Abstract
Objective:
To provide certified athletic trainers, physicians, and other health care professionals with recommendations on best practices for the prevention of overuse sports injuries in pediatric athletes (aged 6–18 years).
Background:
Participation in sports by the pediatric population has grown tremendously over the years. Although the health benefits of participation in competitive and recreational athletic events are numerous, one adverse consequence is sport-related injury. Overuse or repetitive trauma injuries represent approximately 50% of all pediatric sport-related injuries. It is speculated that more than half of these injuries may be preventable with simple approaches.
Recommendations:
Recommendations are provided based on current evidence regarding pediatric injury surveillance, identification of risk factors for injury, preparticipation physical examinations, proper supervision and education (coaching and medical), sport alterations, training and conditioning programs, and delayed specialization.
Keywords: adolescents, children, chronic injuries, microtrauma, growth, development
Overuse injuries in the pediatric population represent a significant health care concern. Some reports and clinical observations1,2 indicate that 50% of pediatric patients present to sports medicine clinics for chronic injuries. In addition to their costs (direct and indirect medical expenditures), these injuries also result in lost participation time, numerous physician visits, and lengthy and often recurring rehabilitation.3–5 Furthermore, athletes who sustain recurrent overuse injuries may stop participating in sports and recreational activities, thus potentially adding to the already increasing number of sedentary individuals and the obesity epidemic.
In the pediatric population, overuse injuries can include growth-related disorders and those resulting from repeated microtrauma.6 Growth-related disorders include Osgood-Schlatter disease, Sever disease, and other apophyseal injuries. Overuse injuries resulting from repetitive microtrauma and chronic submaximal loading of tissues include stress fractures, similar to those described in adult athletes.6 However, overlap exists between broad classifications; some growth-related disorders may occur in sedentary children but much less often than in their active peers.6 Regardless of the cause, these injuries can result in significant pain and disability. Although little research has identified causative factors for overuse injuries in children and adolescents, these injuries may be caused by training errors, improper technique, excessive sports training, inadequate rest, muscle weakness and imbalances, and early specialization.6–10 More than half of all reported overuse injuries are speculated to be preventable,5 but few empirical data support this statistic.
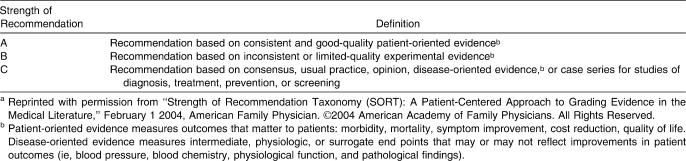
The purpose of this position statement is to provide certified athletic trainers, physicians, and other health care professionals with current best practice recommendations regarding the prevention of overuse injuries in pediatric athletes, including children (aged 6–12 years) and adolescents (aged 13–18 years).11 Even though specific age ranges have been identified, it is important to note that the occurrence of puberty, followed by skeletal maturity, is a far more important marker of maturity than chronologic age when managing pediatric overuse injuries. In particular, this position statement will provide recommendations based on current evidence (Table 1) pertaining to injury surveillance (eg, incidence, prevalence), identification of risk factors for injury, preparticipation physical examinations (PPEs), proper supervision and education (coaching and medical), sport alterations, training and conditioning programs, and delayed specialization.
Table 1.
Strength of Recommendation Taxonomy (SORT)a
RECOMMENDATIONS
Injury Surveillance
Research should be devoted to improved understanding of the prevalence, incidence, and economic cost of overuse injuries among pediatric athletes in the United States and should focus on prevention and treatment of these overuse injuries.12,13 Evidence Category: C
Funding and support for research into the prevalence, incidence, prevention, and treatment of pediatric overuse injuries should be increased.12,13 Evidence Category: C
All athletic health care providers should participate in injury-surveillance efforts, including accurate documentation in keeping with good clinical practice, and Web-based and other registries.12–14 Evidence Category: C
Resources and training for athletic health care providers (eg, certified athletic trainer, physician, physical therapist) to collect high-quality injury data must be developed.12,13 Evidence Category: C
Preparticipation Physical Examination
The PPE should be used as a means to screen each athlete for potential risk factors, including injury history, stature, maturity, joint stability, strength, and flexibility, which may be important for preventing recurrent injuries.5,6,15,16 Evidence Category: C
Children and adolescents with noted deficits on the PPE should be referred to appropriate medical specialists and health care providers (eg, physician specialist, certified athletic trainer, physical therapist) for further evaluation and corrective rehabilitation.5,15 Evidence Category: C
Robust documentation and injury-surveillance systems need to be developed to link PPE findings with injury, thereby identifying which measured factors may confer increased risk.14,17 Evidence Category: C
More research is needed to improve the effectiveness of the PPE, including strategies to implement the beneficial components more consistently and efficiently in the context of broader health-supervision and morbidity-prevention efforts for adolescents.14,17 Evidence Category: C
Identification of Risk Factors
Arm pain, fatigue, and decreased throwing performance should be recognized by athletes, coaches, parents, and medical personnel as early warning signs of potential overuse injuries in pediatric throwers.18,19 Evidence Category: A
Decreasing the volume of pitches as a means to prevent overuse injuries in throwing athletes is recommended.19–21 Evidence Category: A
Health care professionals should recognize that certain anatomic factors may predispose the athlete to overuse injury, including leg-length discrepancies, genu valgus, genu varus, pelvic rotation, and generalized joint hypermobility.9,10,22–24 Evidence Category: C
Coach Education and Medical Supervision
Pediatric athletes, parents, and coaches should be educated about the signs and symptoms of overuse injuries, and athletes should be instructed to notify an adult when such symptoms occur.18,19,25 Evidence Category: A
Coaches of youth and high school sports should have certifications or credentials identifying specific knowledge in areas related to sports safety, sports techniques and skills, psychosocial aspects of childhood and adolescence, growth and development, and common health and medical concerns.13,16,26,27 Evidence Category: C
Organized youth and interscholastic sports should be supervised by adults, ideally those with knowledge and training in monitoring for overuse injuries.5,13 Evidence Category: C
Medical personnel with training and education in pediatric sports injuries should be identified as referral sources to recognize, evaluate, and rehabilitate suspected overuse injuries.14,16Evidence Category: C
Sport Alterations
Emerging evidence indicates that the sheer volume of sport activity, whether measured as number of throwing repetitions18–21,28 or quantity of time participating,29,30 is the most consistent predictor of overuse injury. Efforts should be made to limit the total amount of repetitive sport activity engaged in by pediatric athletes to prevent or reduce overuse injuries. Evidence Category: B
Although injury thresholds are yet to be determined for specific activities and age ranges, some data suggest a general guideline of no more than 16 to 20 hours per week of vigorous physical activity by pediatric athletes.30 Evidence Category: B
Alterations or modifications to the existing rules for adult sports may help to prevent overuse injuries in pediatric athletes and should be considered by coaches and administrators for sports in which youth rules are lacking.5,13,31 Evidence Category: C
Adults should ensure that pediatric athletes play only 1 overhead throwing sport at a time, avoid playing that sport year-round, and use caution when combining pitching with other demanding throwing positions (eg, pitch 1 day and catch the next day) to ensure adequate time for recovery.7,28,32 Evidence Category: C
Parents and coaches should restrict the use of breaking pitches in order to prevent pitching-related arm injuries.20 If an individual pitcher can throw breaking pitches on a limited basis and remain symptom free, then it may be allowed; however, if the use of this pitch precedes the development of any throwing-related symptoms, it should be immediately terminated and the athlete should seek medical attention. Evidence Category: C
Pitching limits should be established for players 9 to 14 years old: full-effort throwing (ie, in competition) should be limited to 75 pitches per game, 600 pitches per season, and 2000 to 3000 pitches per year.20,33 Evidence Category: B
Pitchers between 15 and 18 years of age should throw no more than 90 pitches per game and pitch no more than 2 games per week.21,33Evidence Category: C
Training and Conditioning Programs
Preseason and in-season preventive training programs focusing on neuromuscular control, balance, coordination, flexibility, and strengthening of the lower extremities are advocated for reducing overuse injury risk, especially among pediatric athletes with a previous history of injury.34–36 Evidence Category: A
All pediatric athletes should begin participating in a general fitness program, emphasizing endurance, flexibility, and strengthening, at least 2 months before the sport season starts.5,9,37,38 Evidence Category: C
Pediatric athletes should have at least 1 to 2 days off per week from competitive practices, competitions, and sport-specific training.12,31 Coaches and administrators should consider these required days off when organizing season schedules. Evidence Category: C
Pediatric athletes should participate on only 1 team of the same sport per season when participation on 2 or more teams of the same sport (eg, high school and club) would involve practices or games (or both) more than 5 days per week.31 Evidence Category: C
Progression of training intensity, load, time, and distance should only increase by 10% each week to allow for adequate adaptation and to avoid overload.5,31 Evidence Category: C
After injury or delayed time without throwing, pediatric throwing athletes should pursue a gradual return-to-throwing program over several weeks before beginning or resuming full throwing activities.7,32 Evidence Category: C
Delayed Specialization
Pediatric athletes should be encouraged to participate in multiple sports and recreational activities throughout the year to enhance general fitness and aid in motor development.5,13 Evidence Category: C
Pediatric athletes should take time off between sport seasons and 2 to 3 nonconsecutive months away from a specific sport if they participate in that sport year-round.31 Evidence Category: C
Pediatric athletes who participate in simultaneous (eg, involvement in high school and club sports at the same time) or consecutive seasons of the same sport should follow the recommended guidelines with respect to the cumulative amount of time or pitches over the year.31 Evidence Category: C
BACKGROUND AND LITERATURE REVIEW
Repetitive stress on the musculoskeletal system without adequate and appropriate preparation and rest can result in chronic or overuse injuries in athletes of any age. In children and adolescents, this fact is complicated by the growth process, which can result in a unique set of injuries among pediatric athletes. Growth-related injuries most frequently affect the epiphyseal plates, where long bone growth occurs, and the apophyses, which serve as the bony attachments for musculotendinous units.6 Compression is usually responsible for epiphyseal injuries, whereas repeated tension or traction forces injure the apophyses.39 Differences in growth rates between the epiphyses and apophyses and between bone and muscle tissue are factors in apophyseal injury risk. These different growth rates may lead to relative myotendinous inflexibility and increased traction forces on the apophyses, contributing to traction apophyseal injuries.40,41 In throwers, repetitive microtrauma can lead to further bony insult, resulting in capitellar osteochondritis dissecans, a localized lesion of uncertain cause that involves the separation of articular cartilage and subchondral bone.42,43 Although most cases of osteochondritis dissecans resolve without consequence, lesions that do not heal after surgical intervention or a period of reduced repetitive impact loading may be responsible for future sequelae, including degenerative changes.44
Growth-center injuries may have long-term physical consequences and affect normal growth and development.16,40 However, little high-quality evidence supports or refutes this suggestion. In a systematic review45 of repetitive loading in gymnasts, females were at risk for stress-related injuries of the distal radius, including distal radial physeal arrest, but the lower-quality evidence of most of the included studies limited the strength of conclusions regarding whether physeal injury can inhibit radial growth. In a more recent systematic review,16 12 studies of baseball pitchers (3 case series, 9 case studies) with acute or chronic physeal injuries related to organized sport were analyzed. Stress-related changes were reported in all studies, including physeal widening in 8 reports, osteochondritis and radiographic widening of the proximal humeral growth plate in 2 reports, and humeral physis in 1 report.16 Most of these patients improved with rest and were able to return to baseball, although some did not continue to pitch.
Data from lower extremity physeal injury studies were also extracted for review. Ten studies16 of lower extremity physeal injury revealed that these injuries occurred mainly in runners, but soccer, tennis, baseball (catcher), and gymnastics athletes also showed radiographic changes of physeal widening. Among the 17 studies (11 case reports, 6 case series) of physeal injury in gymnasts, traumatic physeal arrest was described in 1, stress changes or fractures in 6, physeal widening in 5, and premature growth-plate closure in 5. In the 8 cross-sectional gymnastics studies reviewed, a distal physeal stress reaction was noted on radiographs from 10% to 85% of the athletes. Although the authors concluded that stress-related physeal injuries in pediatric athletes often resolve without growth complication after adequate rest and rehabilitation,16 prospective, randomized studies must be performed to provide stronger evidence before clinicians should relax their vigilance concerning the potential for growth disturbance.
An estimated 50% of overuse injuries in physically active children and adolescents may be preventable.5 The prevention of pediatric overuse injuries requires a comprehensive, multidimensional approach that includes (1) improved injury surveillance (ie, improved understanding of epidemiology), (2) identification of risk factors for injury, (3) thorough PPEs, (4) proper supervision and education (both coaching and medical), (5) sport alterations, (6) improved training and conditioning programs, and (7) delayed specialization. This preventive approach has been advocated by several prominent sports and health care organizations, including the American College of Sports Medicine,5 the World Health Organization and International Federation of Sports Medicine,13 the American Academy of Pediatrics,31 and the International Olympic Committee.12
Injury Surveillance
Before implementing any new prevention strategies or aiming to improve injury management, we must have adequate studies of epidemiology and a good understanding of the risk factors for pediatric overuse injuries.15 The literature regarding the epidemiology of overuse injuries in pediatric athletes is scarce at best, particularly the literature concerning American children.
However, the epidemiology of chronic injuries has been investigated in several international studies. In a 2003 Japanese study,46 the authors reviewed 196 stress fractures (125 males, 71 females) among 10 726 patients over a 10-year period. The average age of those with stress fractures was 20.1 years (range, 10–46 years), with 42.6% of patients between the ages of 15 and 19 years. The location of the stress fracture was somewhat specific to sport: the olecranon in baseball players, ribs in rowers, and tibial shaft stress fractures in ballet dancers, runners, and tennis, basketball, and volleyball players. Basketball players also sustained stress fractures to the metatarsals, whereas track athletes and soccer players incurred stress fractures to the tibial shaft and pubic bone. The authors concluded that stress fractures were common in high-functioning adolescent athletes, with similar proportions among male and female athletes. In another Japanese study29 of stress fractures in 208 athletes under the age of 20 years, the researchers found that the peak age of occurrence was 16 years, the most frequent site was the tibial shaft, and basketball was the sport most commonly associated with stress fractures. A 2006 retrospective study47 of stress fractures among 25 juveniles demonstrated that the age of onset was 12.9 ± 4.3 years (range, 3–17 years) and the tibia was most often affected (48%, n = 13), followed by the metatarsals (18.5%, n = 5). Using data from the High School Report Injuries Online (RIO) injury surveillance system, Fernandez et al48 reported that 4350 athletic injuries occurred among athletes participating in 9 high school sports during 1 academic year. Although these authors did not focus solely on overuse injuries, they noted that 53% (n = 2298) of these injuries were to the lower extremity; 2% of these injuries were classified as tendinitis and 1.3% as stress fractures. Specific investigations of the epidemiology of overuse injuries are warranted in the high school population.
Although studies on the general prevalence of pediatric overuse injuries are lacking, investigators have addressed the sport-specific prevalence of overuse injuries. Dubravcic-Simunjak et al2 retrospectively surveyed 469 elite junior figure skaters in Croatia, with 42% of female skaters and 45% of male skaters self-reporting an overuse injury at some point in their skating careers. In female singles ice skaters, the most frequent injury was a stress fracture (approximately 20%), followed by patellar tendinitis (14.9%). Male singles ice skaters were more likely to experience jumper's knee (16%), followed by Osgood-Schlatter disease (14.2%). Maffulli et al49 reported on overuse injuries of the elbow among elite gymnasts in the United Kingdom and found that 12 elbows of 8 patients (aged 11–15 years) displayed a spectrum of radiologic abnormalities, including olecranon physis widening and epiphyseal fragmentation.
In a recent investigation of Norwegian soccer players, the rates of overuse injuries were 0.2 (95% confidence interval [CI] = 0.1, 0.4) and 0.4 (95% CI = 0.0, 0.8) per 1000 player-hours in 6- to 12-year-old boys and girls, respectively.50 An increase in the incidence of overuse injuries was noted in an older cohort (13–16 years old) of boys (0.7, 95% CI = 0.4, 1.0) and girls (0.7, 95% CI = 0.3, 1.1) per 1000 player-hours, with the relative risk (RR) of overuse injury calculated as 2.9 (95% CI = 1.3, 6.4) and 1.7 (95% CI = 0.6, 5.5) in older boys and girls, respectively.50 In addition, 87% of the reported overuse injuries resulted in time loss from soccer that ranged from 1 to more than 21 days. Similarly, LeGall et al51 investigated the incidence of soccer-related injuries in elite French youth players and found that those younger than age 14 had more injuries during training sessions (ie, practices) and more growth-related overuse injuries, whereas older athletes more often sustained injuries during games. Overuse injuries accounted for 17.2% of all injuries and were mainly classified as tendinopathies (n = 108, 9.4%), osteochondroses (n = 72, 6.3%), or other overuse (n = 19, 1.6%). In a follow-up study of adolescent female soccer athletes over 8 seasons, overuse injuries accounted for 13.4% of all injuries.52
We need to better understand the prevalence, incidence, and economic impact of overuse injuries among pediatric athletes in the United States. Although few data are currently available about overuse injuries, the more than 7.5 million young people who participate in interscholastic sports53 and millions of others who participate in youth sports programs across the country represent a very large at-risk population worthy of the expenditure of time, effort, money, and improved surveillance by clinicians and researchers alike.
Preparticipation Physical Examination
A consensus has emerged that the PPE, as defined by several leading medical and allied health specialty societies, is the primary means of identifying at-risk athletes and initiating preventive measures.5,6,14,15,17 The main objectives of the PPE are to detect life-threatening or disabling medical or musculoskeletal conditions and to screen athletes for medical or musculoskeletal conditions that may predispose them to injury or illness.17 In the context of this position statement, the history and musculoskeletal examination are important in detecting and possibly preventing overuse injuries. Additional information on other aspects of the PPE can be obtained from the Preparticipation Physical Evaluation monograph.17
The history portion of the PPE should be used to recognize previous injuries and other possible signs of overtraining. Many overuse injuries can be identified from the answers provided in the history component.17 Furthermore, a history of stress fractures or chronic or recurring musculoskeletal injuries may be associated with nutritional insufficiencies, which should be investigated as needed.17
The physical examination of the musculoskeletal system should include evaluation of the athlete's physical stature and maturity (Tanner stage) and any deficits in strength and flexibility.5,17 In addition, the stability, symmetry, and range of motion of all joints and the relative symmetry, strength, and flexibility of all major muscle groups should be evaluated. These musculoskeletal assessments include range-of-motion tests, manual muscle tests, joint stress tests, flexibility tests, and balance tests, compared bilaterally. The Preparticipation Physical Evaluation17 describes the general 14-point musculoskeletal screening examination as an acceptable approach to evaluate the musculoskeletal system in athletes who are asymptomatic and without a history of previous injury. If the athlete describes a previous injury in the history portion or pain or positive findings are noted on the general screening examination, a more thorough joint-specific examination should be conducted.17 Ideally, a biomechanical assessment or functional screening test(s) should be incorporated to evaluate overall posture, gait mechanics, core stability, and functional strength.54 This may include either a single functional screening test, such as the overhead squat test,55 or a series of tasks56 to identify abnormal movement patterns. However, these tasks have yet to be validated in the pediatric population. Any deficits or concerns should be discussed with the athlete and parent, along with recommendations for correcting these deficits, including referral to a physician specialist, athletic trainer, or physical therapist if needed.5,14,15 Future researchers should focus on improving aspects of the musculoskeletal history, validating the general 14-point musculoskeletal screening examination and incorporating additional screening tests as possible predictors of overuse injuries.
A well-designed PPE can serve as a screening process from which prevention mechanisms can be developed.57 This process should be simple to administer and reliable and should use a combination of anthropometric and biomechanical measures to identify risk factors. Unfortunately, the PPE is often incompletely and inconsistently delivered. In most states, the PPE is mandated for high school athletes, but it is often not a requirement for those participating in club-based or youth sports. Required elements in the history and physical examination vary widely and are often not consistent with published national guidelines.58 The Preparticipation Physical Evaluation17 suggests that the ideal location for the PPE is within the athlete's primary care physician's office; however, it acknowledges other approaches, including the coordinated medical team examination and, although not recommended, the locker room-based examination. As a consequence of the lack of mandates, many adolescents seek their PPEs with a variety of providers and may be diverted from a medical “home,” where they can receive ongoing health immunizations and screening for the common psychosocial morbidities of adolescence.59 The lack of continuity also precludes connection with the rehabilitative follow-up deemed essential to injury prevention.60
Finally, the PPE may not be able to meet criteria for an appropriate screening process, even if implemented perfectly, because it is neither sensitive nor specific enough to adequately detect the life-threatening medical conditions that are so exceedingly rare60 or, in its current state, predict the potential for overuse injuries. Furthermore, as noted throughout this position statement, the evidence base is lacking as to which historical, anthropometric, and biomechanical findings confer increased musculoskeletal injury risk and which may be amenable to preventive interventions.
Identification of Risk Factors
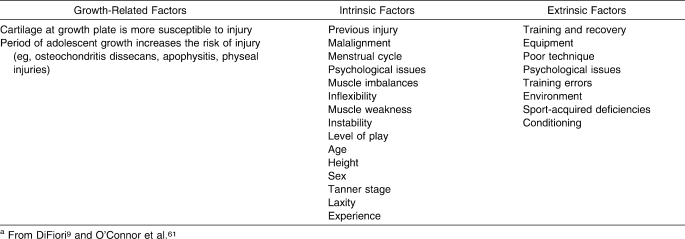
Little rigorous research has been conducted to investigate potential risk factors for overuse injuries in pediatric athletes. Table 2 lists a number of suspected growth-related intrinsic and extrinsic risk factors for overuse injuries, although these classifications and listings of risk factors are primarily based on anecdotal evidence.9,61
Table 2.
Potential Risk Factors Predisposing Pediatric Athletes to Overuse Injuriesa
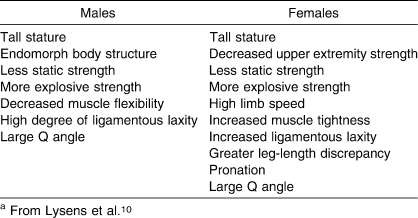
One group10 attempted to identify accident-prone and overuse-prone profiles in young adults by prospectively investigating the effects of numerous physical and psychosocial characteristics on the rate of acute and overuse injuries. They developed an overuse-injury–prone profile for both males and females, which included physical factors such as a lack of stability (eg, decreased static strength coupled with laxity), muscle tightness, malalignment, more explosive strength, and large body size (ie, height and mass), and psychological traits including degree of carefulness, dedication, vitality, and sociability (Table 3).10 Many of these characteristics (eg, anatomical alignment, flexibility, strength, speed) can be measured during a PPE or baseline fitness test, allowing clinicians to identify athletes potentially at risk for overuse injuries and to develop preventive measures.
Table 3.
Profiles of Overuse-Injury–Prone Male and Female Young Athletesa
Not surprisingly, baseball has been the most widely studied youth sport in the United States. Lyman et al18 prospectively evaluated 9- to 12-year-old baseball pitchers for pain or soreness in the shoulder or elbow during or after a pitching outing. Over 2 seasons, shoulder or elbow pain was noted in 47% (n = 141) of the pitchers, with most of the pain complaints considered mild (ie, without loss of time in games or practices). The authors also provided some associated pain-related factors that may be important in identifying those potentially at risk for subsequent overuse injuries. Elbow pain was related to increased age, decreased height, increased mass, increased cumulative pitch counts, arm fatigue, decreased self-perceived performance, participation in a concurrent weightlifting program, and participation in additional baseball leagues.18 The presence of shoulder pain was associated with an increased number of pitches thrown in games, increased cumulative pitch counts, participating with arm fatigue, and decreased self-perceived performance. Both arm fatigue and self-perceived performance were risk factors for both elbow and shoulder pain. Therefore, pain should not be ignored, because it is often the first indicator of an overuse problem.20 Rest should be incorporated in all programs; athletes who participated with arm fatigue were almost 6 times more likely to suffer from elbow pain and 4 times more likely to have shoulder pain that those who did not have arm fatigue.18
A subsequent investigation20 of 3 suspected risk factors (pitch type, pitch count, and pitching mechanics) found that the use of breaking pitches and high pitch counts increased the risk of both elbow and shoulder pain among youth pitchers. Specifically, the risk of elbow pain among pitchers using the slider increased 86% and the risk of shoulder pain in those throwing curveballs increased 52%. In addition, higher single-game pitch counts and higher cumulative (season-long) game pitch counts were associated with an increased risk of shoulder pain. This association between game pitch count and shoulder injury was strongest among 9- to 10-year-old and 13- to 14-year-old pitchers. Interestingly, pitching mechanics were not significantly associated with either elbow or shoulder pain in any of the age groups studied.20 The authors20 concluded that changeups remain the safest pitch for 9- to 14-year-olds to throw and that pitch limits, rather than inning limits, may be a better indicator of when pitchers should be removed from pitching to allow adequate rest.
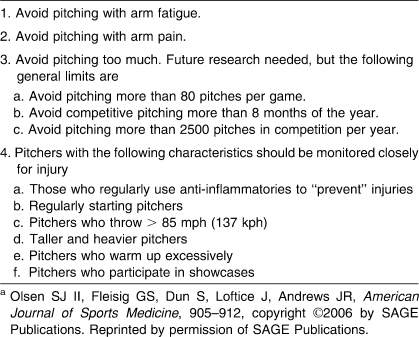
More recently, Olsen et al19 investigated risk factors for shoulder and elbow injuries in adolescent pitchers. Group analyses between pitchers with or without elbow or shoulder injury revealed that a greater percentage of injured pitchers started at another position before pitching, pitched with arm fatigue, and continued to pitch even with arm pain.19 In addition, those who suffered an injury had a greater fastball speed and participated in a greater number of showcases (multiday, high-level events in which athletes may participate in numerous games within a short time span). A subsequent factor analysis revealed the following risk factors: participating in more than 8 months of competitive pitching (odds ratio [OR] = 5.05, 95% CI = 1.39, 18.32), throwing more than 80 pitches per appearance (OR = 3.83, 95% CI = 1.36, 10.77), having a fastball speed greater than 85 mph (136.8 kph) (OR = 2.58, 95% CI = 0.94, 7.02), and pitching either infrequently (OR = 4.04, 95% CI = 0.97, 16.74) or regularly (OR = 36.18, 95% CI = 5.92, 221.22) with arm fatigue.19
With respect to lower extremity injuries, few authors have attempted to identify specific overuse-injury risk factors in pediatric athletes, and their findings are inconclusive. These studies are limited to research on medial tibial stress syndrome (MTSS) and stress fractures.30,62,63 In 2 investigations of risk factors for MTSS in high school cross-country runners, predictive variables differed.62,63 One group62 found that athletes with MTSS had a greater navicular drop (6.6 mm) than those who were asymptomatic (3.6 mm) and that the combination of navicular drop and sex accurately predicted 78% of MTSS cases. However, resting calcaneal position, tibiofemoral varum, and gastrocnemius length (ie, tightness) were not predictive. A subsequent investigation63 revealed that sex and body mass index were predictors of MTSS, with the latter being the only predictor when controlling for orthotic use. Additionally, compared with those without an injury history, high school cross-country runners with a history of previous injury were 2 times more likely to report MTSS (OR = 2.18, 95% CI = 0.07, 6.4) and 3 times more likely to use orthotics (OR = 3.0, 95% CI = 0.09, 9.4).63 Correlates of stress fractures in a general population of female adolescents have also been researched and, although age had the strongest association with a stress-fracture history (27% to 29% increased odds for each year beyond age 11), participation in more than 16 hours per week of vigorous activity (OR = 1.88, 95% CI = 1.18, 3.03) and in high-impact physical activity, such as basketball, soccer, volleyball, running, tennis, or cheerleading (OR = 1.06, 95% CI = 1.03, 1.10), was also related to stress-fracture history.30 They reported a slight (but nonsignificant) increased risk for stress fracture in the most sedentary girls, a reminder that participation in impact-loading physical activity is important in this population because of its positive effects on bone mineral density.30
In a subsequent clinic-based study of adolescent female athletes, only family history of osteoporosis or osteopenia was associated with stress fracture (OR = 2.96, 95% CI = 1.36, 6.45).64 However, in neither adolescent athlete investigation was stress fracture associated with irregular menstrual periods, as has been demonstrated in adult women athletes and military recruits.65 In combination, these investigations may begin to identify safe thresholds for participation in vigorous physical activity (16–20 h/wk). They also suggest that risk stratification must incorporate both intrinsic (eg, inherited skeletal quality) and extrinsic (eg, training volume) factors. Another area of focus concerning risk factors has been generalized joint hypermobility, which is characterized by mobility of multiple joints beyond the normal range of motion. Community prevalence of generalized joint hypermobility appears to depend on age, sex, and race, with reports ranging from 2% (adult Caucasian males) to 57% (African females of mixed ages).66 A considerable number of studies of rheumatology and pediatric clinic-based populations appear to demonstrate relationships between generalized joint hypermobility and insidious-onset arthralgia and fibromyalgia.67–75 Yet prospective studies of nonclinic populations are at best inconclusive as to whether joint hypermobility increases injury risk.
In a prospective study23 of 17-year-old military recruits, those with hypermobility had more injuries during boot camp than those who were not hypermobile. Another prospective study24 of youngsters 6 to 14 years old demonstrated that children with hypermobile joints had more complaints of joint pain than nonhypermobile children. A retrospective study76 of pediatric (aged 6–16 years) netball players in Australia showed that hypermobility was associated with an increased prevalence of self-reported injuries. In another small retrospective study77 including children and adults, more injuries were reported by hypermobile ballet dancers than by their nonhypermobile counterparts. In an attempt to describe overuse-prone profiles of young adults, Lysens et al10 reported that males and females with weak muscles, poor flexibility, and hypermobility may be at increased risk for overuse injuries.
Alternately, several prospective studies of mixed (child and adult) or adult athletic populations do not support the conclusion that joint hypermobility is related to injury risk. A prospective study78 of netball players aged 15 to 36 years demonstrated no differences in injuries based on hypermobility status. Studies of National Collegiate Athletic Association lacrosse players79 and professional soccer players80 also have indicated no differences in injuries based on hypermobility status. Finally, a retrospective study81 of female gymnasts aged 10 to 21 years found no relationship between hypermobility status and reported history of injuries.
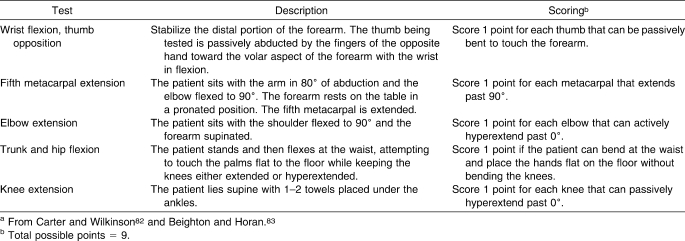
Screening for generalized joint hypermobility is relatively easy using the methods first proposed by Carter and Wilkinson82 and later modified by Beighton and Horan.83 This multijoint active range-of-motion screening procedure is widely accepted (Table 4). Incorporating this screening into the PPE might add only a few minutes to each assessment, but its use should depend upon the time, cost, and level of experience of the examiner administering the PPE.
Table 4.
The Beighton and Horan Joint Mobility Indexa
Proper Supervision and Education
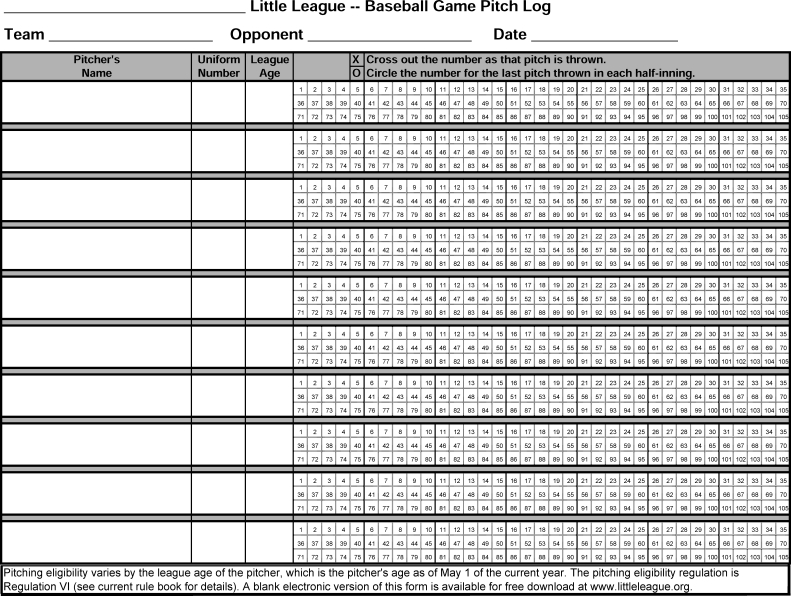
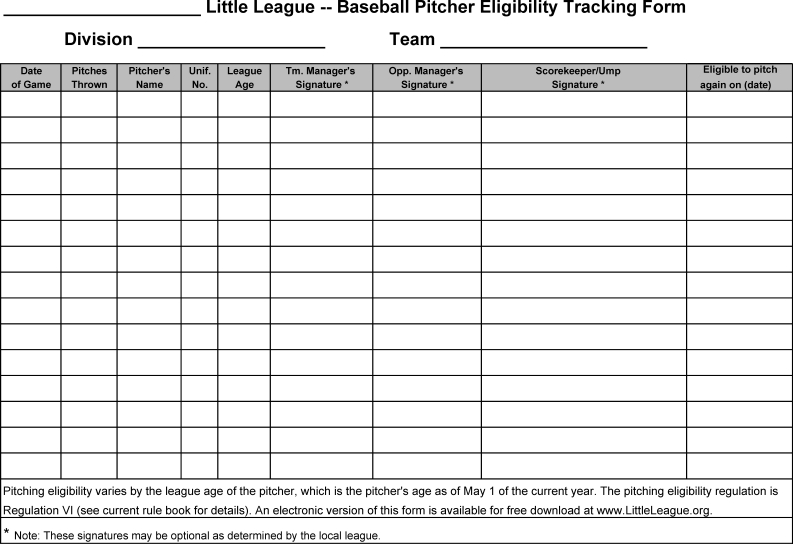
Organizations sponsoring interscholastic or club-based athletics in which pediatric athletes participate have the responsibility to ensure adequate coaching and medical supervision.5,13,14 Proper supervision by coaches and enforcement of the rules of the sport (which includes adequate education of both coaches and officials) may serve as a means to decrease overuse injury risk in this age group.9,15,50 For example, Little League Baseball provides pitch-count regulation (Appendix A), tracking sheet (Appendix B), and pitching eligibility forms, all of which are easily accessible to youth baseball coaches. The guidelines mandating pitch-count limits are adapted from scientific evidence and are updated frequently as new research emerges.84 Moreover, proper medical supervision at competitions and practices may allow for early recognition of overuse injuries in the beginning stages to permit proper evaluation, referral, and rehabilitation before they result in time lost from participation.14,15
Education of all athletes, parents, coaches, and officials regarding overuse injuries and preventive mechanisms is advocated. Athletes, parents, and coaches should all have knowledge of general signs and symptoms of overuse, including but not limited to a gradual onset of pain, pain presenting as an ache, no history of direct injury, stiffness or aching after or during training or competition, increasing periods of time for pain to resolve, point tenderness, visible swelling, missed training sessions as a result of the pain or injury, and a problem that persists.25 These signs and symptoms should not be ignored as “growing pains” but should be taken seriously by the athlete, parent, and coach. Athletes involved in running-based sports should be educated regarding sensible training habits and the proper fit and selection of running shoes to reduce impact forces. Athletes involved in throwing sports should be educated as to the potential risk factors for upper extremity overuse injuries, with specific emphasis on using arm fatigue as an indicator to stop throwing.18,19 All athletes should be educated on proper exercise progression and should gradually increase time, distance, and intensity by the 10% rule (see “Training and Conditioning” section below).57
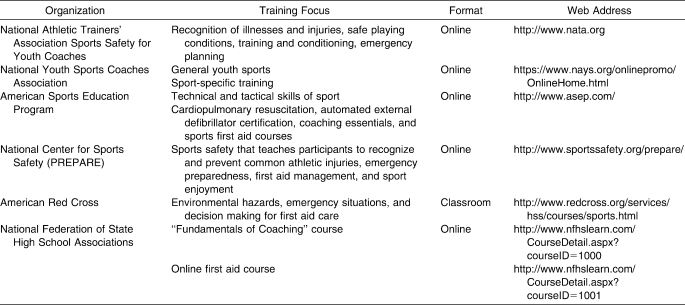
To our knowledge, no published studies have addressed the general knowledge of overuse injuries among coaches; however, reports describe the general lack of first aid, injury recognition, and management knowledge of high school26 and youth27 coaches. No mandated national coaching education program exists in the United States for youth sports, and the requirements for high school athletic coaches vary from state to state, with some requiring only first aid and cardiopulmonary resuscitation (CPR) certification. However, numerous coaching education programs provide information related to proper biomechanics of sporting skills, nutrition, physical conditioning, development of athletes, and prevention, recognition, and management of injuries (Table 5). Completion of at least 1 of these courses is recommended for all coaches working with pediatric athletes. Additionally, coaches should be encouraged to maintain their certifications and participate in continuing education opportunities to remain current with the latest sports safety information.
Table 5.
Coaching Education Programs
Sport Alterations
Alterations or modifications to the existing rules for adults may prevent overuse injuries in children and adolescents.5,13,31 These modifications may be simple, including shorter quarters or halves, bases closer together, less frequent games or practices, or pitch-count limits; or they may be more complex, such as the recommendation to match athletes by height, maturity, or skill as opposed to age.
Some experts are now moving away from the long-held and perhaps largely anecdotal belief that throwing breaking pitches is related to arm injuries in young baseball players. The only prospective study20 we were able to find appears to support this belief: pitchers throwing sliders had an 86% increased risk of elbow pain, and pitchers throwing curveballs had a 52% increased risk of shoulder pain. However, biomechanical studies comparing torque and moments generated by different types of pitches in 11- to 14-year-olds85 and 14- to 18-year-olds86 showed that the fastball imposed more demand than the curveball. Based on the results of these biomechanics studies, some researchers have postulated that throwing breaking pitches is not necessarily risky for young athletes. Yet it is important to recognize that the participants in these studies were healthy, with no history of arm injury, and, in the case of the Nissen et al86 study, perhaps slightly older than the players who are generally the target of the recommendation against throwing breaking balls.
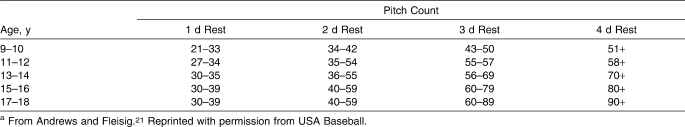
Furthermore, pitching limits should be established for 9- to 14-year-olds, with full-effort (ie, competition) throwing limited to 75 pitches per game and 600 pitches per season.20 Young throwers should also have adequate rest after a pitching event and adjust pitch limits for those rest days accordingly (Table 6). Table 7 lists baseball-pitcher–specific modification recommendations.
Table 6.
Recommendations for Pitch Counts on the First 4 Days After a Pitching Eventa
Table 7.
Suggested Sport-Modification Recommendations for Adolescent Pitchersa
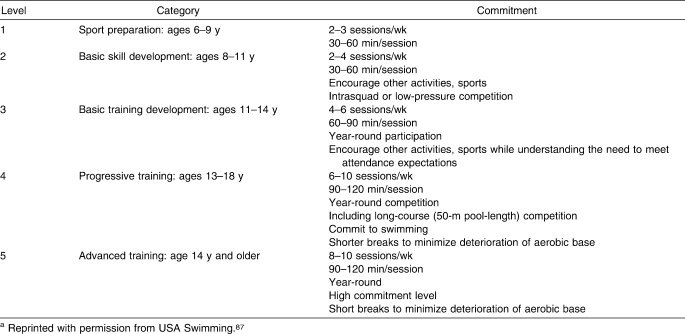
In addition to Little League, other athletic governing bodies and organizations have instituted sport modifications. The US Cycling Federation has imposed gear-ratio limits for athletes between 10 and 16 years of age,54 limiting the maximal stress or effort in those at the lower end of that age range. Running organizations in Australia also have age-related regulations, including set distances in which younger athletes may participate. Adolescents can begin participating in 5-km (3.1-mile) races at age 12 and in 10-km (6.2-mile) races at age 14. Half-marathon (21.1-km; 13.1-mile) and marathon (42.2-km; 26.2-mile) distances can be run beginning at ages 15 to 16 and >18 years, respectively.54 As described in Table 8, USA Swimming has recommendations for the number of sessions per week and the length of each session for various levels of competitive age-group swimming.87
Table 8.
Developmental Progression for Pediatric Swimmersa
Training and Conditioning
Proper training and conditioning, both before and during the season, may prevent overuse injuries. Unfortunately, in today's society, many youngsters are not as active as previous generations, leading to a phenomenon of cultural deconditioning.88,89 There has been a general decline in physical activity, including free play, walking to school, and regular physical-education classes, with a concurrent increase in sedentary activities, including watching television, playing video games, and, in some cases, physical activity limited to sport participation. Athletes with poorer levels of general fitness or conditioning may not be able to tolerate the demands of training required for sport participation. Therefore, all pediatric athletes should begin by establishing a good general-fitness routine that encompasses strengthening, endurance, and flexibility.5,9,37 Sufficient participation in general strength, endurance, and flexibility training, as well as lifestyle physical fitness (eg, taking the stairs instead of the elevator), should precede sport-specific training.38 Once a general foundation of fitness has been established, athletes should begin to gradually increase their training loads. Pediatric athletes are advised to follow the 10% rule, which allows for no more than a 10% increase in the amount of training time, distance, repetitions, or load each week.5,31 For example, a runner who is currently running 15 miles/wk (24 km/wk) should only be allowed to increase mileage to 16.5 miles (27 km) the following week. Similarly, athletes participating in strength training should increase only either repetitions or weight by 10% each week, not both. The goal of the 10% rule is to allow the body to adjust gradually to increased training intensity.
More recently, preventive training programs have been targeted specifically at the pediatric athlete. Although the primary focus of many of these programs has often been for the prevention of noncontact anterior cruciate ligament injuries, several authors34–36 have also investigated whether overuse-injury risk could be reduced among program participants. In a prospective study of a structured warm-up program including technique training, neuromuscular control, and balance and strengthening exercises, Olsen et al36 reported that participants had a reduction in overall injuries (RR = 0.49, 95% CI = 0.36, 0.68), lower limb injuries (RR = 0.51, 95% CI = 0.36, 0.74), and overuse injuries (RR = 0.43, 95% CI = 0.25, 0.75). Similarly, a program that focused on educating and training coaches to incorporate an overall-prevention mentality (consisting of improved warm-up, cool-down, taping unstable ankles, rehabilitation, promoting fair play, and a set of 10 exercises designed to improve joint stability, flexibility, strength, coordination, reaction time, and endurance) resulted in a reduction in both total injuries (0.76 ± 0.89 versus 1.18 ± 1.04, P < .01) and overuse injuries (0.26 ± 0.48 versus 0.44 ± 0.65, P < .05) per player-year.35 Specific to physically active adolescents, a 6-month, home-based balance-training program resulted in improvements in both static and dynamic balance among program participants.34 However, because of the limited number of injuries reported, no conclusions regarding the effectiveness of the program on reducing injuries could be drawn. Still, a clinically important difference was noted in self-reported injuries: program participants reported 3 (95% CI = 5, 35) injuries per 100 adolescents, compared with 17 (95% CI = 3, 24) in the control groups. Interestingly, the program was more effective in reducing injuries among those adolescents who reported sustaining an injury in the previous year,90 thus highlighting the need to identify injury history through a thorough PPE. In general, programs that are successful in reducing the risk of overuse injuries among pediatric athletes seem to include strengthening, neuromuscular control, flexibility exercises, balance, and technique training.
Delayed Specialization
One of the more controversial areas with respect to pediatric overuse injuries deals with the early specialization of athletes participating in the same sport year-round from a young age. Although little evidence-based research demonstrates that this practice has negative consequences on physical growth or psychological outcomes, many clinicians and health care organizations have advocated for diversity in sport participation or delayed specialization.5,9,91,92,93 It is theorized that participation in only 1 sport can result in increased risk for repetitive microtrauma and overuse5 or that multisport athletes who do not obtain adequate rest between daily activities or between seasons and those who participate in 2 or more sports that emphasize the same body part are at higher risk for overuse injuries than those in multiple sports with different emphases.31
Young athletes who participate in a variety of sports tend to have fewer injuries and play longer, thereby maintaining a higher level of physical activity than those who specialize before puberty.92 In addition to the potential for repetitive microtrauma and overuse injury, specialization in 1 sport may be associated with nutritional and sleep inadequacies, psychological or socialization issues, and ultimately burnout. These problems might be avoided with a balanced lifestyle and a strong support system made up of parents, friends, coaches, and health care providers.12
CONCLUSIONS
The major objective in managing repetitive or training injuries in athletes of any age should be to determine risk factors for injury and identify steps to prevent the occurrence of these injuries. Knowledge is growing about risk factors for the occurrence of both acute traumatic injuries and repetitive microtrauma overuse injuries in adults, particularly in such activities as military training, work activities, and sports. However, too little is known about risk factors for overuse injury in pediatric athletes.
Injury surveillance in young athletes should be improved to record the occurrence of injury and the determination of associated risk factors, as well as epidemiologic data (eg, age, sex, height, mass, and, if possible, Tanner stage). Epidemiologic studies in specific environments in pediatric populations would add greatly to the understanding of the risk associated with particular sport activities, thus providing a foundation for future studies of prevention and treatment efficacy.
Acknowledgments
We gratefully acknowledge the efforts of Michael C. Koester, MD, ATC; Laura Purcell, MD; Angela Smith, MD; and the Pronouncements Committee in the preparation of this document.
DISCLAIMER
The NATA publishes its position statements as a service to promote the awareness of certain issues to its members. The information contained in the position statement is neither exhaustive not exclusive to all circumstances or individuals. Variables such as institutional human resource guidelines, state or federal statutes, rules, or regulations, as well as regional environmental conditions, may impact the relevance and implementation of these recommendations. The NATA advises its members and others to carefully and independently consider each of the recommendations (including the applicability of same to any particular circumstance or individual). The position statement should not be relied upon as an independent basis for care but rather as a resource available to NATA members or others. Moreover, no opinion is expressed herein regarding the quality of care that adheres to or differs from NATA's position statements. The NATA reserves the right to rescind or modify its position statements at any time.
Appendix A.
Little League Pitch Count Tracker. Form provided by Little League International, Williamsport, PA.
Appendix B.
Little League Pitcher Eligibility Tracker. Form provided by Little League International, Williamsport, PA.
REFERENCES
- 1.Watkins J., Peabody P. Sports injuries in children and adolescents treated at a sports injury clinic. J Sports Med Phys Fitness. 1996;36(1):43–48. [PubMed] [Google Scholar]
- 2.Dubravcic-Simunjak S., Pecina M., Kuipers H., Moran J., Haspl M. The incidence of injuries in elite junior figure skaters. Am J Sports Med. 2003;31(4):511–517. doi: 10.1177/03635465030310040601. [DOI] [PubMed] [Google Scholar]
- 3.Patel D. R., Nelson T. L. Sports injuries in adolescents. Med Clin North Am. 2000;84(4):983–1007, viii. doi: 10.1016/s0025-7125(05)70270-4. [DOI] [PubMed] [Google Scholar]
- 4.Stanitski C. L. Management of sports injuries in children and adolescents. Orthop Clin North Am. 1988;19(4):689–698. [PubMed] [Google Scholar]
- 5.American College of Sports Medicine. Current comment from the American College of Sports Medicine: the prevention of sport injuries of children and adolescents. Med Sci Sports Exerc. 1993;25(8 suppl):1–7. [PubMed] [Google Scholar]
- 6.Dalton S. E. Overuse injuries in adolescent athletes. Sports Med. 1992;13(1):58–70. doi: 10.2165/00007256-199213010-00006. [DOI] [PubMed] [Google Scholar]
- 7.Cassas K. J., Cassettari-Wayhs A. Childhood and adolescent sports-related overuse injuries. Am Fam Physician. 2006;73(6):1014–1022. [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics. Injuries in youth soccer: a subject review. Committee on Sports Medicine and Fitness. Pediatrics. 2000;105(3, pt 1):659–661. [PubMed] [Google Scholar]
- 9.DiFiori J. P. Overuse injuries in young athletes: an overview. Athl Ther Today. 2002;7(6):25. [Google Scholar]
- 10.Lysens R. J., Ostyn M. S., VandenAuweele Y., Lefevre J., Vuylsteke M., Renson L. The accident-prone and overuse-prone profiles of the young athlete. Am J Sports Med. 1989;17(5):612–619. doi: 10.1177/036354658901700504. [DOI] [PubMed] [Google Scholar]
- 11.Behrman R. E., Kliegman R., Nelson W. E. Nelson Textbook of Pediatrics. 15th ed. Philadelphia, PA:: WB Saunders; 1996. [Google Scholar]
- 12.Mountjoy M., Armstrong N., Bizzini L., et al. IOC consensus statement on training the elite child athlete. Clin J Sport Med. 2008;18(2):122–123. doi: 10.1097/JSM.0b013e318168e6ea. [DOI] [PubMed] [Google Scholar]
- 13.Federation Internationale de Medecine du Sport/World Health Organization Ad Hoc Committee on Sports and Children. Sports and children: consensus statement on organized sports for children. Bull World Health Organ. 1998;76(5):445–447. [PMC free article] [PubMed] [Google Scholar]
- 14.Almquist J., Valovich McLeod T. C., Cavanna A., et al. Summary statement: appropriate medical care for the secondary school-aged athlete. J Athl Train. 2008;43(4):416–427. doi: 10.4085/1062-6050-43.4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hergenroeder A. C. Prevention of sports injuries. Pediatrics. 1998;101(6):1057–1063. doi: 10.1542/peds.101.6.1057. [DOI] [PubMed] [Google Scholar]
- 16.Caine D., DiFiori J., Maffulli N. Physeal injuries in children's and youth sports: reasons for concern? Br J Sports Med. 2006;40(9):749–760. doi: 10.1136/bjsm.2005.017822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Preparticipation Physical Evaluation Working Group. Preparticipation Physical Evaluation. 4th ed. Grove Village, IL:: American Academy of Pediatrics; 2010. [Google Scholar]
- 18.Lyman S., Fleisig G. S., Waterbor J. W., et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33(11):1803–1810. doi: 10.1097/00005768-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Olsen S. J., 2nd, Fleisig G. S., Dun S., Loftice J., Andrews J. R. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34(6):905–912. doi: 10.1177/0363546505284188. [DOI] [PubMed] [Google Scholar]
- 20.Lyman S., Fleisig G. S., Andrews J. R., Osinski E. D. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30(4):463–468. doi: 10.1177/03635465020300040201. [DOI] [PubMed] [Google Scholar]
- 21.Andrews J. R., Fleisig G. How many pitches should I allow my child to throw? USA Baseball News. April 1996. p. 5.
- 22.Klemp P., Stevens J. E., Isaacs S. A hypermobility study in ballet dancers. J Rheumatol. 1984;11(5):692–696. [PubMed] [Google Scholar]
- 23.Acasuso Diaz M., Collantes Estevez E., Sanchez Guijo P. Joint hyperlaxity and musculoligamentous lesions: study of a population of homogeneous age, sex and physical exertion. Br J Rheumatol. 1993;32(2):120–122. doi: 10.1093/rheumatology/32.2.120. [DOI] [PubMed] [Google Scholar]
- 24.Gedalia A., Press J. Articular symptoms in hypermobile schoolchildren: a prospective study. J Pediatr. 1991;119(6):944–946. doi: 10.1016/s0022-3476(05)83051-3. [DOI] [PubMed] [Google Scholar]
- 25.Hodson A. Too much too soon? The risk of “overuse” injuries in young football players. J Bodyw Mov Ther. 1999;3(2):85–91. [Google Scholar]
- 26.Ransone J., Dunn-Bennett L. R. Assessment of first-aid knowledge and decision making of high school athletic coaches. J Athl Train. 1999;34(3):267–271. [PMC free article] [PubMed] [Google Scholar]
- 27.Valovich McLeod T. C., McGaugh J. W., Boquiren M. L., Bay R. C. Youth sports coaches do not have adequate knowledge regarding first-aid and injury prevention. Appl Res Coach Athlet Ann. 2008;23:130–146. [Google Scholar]
- 28.Carson W. G., Jr, Gasser S. I. Little Leaguer's shoulder: a report of 23 cases. Am J Sports Med. 1998;26(4):575–580. doi: 10.1177/03635465980260041901. [DOI] [PubMed] [Google Scholar]
- 29.Ohta-Fukushima M., Mutoh Y., Takasugi S., Iwata H., Ishii S. Characteristics of stress fractures in young athletes under 20 years. J Sports Med Phys Fitness. 2002;42(2):198–206. [PubMed] [Google Scholar]
- 30.Loud K. J., Gordon C. M., Micheli L. J., Field A. E. Correlates of stress fractures among preadolescent and adolescent girls. Pediatrics. 2005;115(4):e399–e406. doi: 10.1542/peds.2004-1868. [DOI] [PubMed] [Google Scholar]
- 31.Brenner J. S. American Academy of Pediatrics Council on Sports Medicine and Fitness. Overuse injuries, overtraining, and burnout in child adolescent athletes. Pediatrics. 2007;119(6):1242–1245. doi: 10.1542/peds.2007-0887. [DOI] [PubMed] [Google Scholar]
- 32.Benjamin H. J., Briner W. W., Jr Little league elbow. Clin J Sport Med. 2005;15(1):37–40. doi: 10.1097/00042752-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 33.American Sports Medicine Institute. Factors related to arm pain in youth baseball pitchers. http://www.asmi.org/asmiweb/research/youthbaseball.htm. Accessed February 21, 2009.
- 34.Emery C. A., Cassidy J. D., Klassen T. P., Rosychuk R. J., Rowe B. H. Effectiveness of a home-based balance-training program in reducing sports-related injuries among healthy adolescents: a cluster randomized controlled trial. CMAJ. 2005;172(6):749–754. doi: 10.1503/cmaj.1040805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Junge A., Rosch D., Peterson L., Graf-Baumann T., Dvorak J. Prevention of soccer injuries: a prospective intervention study in youth amateur players. Am J Sports Med. 2002;30(5):652–659. doi: 10.1177/03635465020300050401. [DOI] [PubMed] [Google Scholar]
- 36.Olsen O. E., Myklebust G., Engebretsen L., Holme I., Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Flynn J. M., Lou J. E., Ganley T. J. Prevention of sports injuries in children. Curr Opin Pediatr. 2002;14(6):719–722. doi: 10.1097/00008480-200212000-00015. [DOI] [PubMed] [Google Scholar]
- 38.Faigenbaum A. D., Micheli L. J. Preseason conditioning for the preadolescent athlete. Pediatr Ann. 2000;29(3):156–161. doi: 10.3928/0090-4481-20000301-08. [DOI] [PubMed] [Google Scholar]
- 39.Micheli L. J., Fehlandt A. F., Jr Overuse injuries to tendons and apophyses in children and adolescents. Clin Sports Med. 1992;11(4):713–726. [PubMed] [Google Scholar]
- 40.Gerrard D. F. Overuse injury and growing bones: the young athlete at risk. Br J Sports Med. 1993;27(1):14–18. doi: 10.1136/bjsm.27.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Outerbridge A. R., Micheli L. J. Overuse injuries in the young athlete. Clin Sports Med. 1995;14(3):503–516. [PubMed] [Google Scholar]
- 42.Stubbs M. J., Field L. D., Savoie F. H., 3rd Osteochondritis dissecans of the elbow. Clin Sports Med. 2001;20(1):1–9. doi: 10.1016/s0278-5919(05)70243-x. [DOI] [PubMed] [Google Scholar]
- 43.Kocher M. S., Tucker R., Ganley T. J., Flynn J. M. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34(7):1181–1191. doi: 10.1177/0363546506290127. [DOI] [PubMed] [Google Scholar]
- 44.Twyman R. S., Desai K., Aichroth P. M. Osteochondritis dissecans of the knee: a long-term study. J Bone Joint Surg Br. 1991;73(3):461–464. doi: 10.1302/0301-620X.73B3.1670450. [DOI] [PubMed] [Google Scholar]
- 45.Caine D., Howe W., Ross W., Bergman G. Does repetitive physical loading inhibit radial growth in female gymnasts? Clin J Sport Med. 1997;7(4):302–308. doi: 10.1097/00042752-199710000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Iwamoto J., Takeda T. Stress fractures in athletes: review of 196 cases. J Orthop Sci. 2003;8(3):273–278. doi: 10.1007/s10776-002-0632-5. [DOI] [PubMed] [Google Scholar]
- 47.Niemeyer P., Weinberg A., Schmitt H., Kreuz P. C., Ewerbeck V., Kasten P. Stress fractures in the juvenile skeletal system. Intl J Sports Med. 2006;27(3):242–249. doi: 10.1055/s-2005-865649. [DOI] [PubMed] [Google Scholar]
- 48.Fernandez W. G., Yard E. E., Comstock R. D. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14(7):641–645. doi: 10.1197/j.aem.2007.03.1354. [DOI] [PubMed] [Google Scholar]
- 49.Maffulli N., Chan D., Aldridge M. J. Overuse injuries of the olecranon in young gymnasts. J Bone Joint Surg Br. 1992;74(2):305–308. doi: 10.1302/0301-620X.74B2.1544975. [DOI] [PubMed] [Google Scholar]
- 50.Froholdt A., Olsen O. E., Bahr R. Low risk of injuries among children playing organized soccer: a prospective cohort study. Am J Sports Med. 2009;37(6):1155–1160. doi: 10.1177/0363546508330132. [DOI] [PubMed] [Google Scholar]
- 51.Le Gall F., Carling C., Reilly T., Vandewalle H., Church J., Rochcongar P. Incidence of injuries in elite French youth soccer players: a 10-season study. Am J Sports Med. 2006;34(6):928–938. doi: 10.1177/0363546505283271. [DOI] [PubMed] [Google Scholar]
- 52.Le Gall F., Carling C., Reilly T. Injuries in young elite female soccer players: an 8-season prospective study. Am J Sports Med. 2008;36(2):276–284. doi: 10.1177/0363546507307866. [DOI] [PubMed] [Google Scholar]
- 53.National Federation of State High School Associations. 2009–2010 high school athletics participation survey. http://www.nfhs.org/content.aspx?id=3282&linkidentifier=id&itemid=3282. Accessed October 7, 2010.
- 54.Pearce P. Z. Prehabilitation: preparing young athletes for sports. Curr Sports Med Rep. 2006;5(3):155–160. doi: 10.1007/s11932-006-0019-y. [DOI] [PubMed] [Google Scholar]
- 55.Hirth C. Clinical movement analysis to identify muscle imbalances and guide exercise. Athl Ther Today. 2007;12(4):10–14. [Google Scholar]
- 56.Kiesel K., Plisky P. J., Voight M. L. Can serious injury in professional football be predicted by a preseason functional movement screen. North Am J Sport Phys Ther. 2007;2(3):147–158. [PMC free article] [PubMed] [Google Scholar]
- 57.Hreljac A. Etiology, prevention, and early intervention of overuse injuries in runners: a biomechanical perspective. Phys Med Rehabil Clin N Am. 2005;16(3):651–667, vi. doi: 10.1016/j.pmr.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 58.Rausch C. M., Phillips G. C. Adherence to guidelines for cardiovascular screening in current high school preparticipation evaluation forms. J Pediatr. 2009;155(4):584–586. doi: 10.1016/j.jpeds.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 59.Krowchuk D. P., Krowchuk H. V., Hunter D. M., et al. Parents' knowledge of the purposes and content of preparticipation physical examinations. Arch Pediatr Adolesc Med. 1995;149(6):653–657. doi: 10.1001/archpedi.1995.02170190063011. [DOI] [PubMed] [Google Scholar]
- 60.Bundy D. G., Feudtner C. Preparticipation physical evaluations for high school athletes: time for a new game plan. Ambul Pediatr. 2004;4(3):260–263. doi: 10.1367/A02-110R1.1. [DOI] [PubMed] [Google Scholar]
- 61.O'Connor F. G., Howard T. M., Fieseler C. M., Nirschl R. P. Managing overuse injuries: a systematic approach. Phys Sportsmed. 1997;25(5):88–113. doi: 10.3810/psm.1997.05.1359. [DOI] [PubMed] [Google Scholar]
- 62.Bennett J. E., Reinking M. F., Pluemer B., Pentel A., Seaton M., Killian C. Factors contributing to the development of medial tibial stress syndrome in high school runners. J Orthop Sports Phys Ther. 2001;31(9):504–510. doi: 10.2519/jospt.2001.31.9.504. [DOI] [PubMed] [Google Scholar]
- 63.Plisky M. S., Rauh M. J., Heiderscheit B., Underwood F. B., Tank R. T. Medial tibial stress syndrome in high school cross-country runners: incidence and risk factors. J Orthop Sports Phys Ther. 2007;37(2):40–47. doi: 10.2519/jospt.2007.2343. [DOI] [PubMed] [Google Scholar]
- 64.Loud K. J., Micheli L. J., Bristol S., Austin S. B., Gordon C. M. Family history predicts stress fracture in active female adolescents. Pediatrics. 2007;120(2):e364–e372. doi: 10.1542/peds.2006-2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bennell K., Matheson G., Meeuwisse W., Brukner P. Risk factors for stress fractures. Sports Med. 1999;28(2):91–122. doi: 10.2165/00007256-199928020-00004. [DOI] [PubMed] [Google Scholar]
- 66.Remvig L., Jensen D. V., Ward R. C. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: review of the literature. J Rheumatol. 2007;34(4):804–809. [PubMed] [Google Scholar]
- 67.Acasuso-Diaz M., Collantes-Estevez E. Joint hypermobility in patients with fibromyalgia syndrome. Arthritis Care Res. 1998;11(1):39–42. doi: 10.1002/art.1790110107. [DOI] [PubMed] [Google Scholar]
- 68.Adib N., Davies K., Grahame R., Woo P., Murray K. J. Joint hypermobility syndrome in childhood: a not so benign multisystem disorder? Rheumatology (Oxford) 2005;44(6):744–750. doi: 10.1093/rheumatology/keh557. [DOI] [PubMed] [Google Scholar]
- 69.Arroyo I. L., Brewer E. J., Giannini E. H. Arthritis/arthralgia and hypermobility of the joints in schoolchildren. J Rheumatol. 1988;15(6):978–980. [PubMed] [Google Scholar]
- 70.Gedalia A., Person D. A., Brewer E. J., Jr, Giannini E. H. Hypermobility of the joints in juvenile episodic arthritis/arthralgia. J Pediatr. 1985;107(6):873–876. doi: 10.1016/s0022-3476(85)80178-5. [DOI] [PubMed] [Google Scholar]
- 71.Gedalia A., Press J., Klein M., Buskila D. Joint hypermobility and fibromyalgia in schoolchildren. Ann Rheum Dis. 1993;52(7):494–496. doi: 10.1136/ard.52.7.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hoppmann R. A. Instrumental musicians' hazards. Occup Med. 2001;16(4):619–631, iv–v. [PubMed] [Google Scholar]
- 73.Hudson N., Fitzcharles M. A., Cohen M., Starr M. R., Esdaile J. M. The association of soft-tissue rheumatism and hypermobility. Br J Rheumatol. 1998;37(4):382–386. doi: 10.1093/rheumatology/37.4.382. [DOI] [PubMed] [Google Scholar]
- 74.Hudson N., Starr M. R., Esdaile J. M., Fitzcharles M. A. Diagnostic associations with hypermobility in rheumatology patients. Br J Rheumatol. 1995;34(12):1157–1161. doi: 10.1093/rheumatology/34.12.1157. [DOI] [PubMed] [Google Scholar]
- 75.Ofluoglu D., Gunduz O. H., Kul-Panza E., Guven Z. Hypermobility in women with fibromyalgia syndrome. Clin Rheumatol. 2006;25(3):291–293. doi: 10.1007/s10067-005-0040-1. [DOI] [PubMed] [Google Scholar]
- 76.Smith R., Damodaran A. K., Swaminathan S., Campbell R., Barnsley L. Hypermobility and sports injuries in junior netball players. Br J Sports Med. 2005;39(9):628–631. doi: 10.1136/bjsm.2004.015271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Klemp P., Learmonth I. D. Hypermobility and injuries in a professional ballet company. Br J Sports Med. 1984;18(3):143–148. doi: 10.1136/bjsm.18.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hopper D. M., Hopper J. L., Elliott B. C. Do selected kinanthropometric and performance variables predict injuries in female netball players? J Sports Sci. 1995;13(3):213–222. doi: 10.1080/02640419508732230. [DOI] [PubMed] [Google Scholar]
- 79.Decoster L. C., Bernier J. N., Lindsay R. H., Vailas J. C. Generalized joint hypermobility and its relationship to injury patterns among NCAA lacrosse players. J Athl Train. 1999;34(2):99–105. [PMC free article] [PubMed] [Google Scholar]
- 80.Collinge R., Simmonds J. V. Hypermobility, injury rate and rehabilitation in a professional football squad: a preliminary study. Phys Ther Sport. 2009;10(3):91–96. doi: 10.1016/j.ptsp.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 81.Steele V. A., White J. A. Injury prediction in female gymnasts. Br J Sports Med. 1986;20(1):31–33. doi: 10.1136/bjsm.20.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Carter C., Wilkinson J. Persistent joint laxity and congenital dislocation of the hip. J Bone Joint Surg Br. 1964;46:40–45. [PubMed] [Google Scholar]
- 83.Beighton P., Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969;51(3):444–453. [PubMed] [Google Scholar]
- 84.Little League Baseball. Protecting young pitching arms. http://www.littleleague.org/Assets/old_assets/media/Pitch_Count_Publication_2008.pdf. Accessed October 27, 2010.
- 85.Dun S., Loftice J., Fleisig G. S., Kingsley D., Andrews J. R. A biomechanical comparison of youth baseball pitches: is the curveball potentially harmful? Am J Sports Med. 2008;36(4):686–692. doi: 10.1177/0363546507310074. [DOI] [PubMed] [Google Scholar]
- 86.Nissen C. W., Westwell M., Ounpuu S., Patel M., Solomito M., Tate J. A biomechanical comparison of the fastball and curveball in adolescent baseball pitchers. Am J Sports Med. 2009;37(8):1492–1498. doi: 10.1177/0363546509333264. [DOI] [PubMed] [Google Scholar]
- 87.USA Swimming. Foundations of Coaching. Colorado Springs, CO:: USA Swimming; 2007. Organization and administration, part 3: organizing the wet side; pp. 1–4. [Google Scholar]
- 88.Gill T. Jt, Micheli L. J. The immature athlete: common injuries and overuse syndromes of the elbow and wrist. Clin Sports Med. 1996;15(2):401–423. [PubMed] [Google Scholar]
- 89.Micheli L. J., Klein J. D. Sports injuries in children and adolescents. Br J Sports Med. 1991;25(1):6–9. doi: 10.1136/bjsm.25.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Emery C. A. Risk factors for injury in child and adolescent sport: a systematic review of the literature. Clin J Sport Med. 2003;13(4):256–268. doi: 10.1097/00042752-200307000-00011. [DOI] [PubMed] [Google Scholar]
- 91.Micheli L. J., Glassman R., Klein M. The prevention of sports injuries in children. Clin Sports Med. 2000;19(4):821–834, ix. doi: 10.1016/s0278-5919(05)70239-8. [DOI] [PubMed] [Google Scholar]
- 92.American Academy of Pediatrics Committee on Sports Medicine and Fitness. Intensive training and sports specialization in young athletes. Pediatrics. 2000;106(1, pt 1):154–157. [PubMed] [Google Scholar]
- 93.American Orthopaedic Society for Sports Medicine. Stop sports injuries. http://www.sportsmed.org/stop. Accessed December 15, 2010.