Abstract
Introduction
Few couple-focused interventions have been developed to improve distress and relationship outcomes among men diagnosed with localized prostate cancer and their partners.
Aims
We examined the effects of a five session Intimacy-Enhancing Therapy (IET) versus Usual Care (UC) on the psychological and relationship functioning of men diagnosed with localized prostate cancer and their partners. Pre-intervention levels of psychological and relationship functioning were evaluated as moderators of intervention effects.
Methods
Seventy one survivors and their partners completed a baseline survey and were subsequently randomly assigned to receive five sessions of IET or Usual Care (no treatment). Eight weeks after the baseline assessment, a follow-up survey was administered to survivor and partner.
Main outcome measures
Distress, well-being, relationship satisfaction, relationship intimacy, and communication were investigated as the main outcomes..
Results
IET effects were largely moderated by pre-intervention psychosocial and relationship factors. Those survivors who had higher levels of cancer concerns at pre-treatment had significantly reduced concerns following IET. Similar moderating effects for pre-intervention levels were reported for the effects of IET on self-disclosure, perceived partner disclosure, and perceived partner responsiveness. Among partners beginning the intervention with higher cancer-specific distress, lower marital satisfaction, lower intimacy, and poorer communication, IET improved these outcomes.
Conclusions
IET had a marginally significant main effect upon survivor well-being but was effective among couples with fewer personal and relationship resources. Subsequent research is needed to replicate these findings with a larger sample and a longer follow-up.
Keywords: Prostate cancer, Cancer and Sexual Quality of Life, Psychological Intervention, Intimacy-enhancing treatment
Introduction
Existing medical treatments for men diagnosed with localized prostate cancer including surgery, radiation, and androgen deprivation therapy have a number of potential side effects which can include erectile dysfunction (ED), dry orgasm, loss of libido, and urinary incontinence [1–3]. Each has the potential to cause emotional distress as they compromise masculinity, sexual desire, and the ability to engage in sexual activity [1, 2, 4–6]. The diagnosis and treatment of prostate cancer also affects partners, who typically play an important role in medical treatment [7, 8]. Indeed, studies suggest that partners report high levels of psychological distress [9–11]. Specific concerns about the patient’s side effects [10], changes in relationship roles [12], relationship satisfaction [13], sexual satisfaction [14], sexual dysfunction [15], and impairment in survivors’ quality of life associated with sexual and urinary problems [16,17] each contribute to partners’ distress.
These challenges can stress the relationship and ultimately compromise each partner’s psychological adaptation. Recent studies have suggested that marital quality declines after diagnosis, particularly among female partners [11]. Couples must manage practical stressors such as completing medical care, deal with changes in personal priorities, manage their own and their partner’s emotional distress, and attempt to maintain a sense of relationship “normalcy”. For couples who had an active sex life prior to the diagnosis, the loss of desire and/or spontaneity has implications both for the survivor as well as the partner. Communication is critical to managing these stressors effectively. Indeed, research has suggested that couples’ communication can influence both partners’ emotional distress and quality of life (e.g., 15, 18).
Despite the importance of communication, available research suggests that it can be challenging for couples to discuss their cancer-related problems and concerns. For example, Boehmer and Clarke [19] found that there was little direct communication between partners about the disease, with both partners holding back sharing feelings and concerns. Communication about prostate cancer may impact each partner’s individual distress by influencing the level of emotional intimacy each partner experiences. The Relationship Intimacy Model of Cancer Adaptation [20] proposes that communication influences couples’ psychological adaptation through its effects on relational intimacy, which is defined as feelings of emotional closeness with one’s partner. According to this model, communication can be either “relationship-enhancing” or “relationship-compromising”. Relationship-enhancing communication includes self-disclosure and being responsive to one’s partner. Relationship-compromising communication includes one partner pressuring the other to discuss concerns while the other partner withdraws. We examined whether relationship intimacy mediated the association between communication and couples’ distress by studying couples coping with early stage prostate cancer [21]. Results indicated that the association between mutual constructive communication and patient demand-partner withdraw communication with distress could be accounted for by each communication strategy’s influence on relationship intimacy.
To date, there have been three published couple-focused interventions that have addressed relationship intimacy. In one study, survivors were taught methods of addressing sexual concerns with partners [22]. Significant improvements in sexual functioning were reported. Canada and colleagues [23] evaluated a sex therapy intervention for prostate cancer survivors with ED which included spouses in one treatment arm (and not in the other arm). Results suggested the interventions did not have a significant effect on psychological, marital, or sexual outcomes. Northouse and colleagues [24] evaluated a brief education intervention for prostate cancer survivors and their spouses. Results did not indicate significant differences between the intervention and control groups with regard to survivors’ quality of life, but significant group differences were reported for spousal quality of life.
Although bolstering emotional intimacy as a way of improving couples’ adaptation may be an important goal, the majority of studies evaluating methods of addressing emotional intimacy and sexuality have evaluated pharmacological and other medical approaches to improve ED [25–28] rather than address the relationship itself. In this paper, we present a new model of couple therapy for survivors of prostate cancer and their partners, designed to optimize couples’ adaptation to illness challenges by strengthening the quality of their relationship.
When evaluating psychological interventions, it is important to recognize that there are differences with regard to how beneficial psychological interventions are for participants. From a clinical perspective, the identification of subgroups of participants who may benefit more is important because interventions can be targeted to those subgroups [29]. Several studies of individual-level psychological interventions for cancer survivors have suggested that survivors who start the intervention with fewer personal resources such as greater distress [30, 31] and less support [32] benefit most from psychological interventions. However, possessing psychological resources such as optimism [33] and using specific coping strategies [34] also contribute to greater therapeutic benefit. Less is known about factors that may moderate couple-level interventions. In the proposed study, we will evaluate whether pre-intervention levels of psychological and relationship functioning influence treatment outcome. We propose that the new couple-focused intervention will be more effective among individuals beginning treatment with fewer personal resources (i.e., greater distress) and fewer relationship resources (i.e., less relationship satisfaction and poorer communication).
The purpose of the present study was to conduct a pilot evaluation of a conjoint intimacy-enhancing therapy (IET) for men diagnosed with prostate cancer and their partners. This study was considered a pilot investigation because the goal was to examine the initial efficacy of this newly-developed intervention in a relatively small sample and to identify couples for whom this intervention may be most beneficial for a future larger scale trial. Using the Relationship Intimacy Model of Cancer Adaptation [20], we developed a five session intervention designed to improve communication about cancer-related concerns with a focus on the effects of the cancer and its treatment on relationship intimacy. There were three aims. The first aim was to evaluate the impact IET versus Usual Care (UC) on survivor and partner psychological outcomes including distress and well-being and on relationship outcomes including relationship satisfaction and intimacy. The second aim was to evaluate the impact of IET on relationship communication. The third aim was to evaluate the role of pre-intervention levels of each outcome variable on the effects of IET on that outcome. We hypothesized that IET would result in lower levels of distress, greater relationship satisfaction, higher relationship intimacy, and better communication and that IET would have more beneficial effects upon survivors and partners evidencing greater pre-intervention distress, lower relationship quality, and poorer communication. Our ultimate goal was to examine the effects of the couple-focused intervention that would hopefully compliment rehabilitative sexual therapy offered in a sexual medicine clinic, but sexual functioning was not the focus of our intervention.
Materials and Methods
Participants
The sample was comprised of men diagnosed with localized prostate cancer seen at two cancer centers in the Northeastern United States [Memorial Sloan Kettering Cancer Center (MSKCC) and Fox Chase Cancer Center (FCCC)]. Eligibility criteria for survivors were: diagnosed with localized prostate cancer in the last year, Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 [35], and married or living with a significant other of either gender. In addition, survivors and partners had to be 18 years or older, live within a two hour commuting distance of the center from which they were recruited, be English speaking, and not have a hearing impairment.
Procedure
Participants were approached either after an outpatient visit or by telephone. All participants signed an informed consent approved by the Institutional Review Boards at both primary sites. After consents and surveys were received, participants were randomly assigned to Intimacy-Enhancing Therapy (IET) or to the Usual Care control condition (UC). The two assessment time points were pre-intervention (baseline) and two months post-baseline. Couples were mailed surveys either after session 5 in IET or 8 weeks after the baseline survey (for UC and IET participants who dropped out of therapy). A two month time frame was selected so the second assessment corresponded to the end of IET sessions.
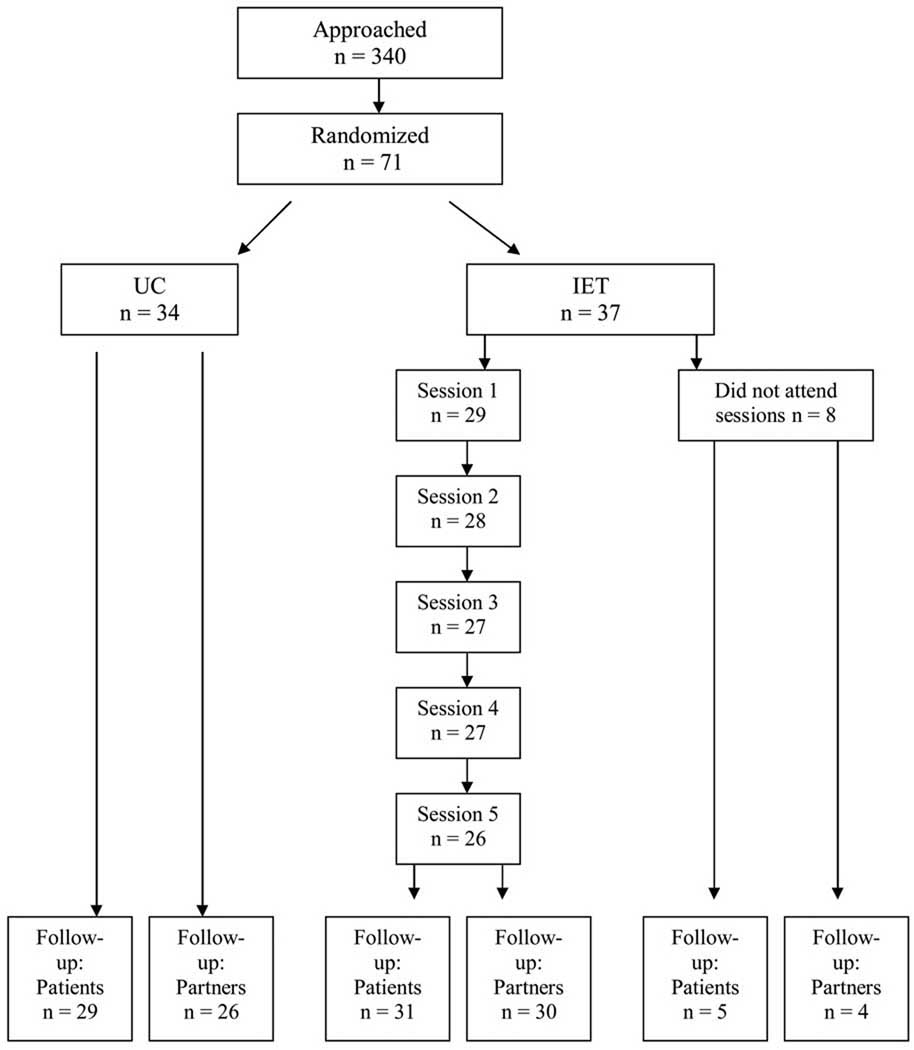
As shown in the CONSORT schema in Figure 1, 340 couples were approached. Seventy-one couples consented and completed the baseline survey (21% acceptance). The most common reasons for refusal were that the study would take “too much time” and that they would not benefit from participation. Comparisons were made between survivor participants and refusers on available data. Participants were significantly younger and had been diagnosed for a longer period of time. The acceptance rate at MSKCC was significantly higher (24%) than FCCC (19%).
Figure 1.
CONSORT Schema
Participants who were assigned to IET but did not attend sessions were asked to complete follow-up surveys. Because intent to treat analyses were conducted, the number of participants who declined participation in sessions but completed follow-up surveys is presented separately in Figure 1 from the number of participants who attended one or more intervention sessions and completed follow-up surveys.
Interventions
IET
This intervention consisted of five 90 minute couples’ sessions. The treatment was manualized and is available upon request. Content focused on improving couples’ ability to comfortably share their thoughts and feelings regarding cancer, promote mutual understanding and support regarding their own and one another’s cancer experience, facilitate constructive discussion of cancer concerns, and to enhance and maintain emotional intimacy. Sessions contained didactic content, in-session skill practice, and home practice assignments. Techniques were drawn from cognitive-behavioral and behavioral marital therapy. Basic communication skills techniques were adapted from the Prevention and Relationship Enhancement Program [36] and from Gottman and colleagues’ communication skills intervention [37] and adapted to the context of dealing with prostate cancer.
UC
Participants assigned to UC received standard psychosocial care, which was the same at both sites: Social work consultations are routinely provided for all survivors at both centers. If indicated, a referral to a psychiatrist or psychologist was provided by physicians at each site.
Interventionists
Five therapists provided the intervention. Therapists underwent five hours of training in the manual-based IET. To facilitate treatment fidelity, the IET manual was structured and there were handouts. Monthly group supervision was provided. Sessions were audiotaped for treatment fidelity purposes.
Instruments
Primary Outcomes–Psychological Functioning
Psychological Distress
The Psychological Distress scale of the Mental Health Inventory [38] consists of 24 items assessing depressive and anxiety symptoms. Higher scores indicate more distress. The coefficient alpha for survivors was .96 at both time points, and the coefficient alpha for partners was .94 at both time points.
Psychological Well-Being
The Psychological Well-Being scale of the Mental Health Inventory [38] consists of 15 items assessing satisfaction with life, a sense of hopefulness about the future, and feelings of calmness. Higher scores indicate greater well-being. The coefficient alpha for survivors was .94 and .95 at Time 1 and 2, respectively, and the coefficient alpha for partners was .95 and .93 at Time 1 and 2, respectively.
Cancer-Specific Distress
The Impact of Events Scale [39] is a 15-item scale which measures the severity of intrusive thoughts, worries, and feelings about having (or one’s spouse having) cancer, avoidance, and numbing. Higher scores indicate greater distress. The coefficient alpha for survivors was .92 and .94 at baseline and Time 2, respectively, and the coefficient alpha for partners was .94 at both time points.
Cancer Concerns
We developed a face valid scale to assess this construct. Survivors rated the degree to which they were concerned about ten cancer-related problems. Partners rated the same items. However, partner concerns about the survivor’s symptoms were rated. Items were averaged for analyses. Higher scores indicated greater concerns. The coefficient alpha for survivors was .86 at both time points. The coefficient alpha for partners was .81 and .76 at baseline and Time 2, respectively.
Primary Outcomes-Relationship Functioning
Relationship Satisfaction
The 32-item Dyadic Adjustment Scale (DAS) is the most widely used measure of relationship functioning and satisfaction [40]. Scores can range from 0 to 151; scores below 97 indicate relationship distress. Higher scores indicate greater satisfaction. The coefficient alpha for survivors was .90 and .92 at baseline and Time 2, respectively, and the coefficient alpha for partners was .92 at both time points.
Relationship Intimacy
The Personal Assessment of Intimacy in Relationships (PAIR) [41] is a 6-item scale assessing emotional closeness. It has been used in studies of relationship intimacy among healthy married couples [42]. The coefficient alpha for survivors was .84 and .82 at baseline and Time 2, respectively, and the coefficient alpha for partners was .85 and .90 at baseline and Time 2, respectively. An item mean is used in analyses and higher scores indicate greater intimacy.
Secondary Outcomes-Relationship Communication
Self-disclosure
We used a 3-item measure adapted from Laurenceau and colleagues [43] and our previous work [44]. Participants rated the degree to which they disclosed thoughts, information, and feelings about cancer to the partner in the past week with higher scores indicating greater self-disclosure. The coefficient alpha for survivors was .93 at both time points and the coefficient alpha for partners was .96 and .94 at baseline and Time 2, respectively.
Perceived Partner Disclosure
We used a 3-item measure adapted from Laurenceau and colleagues [43] and used in our previous research [44]. Participants rated the degree to which their partner disclosed thoughts, information, and feelings and concerns about cancer to them in the past week. Higher scores indicated greater partner disclosure. The coefficient alpha for survivors was .92 and .97 at baseline and Time 2, respectively, and the coefficient alpha for partners was .95 and .91 at baseline and Time 2, respectively.
Perceived Partner Responsiveness
We used a four item measure adapted from Laurenceau and colleagues [43] and used in our previous research [44]. Participants rated the degree to which they felt accepted, understood, cared for, and validated in the past week when discussing cancer-related topics with higher scores indicating greater responsiveness. The coefficient alpha for survivors was .90 and .92 at baseline and Time 2, respectively, and the coefficient alpha for partners was .87 and .81 at baseline and Time 2, respectively.
Mutual Constructive Communication
The Mutual Constructive Communication subscale of the Communications Pattern Questionnaire (CPQ) [45–47] is a 5-item scale adapted for use in the cancer setting by asking the couple to rate how they typically deal with cancer-related stressors or problems [48]. The coefficient alpha for survivors was .85 and .81 at baseline and Time 2, respectively, and the coefficient alpha for partners was .83 and .81 at baseline and Time 2, respectively.
Demand-withdraw communication
The Demand-Withdraw subscale of the CPQ [45–47] is a 6-item scale that has been adapted for use in the cancer setting by asking respondents to rate how they typically deal with cancer-related stressors or problems. Three items assess survivor demand-partner withdrawal and three items assess partner’s demand-survivor withdrawal. The coefficient alpha for survivors was .81 and .78 at baseline and Time 2, respectively, and the coefficient alpha for partners was .78 and .75 at baseline and Time 2, respectively.
Covariates
Demographic and medical information
Age, relationship length, education, and ethnicity were included as possible covariates. Cancer stage and Gleason score at baseline were also used.
Erectile, bowel, and urinary function
The Erectile Function Domain subscale of the IIEF was administered [49]. This scale consisted of six items assessing erection frequency, firmness, penetration ability, and difficulty maintaining an erection. Scores between 26 and 30 indicate no ED, scores between 18 and 25 indicate mild ED, scores between 11 and 17 indicate moderate ED, and scores between 6 and 10 indicate severe ED [50]. The urinary and bowel scales of the UCLA Prostate Cancer Index [51] were used to assess symptomatology. Coefficient alphas were .87 for the IIEF ED scale, .90 for the PCI-Urinary function scale, and .75 for the PCI-bowel function scale.
Treatment Evaluation and Fidelity
A treatment evaluation survey adapted from Borkovec and Nau [52] was administered at Time 2. Fourteen items assessed how helpful each session was, the degree to which the participant learned something new, whether the topics were important, the sessions interesting, helpful, and tuned into needs. Participants reported the percentage of home assignments completed. The fidelity checklist consisted of topics covered, whether in-session exercises were conducted, and whether home assignments were given. The fidelity score consisted of the number of topics completed divided by the total number of fidelity criteria.
Results
Treatment Attendance, Fidelity, and Evaluation
Seventy-three percent of IET couples attended four or five sessions. Approximately five percent of IET participants attended between one and three sessions. Another 21.6% of IET participants attended no sessions after being assigned to IET (pre-treatment drops). Of the 138 sessions conducted, 114 were taped. Treatment fidelity was rated on 33% of these 114 sessions (n = 38). The average fidelity across all sessions rated was 87.4%. Average session fidelity ranged from 80% (for Session 5) to 93% (for Session 2). In terms of treatment evaluation, the average patient rating of the success of sessions was 3.2 (SD = .56) (3 = quite successful, 4 = extremely successful) and the average partner rating was also 3.2 (SD = .62). Survivors felt they learned something new (M = 4.0, SD = 1.0) (5 = strongly agree), felt the topics were important (M = 4.1, SD = .99), and felt the sessions were helpful (M = 4.2, SD = .85). Similar ratings were provided by partners. Self-reported average homework completion was 72% for survivors (SD = 29.0) and partners (SD= 24.8).
Descriptive Results
Sample characteristics are shown in Table 1. The sample was primarily Caucasian and relatively well-educated. Scores on the IIEF Erectile Dysfunction (ED) subscale indicated that 51% of men had severe ED while 7% of men had moderate ED. The average levels of baseline distress among survivors (M = 43.1, SD = 15.3) and partners (M = 46.4, SD = 14) were similar to those reported by Veit and Ware [36] in their normative sample (M = 47.5, SD = 15.4).
Table 1.
Descriptive Information for Sample
| Full Sample | UC | IET | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Survivor | Partner | Survivor | Partner | Survivor | Partner | |||||||||||||||||||
| Variable | n | % | M | SD | n | % | M | SD | n | % | M | SD | n | % | M | SD | n | % | M | SD | n | % | M | SD |
| Age (yes) | 60 | 8.3 | 55.7 | 8.5 | 60.0 | 7.9 | 55.8 | 9.3 | 60 | 8.8 | 55.7 | 7.9 | ||||||||||||
| Gender | ||||||||||||||||||||||||
| Men | 71 | 100 | 2 | 2.8 | 34 | 100 | 0 | 0 | 0 | 0 | 2 | 5.4 | ||||||||||||
| Women | 0 | 0 | 69 | 97.2 | 0 | 0 | 34 | 100 | 37 | 100 | 35 | 94.6 | ||||||||||||
| Ethnicity | ||||||||||||||||||||||||
| White | 63 | 88.7 | 59 | 83.1 | 29 | 85.3 | 27 | 79.4 | 34 | 91.9 | 32 | 86.5 | ||||||||||||
| Non-white | 8 | 11.3 | 8 | 11.3 | 6 | 14.7 | 5 | 14.6 | 3 | 8.1 | 3 | 8.1 | ||||||||||||
| Missing | 0 | 0 | 4 | 5.6 | 0 | 0 | 2 | 2.9 | 0 | 0 | 2 | 5.4 | ||||||||||||
| Education level | ||||||||||||||||||||||||
| Grade school | 0 | 40.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||||||||||||
| Partial high school | 3 | 4.2 | 0 | 0 | 0 | 0 | 0 | 3 | 8.1 | 0 | 0 | |||||||||||||
| High school | 5 | 7.0 | 15 | 1 | 2.9 | 4 | 2.9 | 4 | 10.8 | 11 | 29.7 | |||||||||||||
| Some college | 9 | 12.7 | 11 | 3 | 8.8 | 4 | 8.8 | 6 | 16.2 | 7 | 18.9 | |||||||||||||
| College | 17 | 23.9 | 12 | 8 | 23.5 | 7 | 23.5 | 9 | 24.3 | 13 | 35.1 | |||||||||||||
| Post grad | 37 | 52.1 | 32 | 22 | 84.7 | 19 | 84.7 | 15 | 40.5 | 13 | 35.1 | |||||||||||||
| Missing | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2.7 | |||||||||||||
| Marital status | ||||||||||||||||||||||||
| Married | 69 | 97.2 | 66 | 93.0 | 33 | 97.1 | 32 | 94.1 | 36 | 97.3 | 33 | 89.2 | ||||||||||||
| Cohabitating | 2 | 2.8 | 4 | 5.6 | 1 | 2.9 | 2 | 5.9 | 1 | 2.7 | 2 | 5.4 | ||||||||||||
| Missing | 0 | 0 | 1 | 1.4 | 0 | 0 | 2 | 5.4 | ||||||||||||||||
| Relationship length (years) | 27.0 | 15.1 | 26.8 | 15.1 | 25.8 | 15.4 | 25.8 | 15.6 | 27.7 | 14.6 | 27.7 | 14.6 | ||||||||||||
| Stage of disease | ||||||||||||||||||||||||
| 1 | 11 | 15.5 | 8 | 23.5 | 3 | 8.1 | ||||||||||||||||||
| 2 | 60 | 84.5 | 26 | 76.5 | 34 | 91.9 | ||||||||||||||||||
| Gleason score | ||||||||||||||||||||||||
| 6 | 41 | 57.7 | 21 | 61.8 | 20 | 54.1 | ||||||||||||||||||
| 7 | 25 | 35.2 | 10 | 29 | 15 | 40.5 | ||||||||||||||||||
| 8 | 2 | 2.8 | 2 | 2 | 5.4 | |||||||||||||||||||
| 9 | 3 | 4.2 | 1 | 0 | 0 | |||||||||||||||||||
| ECOG | ||||||||||||||||||||||||
| 0 | 71 | 100 | 34 | 100 | 37 | 100 | ||||||||||||||||||
| Treatment | ||||||||||||||||||||||||
| Surgery only | 44 | 62.0 | 24 | 70.6 | 20 | 54.1 | ||||||||||||||||||
| Radiation only | 20 | 28.1 | 7 | 20.5 | 13 | 35.8 | ||||||||||||||||||
| Hormone therapy | 3 | 4.2 | 0 | 0 | 1 | 2.7 | ||||||||||||||||||
| Radiation and hormone therapy | 0 | 0 | 2 | 5.8 | 0 | 0 | ||||||||||||||||||
| Has not begun treatment | 4 | 5.6 | 1 | 2.9 | 3 | 8.1 | ||||||||||||||||||
| Time since diagnosis (months) | 8.0 | 5.5 | 7.3 | 3.5 | 8.7 | 6.9 | ||||||||||||||||||
Note: ECOG – Eastern Cooperative Oncology Group; IET= Intimacy-enhancing therapy; IIEF = International Index of Erectile Dysfunction
Statistical Analyses
Initially, all variables were assessed to determine if they were normally distributed. In addition, potential covariates were examined by regressing each post-assessment outcome on a set of demographic and medical variables (age, education, income, marital status, Gleason score, urinary, bowel, and erectile function). Any covariate evidencing significance was included in subsequent analyses.
Given the nature of the research design, treatment effects were assessed using an Analysis of Covariance (ANCOVA) in which the baseline value of the outcome was the covariate. Outcomes for the survivors and their partners were analyzed separately. Since one of the assumptions of ANCOVA is the presence of a non-significant interaction between the treatment condition and the covariate, this interaction term was evaluated for each model. Since there was attrition from the study, an intent to treat (ITT) approach was employed. If post-intervention information was missing for any outcome, the baseline value for that outcome was carried forward and substituted for the missing value.
Treatment Effects on Psychological and Relationship Functioning
Survivors
There were no significant treatment main effects for general distress, cancer-specific distress, cancer concerns, relationship satisfaction, and relationship intimacy. After controlling for significant covariates, there was a marginally significant (t (61) = 1.79; p = 0.08) treatment effect on psychological well-being in favor of IET (M = 67.47) compared to UC (M = 65.02).
Partners
There were no significant treatment differences found for general distress, well-being, cancer-specific distress, cancer concerns, relationship satisfaction, and relationship intimacy.
Treatment Effects on Relationship Communication
There were no significant treatment differences for relationship communication outcomes for either survivors or partners.
Moderator Effects
Survivors
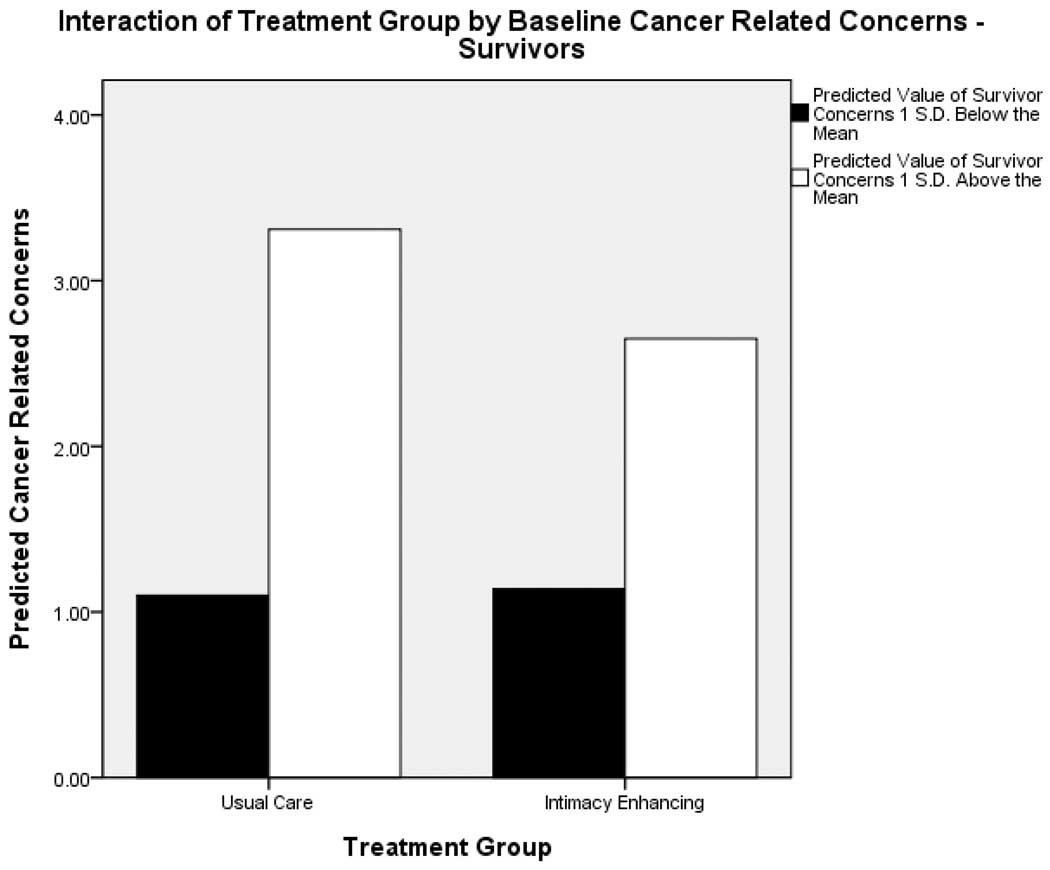
With regard to psychological and relationship outcomes, there were no significant interactions found between intervention group and baseline levels of general distress, well-being, cancer-specific distress, relationship satisfaction, and relationship intimacy. One marginally significant moderator effect was found for cancer concerns. This interaction effect (as well as all other interaction effects) is shown in Table 2. There was a marginally significant (t (64) = −1.68; p = 0.097) treatment group by baseline cancer concerns interaction. To understand this interaction better, treatment effects were evaluated at 1 S.D. above and below the baseline mean on concerns. The interaction is plotted in Figure 2. At 1 S.D. above the mean, there was a significant reduction in concerns at Time 2 for survivors in the IET group compared to controls. At 1 S.D. below the baseline mean, there were no significant treatment differences between the two groups.
Table 2.
Interaction Effects for Survivors and Partners Above and Below the Baseline Levels of Primary and Secondary Outcomes
| Outcome | Predicted Score IET group |
Predicted Score UC group |
t- value | df | p-value | 95% C.I. Intervention Group |
|---|---|---|---|---|---|---|
| Survivors | ||||||
| Interaction effects at 1 S.D below the mean | ||||||
| Cancer-related concerns | 1.14 | 1.10 | 0.15 | 64 | 0.8803 | −0.55, 0.64 |
| Self-disclosure | 15.06 | 10.72 | 3.50 | 67 | 0.0008 | 1.86, 6.81 |
| Partner disclosure | 14.63 | 10.40 | 3.27 | 67 | 0.0017 | 1.65, 6.82 |
| Partner responsiveness | 17.24 | 15.82 | 3.26 | 62 | 0.0341 | 0.11, 2.72 |
| Interaction effects at 1 S.D above the mean | ||||||
| Cancer-related concerns | 2.65 | 3.31 | −2.34 | 64 | 0.0221 | −1.22,−0.10 |
| Self-disclosure | 16.95 | 19.85 | −2.34 | 67 | 0.0221 | −5.37,−0.43 |
| Partner disclosure | 17.82 | 19.93 | −1.62 | 67 | 0.1108 | −4.72, 0.50 |
| Partner responsiveness | 20.61 | 21.22 | −1.07 | 62 | 0.2883 | −1.75, 0.53 |
| Partners | ||||||
| Interaction effects at 1 S.D below the mean | ||||||
| Cancer-specific distress | 2.80 | −1.98 | 1.79 | 65 | 0.0782 | −0.55, 10.11 |
| Relationship satisfaction | 113.13 | 102.43 | 3.94 | 63 | 0.0002 | 5.33, 16.30 |
| Relationship intimacy | 3.72 | 3.03 | 3.42 | 66 | 0.0011 | 0.29. 1.10 |
| Mutual constructive communication | 32.25 | 25.71 | 3.70 | 63 | 0.0005 | 3.01, 10.07 |
| Demand-withdraw communication | 8.38 | 5.83 | 1.28 | 61 | 0.2068 | −1.44, 6.54 |
| Interaction effects at 1 S.D above the mean | ||||||
| Cancer-specific distress | 16.72 | 22.90 | −2.31 | 65 | 0.0239 | −11.52, −0.86 |
| Relationship satisfaction | 129.42 | 134.17 | −2.12 | 63 | 0.0379 | −11.17, −0.33 |
| Relationship intimacy | 4.38 | 4.87 | −2.49 | 66 | 0.0153 | −0.89, −0.10 |
| Mutual constructive communication | 41.27 | 42.74 | −0.80 | 63 | 0.4248 | −5.11, 2.18 |
| Demand-withdraw communication | 18.35 | 23.07 | −2.34 | 61 | 0.0227 | −8.75, −0.68 |
Figure 2.
Plot of the Interaction between Treatment Group × Baseline Survivor Cancer Concerns
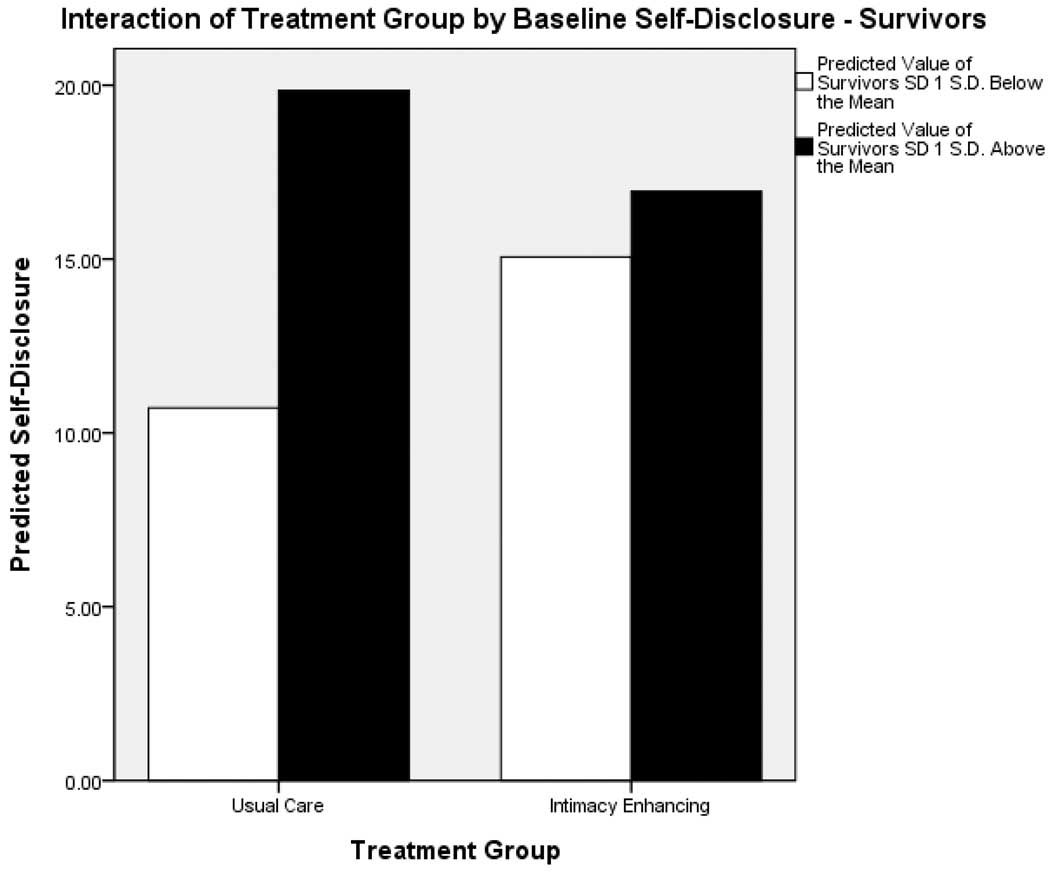
With regard to communication, there were three significant moderator effects found for self-disclosure, perceived partner disclosure, and perceived responsiveness, but no interaction effects found for mutual constructive communication and demand-withdraw communication. First, there was a significant (t (67) = −4.09; p = 0.0001) interaction between treatment group and baseline survivor self-disclosure. This interaction is plotted in Figure 3. As can be seen in Table 2, at 1 S.D. below the baseline mean on self-disclosure, there was a significant increase in disclosure at Time 2 for those in the IET condition compared to controls. However, at 1 S.D. above the mean on baseline self-disclosure, there was a significant decline in self-disclosure for those in the IET condition compared to those in UC. Second, the interaction between perceived partner disclosure at baseline and treatment group was significant (t (67) = −3.43; p = 0.0010). At 1 S.D. below the baseline mean on this measure, there was a significant increase in perceived partner disclosure at Time 2 for those in IET compared to UC. At 1 S.D. above the mean, there were no group differences at Time 2. Third, the interaction between baseline partner responsiveness was significant (t (62) = −2.20; p = 0.0314). At 1 S.D. below the baseline mean on this measure, there was a significant increase in perceived partner responsiveness at Time 2 for those in the IET compared to UC. At 1 S.D. above the mean, there were no treatment differences between the IET and UC groups at Time 2.
Figure 3.
Plot of the Interaction between Treatment Group × Baseline Survivor Self-Disclosure
Partners
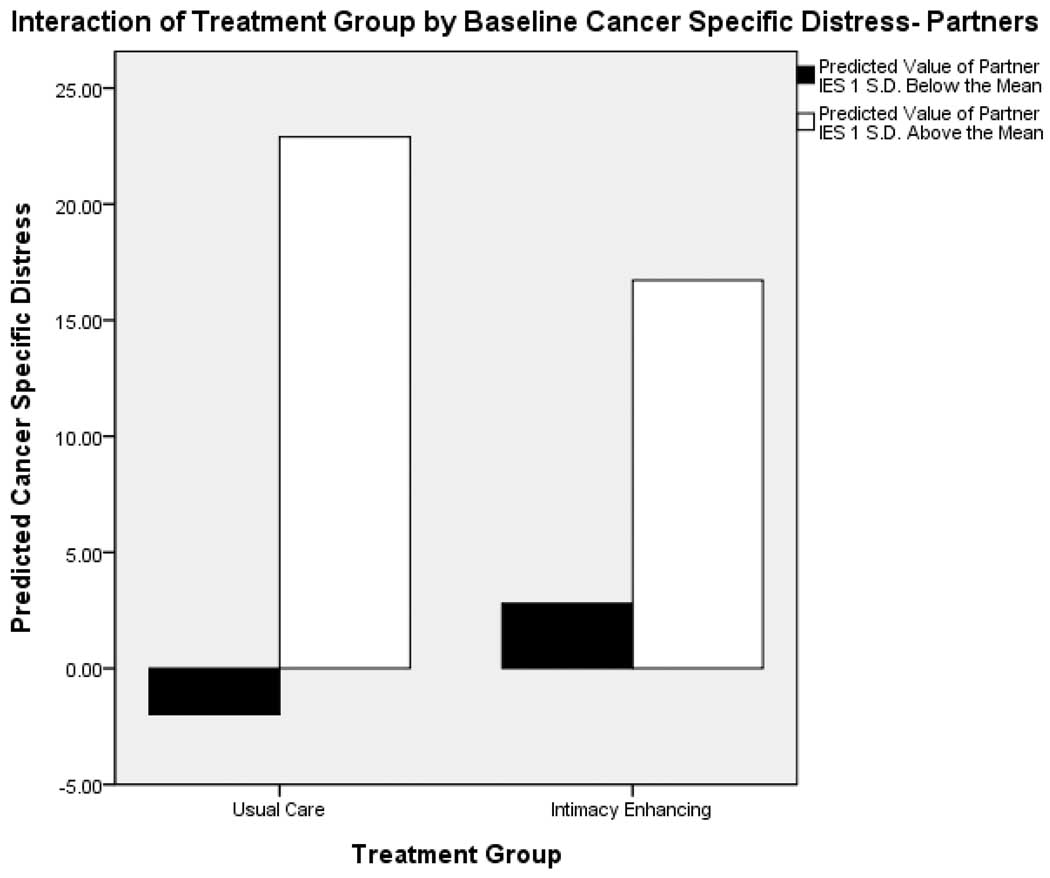
There were three moderator effects noted for partner psychological and relationship functioning outcomes. The first moderator effect was found for baseline cancer-specific distress (IES). After controlling for covariates, there was a significant (t (65) = −2.91; p = 0.005) interaction between intervention group and baseline cancer-specific distress. The interaction is plotted in Figure 4. Results are shown in Table 2. At 1 S.D. above the mean on baseline cancer-specific distress, there was a significant reduction in IES at Time 2 for those in the IET arm compared to UC. However, at 1 S.D. below the mean on baseline IES, there was a marginally significant increase in IES at Time 2 for those in the IET group compared to UC. The second moderator effect was found for baseline relationship satisfaction (DAS). After controlling for covariates, the interaction between intervention group and relationship satisfaction at baseline was significant (t (63) = −4.24; p < 0.0001). As can be seen in Table 2, at 1 S.D. below the baseline DAS mean, there was a significant increase in DAS scores by Time 2 for those in the IET condition compared to UC. However, the situation was reversed when examining treatment effects at 1 S.D. above the mean on baseline DAS in that scores were significantly lower in IET compared to UC. The third moderator effect was found for baseline relationship intimacy. The interaction between baseline relationship intimacy and treatment condition was significant (t (66) = −4.16; p < 0.0001). At 1 S.D. below the baseline mean on this measure, there was a significant increase in relationship intimacy at Time 2 for those in the IET condition compared to UC. However, at 1 S.D. above the mean, there was a significant decline in relationship intimacy at the Time 2 for those in the IET condition compared to UC.
Figure 4.
Plot of the Interaction between Treatment Group × Baseline Partner Cancer-specific distress
There were interactions between intervention group and two communication variables: baseline mutual constructive communication and demand-withdrawal communication. These interaction effects are shown in Table 2. The interaction between baseline mutual constructive communication (MCC) and intervention group was significant (t (63) = −3.17; p = 0.0023). At 1 S.D. below the baseline mean on this measure, there was a significant increase in MCC at Time 2 for those in the IET group compared to UC. At 1 S.D. above the baseline mean, there were no significant group differences. There was a significant (t (61) = −2.50; p = 0.0150) interaction between baseline demand-withdraw communication and intervention group on this outcome at Time 2. At 1 S.D. above the mean on this measure at baseline, there was a significant decline at Time 2 in demand-withdraw communication reported by those in IET compared to UC. At 1 S.D. below the baseline mean, there were no treatment group differences at Time 2.
Discussion
The goal of this pilot study was to evaluate a newly developed couple-focused intervention designed to improve psychological and relationship functioning among men diagnosed with early stage prostate cancer and their partners. The key finding was that, other than a marginal effect upon survivors’ well-being (defined as the level of satisfaction with life, a sense of hopefulness about the future, and feelings of calmness), IET did not have an effect upon psychological, relationship, or communication outcomes for all survivors or partners. Rather, the treatment’s effects were moderated by both individual distress and by relationship characteristics that the individual and couple brought to the first IET session. IET couples who began with fewer personal or relationship resources showed significant improvements in that outcome. Among survivors and partners with higher individual or relational functioning, IET had either no effect or a detrimental effect. In the discussion that follows, we will explore the significance of these findings as well as study limitations, clinical implications, and directions for future research.
Our initial prediction was that IET would reduce couples’ distress, improve their well-being, and improve relationship satisfaction, intimacy, and communication. Other than a marginal beneficial effect upon survivor’s well-being, this intervention did not improve outcomes for well-functioning survivors and their partners as compared with Usual Care. These findings are relatively consistent with the results of previous couple-focused interventions for men diagnosed with prostate cancer and their partners. Canada and colleagues [23] evaluated the impact of a four session sex therapy intervention for prostate cancer survivors and their partners, where men were randomized to receive the intervention alone or with their partner. Analyses of treatment completers indicated no between group differences on psychological, marital, or sexual outcomes. Northouse and colleagues [24] examined the effects of a three session education and supportive intervention for men with prostate cancer and their spouses. Although some treatment effects were noted at the early follow-up they were not maintained at the later follow-ups. Our findings add to the literature suggesting that couple-focused interventions for men diagnosed with prostate cancer may prove challenging if they are offered to all couples.
Although main effects for IET were not present, a benefit among individuals and couples with specific characteristics was found. These characteristics include survivors with greater cancer concerns and less or poorer communication and partners reporting greater cancer-specific distress, lower relationship satisfaction and intimacy, and poorer communication. Pre-treatment factors influencing the efficacy of couple-focused interventions for men with prostate cancer have not been evaluated in previous work, and therefore it is not known whether the previously studied interventions of Canada [23] and Northouse [24] may have proven effective for subgroups of survivors and partners. However, there is one couple-based intervention trial for early stage breast cancer survivors that found that pre-intervention relationship quality and communication (e.g., how supportive the spouse was to the patient) moderated the effects of a couple-focused group intervention [34, 53]. Our findings suggesting that men with more cancer concerns and partners with more cancer-specific distress are consistent with a number of other studies of survivors of other types of cancers that have found that survivors with greater distress [30,54] and individuals possessing fewer psychological resources [22,30,32] benefit more from psychological interventions. In addition, our findings indicating that relationship satisfaction, intimacy, and communication moderated IET’s effects are consistent with the limited previous work in the oncology setting which has suggested that relationship factors moderate treatment effects. Helgeson and colleagues [32] found that group peer support was more effective for women who evidenced less pre-intervention partner support and more negative interactions. Our findings extend this work by suggesting that both patient and partner relationship vulnerability factors contribute to outcomes of couple-based interventions. Our findings also add to a growing recognition in the field of psycho-oncology that delivering psychological interventions broadly carries no benefit, and that targeting interventions to high-risk groups may ultimately prove more effective [52].
Unfortunately, this pilot study suggested IET has the potential for adverse effects, particularly among partners. Partners with low levels of pre-intervention cancer-specific distress who were enrolled in IET evidenced a significant increase in distress and partners reporting high levels of marital satisfaction who were enrolled in IET also reported a significant decline in relationship satisfaction. It is possible that partners who were not feeling distressed may have become more aware of their own and the survivors’ concerns and stresses during the IET sessions, when these issues were discussed with their partner, resulting in increased distress. Our follow-up was brief and this distress may prove temporary. In the same way, among highly martially-satisfied partners, cancer- and non-cancer related relationship issues may have been brought up during sessions and subsequently resulted in lower marital satisfaction. Finally, men who were high self-disclosers who participated in IET reported reductions in self-disclosure, perhaps because they became aware of its impact on their partners during sessions. Taken together with the fact that IET did not significantly alter distress, relationship intimacy, and communication among survivors and partners with higher psychological and relationship functioning, our findings underscore the need to target interventions to lower functioning survivors, partners, and relationships. Our results also underscore the fact that survivors and partners may derive different benefits from couples’ treatments.
Study Limitations
The main limitation is that the sample size was relatively small and our follow-up assessment occurred immediately after the treatment. The cohort was primarily white and middle class, relatively well-educated, and heterosexual. The ability to generalize our findings to other populations of men with prostate cancer and their partners is therefore limited. Although session attendance and survey follow-up completion rates were relatively high, there was a high study refusal rate which may have been lower if we offered subject incentives for survey completion and session attendance. Study participants were younger and had been diagnosed for a longer period of time and, therefore, the intervention may have less applicability to and interest for older survivors and recently diagnosed men. Overall, future research should replicate the findings with a larger sample and a longer follow-up.
Implications for Clinical Practice and Future Research
Although the clinical significance of these findings awaits further replication, our initial results suggest IET may prove beneficial for couples who are having difficulties dealing with prostate cancer, those who report less relationship satisfaction, and/or communication deficits. For these couples, our pilot study has shown the ability for IET to reduce elevated cancer concerns, promote self-disclosure, and improve perceptions of partner disclosure and responsiveness, while also reducing partners’ cancer distress and enhancing their relationship satisfaction and communication.
Given that a key goal was to enhance relationship closeness, it was surprising that IET did not result in improved relationship intimacy for survivors in either the main effect or moderator effect analyses. In future research, it may be helpful to tailor the intervention to barriers to intimacy that survivors report, including fear of recurrence, worries about physical symptoms such as urinary leakage, ED, and other cancer concerns that may not have been addressed adequately in sessions so that survivor and partner can address methods of coping with these concerns. It may also be helpful to interview survivors who have completed IET sessions to determine whether there were unaddressed issues with intimacy that were not discussed in sessions.
Overall, our findings add to the literature on the efficacy of couple-based approaches for men diagnosed with prostate cancer by suggesting that such interventions may be most effective for individuals and for couples possessing fewer personal and relationship resources and may be ineffective for couples who are not distressed.
References
- 1.Burnett A, Aus G, Canby-Hagino E, et al. Erectile function outcome reporting after clinically localized prostate cancer treatment. J Urol. 2007;178:597–601. doi: 10.1016/j.juro.2007.03.140. [DOI] [PubMed] [Google Scholar]
- 2.Bokhour B, Clark J, Inui T, Silliman R, Talcott J. Sexuality after Treatment for Early Prostate Cancer. J Gen Intern Med. 2001;16:649–655. doi: 10.1111/j.1525-1497.2001.00832.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elliott S, Latini DM, Walker LM, Wassersug R, Robinson JW. Androgen Deprivation Therapy for Prostate Cancer: Recommendations to Improve Patient and Partner Quality of Life. J Sex Med. 2010;7:2996–3010. doi: 10.1111/j.1743-6109.2010.01902.x. [DOI] [PubMed] [Google Scholar]
- 4.O'Leary M, Althof S, Cappelleri J, Crowley A, Sherman N, Deuttagupta S. Self-Esteem, Confidence and Relationship Satisfaction of Men With Erectile Dysfunction Treated With Sildenafil Citrate: A Multicenter, Randomized, Parallel Group, Double-Blind, Placebo Controlled Study in the United States. J Urol. 2006;175:1058–1062. doi: 10.1016/S0022-5347(05)00418-0. [DOI] [PubMed] [Google Scholar]
- 5.Nelson CJ, Deveci S, Stasi J, Scardino PT, Mulhall JP. Sexual bother following radical prostatectomyjsm. J Sex Med. 2010;7(1 Pt 1):129–133. doi: 10.1111/j.1743-6109.2009.01546.x. [DOI] [PubMed] [Google Scholar]
- 6.Sadovsky R, Basson R, Krychman M, Morales AM, Schover L, Wang R, et al. Cancer and sexual problems. J Sex Med. 2010;7(1 Pt 2):349. doi: 10.1111/j.1743-6109.2009.01620.x. [DOI] [PubMed] [Google Scholar]
- 7.Malinski SL, Heilemann MV, McCorkle R. Mastery of postprostatectomy incontinence and impotence: his work, her work, our work. Oncol Nurs Forum. 2001;28:985–992. [PubMed] [Google Scholar]
- 8.Davison BJ, Degner LF, Morgan TR. Information and decision-making preferences of men with prostate cancer. Oncol Nurs Forum. 1995;22:1401–1408. [PubMed] [Google Scholar]
- 9.Cliff A, Macdonagh R. Psychosocial morbidity in prostate cancer: ll. A comparsion of patients and partners. BJU International. 2000;86:834–839. doi: 10.1046/j.1464-410x.2000.00914.x. [DOI] [PubMed] [Google Scholar]
- 10.Kornblith AB, Herr HW. Quality of Life of Patients with Prostate Cancer and Their Spouses. Cancer. 1994;73:2791–2802. doi: 10.1002/1097-0142(19940601)73:11<2791::aid-cncr2820731123>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 11.Couper J, Bloch S, Love A, Macvean M, Duchesne GM, Kissane D. Psychosocial adjustment of female partners of men with prostate cancer: a review of the literature. Psychooncology. 2006;15:937–953. doi: 10.1002/pon.1031. [DOI] [PubMed] [Google Scholar]
- 12.Sanders S, Pedro L, Bantum E, Galbraith M. Couples surviving prostate cancer: Long-term intimacy needs and concerns following treatment. Clin J Oncol Nurs. 2006;10:503–508. doi: 10.1188/06.CJON.503-508. [DOI] [PubMed] [Google Scholar]
- 13.Manne SL, Kissane D, Zaider T, Nelson C. Couples coping with prostate cancer: analysis and intervention. Unpublished data. [Google Scholar]
- 14.Garos S, Kluck A, Aronoff D. Prostate cancer patients and their partners: differences in satisfaction indices and psychological variables. J Sex Marital Ther. 2007;4:1394–1403. doi: 10.1111/j.1743-6109.2007.00545.x. [DOI] [PubMed] [Google Scholar]
- 15.Badr H, Taylor CL. Sexual dysfunction and spousal communication in couples coping with prostate cancer. Psychooncology. 2009;18:735–746. doi: 10.1002/pon.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harden J, Schafenacker A, Northouse L, et al. Couples' experiences with prostate cancer: Focus group research. Oncol Nurs Forum. 2002;29:701–709. doi: 10.1188/02.ONF.701-709. [DOI] [PubMed] [Google Scholar]
- 17.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358:1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 18.Lepore SJ, Helgeson VS. Social Constraints, Intrusive Thoughts, and Mental Health After Prostate Cancer. J Soc Clin Psychol. 1998;17:89–106. [Google Scholar]
- 19.Boehmer U, Clark J. Communication about prostate cancer between men and their wives. J Fam Pract. 2001;50:226–231. [PubMed] [Google Scholar]
- 20.Manne SL, Badr H. Intimacy and relationship processes in couples' psychosocial adaptation to cancer. Cancer. 2008;112:2541–2555. doi: 10.1002/cncr.23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manne S, Badr H, Zaider T, Nelson C, Kissane D. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. J Cancer Surviv. 2009;4:74–85. doi: 10.1007/s11764-009-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Molton IR, Siegel SD, Penedo FJ, et al. Promoting recovery of sexual functioning after radical prostatectomy with group-based stress management: the role of interpersonal sensitivity. J Psychosom Res. 2008;64:527–536. doi: 10.1016/j.jpsychores.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Canada AL, Neese LE, Sui D, Schover LR. Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer. 2005;104:2689–2700. doi: 10.1002/cncr.21537. [DOI] [PubMed] [Google Scholar]
- 24.Northouse LL, Mood DW, Schafenacker A, et al. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007;110:2809–2818. doi: 10.1002/cncr.23114. [DOI] [PubMed] [Google Scholar]
- 25.Miles CL, Candy B, Jones L, Williams R, Tookman A, King M. Interventions for sexual dysfunction following treatments for cancer. Cochrane Database Syst Rev. 2007;(4):CD005540. doi: 10.1002/14651858.CD005540.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Seftel AD, Buvat J, Althof SE, McMurray JG, Zeigler HL, Burns PR, et al. Improvements in confidence, sexual relationship and satisfaction measures: results of a randomized trial of tadalafil 5 mg taken once daily. Int J Impot Res. 2009;1(4):240–248. doi: 10.1038/ijir.2009.22. [DOI] [PubMed] [Google Scholar]
- 27.Verheyden B, Roumeguere T, Bitton A, Belger M, Schmitt H. Effects of 12-Month Tadalafil Therapy for Erectile Dysfunction on Couple Relationships: Results from the DETECT Study. J Sex Med. 2009:3458–3468. doi: 10.1111/j.1743-6109.2009.01527.x. [DOI] [PubMed] [Google Scholar]
- 28.Prasad MM, Prasad SM, Hevelone ND, Gu X, Weinberg AC, Lipsitz SR, et al. Utilization of pharmacotherapy for erectile dysfunction following treatment for prostate cancer. J Sex Med. 2010;7(3):1062–1073. doi: 10.1111/j.1743-6109.2009.01644.x. [DOI] [PubMed] [Google Scholar]
- 29.Sherman AC, Mosier J, Leszcz M, et al. Group Interventions for Patients with Cancer and HIV disease: Part III. Moderating Variables and Mechanisms of Action. Int J Group Psychother. 2004;54:347–387. doi: 10.1521/ijgp.54.3.347.40339. [DOI] [PubMed] [Google Scholar]
- 30.Helgeson VS, Lepore SJ, Eton DT. Moderators of the benefits of psychoeducational interventions for men with prostate cancer. Health Psychol. 2006;25:348–354. doi: 10.1037/0278-6133.25.3.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sheard TAB, Maguire P. The effect of psychological interventions on anxiety and depression in cancer patients: result of two meta-analyses. Br J Cancer. 1999;80:1770–1780. doi: 10.1038/sj.bjc.6690596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Helgeson V, Cohen S, Schulz R, Yasko JM. Long-term effects of educational and peer discussion group interventions on adjustment to breast cancer. Health Psychol. 2001;20:387–392. doi: 10.1037//0278-6133.20.5.387. [DOI] [PubMed] [Google Scholar]
- 33.Antoni M, Lehman J, Kilbourn K, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early- stage breast cancer. Health Psychol. 2001;20:20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 34.Manne SL, Ostroff J, Winkel G. Social-cognitive processes as moderators of a couple-focused group intervention for women with early stage breast cancer. Health Psychol. 2007;26:735–744. doi: 10.1037/0278-6133.26.6.735. [DOI] [PubMed] [Google Scholar]
- 35.Zubrod CG, Schneiderman M, Frei E, Brindley C, Gold G, Schnider B. Appriasal of methods for the study of chemotherapy of cancer in man: Comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. J Chronic Dis. 1960;11:17–33. [Google Scholar]
- 36.Markman H, Blumberg S, Stanley S. PREP-Manual for Leaders. PREP educational products, Inc; 1995. [Google Scholar]
- 37.Gottman J, Notarius C, Gonso J, Markman H. Couples Guide to Communication. Research Press; 1976. [Google Scholar]
- 38.Veit CT, Ware JE., Jr The structure of psychological distress and well-being in general populations. J Consult Clin Psychol. 1983;51:730–742. doi: 10.1037//0022-006x.51.5.730. [DOI] [PubMed] [Google Scholar]
- 39.Horowitz M, Wilner N, Alvarez W. Impact of event scale: A measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Spanier GB, Filsinger EE. Marriage and Family Assessment: A Sourcebook for Family Therapy. First ed. Beverly Hills: Sage; 1983. The dyadic adjustment scale; pp. 155–168. [Google Scholar]
- 41.Schaefer MT, Olson DH. Assessing intimacy: The pair inventory. J Marital Fam Ther. 1981:47–60. [Google Scholar]
- 42.Talmadge L, Dabbs JM. Intimacy, conversational patterns, and concomitant cognitive/emotional processes in couples. J Soc Clin Psychol. 1990;9:473–488. [Google Scholar]
- 43.Laurenceau JP, Barrett LF, Pietromonaco PR. Intimacy as an interpersonal process: The importance of self-disclosure, partner disclosure and perceived partner responsiveness in interpersonal exchanges. J Pers Soc Psychol. 1998;74 doi: 10.1037//0022-3514.74.5.1238. [DOI] [PubMed] [Google Scholar]
- 44.Manne SL, Ostroff J, Rini C, Fox K, Goldstein L, Grana G. The interpersonal process model of intimacy: The role of self-disclosure, partner disclosure and partner responsiveness in interactions between breast cancer patients and their partners. J Fam Psychol. 2004;18:589–599. doi: 10.1037/0893-3200.18.4.589. [DOI] [PubMed] [Google Scholar]
- 45.Christensen A, Sullaway M. Communication Patterns Questionnaire. Unpublished manuscript. Los Angeles: University of California; 1984. [Google Scholar]
- 46.Christensen A. Dysfunctional Interaction Patterns in Couples. Perspectives on Marital Interaction. 1988:30–52. [Google Scholar]
- 47.Heavey CL, Layne C, Christensen A. Gender and Conflict Structure in Marital Interaction:A Replication and Extension. J Consult Clin Psychol. 1993;61:16–27. doi: 10.1037//0022-006x.61.1.16. [DOI] [PubMed] [Google Scholar]
- 48.Manne SL, Ostroff J, Norton T, Fox K, Goldstein L, Grana G. Cancer-Related Relationship Communication in Couples Coping with Early Stage Breast Cancer. Psychooncology. 2006;15:234–247. doi: 10.1002/pon.941. [DOI] [PubMed] [Google Scholar]
- 49.Rosen RC, Riley A, Wagner G, Osterloh I, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): A multidemsional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 50.Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54(2):346–351. doi: 10.1016/s0090-4295(99)00099-0. [DOI] [PubMed] [Google Scholar]
- 51.Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA Prostate Cancer Index: Development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36:1002–1012. doi: 10.1097/00005650-199807000-00007. [DOI] [PubMed] [Google Scholar]
- 52.Schneider S, Moyer A, Knapp Oliver S, Sohl S, Cannella D, Targhetta V. Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: a meta-analysis. J Beh Med. 2010;33:1–14. doi: 10.1007/s10865-009-9227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Manne S, Ostroff J, Winkel G, et al. Couple-Focused Group Intervention for Women with Early Stage Breast Cancer. J Consult Clin Psychol. 2005;73:634–646. doi: 10.1037/0022-006X.73.4.634. [DOI] [PubMed] [Google Scholar]
- 54.Taylor KL, Lamdan RM, Siegel JE, Shelby R, Moran-Klimi K, Hrywna M. Psychological adjustment among African American breast cancer patients: one-year follow-up results of a randomized psychoeducational group intervention. Health Psychol. 2003;22:316–323. doi: 10.1037/0278-6133.22.3.316. [DOI] [PubMed] [Google Scholar]