Abstract
Oncology nurses are playing an important role in the provision of survivorship care. Their involvement includes educating and coordinating multidiscipline teams to initiate and provide care to patients and families. Oncology nurses participate in this evolving model of care in a variety of ways. Using the IOM report recommendations for the provision of quality cancer care nurses provide care based on the specific characteristics of individual health care settings and the populations they serve. Evaluating the settings resources and goals for desired survivorship activities as part of the planning process can be the difference between success and failure. Collaborating with local and national resources for cancer survivors can help expand services for a setting in an efficient and cost effective manner.
Models of care vary and resources and communication differs among cancer care settings. Survivorship care differs as a result, across different models. Nurses are key to the dissemination and coordination of survivorship activities and are critical in facilitating communication between health care providers, the patients and caregivers. Nurses have a significant role in the dissemination and coordination of information between the patient and other health care providers. Oncology care does not end when treatment ends.
Introduction
Current projections from American Cancer Society predict a population of 20 million cancer survivors by 2020. (American Cancer Society (ACS)). Health care needs of this population are unique, and involve (1) specific cancer prevention and detection activities, (2) individual surveillance recommendations, (3) interventions for the consequences of cancer and cancer treatment and (4) Coordination of Care. Planning and coordinating these health care needs involves communication between patients and health providers based on individualized treatment summaries (TS) and survivorship care plans (SCP).
Oncology nurses have been instrumental in developing and integrating cancer survivorship care into current health care settings (B. R. Ferrell & Winn, 2006). One hundred and two oncology nurses have participated in the National Cancer Institute (NCI) supported program on Survivorship Education for Quality Cancer Care.(M. Grant, Economou, Ferrell, & Bhatia, 2007) Reported here are examples of oncology nurses who attended this program and are now implementing cancer survivorship care in their settings. In this report we will briefly define what is recommended for survivorship care, the content of the funded project Survivorship Education for Quality Cancer Care that included 50% nurses, and provide examples of how these nurses are implementing survivorship care in their specific cancer settings. We will conclude with recommendations for survivorship care activities for all oncology nurses. We hope this content will inspire oncology nurses to join in providing quality survivorship care for all cancer patients.
Background
The cancer survivorship movement began with the establishment of the National Coalition of Cancer Survivors (NCCS) in 1986 and the recognition of cancer survivors as a unique population. Efforts to improve survivorship care proceeded steadily and included advocacy at the national level, development of patient educational materials, and eventually establishment of the Office of Cancer Survivorship at the National Cancer Institute (NCI) in 1996. (Office of Cancer Survivorship, 2006) (Table 1) Survivorship activities in cancer settings began to increase in response to the publication of the Institute of Medicine (IOM) report, From Cancer Patient to Cancer Survivor-Lost in Transition in 2006. (Hewitt, Greenfield, & Stovall, 2006) This push for the establishment of cancer survivorship care continues as reflected in the priority for survivorship programs endorsed by the Association of Community Cancer Centers (ACCC)(Lamkin, 2002).
Table 1.
Nationals Organization Recommendations for Survivorship Care
| Agency | Report | Web site |
|---|---|---|
| American Cancer Society (ACS) |
National Action Plan for Childhood Cancer |
http://www.cancer.org/docroot/home/index.asp |
| Office of Cancer Survivorship (OCS) |
Cancer Survivorship: Moving the Science and Art of Research and Care Beyond Cure |
http://cancercontrol.cancer.gov/ocs/ |
| Center for Disease control (CDC) |
The National Action Plan |
http://www.cdc.gov/ |
| National Cancer Institute (NCI) |
Living with and Beyond Cancer |
http://www.cancer.gov/ |
| American Society of Clinical Oncology (ASCO) |
Clinical Practice Guidelines |
http://www.asco.org/ |
| Association of Community Cancer Centers (ACCC) |
Living in the Future: Cancer Survivorship Program |
http://accc-cancer.org/ |
After experiencing cancer and cancer treatment, survivors return to their former lives as different people with long lasting symptoms and risks to their future health. (Doyle, 2008) The NCCS defines a cancer survivor as someone who has been diagnosed with cancer. For this report we will use the perspective of the IOM report and others by focusing on care following completion of treatment. (Hewitt, et al., 2006) (Ganz, Casillas, & Hahn, 2008)
Survivorship Care Defined
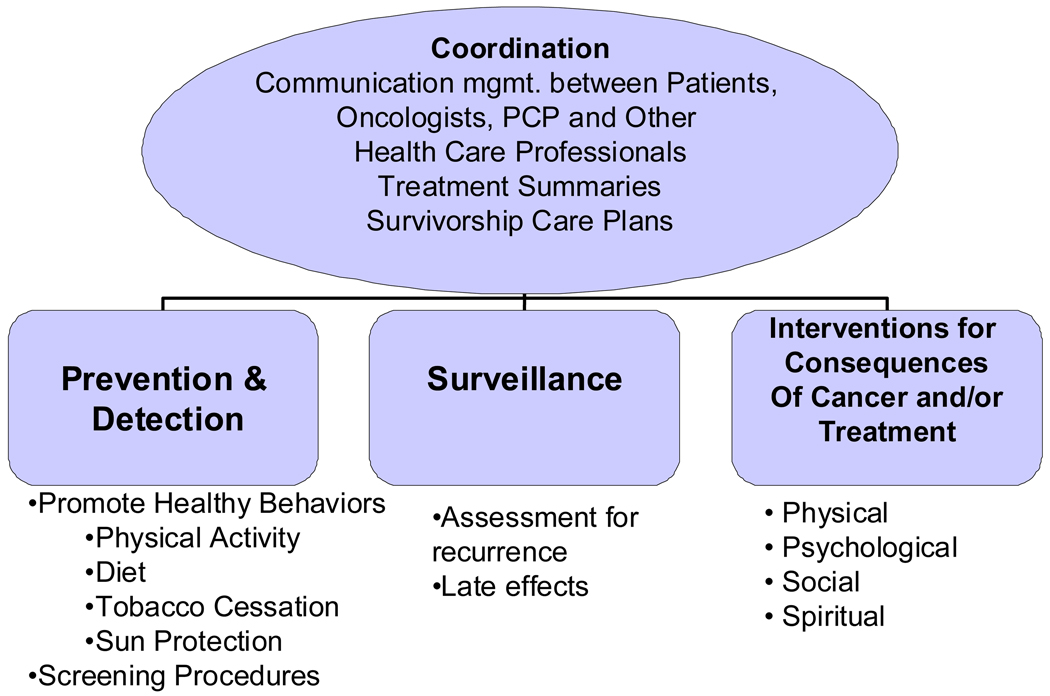
A range of activities is included in survivorship care and has been organized within the IOM report into four major components. (Figure 1). Prevention and detection is defined as the promotion of healthy living behaviors and screening for the early detection of cancer. Healthy living behaviors include a diet low in saturated fats, regular physical activity several times a week, tobacco cessation or avoidance of smokeless tobacco and protection from UV sun rays. Surveillance focuses on medical follow up care related to specific cancers or cancer treatments. Surveillance includes colonoscopy and skin examinations as well as gender specific procedures such as mammography, pap smears, PSA and prostate examinations. Interventions focus on symptom management or education for long term effects of cancer and cancer treatments. These can be organized in relation to the four domains of quality of life which include: physical, psychological, social and spiritual interventions (B.R. Ferrell, Hassey Dow, & Grant, 1995). Physical interventions include management of symptoms such as pain or lymphedema. Psychological support could include depression and stress management, or support groups. Social interventions could include managing work related problems, changes in family structure, disability or discrimination issues. Spiritual interventions includes supporting specific spiritual activities, and helping patients connect with spiritual counselors or chaplains, contacting specific religious organizations to provide spiritual guidance or special interventions requested by the patient. Patients or families may request a priest or rabbi to work through issues or other spiritual counselors as requested. (Aziz, 2007; Miller, 2008)
Figure 1. IOM Components of Survivorship Care.
Adapted from IOM Report (2006) & Aziz & Rowland (2003)
Finally, coordination of care relates to communication between the patient, oncologist and primary care physician and/or other healthcare providers. None of these previously defined activities can occur without taking into account what cancer is present and which cancer treatment a specific patient received. The primary tools used to provide this coordination include the Treatment Summary (TS) and Survivorship Care Plan (SCP). The TS records the specific cancer treatment an individual patient has received and provides the information needed to develop a personalized survivorship care plan. TS’s describe surgical procedures performed, documents the chemotherapy received including dose and number of courses, and identifies the amount of radiation received and specific fields involved. Any important events that occur during treatment are also recorded on the TS.
The SCP is based on the TS and specifies exactly what the individual patient should do in relation to prevention and detection, surveillance, and interventions. This document should include when follow up should occur and individualized recommendations. For example it should include dates for follow up tests, what are the expected effects such as lymphedema and how they should be treated, when late effects such as cardiac toxicity should be evaluated. Because TS and SCP’s are complex documents that require time and effort by educated personal, templates for developing personalized patient documents have been developed. The Lance Armstrong Foundation has combined with Oncolink at the University of Pennsylvania to develop the LIVESTRONG CarePlan as one of the two current electronically available care plan building sites. (LIVESTRONG Care Plan) This program links through Oncolink and Oncopilot to help keep track of treatments. The care plan building program is directed towards adult cancer survivors. Journeyforward.org is the second program created by collaboration among the National Coalition for Cancer Survivorship (NCCS), UCLA Cancer Survivorship Center at the Jonsson Comprehensive Cancer Center, WellPoint, Inc. and Genentech. These templates include American Society of Clinical Oncologists (ASCO) treatment summary templates and surveillance guidelines. Survivorship resources are listed in Table 2. The information in the TS and SCP can impact future health for each patient. Providing the TS and SCP to all providers and the patient ensures personalized survivorship care.
Table 2.
Models for Delivering Survivorship Care
| Type of Setting |
NCI-designated Cancer Centers/ Academic Institutions |
Free Standing NCI-designated Cancer Settings |
Community Cancer Programs |
Ambulatory Care Settings |
|---|---|---|---|---|
|
Population Served |
Adult & Pediatric | Adult & Pediatric | Adults Only | |
|
Disciplines included |
Large multidiscipline medical centers |
Multidiscipline Support Services Available |
Limited Support services (Psychosocial, Dietician, PT) |
Limited Support Services (Psychosocial, Dietician, PT) |
| Settings | In-Patient & Out- Patient |
In-Patient & Out- Patient Cancer Tx. Only |
In-Patient & Out- Patient |
Out-Patient Only |
|
Academic Training Y/N |
Yes | Yes Outreach for Academic Residency Programs |
No May be outreach site for Academic Residency Programs |
No |
|
Depend on Community Resources |
Sometimes | Sometimes | Yes | Yes |
|
Grant Funded Research Y/N |
Yes | Yes | Sometimes | Sometimes |
| Innovation | Research Focused Multidiscipline Programs |
Oncology Only Focus |
Community Resources Limited Disciplines |
Community Resources Limited Disciplines |
| Leadership | MD Shared Care Nurse-Led F/U Programs |
MD Shared Care Nurse-Led F/U Programs |
Staff share responsibilities Refer to community resources as needed |
Nurse led activities coordinated with local community resources |
|
Setting Examples |
• UMICH • UCLA • UPENN • Dartmouth |
• MSKCC • Fox chase • City of Hope |
• Pearlman CC • Sanford CC |
• Dayton Physicians, Hematology & Oncology |
In summary, survivorship care encompasses a broad spectrum of activities from prevention and surveillance to treatment of specific long term and late effects. Coordination of this care includes an individualized treatment summary and a care planning process that addresses future health care needs. Activities in this area are important for our entire population, as well as cancer survivors, and include many activities already provided within cancer and non-cancer health facilities.
Survivorship Education for Quality Care
An NCI grant funded research educational program, “Survivorship Education for Quality Cancer Care” provided 3-day survivorship education via four annual workshops held at the City of Hope, to 204 two-person multidiscipline teams from across the nation. (M. Grant, Economou, D., 2007) The primary aim of the program was to improve quality of care, and quality of life for cancer survivors. The teams were composed of an MD, RN, Administrator or SW as one member and another professional for the second member. Each team developed three goals to be implemented when they returned to their setting. Follow-up evaluations were done with each individual team and included goal achievement, telephone interviews, an Institutional Assessment and an Institutional Survey at 6, 12, and 18 months post course. The information gained from these different teams describes nursing promotion of survivorship care at many different levels to cancer survivor populations. Examples from each of the cancer settings will illustrate how care is integrated into the standards of care by oncology nurses practicing in a variety of settings.
Settings and Examples of Survivorship Care
Models for delivering survivorship programs are evolving and are related to the type of setting, staffing resources and survivor populations served. (Haylock, 2007; Oeffinger & McCabe, 2006) The size of the institution, number of cancer patients served, kinds of cancers treated, availability of institutional and community resources are characteristics that influence the services that can be provided. For this report we divided health care settings into four categories. (Table 2)
NCI-designated Cancer Centers within Academic Institutions
These large multidisciplinary medical centers including academic training for health professionals, adult and/or pediatric programs, and multiple out-patient clinics, services and research programs. These settings generally address all diseases as well as conduct basic and clinical research. They provide multiple medicine, surgical and oncology clinics and may have nurse-led follow-up clinics and supportive care programs. Developing separate survivorship follow-up clinics may fit within this multiple clinic set up, and be designed as disease-specific clinics that provide survivorship education and follow-up care. Accessibility of multiple disciplines and expanded medical records provide the information needed for TS’s and SCP’s. Examples of academic settings whose teams attended Survivorship Education for Quality Cancer Care include University of Michigan, University of California, Los Angeles (UCLA) and the University of Pennsylvania (UPENN) and Norris Cotton Cancer Center at Dartmouth.
The University of Michigan Comprehensive Cancer Center team included an Administrator RN, PhD and a nurse practitioner (NP) who were Co-Directors of the Center for Cancer Survivorship. Following the CoH course they held focus groups to identify cancer survivors’ needs. This resulted in a course entitled, “Preparing for Life as a New Survivor”. They also developed a research infrastructure within the cancer survivorship program to support areas of research in cancer survivorship. Their initial focus was on the pediatric, prostate, and breast cancer populations. Focus groups were held to identify cancer survivors’ needs and resulted in a course entitled, “Preparing for Life as a New Survivor”.
UCLA’s team included an MD director of the Childhood Cancer Survivors Mattel Children’s Hospital long-term follow-up clinic and an RN, NP for the UCLA LIVESTRONG Survivorship Center of Excellence program. Following the CoH course they developed templates for their childhood cancer survivorship program and transitioning pediatric to adult survivors using the Children’s Oncology Group survivorship guidelines. These guidelines were then used to educate providers and adult childhood cancer survivors regarding treatment history and risk for late effects. In addition, they established a follow up symptom management clinic for survivors led by the nurse practitioner. The UCLA team was instrumental in the development of the Journey Forward survivorship care plan template. http://www.journeyforward.org/
UPENN’s team included a PhD nurse, who is the director of survivorship research for the LIVESTRONG Survivorship Center of Excellence at the Abramson Cancer Center and an NP who is the survivorship project manager. Following the CoH course they 1) integrated cancer TS’s into the breast cancer clinical practices, 2) developed an educational initiative for clinicians to raise awareness and knowledge of survivorship issues and 3) developed an infrastructure and resources to organize the PENN Cancer Network Hospitals for community based outreach survivorship programs. TS’s for breast cancer patients were created with the Oncolink template, which later with the collaboration of the LAF transitioned into the LIVESTRONGCarePlan.org site. As a team they also provided education to NPs in the network hospitals on survivorship care and on the use of electronic care plans. UPENN’s team also developed an educational program to provide primary care physicians with survivorship education. As part of their LIVESTRONG Center of Excellence requirements UPENN supports outreach programs in the community. They have assisted their affiliate hospital in conducting breast cancer survivor needs assessment and subsequently providing an educational program to its cancer survivors. In partnership with the Lance Armstrong Foundation (LAF) they piloted the new LIVESTRONG Care Plan and assisted two of their outreach hospital programs in integrating the treatment summaries and survivorship care plans into their breast cancer practices.
The team from Norris Cotton Cancer Center at Dartmouth Hitchcock Medical Center consisted of two NPs. They completed a patient survivor needs assessment and compiled the results for presentation to the Cancer Steering Committee for administrative support and implementation. Using that approach, they gained administrative support and defined the infrastructure needed for the planned APN led clinic. Next they identified available resources and submitted three grant applications for 10% salary support for each APN in the clinic. Future plans include applying for philanthropic grant money to help support their NP’s clinics.
Free Standing NCI-designated Cancer Settings
are only focused on cancer care and generally have both in-patient and ambulatory patient services. Resources for cancer patients are broadly provided, including support groups, educational materials, and multidisciplinary support. Within these settings, disease-specific clinics for cancer survivors are developing; and often are run by Nurse Practitioners (NP’s). A component less frequently found in these settings is medical expertise for non-cancer complications, such as cardiac complications related to chemotherapy toxicity. An example of a free standing cancer center is Memorial Sloan Kettering Cancer Center (MSKCC).
One of the three teams that have attended from Memorial Sloan Kettering Cancer Center (MSKCC) included an NP and Program Coordinator who have worked together as part of the survivorship services provided by MSKCC. Survivorship activities included providing a TS to patients in the survivorship program and by also mailing the same information to their community physicians to facilitate coordination of care across settings. In addition, they adapted the children’s oncology group guidelines to transition those grown pediatric patients to the adult clinic. A unique piece in the MSKCC Survivorship Program is the survivor newsletter. With the support of a volunteer survivor who was an editor, the Survivor program coordinator produces a newsletter, Bridges- Connecting Cancer Survivors. This newsletter is mailed to all survivors and serves as a sounding board for survivors to discuss their experiences and has been an important asset for patients and families. To gather information, survivors are asked to visit www.mskcc.org/bridges to submit their personal cancer stories.
Community Cancer Programs
are found in both large and small community hospitals. They provide both in-patient and out-patient care to patients and may include a designated oncology center or unit. Survivorship care in these hospitals is usually provided in the out-patient or rehabilitation departments. These institutions frequently do not provide academic training or multiple in-house specialty services and may or may not include a pediatric department. Community programs may have limited psychosocial, rehabilitation and dietary resources. Their specific services are generally related to the expertise of their staff. They may provide or coordinate to specific supportive services such as support groups and cancer rehabilitation. Providing TS’s or SCP’s is more difficult in these settings. Smaller community cancer programs have limited financial support to build specific survivorship programs and provide resources. One approach used is to collaborate with local or national community resources in an effort to provide supportive services to cancer survivors. In community cancer programs Oncologists and Primary Care Physicians (PCP) share care of a cancer survivor. Private foundations such as Lance Armstrong Foundation (LAF), the American Cancer Society (ACS) and, Cancer Care can provide survivorship services and resources to settings and families and can be especially valuable in smaller community and rural settings. Nurses can refer patients to on-line and telephone support groups and educational sessions. ACS resources for prevention and detection education and health promotion programs are resources that are available to patients, caregivers and families. (Table 3)
Table 3.
Survivorship Resource Web Sites
| Source | Resources Available | Web Site |
|---|---|---|
| CancerCare | Survivorship Support Groups and Educational Resources |
http://cancercare.org |
|
American Cancer Society |
Educational Resources Professional,Patient, Caregivers and Families |
http://www.cancer.org |
|
National Coalition for Cancer Survivorship (NCCS) |
Survivorship education for Patient, Professional and Caregiver Cancer Survival Toolbox Cancer Advocacy Now Everyday Heros |
www.advocacy@canceradvocacy.org |
| Medicine(IOM), Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. 2007, The National Academies Press: Washington DC. |
Survivorship education and resources for Psychosocial support of cancer survivors. |
http://books.nap.edu/openbook.php?record_id=11993 |
|
Lance Armstrong Foundation/ LIVESTRONG Program |
Survivorship education and resources. LIVESTRONG Care Plan Template |
http://www.livestrong.org organizations: www.livestrong.org/communitytoolkit www.livestrongcareplan.org |
|
Journey Forward Care Plan |
Survivorship education and resources and Care Plan Template |
www.journeyforward.org |
|
City of Hope Pain & Palliative Care Resource Center |
Educational Resources and evaluation tools. |
http://prc.coh.org |
Examples of community cancer programs implementing survivorship activities are Pearlman Cancer Center at South Georgia Medical Center and Sanford Cancer Center Oncology Clinic in Sioux Falls, SD. The team at Pearlman Cancer Center at South Georgia Medical Center involved two nurses. They began with creating a timeline for implementation of a comprehensive survivorship program at their institution, they were also part of a larger State collaboration with the NCI Community Cancer Centers Program (NCCCP). So part of their activities included helping to coordinate survivorship programs from a state wide perspective. That collaboration led to the development of an SCP template for breast cancer patients and refinement of a cancer survivors’ needs assessment tool that had been developed by the Cancer Education Program at Mayo Clinic Cancer Center. This needs assessment tool helped them identify and develop the survivorship components of care they would provide at their institution. The needs assessment can be obtained through the City of Hope PRC web site http://prc.coh.org.
The team at Sanford Cancer Center Oncology Clinic in Sioux Falls, SD consisted of an NP and an Administrator. Their survivorship activities included educational and psychosocial programs to the survivorship population in their community. They developed an educational program called “Journey to Cancer Wellness” that also directed survivors to local psychosocial support services. Next they developed a series of educational sessions: 1) Cancer Corrections that focused on healthy lifestyle changes and exercise, and 2) Cancer Kickers Support Group designed to help patients and families cope with daily issues surrounding their cancer diagnosis. Exercise and yoga classes already available were expanded to support the needs of survivors and reduce stress. Future plans include a follow up clinic but await hiring a full time physician to lead the program.
Ambulatory Care Settings
These settings include large and small free-standing physician office practices that may provide infusion services and possibly radiation services but have limited supportive services for psychosocial care, physical therapy or dietary support. Staffing for survivorship clinics for follow up care is usually non-existent and collaboration with local and national resources are often used to provide psychosocial support. Providing TS or SCP in these settings is challenging and requires considerable additional staff and physician support. Acute clinical treatment takes priority, thus, using resources from the community is essential. An example of an ambulatory care setting is Dayton Physicians, Hematology & Oncology, in Dayton, Ohio. The NP and RN Clinical Educator team from this setting focused on finalizing a template for TS and SCP documentation in their setting. They began using The Lance Armstrong Survivorship handouts (e.g. Patient Notebooks) and a locally developed patient resource guide which they provided to all patients at the completion of treatment to introduce the concept of survivorship from the time of diagnosis. They then focused on educating their staff about survivorship issues to build an awareness of survivorship care and presented in-services on survivorship needs and issues to the medical and radiation oncology office staff. Reaching out to the greater community, these nurses also provided education on survivorship care at their local Oncology Nursing Society chapter meetings. This team has also been asked to participate with a local hospital-based task force on survivorship care. They are planning to collaborate with this hospital for breast cancer survivor specific programs. The team’s biggest barrier continues to be physician support when time is taken away from acute patient care. In an effort to start exploring how TS and SCP’s could be developed, they are evaluating existing templates from LIVESTRONG and Journey Forward. (LIVESTRONG Care Plan; The Journey Forward Care Plan Builder)
To summarize, nurses across settings from large academic NCI-Comprehensive Cancer Settings to small ambulatory clinics, nurses are able to initiate and implement many survivorship care activities. The most common activities appear to be related to providing interventions for cancer and cancer treatment long term effects such as symptom management and psychosocial support. The most challenging activities across all settings are the development and distribution of individualized TS and SCP’s. Staffing and treatment priorities are the biggest barriers to overcome in developing these documents and distributing them to patients, oncologists and primary care physicians. The least frequent activity in our examples is prevention and surveillance activities, which are not traditionally found in cancer settings. Providing the many components of survivorship care to the ever increasing population of cancer survivors will continue to be a challenge.
Practice Implementation for Oncology Nurses
How nurses integrate survivorship care into their current position and practice setting requires first assessing the setting and the cancer populations served. In assessing the setting, one approach to use would be to identify resources for survivorship care already available at the institution. This could be organized under the four components of care found in Figure 1.
For prevention, do patients have access to screening procedures and if not, where are they referred to? Is there anyone in the setting that could address healthy living recommendations, either in written material or educational groups?
For Surveillance, are patients referred for routine follow up evaluations specific to their cancer? For example, are MRIs required for specific diseases, and who does this scheduling? Are patients taught what to look for and when to contact their PCP or Oncologist?
For Interventions, a whole range of activities are relevant. Are there existing support groups for specific cancer diagnoses, and could those provide time for an educational session on survivorship issues? Are there clinics that can take care of long term effects, such as pain management, lymphedema? Is there a way to provide the Survivor Toolkit from the National Coalition of Cancer Survivors to every patient who completes treatment? Are there survivorship activities in the community that survivors could be referred to? Providing CancerCare Calendar of programs and other outside resources can be an efficient way to expand your settings services. (Table 3)
For Coordination and Communication, what system is currently used for recording patient data? Is there an electronic medical record? Is it possible to begin filling in a treatment summary with all new patients? Is there a group of interested professional staff that could examine the templates currently available for TS and SCP’s and evaluate whether one or the other might be what fits best within their setting?
A few resources are available that can help with these initial questions. (Table 4) A needs survey for cancer patients can be used to identify specific needs of specific populations, e.g. breast cancer survivors. Once this information is gathered, initial activities can focus on resources currently available that can be adapted or expanded to include survivors and educational materials already available that can be distributed as patient’s complete treatment. Further development may depend on resources to provide staffing and identification of priorities within an institution. Armed with the above information, oncology nurses can provide valuable information in building a survivorship programs or incorporating survivorship focused activities within the institution or setting.
Table 4.
Assessing a Setting for Survivorship Care
| 1. Is your staff informed about survivorship issues related to cancer care? |
| 2. Are there champions of care who will support and participate in survivorship services in your setting? |
| 3. What are the 5 largest disease populations you see in your setting? |
| 4. What are the needs or deficits in their care? |
| 5. What services does your setting currently offer for patient support during treatment? |
| 6. Who are the people in your setting that provide these services? |
| 7. What community resources are available to meet survivors’ needs? |
| 8. Do you have any relationships with these community resources? |
| 9. Examine the services offered in your setting and expand them to include components of survivorship care. (Prevention, detection, surveillance, interventions and coordination |
In summary, cancer survivors are a growing population, and need care beyond the end of treatment. Survivorship care falls within four major areas: prevention, surveillance, interventions, and coordination. Examples from the course on Survivorship Education for Quality Cancer Care provides information on how nurses from various settings who attended this course have begun to integrate survivorship activities into their individual settings. Nurses can play a significant role in helping to disseminate and coordinate information, connect with community resources, spearhead survivorship activities within their own settings, and provide public and professional education on survivorship care. The role of the oncology nurse has traditionally been to coordinate care during treatment. That role needs to expand to include a focus beyond treatment to the needs of the cancer survivor.
Acknowledgments
Grant Supported
NCI 1-R25CA 107109 Survivorship Education for Quality Cancer Care
References
- American Cancer Society (ACS) [Retrieved 3-18-10, 2010]; from www.cancer.org.
- Aziz NM, editor. Late Effects of Cancer Treatment. Springer; 2007. [Google Scholar]
- Bloom BS. Taxonomy of Educational Objectives, Handbook I; The Cognitive Domain. New York: David McKay Co Inc.; 1956. [Google Scholar]
- Caffarella R. Planning Programs for Adult Learners: A Practical Guide for Educators, Trainers, and Staff Developers. Vol. 2e. San Francisco: Jossey-Bass, A Wiley Company; 2002. [Google Scholar]
- Doyle N. Cancer survivorship: evolutionary concept analysis. J Adv Nurs. 2008;62(4):499–509. doi: 10.1111/j.1365-2648.2008.04617.x. [DOI] [PubMed] [Google Scholar]
- Ferrell BR, Hassey Dow K, Grant M. Measurement of the quality of life in cancer survivors. Quality of Life Research. 1995;4:523–531. doi: 10.1007/BF00634747. [DOI] [PubMed] [Google Scholar]
- Ferrell BR, Winn R. Medical and nursing education and training opportunities to improve survivorship care. J Clin Oncol. 2006;24(32):5142–5148. doi: 10.1200/JCO.2006.06.0970. [DOI] [PubMed] [Google Scholar]
- Ganz PA, Casillas J, Hahn EE. Ensuring quality care for cancer survivors: implementing the survivorship care plan. Semin Oncol Nurs. 2008;24(3):208–217. doi: 10.1016/j.soncn.2008.05.009. [DOI] [PubMed] [Google Scholar]
- Grant M, Economou D, Ferrell B, Bhatia S. Preparing professional staff to care for cancer survivors. J Cancer Surviv. 2007;1(1):98–106. doi: 10.1007/s11764-007-0008-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant M, Economou D. Survivorship Education for Quality Cancer Care. Oncology Issues. 2007 July/August;:24–29. [Google Scholar]
- Haylock PH, Curtiss CP. Nursing responds: coming together to improve the care of survivors of adult cancers. American Journal of Nursing. 2007;33(2) [Google Scholar]
- Hewitt M, Greenfield S, Stovall E. From Cancer Patient to Cancer Survivor Lost in Transition. Institute of Medicine; 2006. [Google Scholar]
- Knowles MS. The Adult Learner. A Neglected Species. Vol. 4e. Houston: Gulf Publishing; 1973; 1990. [Google Scholar]
- Lamkin L, Rosiak J, Buerhaus P, Mallory G, Williams M. Oncology Nursing Society Workforce Survey. Part II: perceptions of the nursing workforce environment and adequacy of nurse staffing in outpatient and inpatient oncology settings. Oncol Nurs Forum. 2002;29(1):93–100. doi: 10.1188/ONF.93-100. [DOI] [PubMed] [Google Scholar]
- LIVESTRONG Care Plan. [Retrieved March 17, 2010]; from www.livestrongcareplan.org.
- Miller KD. Cancer survivors, late and long-term issues. Cancer J. 2008;14(6):358–360. doi: 10.1097/PPO.0b013e31818f046c. [DOI] [PubMed] [Google Scholar]
- NCCS. National Coalition of Cancer Survivors (NCCS) from www.canceradvocacy.org.
- Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006;24(32):5117–5124. doi: 10.1200/JCO.2006.07.0474. [DOI] [PubMed] [Google Scholar]
- Office of Cancer Survivorship. [Retrieved May 17, 2010];Fact Sheet. 2006 from http://cancercontrol.cancer.gov/ocs/
- [Retrieved March 17, 2010];The Journey Forward Care Plan Builder. from www.journeyforward.org.