Abstract
Background
Since heart failure (HF) is the final common pathway for most heart diseases, we examined its 10-year prevalence trend by race, gender, and age in Tennessee.
Methods and Results
HF hospitalization data from the Tennessee Hospital Discharge Data System were analyzed by race, gender and age. Rates were directly age-adjusted using the Year 2000 standard population. Adult (age 20+) in-patient hospitalization for primary diagnosis of HF (HFPD) increased from 4.2% in 1997 to 4.5% in 2006. Age-adjusted hospitalization for HF (per 10,000 population) rose by 11.3% (from 29.3 in 1997 to 32.6 in 2006). Parallel changes in secondary HF admissions were also noted. Age-adjusted rates were higher among blacks than whites and higher among men than women. The ratios of black to white by gender admitted with HFPD in 2006 were highest (9:1) among the youngest age categories (20-34 and 35-44 years). Furthermore, for each age category of black men below 65 years, there were higher HF admission rates than for white men in the immediate older age category. In 2006, the adjusted rate ratios for HFPD in black to white men aged 20-34 and 35-44 years were OR=4.75, CI (3.29-6.86) and OR 5.10, CI (4.15-6.25) respectively. Hypertension was the independent predictor of HF admissions in black men age 20-34 years.
Conclusions
The higher occurrence of HF among young adults in general, particularly among young black men, highlights the need for prevention by identifying modifiable biological and social determinants in order to reduce cardiovascular health disparities in this vulnerable group.
Keywords: heart failure, hospitalization, prevention, diagnosis, risk factors
Heart failure (HF) is a leading cause of morbidity and mortality, and represents the final common pathway for most forms of heart disease. It affects 5.8 million Americans with an annual diagnosis of 670,000 adults, and approximately 20% of the newly diagnosed die within a year.1 In 2006, HF was regarded as a contributing cause of mortality among 282,754 Americans.1 Advances in pharmaco-therapeutics have shown remarkable mortality benefits, 2-21 but have not stemmed the tide of HF as a 21st century epidemic.22, 23 In fact, improvement in survival from these therapeutic agents has contributed to the observed increase in HF prevalence and the economic burden of treating the aging United States (US) population. 24, 25 In the most recent analysis of the US national hospital bill, congestive HF ranked second among the top twenty most expensive conditions billed to Medicare, and was among the top five most expensive conditions treated in the US overall.26 The economic burden of HF in 2010 (including the healthcare and lost productivity) is estimated to be $39.9 billion.1
Racial disparities in HF and cardiovascular disease (CVD) in general are well documented, as are the special vulnerabilities of the elderly, immigrant and other low-income populations, and those with chronic mental and/or physical health conditions.27, 28 The southeastern US is also disproportionately affected by CVD.29 A recent report from the Coronary Artery Risk Development in Young Adults (CARDIA) study,30 also showed remarkable racial differences in incident heart failure (HF) among young adults (< 50 years of age). Specifically, the likelihood of African Americans developing HF was 20 times higher than that of comparable whites. Hypertension, obesity, kidney disease, and systolic dysfunction before the age of 40 years were all significant antecedents.
Tennessee, located in the southeastern US, is one of the unhealthiest states in the US.25 Additionally, Tennessee's rate of diabetes (pre-clinical HF–Stage A) exceeds that of all other states in America according to a recent Behavioral Risk Factor Surveillance System Report (BRFSS), which evaluated trends for specific risk factors from 1997 to 2007. 27 The projected 2010 diabetes prevalence of 13.2% in Tennessee is in excess of the Healthy People 2010 target goal of 2.5%.31 In addition, more than one-third of Tennesseans suffer from hypertension, another qualifier for HF Stage A. In the present report we describe contemporary, ten-year trends for HF hospitalization in Tennessee (1997-2006) and discuss potential policy implications.
Methods
Data
We used ten-year Hospital Discharge Data System (HDDS) inpatient information for 1997 to 2006. The Division of Health Statistics, Tennessee Department of Health (TDH), compiles the HDDS. One aim is to ensure horizontal equity in the analyses and comparison of services. All hospitals licensed by the TDH are required by law to report patient-level discharge information.32 All data are reported on a uniform billing form developed by the National Uniform Billing Committee. Although the current version of the data collection form (UB-04) was launched in 2007, the data for the ten-year period analyzed was collected using the preceding version (UB-92).32 Regardless, all variables collected in the HDDS conform to the national standards of the Uniform Hospital Discharge Data Set (UHDDS) put forth by the Department of Health and Human Services.33, 34, These variables include but are not limited to: date of birth; gender; race/ethnicity; county and US Postal Zip Code of residence; date of admission; type of admission and discharge; admitting and discharge principal and secondary diagnosis codes (ICD-9); discharge status; principal procedure code; principal procedure date; total charges and expected sources of payment.32
We used ICD-9 codes 402, 404, and 428 for HF (see Table 1) as previously employed by Fang et al.25 For each year, we identified cases with at least one admission in which HF was a principal (primary). While an individual may appear in more than one year, each individual appears only once in the analyses for any one year. We also identified cases of secondary diagnoses of HF (HFSD) to determine whether they parallel trends in admissions for primary HF diagnosis (HFPD). In order to assure that the primary and secondary groups were mutually exclusive, the primary group (HFPD) was defined as beneficiaries with either a primary diagnosis alone or both a primary and a secondary diagnosis of HF. The secondary group (HFSD) was defined as beneficiaries with admissions for which HF was only a secondary diagnosis with the primary diagnosis always being other than HF (e.g., cancer). Relevant inpatient data were extracted with a focus on gender, categories of age, and race, that is, non-Hispanic whites and blacks who constitute 95% of Tennessee population. Yearly race-gender specific rates were also obtained for hypertension and diabetes among heart failure patients. There were no significant changes in the definitions or coding for hypertension and diabetes during the period of observation. Since comparable data for obesity were not consistently available from the hospital discharge data, we used results from the US Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System (BRFSS)35 for this purpose.
Table 1. ACC/AHA Heart Failure Performance Measures ICD-09-CM Diagnostic Codes.
| ICD-9-CM Code | Description |
|---|---|
| 402.01 | Malignant, hypertensive heart disease with heart failure |
| 402.11 | Benign, hypertensive heart disease with heart failure |
| 402.91 | Unspecified, hypertensive heart & renal disease with heart failure |
| 404.01 | Malignant, hypertensive heart & renal disease with heart failure |
| 404.03 | Malignant, hypertensive heart & renal disease with heart failure & renal failure |
| 404.11 | Benign, hypertensive heart & renal disease with heart failure |
| 404.13 | Benign, hypertensive heart & renal disease with heart failure & renal failure |
| 404.91 | Unspecified, hypertensive heart & renal disease with heart failure |
| 404.93 | Unspecified, hypertensive heart & renal disease with heart failure & renal failure |
| 428.00 | Unspecified, congestive heart failure |
| 428.01 | Left heart failure |
| 428.09 | Unspecified, heart failure |
| 428.20 | Unspecified, systolic heart failure |
| 428.21 | Acute systolic heart failure |
| 428.22 | Chronic systolic heart failure |
| 428.23 | Acute or chronic systolic heart failure |
| 428.30 | Unspecified, diastolic heart failure |
| 428.31 | Acute diastolic heart failure |
| 428.32 | Chronic diastolic heart failure |
| 428.33 | Acute or chronic diastolic heart failure |
| 428.40 | Unspecified, combined systolic & diastolic heart failure |
| 428.41 | Acute combined systolic & diastolic heart failure |
| 428.42 | Chronic combined systolic & diastolic heart failure |
| 428.43 | Acute or chronic combined systolic & diastolic heart failure |
ACC/AHA = American College of Cardiology/American Heart Association; ICD-09-CM = International Classification of Diseases-Ninth Revision-Clinical Modification
Statistical analysis
All rates (per 10,000) were age-standardized by the direct method and indexed to the Year 2000 Standard Population per methodology provided by the US Centers for Disease Control and Prevention.36 Numerators for hospitalization rates for 1997 through 2006 were the estimated number of hospitalizations according to Department of Health and Human Services (DHHS). Denominators were from the US Census.37 Age-specific rates and trends in gender and race were evaluated in conjunction with estimation of relative percentage changes between 1997 and 2006. Fishers Exact Test was utilized for comparison of prevalence of comorbidities by race and gender. Percentages of HF admissions in each period were compared using a Pearson chi-square test with Yates' correction for continuity and odd ratios were obtained through logistic regression analyses, which controlled for age, hypertension, diabetes, and any coronary heart disease. SPSS (Statistical Package for the Social Sciences, version 11, McGraw Hill Publishers, 2002) software was utilized for all analyses. A p-value of <0.05 was the accepted threshold for statistical significance.
Results
Overall Trends in HF Hospitalization
During the 10-year period, the proportion of hospitalized patients (aged 20+) with a primary diagnosis of HF (HFPD) increased from 4.2% in 1997 (15,614 of 371,646) to 4.5% (20,459 of 455,753) in 2006 (see columns one and two in Table 2). The age-adjusted rate (per 10,000 population) for HFPD jumped from 29.3 in 1997 to 32.6 in 2006, corresponding to an increase of 11.3%.
Table 2. Selected Characteristics of Hospitalized Patients Age 20+ with Primary Diagnosis of Heart Failure 1997 & 2006 (HDDS).
| HF Primary | TOTAL | WHITE | BLACK | MALE | FEMALE | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1997 | 2006 | 1997 | 2006 | 1997 | 2006 | 1997 | 2006 | 1997 | 2006 | |
| Columns → | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| HFPD (n) | 15,614 | 20,459 | 11,614 | 15,752 | 3,096 | 4,470 | 6,754 | 9,337 | 8,858 | 11,122 |
| Rate/10k§ | 29.3 | 32.6 | 24.8 | 28.6 | 48.9* | 58.3* | 29.4* | 36.3* | 26.1 | 30.0 |
| Mean Age | 72 | 71 | 74 | 74 | 66 | 62 | 70 | 68 | 74 | 74 |
| Female % | 57.6 | 54.4 | 56.1 | 54.6 | 59.1 | 52.8 | - | - | - | - |
| HFPD % per Age Category | ||||||||||
| 20-34 | 0.9 | 1.1 | 0.5 | 0.5 | 2.4 | 3.1 | 1.1 | 1.4 | 0.7 | 0.7 |
| 35-44 | 3.0 | 3.5 | 1.6 | 1.1 | 7.8 | 9.7 | 3.3 | 4.5 | 2.7 | 2.6 |
| 45-54 | 7.3 | 9.6 | 5.4 | 6.3 | 14.5 | 21.7 | 8.7 | 11.6 | 6.2 | 7.9 |
| 55-64 | 14.3 | 16.2 | 13.2 | 14.7 | 18.5 | 21.9 | 17.5 | 19.7 | 11.9 | 13.3 |
| 65-74 | 25.5 | 22.7 | 25.8 | 23.4 | 24.6 | 19.1 | 28.7 | 24.6 | 23.0 | 21.1 |
| 75-84 | 30.8 | 28.1 | 33.5 | 31.5 | 20.8 | 16.4 | 29.0 | 26.1 | 32.2 | 29.8 |
| 85+ | 18.2 | 18.9 | 20.0 | 22.0 | 11.4 | 8.1 | 11.6 | 12.1 | 23.3 | 24.6 |
| Prevalence of Co-morbidities | ||||||||||
| HTN % | 59.5 | 78.4 | 55.7 | 75.3 | 75.5* | 90.0* | 55.3 | 75.4 | 62.7* | 81.1* |
| DM % | 36.8 | 43.8 | 35.6 | 42.5 | 40.5 | 48.9* | 35.0 | 43.6 | 38.3* | 44.2 |
| CHD, any % | 58.7 | 46.1 | 62.6* | 44.5 | 44.0 | 52.4* | 63.7* | 45.7 | 54.3 | 46.5 |
HF, heart failure; HFPD, heart failure primary diagnosis; HTN= hypertension; DM= Diabetes mellitus; CHD= coronary heart disease
Black vs. White differences in 1997 and 2006 (see columns 5 vs. 3 and 6 vs. 4) and Male vs. Female differences (columns 7 vs. 9 and 8 vs. 10) in 1997 and 2006 are significant at p < 0.000
With-in group differences between 1997 and 2006 are significant at p<0.001
Rates per 10K are age-adjusted, all ages.
We compared selected characteristics of HFPD hospitalizations for 1997 and 2006 (Table 2). The average age in 1997 was 72 years, and 71 years in 2006. The proportion of elderly (aged 65+) with HFPD dropped from 74.5% in 1997 to 69.7% in 2006. Furthermore, the HFPD patients had a high prevalence of co-morbid conditions including hypertension (60% in 1997 and 78% in 2006), diabetes (37% in 1997 and 44% in 2006), and coronary heart diseases (59% in 1997 and 46% in 2006).
HF Rates By Race, Gender, & Age categories
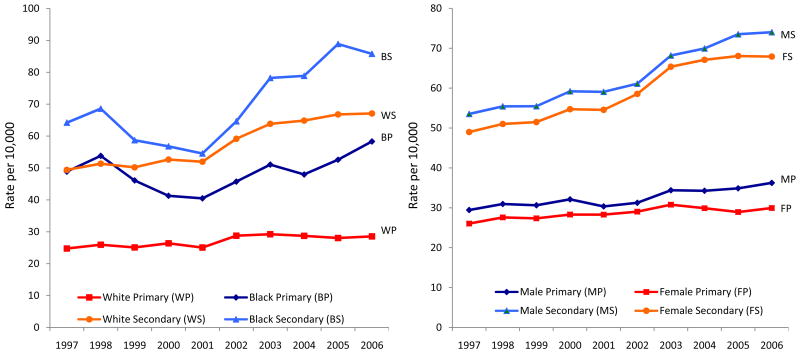
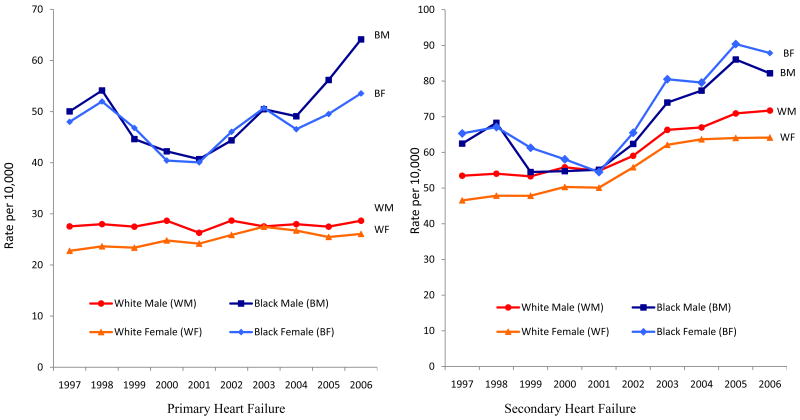
There were racial and gender differences in the age-adjusted hospitalization rates (Figure 1a) for HFPD, with higher rates among blacks compared to whites and among males compared to females during this 10-year period. Furthermore, within each gender there were racial differences in the age-adjusted hospitalization rates for HFPD, with higher rates among black males than white males, and among black woman than white women (Figure 1b). These noted intra-gender racial differences in age-adjusted hospitalization rates were most profound for HFPD. A breakdown of these age-adjusted rates in Table 2 further substantiates the observation in that the rates of hospitalization for HFPD among blacks and males were higher compared to whites and females respectively, in both 1997 and 2006. However, both graphs (in Figure 1a) show that rates for blacks follow a complicated pattern, with declines in 2000 and 2001.
Figure 1.
Figure 1a: Age-adjusted Hospitalization Rates for Heart Failure by Race and Gender, 1997-2006 (HDDS)
Figure 1b: Age-adjusted Intra-gender Hospitalization Rates for Primary and Secondary Diagnosis of Heart Failure by Race, 1997-2006 (HDDS)
Table 3 shows both the unadjusted and adjusted ratios of black to white hospitalization rates for HFPD. In both 1997 and 2006, the black to white ratio was significantly >1.0 for all ages except 85+. The highest values for the black to white rate ratio occurred among 20 to 34 and 35 to 44 year olds. Further analysis revealed that the HF rates were 3 to 8 times higher among blacks (under the age of 65) compared to their white peers. These higher black to white rate ratios (unadjusted) were reduced to 5 times in logistic regression models that controlled for age, hypertension, diabetes, and coronary heart disease. Even so, in 2006 the black to white adjusted ratios for HFPD hospitalization were 4.70 (95% CI 3.52, 6.29) and 4.78 (95% CI 4.08, 5.60) among blacks ages 20 to 34 and 35-44 respectively.
Table 3. Age-adjusted Rate per 10,000, Rate Ratios, and Odd Ratio for Primary Diagnosis of Heart Failure by Race and Gender in 1997 & 2006.
| Primary Diagnosis By Race | Rate per 10K | Unadjusted OR | Adjusted OR & 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Category | Black 1997 | Black 2006 | White 1997 | White 2006 | B/W Ratio 1997 | B/W Ratio 2006 | B/W Odds Ratio 1997 | CI 1997 | B/W Odds Ratio 2006 | CI 2006 |
| Column → | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 20-34 | 3.6 | 6.6 | 0.5 | 0.8 | 6.6 | 8.7 | 3.84 | 2.68-5.50 | 4.70 | 3.52-6.29 |
| 35-44 | 17.2 | 31.4 | 2.6 | 3.6 | 6.5 | 8.8 | 3.94 | 3.23-4.80 | 4.78 | 4.08-5.60 |
| 45-54 | 49.5 | 68.1 | 10.0 | 13.0 | 5.0 | 5.3 | 3.06 | 2.60-3.49 | 3.41 | 3.10-3.74 |
| 55-64 | 104.8 | 121.1 | 35.4 | 39.4 | 3.0 | 3.1 | 1.97 | 1.77-2.19 | 2.25 | 2.08-2.44 |
| 65-74 | 83.3 | 197.7 | 89.4 | 102.9 | 2.1 | 1.9 | 1.68 | 1.53-1.83 | 1.60 | 1.48-1.73 |
| 75-84 | 261.8 | 302.9 | 189.2 | 215.1 | 1.4 | 1.4 | 1.32 | 1.21-1.45 | 1.31 | 1.20-1.42 |
| 85+ | 377.7 | 340.9 | 346.5 | 397.4 | 1.1 | 1.1 | 1.08 | 0.95-1.21 | 0.90 | 0.80-1.01 |
| All Ages | 48.9 | 58.3 | 24.8 | 28.6 | 1.97 | 2.0 | 1.74 | 1.67-1.82 | 1.90 | 1.83-1.96 |
| Primary Diagnosis By Gender | Rate per 10K | Unadjusted OR | Adjusted OR & 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Category | Male 1997 | Male 2006 | Female 1997 | Female 2006 | M/F Ratio 1997 | M/F Ratio 2006 | M/F Odds Ratio 1997 | CI 1997 | M/F Odds Ratio 2006 | CI 2006 |
| 20-34 | 1.2 | 2.2 | 1.0 | 1.4 | 1.2 | 1.6 | 2.68 | 1.85-3.88 | 3.49 | 2.60-4.67 |
| 35-44 | 5.1 | 9.7 | 5.2 | 6.4 | 1.0 | 1.5 | 1.13 | 0.96-1.37 | 2.02 | 1.72-2.36 |
| 45-54 | 16.9 | 24.8 | 14.9 | 19.0 | 1.1 | 1.3 | 1.05 | 0.93-1.19 | 1.45 | 1.32-1.59 |
| 55-64 | 51.2 | 56.9 | 40.9 | 42.4 | 1.2 | 1.3 | 1.04 | 0.95-1.14 | 1.35 | 1.26-1.45 |
| 65-74 | 116.9 | 123.4 | 95.9 | 104.6 | 1.2 | 1.2 | 1.03 | 0.96-1.10 | 1.15 | 1.08-1.22 |
| 75-84 | 232.1 | 249.8 | 195.0 | 208.6 | 1.2 | 1.2 | 1.04 | 0.98-1.11 | 1.17 | 1.11-1.24 |
| 85+ | 386.7 | 433.7 | 366.7 | 381.2 | 1.1 | 1.1 | 0.95 | 0.86-1.04 | 1.07 | 0.99-1.15 |
| All Ages | 29.4 | 36.3 | 26.1 | 30.0 | 1.1 | 1.2 | 1.09 | 1.05-1.13 | 1.31 | 1.26-1.35 |
The higher ratio of HF admissions amongst blacks was preserved when further analyzed by gender (Table 4). In 2006, a significant trend in HF hospitalization was noted amongst black males relative to white males (HF admissions 3 to 10 times higher before the age of 65; see column 6). In fact, both in 1997 and 2006, high black to white admission ratios for HFPD were noted in the young and middle-aged categories. These race and gender relationships were preserved in 2006 adjusted rate ratios comparing black males to white males [in column 9, patients aged 20-34, OR=4.75, CI (3.29-6.86, and among patients aged 35-44, OR 5.10, CI (4.15-6.25)]. Similar higher adjusted ratios emerged for black females to white females [among 20-34 year olds, OR=4.60, CI (2.86-7,41) and among females aged 35-44 year olds, OR=4.21, CI (3.28-5.40)].
Table 4. Age-adjusted Rate per 10,000, Rate Ratios, and Odds Ratios for Primary Diagnosis of Heart Failure by Gender across Race & Age in 1997 & 2006.
| Male Primary Diagnosis | Unadjusted OR | Adjusted OR & 95% CI | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Category | BM 1997 | WM 1997 | BM 2006 | WM 2006 | BM/WM Ratio 1997 | BM/WM Ratio 2006 | BM/WM Odds Ratio 1997 | CI 1997 | BM/WM Odds Ratio 2006 | CI 2006 |
| Column → | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 20-34 | 4.5 | 0.5 | 8.5 | 1.0 | 8.4 | 8.5 | 4.71 | 2.89-7.68 | 4.75 | 3.29-6.86 |
| 35-44 | 6.8 | 2.8 | 39.3 | 3.7 | 5.9 | 10.6 | 3.68 | 2.78-4.88 | 5.10 | 4.15-6.25 |
| 45-54 | 48.4 | 11.4 | 80.8 | 13.7 | 4.2 | 5.9 | 2.87 | 2.38-3.45 | 3.76 | 3.32-4.27 |
| 55-64 | 116.7 | 40.4 | 139.7 | 40.7 | 2.9 | 3.4 | 2.16 | 1.86-2.51 | 2.32 | 2.08-2.59 |
| 65-74 | 188.2 | 102.5 | 211.2 | 104.3 | 1.8 | 2.0 | 1.70 | 1.49-1.95 | 1.67 | 1.48-1.88 |
| 75-84 | 262.3 | 215.5 | 303.2 | 216.5 | 1.2 | 1.4 | 1.24 | 1.07-1.44 | 1.31 | 1.14-1.51 |
| 85+ | 377.1 | 362.8 | 355.8 | 389.5 | 1.0 | 0.9 | 1.22 | 0.90-1.40 | 0.94 | 0.74-1.18 |
| All Ages | 50.0 | 27.6 | 64.1 | 28.7 | 1.8 | 2.2 | 1.84 | 1.72-1.97 | 2.18 | 2.06-2.30 |
| Female Primary Diagnosis | Unadjusted OR | Adjusted OR & 95% CI | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Category | BF 1997 | WF 1997 | BF 2006 | WF 2006 | BF/WF Ratio 1997 | BF/WF Ratio 2006 | BF/WF Odds Ratio 1997 | CI 1997 | BF/WF Odds Ratio 2006 | CI 2006 |
| 20-34 | 2.8 | 0.5 | 5.0 | 0.6 | 8.4 | 9.1 | 2.70 | 1.57-4.62 | 4.60 | 2.86-7.41 |
| 35-44 | 17.5 | 2.5 | 24.6 | 2.8 | 5.9 | 8.8 | 4.04 | 3.05-5.34 | 4.21 | 3.28-5.40 |
| 45-54 | 50.3 | 8.6 | 57.3 | 11.2 | 4.2 | 5.1 | 3.20 | 2.66-3.85 | 3.01 | 2.62-3.46 |
| 55-64 | 95.8 | 30.9 | 106.1 | 32.9 | 7.9 | 3.2 | 1.75 | 1.51-2.03 | 2.14 | 1.90-2.40 |
| 65-74 | 179.9 | 79.0 | 188.3 | 94.0 | 1.8 | 2.0 | 1.64 | 1.46-1.85 | 1.52 | 1.37-1.70 |
| 75-84 | 261.6 | 174.1 | 303.3 | 196.7 | 1.2 | 1.5 | 1.37 | 1.22-1.54 | 1.30 | 1.16-1.43 |
| 85+ | 377.9 | 340.8 | 349.4 | 381.5 | 1.0 | 0.92 | 1.05 | 0.91-1.21 | 0.90 | 0.77-1.01 |
| All Ages | 48.0 | 22.8 | 53.6 | 26.1 | 1.8 | 2.1 | 1.67 | 1.57-1.76 | 1.66 | 1.58-1.75 |
The age-adjusted hospitalization rates for HF by race from 1997 through 2006 show higher rates for both HFPD among blacks by gender in every year (Figure 1b). Through this 10 year period, the rates for young black males 20-34 & 35-44 years old increased nearly two- and six-fold respectively, compared to their white counterparts; while higher rates of HF admission existed among black females compared to white females, the pattern is less striking (Table 4). Analyses of admissions for HFSD revealed changes that paralleled trends in HFPD (Figures 1a and b), with similar characteristics of hospitalized patients, race and gender relationships (detailed data not shown)
HF Co-morbidities
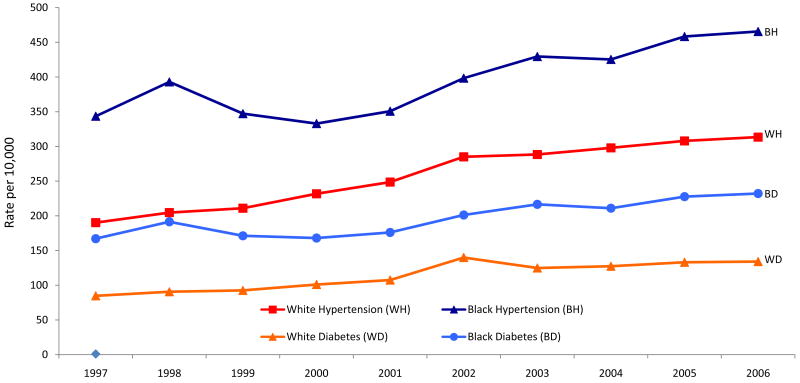
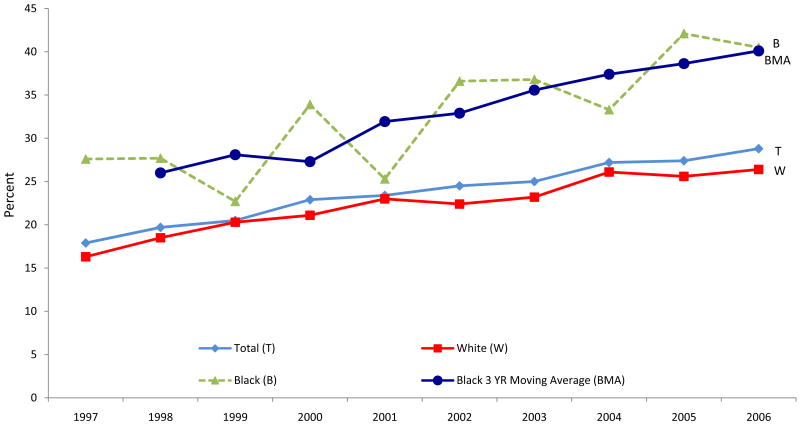
Since HF rates had significantly increased from 1997 to 2006, we evaluated the prevalence of co-morbid conditions associated with HFPD. Black in-patients with HFPD (Table 2, column 3 and 5) had higher rates than whites for hypertension (in 1997, 75.5% for blacks versus 55.7% for whites), diabetes (40.5% versus 35.6%) and lower rates for coronary heart disease (44.0% versus 62.6%); this pattern was preserved in 2006 (see column 4 and 6) except that there was a higher percentage of coronary heart disease among blacks (52.4%) compared to whites (44.5%). The trend in HF co-morbidities by race and gender for each age category is shown in Table 5. In 2006, younger black men admitted for HFPD had higher rates of hypertension compared to their white peers and those in older age categories; this was not observed for diabetes and coronary heart disease. Similar trends were observed for 1997 (not shown here). Collectively, this suggests that hypertension is the dominant co-morbidity linked with the observed HF disparity (see Figure 2 indicating higher prevalence of hypertension among blacks compared to whites from 1997 to 2006). Similar trends existed for diabetes among HF patients (see Figure 2). Comparable data for obesity on these patients were not consistently available. However, BRFSS data relative to obesity in Tennessee (see Figure 3) shows that obesity rates were higher among blacks compared to whites over a number of years. This appears to be consistent with observations for diabetes among HF patients.
Table 5. Percent Prevalence of Co-morbid Conditions Among Heart Failure Patients (HFPD) In 2006 by Age, Race, and Gender.
| Age Category | BM | WM | BF | WF | ||
|---|---|---|---|---|---|---|
| %(N) | % (N) | p-Value | % (N) | % (N) | p-Value | |
| Hypertension | ||||||
| 20-34 | 84(82) | 54 (48) | <0.000 | 79 (56) | 62 (26) | NS |
| 35-44 | 88(250) | 68 (161) | <0.000 | 91(183) | 71(102) | <0.000 |
| 45-54 | 89(529) | 74 (536) | <0.000 | 90(441) | 72 (423) | <0.000 |
| 55-64 | 91(504) | 74 (1,311) | <0.000 | 92(473) | 77 (987) | <0.000 |
| 65-74 | 91(374) | 73(1,885) | <0.000 | 92(479) | 81 (1,848) | <0.000 |
| 75-84 | 90(255) | 71(2,160) | <0.000 | 91(482) | 80 (2,804) | <0.000 |
| 85+ | 84(91) | 66 (1,029) | <0.000 | 89(271) | 78 (2,432) | <0.000 |
| Diabetes | ||||||
| 20-34 | 21 | 19 | NS | 29 | 42 | NS |
| 35-44 | 32 | 39 | NS | 33 | 37 | NS |
| 45-54 | 41 | 46 | NS | 50 | 54 | NS |
| 55-64 | 50 | 54 | NS | 62 | 58 | NS |
| 65-74 | 55 | 52 | NS | 66 | 53 | <0.000 |
| 75-84 | 44 | 39 | NS | 56 | 41 | <0.000 |
| 85+ | 30 | 25 | NS | 37 | 25 | <0.000 |
| Coronary Heart Disease | ||||||
| 20-34 | 37 | 35 | NS | 48 | 65 | NS |
| 35-44 | 44 | 44 | NS | 55 | 46 | NS |
| 45-54 | 53 | 47 | <0.02 | 52 | 47 | NS |
| 55-64 | 52 | 47 | 0.06 | 57 | 50 | <0.008 |
| 65-74 | 53 | 46 | <0.008 | 56 | 44 | <0.000 |
| 75-84 | 50 | 43 | <0.03 | 52 | 44 | <0.000 |
| 85+ | 52 | 40 | <0.02 | 54 | 41 | <0.000 |
BM, black males; WM, white males; BF, black females; WF, white females; Denominator (N) in each cell used for percentage (%) calculations in Hypertension are the same for Diabetes and CHD; HFPD, heart failure primary diagnosis
Figure 2. Racial Disparities in the 10-year Prevalence Trend of Hypertension and Diabetes in Tennessee (HDDS).
Figure 3. Racial Disparities in the 10-year Prevalence Trend of Obesity in Tennessee (BRFSS) HDDS, Hospital Discharge Data System; BRFSS, Behavioral Risk Factor Surveillance System.
Discussion
In a recent report by Fang et al. 25 the nation-wide number of hospitalization for HF had increased over the past 2-3 decades; however, they did not report on racial differences due to data limitations. Our findings indicate that the pattern of HF hospitalizations in Tennessee mirrors reported national trends, demonstrating an overall increase in all HFPD hospitalizations. Also, HFPD hospitalizations increased exponentially with age, and 75% of all admissions in 1997 and 70% in 2006 were among Medicare patients (>65 years).
Overall, blacks (under 65) had greater rates for HFPD than whites, and men greater than women. Similarly, in both men and women there was an exponential increase in the ratio of black to white hospitalization rates for every decade drop in age below 85 years. However, the remarkably higher rates of HFPD admissions among black men, with higher HFPD hospitalization rates among blacks relative to whites for each age category below 65 years are particularly alarming. Furthermore, among young adults aged 20-34 and 35-44 years the rates for black males increased nearly 2 and 6 times respectively, during the 10-year period unlike their white peers. These findings add to a growing body of evidence on the increasing incidence and prevalence of HF amongst younger men as well as the racial differences therein. In a recent report from the CARDIA study for example, incident HF among young adults (< 50 years) was 20 times more likely in blacks compared with their white peers, and hypertension and obesity were some of the noted antecedents manifest before age 40 years.30
Elimination of CV health disparities involves a systematic assessment of behavioral and lifestyle choices, environmental factors, healthcare access limitations, health literacy and numeracy levels, cultural factors, and genetic and gene-environment interactions.38, 39 These factors may explain some of the observed HF health disparities. However, the high prevalence of apparently modifiable risk factors provides great opportunity for the prevention and treatment. In our study, a significant proportion of the patients admitted with HF suffered from hypertension and diabetes, with a statistically significant difference in prevalence between blacks and whites. Another contributory factor to health disparity is the fact that despite advances in pharmacologic treatment for HF, 2-21 the translation of evidenced-based therapy has been poor.40, 41 This, in turn, is consistent with the observation by Phelan et al. 42 that black-white disparities in US mortality are greatest for conditions we know how to treat or prevent.
In Tennessee, the State Department of Health has taken a first step by developing a comprehensive Heart Disease and Stroke Prevention Plan.43 This is consistent with the observations of various models of care 44 including those of Rust et al.45, which show that the greatest successes in reducing US mortality during the 20th century came about with public health and medical care collaboration – particularly as regards primary care.
Limitations and Strengths
There are important limitations of the HDDS data, which do not compromise data validity or internal accuracy but are worthy of mention. The HDDS being an administrative file is devoid of clinical data to verify diagnoses, measure severity of illness or identify pharmaceutical treatment. Also, while co-morbidity analyses would have benefitted from inclusion of obesity, the low percentages of patients discharged with such a diagnosis (3.3% for white males, 2.8% for black males, 4.0% for white females and 5.8% for black females suggested severe under-ascertainment, most probably because in-patient evaluation and management for obesity was not rendered as part of the admission. A major strength of HDDS data, however, is the opportunity for describing long-term hospitalization trends along with the cost of hospitalization based on a large representative data set derived from standardized methodology.
Conclusion
In summary, the overall prevalence of HFPD hospitalizations in Tennessee has increased over the last ten years, and it mirrors previously reported pattern of HF hospitalizations nation-wide. However, younger black men (aged 20-34 years) had higher rates of hospitalization for HF, which nearly doubled during a 10-year period. Even more concerning is the fact that within each age category there were higher HFPD hospitalization rates for blacks. Similar trends were noted for HFSD hospitalizations. In general, hypertension and diabetes were co-morbidities independently associated with HFPD; however, amongst younger black men (aged 20-34 years) hypertension was the only independent risk factor. The higher prevalence of hypertension and diabetes (HDDS data), and obesity (BRFSS data) amongst blacks in Tennessee indicate important areas of focus. Granting the overarching importance of social determinants of health, these observations also highlight the need for prevention as well as aggressive risk factor modulation in our clinical care settings. It also calls for a renewed philosophy in our care delivery approach to vulnerable populations to reduce the tide of cardiovascular health disparities.
Acknowledgments
Sources of Funding: This analysis was supported by a grant from CDC #U58CCU422782 to Tennessee Department of Health (#ED-07-20811-00 to Tennessee State University, B.A. Husaini, PI) and NIH grant # P20-MD000516 (National Center on Minority Health & Health Disparity to Meharry Medical College; Drs. Levine, Husaini, Hull, and Cain are supported in part by this NIH grant; The views expressed do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention by trade names, commercial practices, or organizations imply endorsement by the U.S. Government). Dr U. K. Sampson is supported in part by Harold Amos Medical Faculty Award of the Robert Wood Johnson Foundation and the Vanderbilt CTSA grant UL1RR024975 NCRR/NIH).
Footnotes
Disclosures: George Mensah is employed by PepsiCo, although no conflicts of interest have been identified in his role.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics--2010 update: A report from the american heart association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Pitt B, Poole-Wilson PA, Segal R, Martinez FA, Dickstein K, Camm AJ, Konstam MA, Riegger G, Klinger GH, Neaton J, Sharma D, Thiyagarajan B. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: Randomised trial--the losartan heart failure survival study ELITE II. Lancet. 2000;355:1582–1587. doi: 10.1016/s0140-6736(00)02213-3. [DOI] [PubMed] [Google Scholar]
- 3.Effects of enalapril on mortality in severe congestive heart failure. Results of the cooperative north scandinavian enalapril survival study (consensus). The consensus trial study group. N Engl J Med. 1987;316:1429–1435. doi: 10.1056/NEJM198706043162301. [DOI] [PubMed] [Google Scholar]
- 4.Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF) Lancet. 1999;353:2001–2007. [PubMed] [Google Scholar]
- 5.Leizorovicz A, Lechat P, Cucherat M, Bugnard F. Bisoprolol for the treatment of chronic heart failure: A meta-analysis on individual data of two placebo-controlled studies--cibis and cibis ii. Cardiac insufficiency bisoprolol study. Am Heart J. 2002;143:301–307. doi: 10.1067/mhj.2002.120768. [DOI] [PubMed] [Google Scholar]
- 6.Eichhorn EJ, Bristow MR. The carvedilol prospective randomized cumulative survival (copernicus) trial. Curr Control Trials Cardiovasc Med. 2001;2:20–23. doi: 10.1186/cvm-2-1-020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waagstein F, Caidahl K, Wallentin I, Bergh CH, Hjalmarson A. Long-term beta-blockade in dilated cardiomyopathy. Effects of short- and long-term metoprolol treatment followed by withdrawal and readministration of metoprolol. Circulation. 1989;80:551–563. doi: 10.1161/01.cir.80.3.551. [DOI] [PubMed] [Google Scholar]
- 8.Engelmeier RS, O'Connell JB, Walsh R, Rad N, Scanlon PJ, Gunnar RM. Improvement in symptoms and exercise tolerance by metoprolol in patients with dilated cardiomyopathy: A double-blind, randomized, placebo-controlled trial. Circulation. 1985;72:536–546. doi: 10.1161/01.cir.72.3.536. [DOI] [PubMed] [Google Scholar]
- 9.Pollock SG, Lystash J, Tedesco C, Craddock G, Smucker ML. Usefulness of bucindolol in congestive heart failure. Am J Cardiol. 1990;66:603–607. doi: 10.1016/0002-9149(90)90488-m. [DOI] [PubMed] [Google Scholar]
- 10.Andersson B, Blomstrom-Lundqvist C, Hedner T, Waagstein F. Exercise hemodynamics and myocardial metabolism during long-term beta-adrenergic blockade in severe heart failure. J Am Coll Cardiol. 1991;18:1059–1066. doi: 10.1016/0735-1097(91)90767-4. [DOI] [PubMed] [Google Scholar]
- 11.Eichhorn EJ, Bedotto JB, Malloy CR, Hatfield BA, Deitchman D, Brown M, Willard JE, Grayburn PA. Effect of beta-adrenergic blockade on myocardial function and energetics in congestive heart failure. Improvements in hemodynamic, contractile, and diastolic performance with bucindolol. Circulation. 1990;82:473–483. doi: 10.1161/01.cir.82.2.473. [DOI] [PubMed] [Google Scholar]
- 12.Eichhorn EJ, Heesch CM, Barnett JH, Alvarez LG, Fass SM, Grayburn PA, Hatfield BA, Marcoux LG, Malloy CR. Effect of metoprolol on myocardial function and energetics in patients with nonischemic dilated cardiomyopathy: A randomized, double-blind, placebo-controlled study. J Am Coll Cardiol. 1994;24:1310–1320. doi: 10.1016/0735-1097(94)90114-7. [DOI] [PubMed] [Google Scholar]
- 13.Packer M, Coats AJ, Fowler MB, Katus HA, Krum H, Mohacsi P, Rouleau JL, Tendera M, Castaigne A, Roecker EB, Schultz MK, DeMets DL. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344:1651–1658. doi: 10.1056/NEJM200105313442201. [DOI] [PubMed] [Google Scholar]
- 14.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med. 1999;341:709–717. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 15.Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, Olofsson B, Ostergren J, Yusuf S, Pocock S. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: The charm-overall programme. Lancet. 2003;362:759–766. doi: 10.1016/s0140-6736(03)14282-1. [DOI] [PubMed] [Google Scholar]
- 16.Pfeffer MA, McMurray JJ, Velazquez EJ, Rouleau JL, Kober L, Maggioni AP, Solomon SD, Swedberg K, Van de Werf F, White H, Leimberger JD, Henis M, Edwards S, Zelenkofske S, Sellers MA, Califf RM. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003;349:1893–1906. doi: 10.1056/NEJMoa032292. [DOI] [PubMed] [Google Scholar]
- 17.Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation. 1990;81:1161–1172. doi: 10.1161/01.cir.81.4.1161. [DOI] [PubMed] [Google Scholar]
- 18.Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The solvd investigators. N Engl J Med. 1991;325:293–302. doi: 10.1056/NEJM199108013250501. [DOI] [PubMed] [Google Scholar]
- 19.Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. The solvd investigattors. N Engl J Med. 1992;327:685–691. doi: 10.1056/NEJM199209033271003. [DOI] [PubMed] [Google Scholar]
- 20.Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. The acute infarction ramipril efficacy (aire) study investigators. Lancet. 1993;342:821–828. [PubMed] [Google Scholar]
- 21.Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, Bittman R, Hurley S, Kleiman J, Gatlin M. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309–1321. doi: 10.1056/NEJMoa030207. [DOI] [PubMed] [Google Scholar]
- 22.Braunwald E. Shattuck lecture--cardiovascular medicine at the turn of the millennium: Triumphs, concerns, and opportunities. N Engl J Med. 1997;337:1360–1369. doi: 10.1056/NEJM199711063371906. [DOI] [PubMed] [Google Scholar]
- 23.Croft JB, Giles WH, Pollard RA, Keenan NL, Casper ML, Anda RF. Heart failure survival among older adults in the united states: A poor prognosis for an emerging epidemic in the medicare population. Arch Intern Med. 1999;159:505–510. doi: 10.1001/archinte.159.5.505. [DOI] [PubMed] [Google Scholar]
- 24.Bonow RO, Bennett S, Casey DE, Jr, Ganiats TG, Hlatky MA, Konstam MA, Lambrew CT, Normand SL, Pina IL, Radford MJ, Smith AL, Stevenson LW, Bennett SJ, Burke G, Eagle KA, Krumholz HM, Linderbaum J, Masoudi FA, Ritchie JL, Rumsfeld JS, Spertus JA. Acc/aha clinical performance measures for adults with chronic heart failure: A report of the american college of cardiology/american heart association task force on performance measures (writing committee to develop heart failure clinical performance measures) endorsed by the heart failure society of america. J Am Coll Cardiol. 2005;46:1144–1178. doi: 10.1016/j.jacc.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 25.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the u.S., 1979 to 2004. J Am Coll Cardiol. 2008;52:428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 26.Russo C, Andrews R. Agency for healthcare research and quality; rockville, md: [april 5, 2010]. The national hospital bill: The most expensive conditions, by payer, 2004; hcup statistical brief #13; september 2006. Http://www.Hcup-us.Ahrq.Gov/reports/statbriefs/sb13.Pdf. [PubMed] [Google Scholar]
- 27.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. Acc/aha 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: A report of the american college of cardiology/american heart association task force on practice guidelines (writing committee to update the 2001 guidelines for the evaluation and management of heart failure): Developed in collaboration with the american college of chest physicians and the international society for heart and lung transplantation: Endorsed by the heart rhythm society. Circulation. 2005;112:e154–235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 28.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: A conceptual framework. Am J Public Health. 2006;96:2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O'Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y. Heart disease and stroke statistics--2009 update: A report from the american heart association statistics committee and stroke statistics subcommittee. Circulation. 2009;119:e21–181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 30.Bibbins-Domingo K, Pletcher MJ, Lin F, Vittinghoff E, Gardin JM, Arynchyn A, Lewis CE, Williams OD, Hulley SB. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tennessee's behavioral risk factor surveillance system report 2007. [december 25, 2009]; Http://health.State.Tn.Us/statistics/pdffiles/behavioralrsksrvy_2007.Pdf.
- 32.Tennessee department of health, division of health statistics 2007 hospital discharge data system user manual. [december 26, 2009]; Http://www.Tha-hin.Com/files/hdds-manual-ub04-1_0307.Pdf.
- 33.Uniform hospital abstract: Minimum basic data set. A report of the united states national committee on vital and health statistics. Vital Health Stat 1. 1972;4:1–17. [PubMed] [Google Scholar]
- 34.Health information policy council; 1984 revision of the uniform hospital discharge data set--hhs. Notice. Fed Regist. 1985;50:31038–31040. [PubMed] [Google Scholar]
- 35.National center for chronic disease prevention and health promotion behavioral risk factor surveillance system Http://www.Cdc.Gov/brfss/index.Htm.
- 36.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected u.S. Population. Healthy People 2010 Stat Notes. 2001:1–10. [PubMed] [Google Scholar]
- 37.Kozak LJ, DeFrances CJ, Hall MJ. National hospital discharge survey: 2004 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2006:1–209. [PubMed] [Google Scholar]
- 38.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: A systematic review. Ethn Dis. 2007;17:143–152. [PubMed] [Google Scholar]
- 39.Rooks RN, Simonsick EM, Klesges LM, Newman AB, Ayonayon HN, Harris TB. Racial disparities in health care access and cardiovascular disease indicators in black and white older adults in the health abc study. J Aging Health. 2008;20:599–614. doi: 10.1177/0898264308321023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Albert NM, Yancy CW, Liang L, Zhao X, Hernandez AF, Peterson ED, Cannon CP, Fonarow GC. Use of aldosterone antagonists in heart failure. Jama. 2009;302:1658–1665. doi: 10.1001/jama.2009.1493. [DOI] [PubMed] [Google Scholar]
- 41.Krantz MJ, Tanner J, Horwich TB, Yancy C, Albert NM, Hernandez AF, Dai D, Fonarow GC. Influence of hospital length of stay for heart failure on quality of care. Am J Cardiol. 2008;102:1693–1697. doi: 10.1016/j.amjcard.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 42.Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. “Fundamental causes” of social inequalities in mortality: A test of the theory. J Health Soc Behav. 2004;45:265–285. doi: 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- 43.Tennessee department of health and tennessee state university, center for health research . Tennessee heart disease and stroke prevention and care plan 2008-2012. Nashville, tn: Tennessee department of health; 2007. [Google Scholar]
- 44.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD. Defining and setting national goals for cardiovascular health promotion and disease reduction: The american heart association's strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 45.Rust G, Satcher D, Fryer GE, Levine RS, Blumenthal DS. Triangulating on success: Innovation, public health, medical care, and cause-specific us mortality rates over a half century (1950-2000) Am J Public Health. 2010;100 1:S95–104. doi: 10.2105/AJPH.2009.164350. [DOI] [PMC free article] [PubMed] [Google Scholar]