are present. Mechanical instability is thought to result from various anatomic changes that may exist in isolation or in combination. These changes are proposed to lead to insufficiencies that predispose the person to further episodes of instability. Functional instability is proposed to result from functional insufficiencies such as impaired proprioceptive and neuromuscular control.4 When mechanical and functional insufficiencies are present, recurrent sprain results. However, anecdotally, participants have reported residual feelings of instability and ankle laxity after ankle sprain but have not reinjured their ankles. This has led to a potential evolution of the Hertel model, separating recurrent sprain from the presence of both instabilities. Thus, our first objective was to propose a refinement of the CAI model proposed by Hertel. The new model expands the number of subgroups from 3 to at least 7 and examines the fit of available ankle data to both models.
We hypothesized, based on preliminary evidence, that impairments may vary among the subgroups of the proposed model.34,39,40,45 For example, previous researchers34,39,48 demonstrated that postural stability was impaired in participants with functional instability, whether or not mechanical instability was present. In contrast, peroneal reaction times after an inversion perturbation were longer in participants with functional instability without mechanical instability than in those with mechanical instability alone.45 Thus, depending on the impairment, participants with mechanical and functional instability may perform differently than those with only functional instability. Further exploration of all subgroups in the proposed model may reveal unique sets of impairments characterizing that subgroup.
If homogeneous subgroups exist within the broad category of those with CAI, then the presence or absence of impairments and the relationships among impairments, activity limitations, and participant restrictions can be better clarified. Our second objective, therefore, was to explore if impairments within the subgroups differ from those within a control group or from each other.
METHODS
Objective 1: Fit of Data to the Models
Proposed Subgroups Within CAI
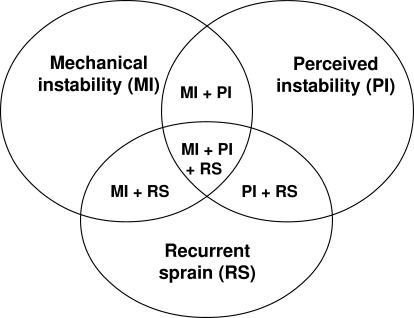
The model that we propose is an evolution of the Hertel original model. Hertel4 originally described CAI as consisting of 2 subgroups, classified according to the presence of either mechanical instability or functional instability; when these 2 impairments coexist, a third subgroup, recurrent sprain, arises. Unlike the Hertel model, however, our new model proposes that all 3 subgroups, including recurrent sprain, can be present either independently or as comorbid entities, resulting in 7 subgroups (Figure 1). We developed the new model while analyzing data from 2 recent studies49,50 to enable classification of all ankles with CAI, because not all ankles could be classified according to the Hertel model. In particular, a number of participants had both mechanical and functional instability but did not suffer recurrent sprains, and, conversely, some participants suffered recurrent sprains but had neither mechanical nor functional instability.
Figure 1.
Chronic ankle instability model showing the 7 proposed subgroups.
Because functional instability is now used with widely different meanings, we further propose that the term functional instability be replaced by perceived instability. The single characteristic of functional instability on which there is consensus dating back to the original observations of Freeman37 is that the patient perceives the ankle to be unstable, whether or not this perception is associated with physical signs. Recently, questionnaires have been developed to quantify functional instability,51–54 and each of these has consistently relied on the perception of instability as the basis for the instrument. Use of the term perceived instability would clarify the difference between the impairments involved in CAI and any functional or activity limitations that may result or coexist.
Data Extraction
To examine the fit of available ankle data to both models, we used data from 2 of our recent studies.49,50 In one study,50 we assessed 115 adolescent dancers (age = 14.2 ± 1.8 years) at baseline, and followed them for 13 months or until they sustained an inversion ankle sprain. In the other study,49 we tested 41 adults (age = 23.1 ± 6.7 years) with functional ankle instability for various impairments and compared them with 20 healthy control participants (age = 24.5 ± 9.9 years). Functional ankle instability was defined as the perception that the ankle was chronically weaker, more painful, or less functional than the other ankle or than before the first sprain.
The following criteria were used for fitting data to the models. Functional or perceived instability was defined as a score of ≤27 on the Cumberland Ankle Instability Tool (CAIT).51 The CAIT is a valid and reliable measure of functional ankle instability.51 To assess mechanical instability at the ankle, the modified anterior drawer test (in which the tibia is moved backward on the talus) was performed. On a 4-point scale, hypomobility was defined as 0, normal range as 1 or 2, and severely lax and mechanically unstable as 3. Although using a manual test for ligament laxity has known limitations, the same examiner tested all ankles and was blind to ankle status. Intrarater reliability for this method is excellent.55 For the purposes of this paper and in the absence of an agreed-upon definition, we defined recurrent sprain as a history of 3 or more sprains to the same ankle.
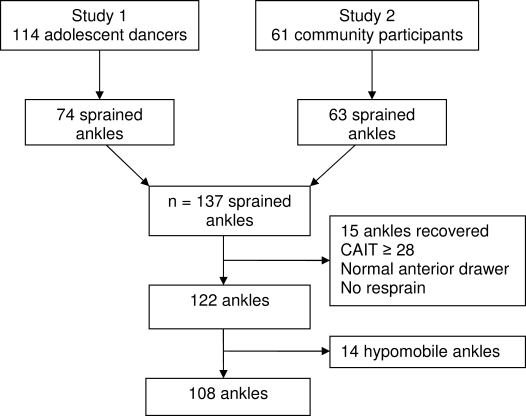
In the 2 studies combined, a total of 137 ankles had sustained sprains. Excluded from further analysis were 29 ankles: 15 were considered recovered because they had a normal anterior drawer test, CAIT score ≥28, and no resprain; 14 displayed hypomobility on the anterior drawer test. Thus, 108 ankles were included in the first analysis (Figure 2).
Figure 2.
Flow chart of ankle selection for objective 1: fit of ankles to the models. Abbreviation: CAIT, Cumberland Ankle Instability Tool.
Objective 2: Types of Impairments Associated With Subgroups and Compared With Controls
To explore whether impaired performance in selected physiologic and functional tests was associated with different subgroups and was not impaired in control participants, we compared the findings on these tests from our same 2 studies.49,50 We included those tests common to the 2 studies: 2 measures of balance and 1 measure of motor control. One measure of balance was the number of foot lifts in 30 seconds while balanced on 1 leg with the eyes closed.49 For this test, participants stood in a standardized position on 1 leg. They looked straight ahead, and their arms were relaxed by their sides. The non–weight-bearing leg was bent so that the foot touched the calf of the stance leg. The number of times any part of the stance foot lifted off the floor was counted in a 30-second period. Foot lifts included, for example, lifting of the first metatarsophalangeal or toe joint or shifting of the foot across the floor. The second test was the ability to balance on the ball of the foot (demipointe) for 5 seconds.49 From a standardized position, the heel was lifted from the floor and the participant balanced without moving. Motor control was assessed as the time to recover from an inversion perturbation. Oscillation in the mediolateral direction was measured using a 3-dimensional tracking device (FASTRAK; Polhemus, Colchester, VT) while standing on 1 leg with the foot flat. A 15° inversion perturbation was applied, and the time until stabilization of the mediolateral oscillation was determined. Further information on these methods is published elsewhere.49,50
To analyze relationships between test performance and group, data from only 1 ankle of each participant were included. Therefore, for participants with bilateral instability, we analyzed data from the more severely affected ankle, that is, the ankle that could be classified in several subgroups. In cases of bilateral instability with the same classification for both ankles, the ankle with the lower CAIT score was used.
Data from healthy, uninjured participants (external controls) from these same 2 studies were included to enable further comparison. To be included as an external control, participants were required to have no history of ankle sprain, a CAIT score ≥28, and a normal anterior drawer test in each ankle. The test ankle for external controls was randomly selected.
Of the original 175 participants, 52 were excluded, either because they had fully recovered from an ankle sprain (n = 15) or because they were healthy uninjured participants who did not meet the inclusion criteria (n = 37). This resulted in 81 participants with CAI and 42 external controls. Of the participants with CAI, 45 had unilateral CAI and 36 had bilateral CAI. The test ankle for 15 of the participants with bilateral instability was selected on the basis of CAIT score because of similar classification for both ankles.
To explore if hypomobility is associated with different impairments, we included the data from participants with that characteristic. Of the 81 participants, 10 were classified as hypomobile. For participants with bilateral hypomobility, the same criteria used above were used to determine which ankle to include.
Statistical Analysis
Because the study was a retrospective exploration, we performed no statistical analysis for significance. Refinement of the Hertel model (objective 1) was determined by calculating the numbers and percentage fit of the ankles into each of the subgroups. To assess whether impairments within the different subgroups differed from a control group or from each other (objective 2), we described the measures of balance, which included the average number of foot lifts (mean ± SE) and the number of people in each subgroup and among the external controls who failed to balance on demipointe. In addition, for each subgroup and the external controls, we described the measure of motor control, which was the time to recover from an inversion perturbation (mean ± SE). A number of participants failed to return to their preperturbation performance in the test time, so they were assigned a time of 4.5 seconds, which was 0.5 seconds longer than the longest recovery time of those who completed the task. This method of analysis has been used previously.56 Ideally, survival analysis would be used for such data, but it is inappropriate here because of the retrospective nature of this analysis.
To assist in comparing the external-control participants with the various subgroups and to give some indication of impairment severity, the Cohen d, using the pooled SD of the external controls and the subgroup of interest, was calculated. In addition, plots were drawn of the mean and 95% confidence intervals for the number of foot lifts in 30 seconds and the time for each group to recover from a perturbation. If confidence intervals overlap by a quarter of the average length of the intervals and the group sizes are greater than 10, then this is an indication that the P value would be close to .05.57
RESULTS
Objective 1: Fit of Data to the Models
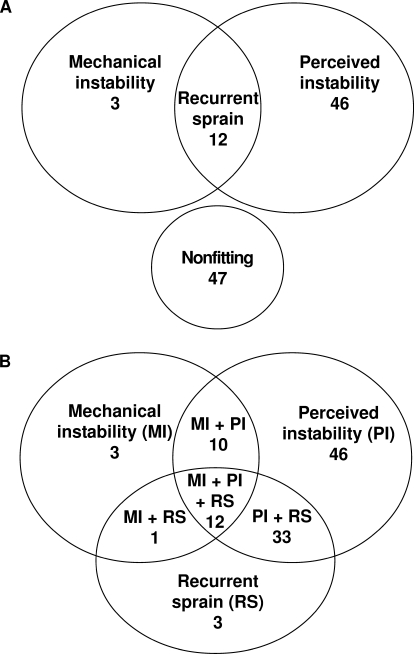
In the first analysis (n = 108 ankles), 61 ankles (56.5%) fit the Hertel model and 47 ankles did not (Figure 3). Data from all 108 ankles fit the new proposed model with high fidelity for each subgroup. The percentage fit for the proposed subgroups was perceived instability, 42.6%; perceived instability and recurrent sprain, 30.5%; perceived and mechanical instability and recurrent sprain, 11.1%; mechanical and perceived instability, 9.3%; mechanical instability, 2.8%; recurrent sprain, 2.8%; and mechanical instability and recurrent sprain, 0.9%.
Figure 3.
Fit of the ankle data to the Hertel4 model (A) and the new model (B). A total of 47 ankles did not fit the Hertel model.
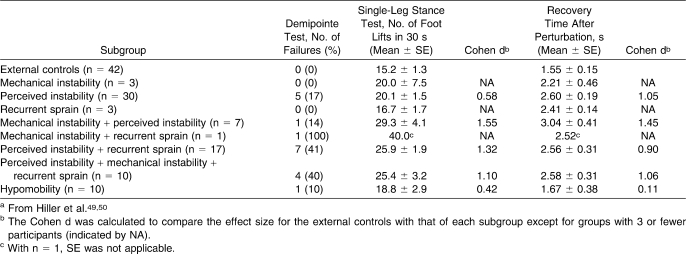
Objective 2: Level of Impairments Within Different Subgroups Compared With Control Group
The second analysis of 81 participants suggested that all subgroups were impaired on at least 1 measure compared with external controls: that is, they experienced more failures in the demipointe perturbation test, had more foot lifts in the single-leg–stance test, and took longer to recover from a perturbation (Table; Figures 4 and 5). However, impairment severity varied. We could not further explore 3 subgroups (mechanical instability, recurrent sprain, and mechanical instability plus recurrent sprain) because each cell contained too few participants.
Table.
Fit of Data According to the Proposed Subgroups and Controlsa
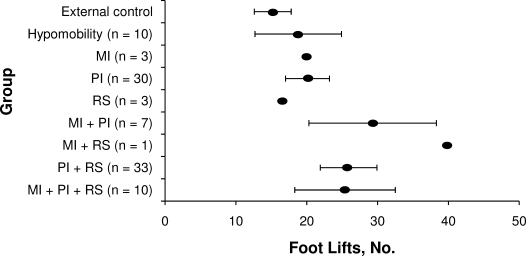
Figure 4.
Forest plot of the foot-lifts balance test in which the number of foot lifts was determined in a 30-second period (mean and 95% confidence intervals for groups with n > 6). Abbreviations: MI, mechanical instability; PI, perceived instability; RS, recurrent sprain.
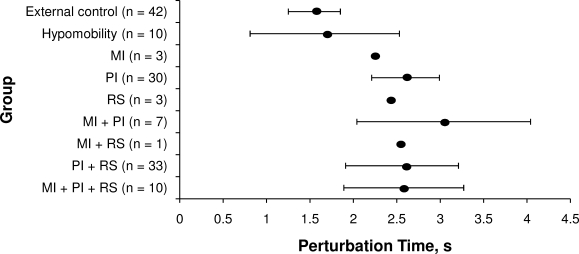
Figure 5.
Forest plot of the time to recover from an inversion perturbation (mean and 95% confidence intervals for groups with n > 6). Abbreviations: MI, mechanical instability; PI, perceived instability; RS, recurrent sprain.
Performance in the foot-lifts test of balance was impaired in all subgroups compared with external controls, although the hypomobility group appeared to be less impaired. In contrast, performance in the balancing-on-demipointe test indicated that participants with recurrent sprain in combination with mechanical or perceived instability (or both) performed more poorly than participants with perceived instability with or without mechanical instability and the hypomobility group. The level of impaired performance was similar for the test of recovery from a perturbation among the tested subgroups except for the hypomobility group, which appeared to be unimpaired compared with the external controls.
DISCUSSION
Fit of the New Model
The good data fit from our 2 recent studies to the new model gives preliminary support to the proposed 7 subgroups of CAI. The original concept of subgroups based on mechanical instability, perceived instability, and recurrent sprain remains the same, but we propose that each of these, including those with recurrent sprain, can exist independently or in combination. The data fit demonstrated that it is possible to have mechanical instability and perceived instability without experiencing recurrent sprain. Previously, this would not have been expected. It should be noted, however, that the numeric values within each cell should not be taken as an indication of the expected prevalence of the different subgroups; they merely indicate that all data from the presented studies fit the model and that subgroups appear to exist. The numeric values noted here reflect the recruitment criteria for the 2 studies. Prevalence of each subgroup should therefore be tested in future research.
Exploring possible associations of different subgroups with different impairments indicates some potential trends. For example, all groups with perceived instability had greater impairment on the foot-lifts test of balance than the hypomobility group. The presence of recurrent sprain appeared to make it more likely that a person could not balance on demipointe when compared with subgroups without recurrent sprain. Finally, perceived instability alone or in combination appeared to be associated with a longer time to recover from an inversion perturbation than was demonstrated by either external controls or participants with ankle hypomobility.
Perceived instability appears to lead to the same degree of impairment as recurrent sprain in some tests, whereas the presence of hypomobility may modulate some effects. Chronic ankle instability has often been defined as the presence of recurrent sprain,4 with or without perceived instability.54,58,59 However, 52% of participants in the current study had perceived instability without recurrent sprain. It may be that the feeling of instability is the most prominent factor and is associated with increased severity of some functional impairments, activity limitations, and participation restrictions.
Of interest is that hypomobility, rather than mechanical instability, can also be associated with ankle sprain.59,60 Hypomobility in the current study appeared to result in either a decrease in degree or even an absence of some impairments. The presence of participants with hypomobility in CAI studies may, therefore, “wash out” significant findings and provide one explanation for inconsistent results. Hypomobility may constitute the basis for an additional subgroup and should be further investigated.
Impairments Associated With Specific Subgroups
We applied the new model to previously published reports to determine whether similar trends in impairment levels could be better interpreted. A review of ankle-instability research was undertaken and studies were examined when sufficient information was provided about participants' perceived and mechanical instability and recurrent sprains.4,34,39,45,48,58,61 Criteria for perceived instability included reports of persistent feelings of weakness, instability, or giving way. The specific impairments for which associations with the new subgroups were sought included balance, recovery from an inversion perturbation, and functional tasks.
This further exploration indicated that single-leg balance was impaired in participants with perceived ankle instability but not in those with mechanical instability or in external controls.34,39,40 Tropp et al39 found increased postural sway, measured using stabilometry, in participants with both perceived ankle instability and recurrent sprain compared with external controls. Both Konradsen and Ravn48 and Ryan34 found differences in postural sway between external controls and participants with either perceived ankle instability alone or perceived ankle instability in combination with mechanical instability. These studies and the current study provide preliminary evidence that perceived instability, when present in any combination, is associated with the ability to balance on a flat foot.
Recovery from an inversion perturbation has also been studied by measuring peroneal reaction times rather than the protocol we used. Peroneal latency times were similar for external controls and participants with either mechanical instability alone61 or mechanical instability combined with recurrent sprain.45 In contrast, latency times were longer for participants with perceived ankle instability combined with either recurrent sprain or mechanical instability than for external controls.40,45,48 Again, the perceived instability appears to mediate the impairment.
In contrast, in an investigation58 of ankle motion during functional tasks, patterns of motion were altered in participants with mechanical instability combined with perceived instability but not in either those with perceived instability alone or those who had recovered. In this study, mechanical instability appeared to be a mediating factor. Repeated episodes of giving way or recurrent sprain were inclusion criteria, so it would have been illuminating to divide both the mechanical and functional instability groups into those with and without recurrent sprain.
Taken together, these findings provide preliminary evidence for different associations or levels of impairment with different subgroups. However, although the new model provides preliminary evidence for the proposed subgroups within CAI, it does not resolve all issues. A single test of mechanical instability may not comprehensively detect pathologic laxity of all ankle ligaments. For example, Hubbard et al62 found no correlation among various tests of mechanical instability in participants with CAI. The tests investigated were fibular position using fluoroscopy, instrumented ankle laxity in 3 directions, and talar hypomobility. Yet in a related study, anterior and inversion laxity were the factors most predictive of CAI group membership,5 and, therefore, we suggest that at least these 2 directions be considered when assessing mechanical instability.
The definition of recurrent sprain also varies widely across studies. A review of the literature shows that definitions of recurrent sprain range from 2 to 8 previous sprains, with various time requirements since the last sprain. It is also unclear whether a lifetime history of 3 sprains separated by a number of years results in the same impairments or activity limitations as a recent history of 3 sprains separated by weeks or months. Finally, giving way of the ankle is often used as an inclusion criterion for studies of CAI. Because giving way can be either perceived or actual, we do not know if it belongs in the current model as part of perceived instability, as a recurrent sprain that does not have a physical response, or as a uniquely different subgroup.
A further interesting question is whether increasing severity of CAI is reflected in a hierarchy in the subgroups. Intuitively, we would expect that people in a subgroup with more components to be more seriously limited in activity and participation than those with only a single component, but this possibility requires further investigation.
Limitations
The present study had a number of limitations. Testing the model by fitting the data retrospectively means that although all subgroups can be shown to exist, the testing was limited to a single common test for mechanical and perceived instability and recurrent sprain. In particular, mechanical instability was tested only in the anterior-posterior plane using clinical tests (ie, manual testing), although instrumented arthrometry or radiographic measures in at least 2 planes is likely to be more accurate. The model requires validation with a separate group of participants. In addition, research for which participants are recruited using a broad definition of CAI and across a wide range of ages and activity levels would provide a better indication of subgroup prevalence. Specifically, such a study would determine whether it is possible for a participant to have recurrent sprain without mechanical or perceived instability. The retrospective nature of our exploration of impairments also limited the numbers and types of impairment that could be included and the statistical analysis.
Future Directions
To further our understanding of the impairments, activity limitations, and participation restrictions associated with CAI, we recommend that future authors describe participants using validated measurements of those variables that define the subgroups in both the original and evolved models. We further suggest that hypomobility status be reported to enable exploration of its role in CAI. In this way, homogeneous subgroups will ultimately be defined, enabling identification of the mechanisms causing persistent symptoms and design of specifically targeted treatments. To achieve these goals, we recommend standardized and comprehensive measurement of the relevant variables. Mechanical instability should be tested in at least the anterior-posterior and medial directions. Validated tools, such as the CAIT, should be used for assessing perceived instability, and the number and time frame of recurrent sprains should be recorded. In addition, the number of recent giving-way episodes, both perceived and real, should be noted. We also advise that activity limitation and participation restriction be measured using instruments such as the Foot and Ankle Ability Measure63 or the Foot and Ankle Outcome Score64 to increase our understanding of the relationships among subgroup, impairment, and lifestyle changes.
Clinical Implications
The new model may provide a basis for improved patient care. If different subgroups exhibit different deficits or different severities of deficit, then rehabilitation can be targeted to those deficits. Ultimately, a clinical-prediction rule may be developed to assist clinicians in determining both prognosis and the most efficacious treatment for individual patients.
CONCLUSIONS
The proposed new model of CAI is supported by data from previous studies. More subgroups have now been identified, and a common link among subgroups in the current study and others is the presence of perceived instability. With our proposed model, greater insight may be possible into the impairments, activity limitations, and participation restrictions in those with CAI. Although it requires further validation, the proposed model is likely to have a significant effect on clinical research and practice because specific rehabilitation and prevention programs can be developed for subgroups of patients with CAI.
Acknowledgments
Support for this study was provided by the National Health and Medical Research Council–Dora Lush Scholarship, Canberra, Australia (C.E.H.).
REFERENCES
- 1.Fong D. T., Hong Y., Chan L. K., Yung P. S., Chan K. M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 2.Bridgman S. A., Clement D., Downing A., Walley G., Phair I., Maffulli N. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg Med J. 2003;20(6):508–510. doi: 10.1136/emj.20.6.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Rijn R. M., van Os A. G., Bernsen R. M., Luijsterburg P. A., Koes B. W., Bierma-Zeinstra S. M. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121(4) doi: 10.1016/j.amjmed.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 4.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 5.Hubbard T. J., Kramer L. C., Denegar C. R., Hertel J. Contributing factors to chronic ankle instability. Foot Ankle Int. 2007;28(3):343–354. doi: 10.3113/FAI.2007.0343. [DOI] [PubMed] [Google Scholar]
- 6.Jette A. M., Keysor J. J. Disability models: implications for arthritis exercise and physical activity interventions. Arthritis Rheum. 2003;49(1):114–120. doi: 10.1002/art.10909. [DOI] [PubMed] [Google Scholar]
- 7.Snyder A. R., Parsons J. T., Valovich McLeod T. C., Curtis Bay R., Michener L. A., Sauers E. L. Using disablement models and clinical outcomes assessment to enable evidence-based athletic training practice, part I: disablement models. J Athl Train. 2008;43(4):428–436. doi: 10.4085/1062-6050-43.4.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Safran M. R., Benedetti R. S., Bartolozzi A. R., 3rd, Mandelbaum B. R. Lateral ankle sprains: a comprehensive review, part 1: etiology, pathoanatomy, histopathogenesis, and diagnosis. Med Sci Sports Exerc. 1999;31(7 suppl):S429–S437. doi: 10.1097/00005768-199907001-00004. [DOI] [PubMed] [Google Scholar]
- 9.Davis P. F., Trevino S. G. Ankle injuries. In: Baxter D. E., editor. The Foot and Ankle in Sport. Vol 1. St Louis, MO:: Mosby-Yearbook; 1995. pp. 158–164. [Google Scholar]
- 10.Karlsson J., Lansinger O. Lateral instability of the ankle joint. Clin Orthop Relat Res. 1992;276:253–261. [PubMed] [Google Scholar]
- 11.Bernier J. N., Perrin D. H., Rijke A. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32(3):226–232. [PMC free article] [PubMed] [Google Scholar]
- 12.Cooper P. S. Proprioception in injury prevention and rehabilitation of ankle sprains. In: Sammarco G. J., editor. Rehabilitation of the Foot and Ankle. St Louis, MO:: Mosby; 1995. [Google Scholar]
- 13.Corrigan B., Maitland G. D. Practical Orthopaedic Medicine. Cambridge, England:: Butterworth and Co Ltd; 1988. pp. 181–182. [Google Scholar]
- 14.Ng Z. D., Das De S. Modified Brostrom-Evans-Gould technique for recurrent lateral ankle ligament instability. J Orthop Surg (Hong Kong) 2007;15(3):306–310. doi: 10.1177/230949900701500313. [DOI] [PubMed] [Google Scholar]
- 15.Soderberg G. L., Cook T. M., Rider S. C., Stephenitch B. L. Electromyographic activity of selected leg musculature in subjects with normal and chronically sprained ankles performing on a BAPS board. Phys Ther. 1991;71(7):514–522. doi: 10.1093/ptj/71.7.514. [DOI] [PubMed] [Google Scholar]
- 16.Lentell G., Katzman L. L., Walters M. R. The relationship between muscle function and ankle stability. J Orthop Sport Phys Ther. 1990;11(12):605–611. doi: 10.2519/jospt.1990.11.12.605. [DOI] [PubMed] [Google Scholar]
- 17.Liu S. H., Jason W. J. Lateral ankle sprains and instability problems. Clin Sports Med. 1994;13(4):793–809. [PubMed] [Google Scholar]
- 18.Tropp H. Functional ankle instability revisited. J Athl Train. 2002;37(4):512–515. [PMC free article] [PubMed] [Google Scholar]
- 19.Eiff M. P. Ankle injuries in sport. In: Richmond J. C., Shahady E. J., editors. Sports Medicine for Primary Care. Cambridge, England:: Blackwell Science; 1996. pp. 447–458. [Google Scholar]
- 20.Hintermann B. Biomechanics of the unstable ankle joint and clinical implications. Med Sci Sports Exerc. 1999;31(7 suppl):S459–S469. doi: 10.1097/00005768-199907001-00007. [DOI] [PubMed] [Google Scholar]
- 21.Freeman M. A. R., Dean M. R. E., Hanham I. W. F. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47(4):678–685. [PubMed] [Google Scholar]
- 22.Kaminski T. W., Hartsell H. D. Factors contributing to chronic ankle instability: a strength perspective. J Athl Train. 2002;37(4):394–405. [PMC free article] [PubMed] [Google Scholar]
- 23.Garn S. N., Newton R. A. Kinesthetic awareness in subjects with multiple ankle sprains. Phys Ther. 1988;68(11):1667–1671. doi: 10.1093/ptj/68.11.1667. [DOI] [PubMed] [Google Scholar]
- 24.Lofvenberg R. Chronic lateral instability of the ankle joint. Acta Orthop Scand. 1994;65:96–97. doi: 10.3109/17453678909150088. [DOI] [PubMed] [Google Scholar]
- 25.Vaes P., Van Gheluwe B., Duquet W. Control of acceleration during sudden ankle supination in people with unstable ankles. J Orthop Sport Phys Ther. 2001;31(12):741–752. doi: 10.2519/jospt.2001.31.12.741. [DOI] [PubMed] [Google Scholar]
- 26.Monaghan K., Delahunt E., Caulfield B. Ankle function during gait in patients with chronic ankle instability compared to controls. Clin Biomech (Bristol, Avon) 2006;21(2):168–174. doi: 10.1016/j.clinbiomech.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 27.Lofvenberg R., Karrholm J., Lund B. The outcome of nonoperated patients with chronic lateral instability of the ankle: a 20-year follow-up study. Foot Ankle Int. 1994;15(4):165–169. doi: 10.1177/107110079401500401. [DOI] [PubMed] [Google Scholar]
- 28.Konradsen L., Bech L., Ehrenbjerg M., Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12(3):129–135. doi: 10.1034/j.1600-0838.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- 29.Verhagen R. A., de Keizer G., van Dijk C. N. Long-term follow-up of inversion trauma of the ankle. Arch Orthop Traum Surg. 1995;114(2):92–96. doi: 10.1007/BF00422833. [DOI] [PubMed] [Google Scholar]
- 30.Birmingham T. B., Chesworth B. M., Hartsell H. D., Stevenson A. L., Lapenskie G. L., Vandervoot A. A. Peak passive resistive torque at maximum inversion range of motion in subjects with recurrent ankle inversion sprains. J Orthop Sport Phys Ther. 1997;25(5):342–348. doi: 10.2519/jospt.1997.25.5.342. [DOI] [PubMed] [Google Scholar]
- 31.Evans G. A., Hardcastle P., Frenyo A. D. Acute rupture of the lateral ligaments of the ankle: to suture or not to suture? J Bone Joint Surg Br. 1984;66(2):209–212. doi: 10.1302/0301-620X.66B2.6368563. [DOI] [PubMed] [Google Scholar]
- 32.Gerber J. G., Williams G. N., Scoville C. R., Arciero R. A., Taylor D. C. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 33.Moller-Larsen F., Wethelund J. O., Jurik A. G., de Carvalho A., Lucht U. Comparison of three different treatments for ruptured lateral ankle ligaments. Acta Orthop Scand. 1988;59(5):564–566. doi: 10.3109/17453678809148786. [DOI] [PubMed] [Google Scholar]
- 34.Ryan L. Mechanical stability, muscle strength and proprioception in the functionally unstable ankle. Aust J Physiother. 1994;40(1):41–47. doi: 10.1016/S0004-9514(14)60453-0. [DOI] [PubMed] [Google Scholar]
- 35.Anandacoomarasamy A., Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. doi: 10.1136/bjsm.2004.011676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bosien W. R., Staples O. S., Russell S. W. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37(6):1237–1243. [PubMed] [Google Scholar]
- 37.Freeman M. A. R. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):669–677. [PubMed] [Google Scholar]
- 38.Konradsen L. Factors contributing to chronic ankle instability: kinesthesia and joint position sense. J Athl Train. 2002;37(4):381–385. [PMC free article] [PubMed] [Google Scholar]
- 39.Tropp H., Odenrick P., Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985;6(3):180–182. doi: 10.1055/s-2008-1025836. [DOI] [PubMed] [Google Scholar]
- 40.Konradsen L., Ravn J. B. Ankle instability caused by prolonged peroneal reaction time. Acta Orthop Scand. 1990;61(5):388–390. doi: 10.3109/17453679008993546. [DOI] [PubMed] [Google Scholar]
- 41.Casillas M. M. Ligament injuries of the foot and ankle in adult athletes. In: DeLee J. C., Drez D., editors. Sports Medicine: Principles and Practice. Vol 2. 2nd ed. Philadelphia, PA:: WB Saunders; 2002. pp. 2323–2348. [Google Scholar]
- 42.Konradsen L., Beynnon B. D., Renstrom P. A. Proprioception and sensorimotor control in the functionally unstable ankle. In: Lephart S. M., Fu F. H., editors. Proprioception and Neuromuscular Control in Joint Stability. Champaign, IL:: Human Kinetics; 2000. pp. 237–246. [Google Scholar]
- 43.Karlsson J., Peterson L., Andreason G., Hogfors C. The unstable ankle: a combined EMG and biomechanical modelling study. Int J Sport Biomech. 1992;8:129–144. [Google Scholar]
- 44.Denegar C. R., Miller S. J., 3rd Can chronic ankle instability be prevented? Rethinking management of lateral ankle sprains. J Athl Train. 2002;37(4):430–435. [PMC free article] [PubMed] [Google Scholar]
- 45.Rosenbaum D., Becker H-P., Gerngroß H., Claes L. Peroneal reaction times for diagnosis of functional ankle instability. Foot Ankle Surg. 2000;6(1):31–38. [Google Scholar]
- 46.MacAuley D. Ankle injuries: same joint, different sports. Med Sci Sports Exerc. 1999;31:S409–S411. doi: 10.1097/00005768-199907001-00001. [DOI] [PubMed] [Google Scholar]
- 47.Wester J. U., Jespersen S. M., Nielsen K. D., Neumann L. Wobble board training after partial sprains of lateral ligaments of the ankle: a prospective randomised study. J Orthop Sports Phys Ther. 1996;23(5):332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 48.Konradsen L., Ravn J. B. Prolonged peroneal reaction time in ankle instability. Int J Sports Med. 1991;12(3):290–292. doi: 10.1055/s-2007-1024683. [DOI] [PubMed] [Google Scholar]
- 49.Hiller C. E., Refshauge K. M., Herbert R. D., Kilbreath S. L. Balance and recovery from a perturbation are impaired in people with functional ankle instability. Clin J Sport Med. 2007;17(4):269–275. doi: 10.1097/JSM.0b013e3180f60b12. [DOI] [PubMed] [Google Scholar]
- 50.Hiller C. E., Refshauge K. M., Herbert R. D., Kilbreath S. L. Intrinsic predictors of lateral ankle sprain in adolescent dancers: a prospective cohort study. Clin J Sport Med. 2008;18(1):44–48. doi: 10.1097/JSM.0b013e31815f2b35. [DOI] [PubMed] [Google Scholar]
- 51.Hiller C. E., Refshauge K. M., Bundy A. C., Herbert R. D., Kilbreath S. L. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 52.Hubbard T. J., Kaminski T. W. Kinesthesia is not affected by functional ankle instability status. J Athl Train. 2002;37(4):481–486. [PMC free article] [PubMed] [Google Scholar]
- 53.Rozzi S. L., Lephart S. M., Sterner R., Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29(8):478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- 54.Docherty C. L., Gansneder B. M., Arnold B. L., Hurwitz S. R. Development and reliability of the Ankle Instability Instrument. J Athl Train. 2006;41(2):154–158. [PMC free article] [PubMed] [Google Scholar]
- 55.Baumhauer J. F., Alosa D. M., Renstrom P. A. F. H., Trevino S., Beynnon B. Test-retest reliability of ankle injury risk factors. Am J Sports Med. 1995;23(5):571–574. doi: 10.1177/036354659502300509. [DOI] [PubMed] [Google Scholar]
- 56.Hiller C. E., Refshauge K. M., Beard D. J. Sensorimotor control is impaired in dancers with functional ankle instability. Am J Sports Med. 2004;32(1):216–223. doi: 10.1177/0363546503258887. [DOI] [PubMed] [Google Scholar]
- 57.Belia S., Fidler F., Williams J., Cumming G. Researchers misunderstand confidence intervals and standard error bars. Psychol Meth. 2005;10(4):389–396. doi: 10.1037/1082-989X.10.4.389. [DOI] [PubMed] [Google Scholar]
- 58.Brown C., Padua D., Marshall S. W., Guskiewicz K. M. Individuals with mechanical instability exhibit different motion patterns than those with functional ankle instability and ankle sprain copers. Clin Biomech (Bristol, Avon) 2008;23(6):822–831. doi: 10.1016/j.clinbiomech.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 59.Hubbard T. J., Olmsted-Kramer L. C., Hertel J., Sherbondy P. Anterior–posterior mobility of the talus in subjects with chronic ankle instability. Phys Ther Sport. 2005;6(3):146–152. [Google Scholar]
- 60.Santos M. J., Liu W. Possible factors related to functional ankle instability. J Orthop Sports Phys Ther. 2008;38(3):150–157. doi: 10.2519/jospt.2008.2524. [DOI] [PubMed] [Google Scholar]
- 61.Isakov E., Mizrahi J., Solzi P., Susak Z., Lotem M. Response of the peroneal muscles to sudden inversion of the ankle during standing. Int J Sport Biomech. 1986;2:100–109. [Google Scholar]
- 62.Hubbard T. J., Kramer L. C., Denegar C. R., Hertel J. Correlations among multiple measures of functional and mechanical instability in subjects with chronic ankle instability. J Athl Train. 2007;42(3):361–366. [PMC free article] [PubMed] [Google Scholar]
- 63.Martin R. L., Irrgang J. J., Burdett R. G., Conti S. F., Van Swearingen J. M. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 64.Roos E. M., Brandsson S., Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 2001;22(10):788–794. doi: 10.1177/107110070102201004. [DOI] [PubMed] [Google Scholar]