Abstract
Objective
To review the theory and research evidence suggesting that tailored interactive multimedia computer programs (IMCPs) aimed at optimizing patient health behaviors could lessen socio-demographic health disparities.
Methods
Selective critical review of research regarding IMCPs tailored to psychological mediators of behavior and their effects on health behavior and outcomes among socio-demographically disadvantaged patients.
Results
Tailored IMCPs can address patient factors (e.g. language barriers, low self-efficacy) and buffer provider (e.g. cognitive bias) and health system (e.g. office visit time constraints) factors that contribute to poor provider-patient communication and, thereby, suboptimal health behaviors. Research indicates disadvantaged individuals' interactions with providers are disproportionately affected by such factors, and that their behaviors respond favorably to tailored information, thus suggesting tailored IMCPs could mitigate disparities. However, no randomized controlled trials (RCTs) have examined this question. The optimal design and deployment of tailored IMCPs for disadvantaged patients also requires further study.
Conclusion
Preliminary research suggests tailored IMCPs have the potential to reduce health disparities. RCTs designed expressly to examine this issue are warranted.
Practice Implications
Many socio-demographic health disparities exist, and there is a dearth of proven disparity-reducing interventions. Thus, if tailored IMCPs were shown to lessen disparities, the public health implications would be considerable.
Keywords: health disparities, patient education as topic, tailored health information, therapy-computer assisted, vulnerable populations
1. Introduction
Providing individuals with generic, non-personalized information regarding health risks and conditions improves knowledge of such issues but is not strongly associated with improvements in related health behaviors.1 By contrast, providing individuals with personally tailored health information improves knowledge, health behaviors, and health outcomes.1 Whether broader use of tailored patient health information could help mitigate socio-demographic health disparities has been little considered. Yet this is a question of pressing importance, given the magnitude of the problem of health disparities2 and the dearth of interventions with disparity-reducing potential.3
In this review, we present a theoretical model of the effects of tailored information on health behavior, and review research evidence supporting the model. We then highlight how providing tailored information via interactive multimedia computer programs (IMCPs) could help to lessen socio-demographic health disparities. Finally, we propose a research agenda for studying the effects of tailored IMCPs on health disparities. We focus on tailored IMCPs for two reasons. First, they are rapidly becoming the standard medium for providing tailored health information.4–10 Second, relevant to the issue of disparities, they can deliver tailored information in ways not possible with printed documents, such as via audio and video, making information more accessible to those less likely to absorb printed text information, such as those with poor reading skills, low English proficiency, and/or poor vision.
2. Methods
We conducted a selective review of the relevant English-language health care literature from 1966–2009, gathering and critically reviewing theoretical and preliminary research publications most relevant to consideration of the potential for tailored IMCPs to mitigate health disparities. Consistent with this broad aim, there were no restrictions based on research design or type of publication. Databases searched were PubMed, PsychINFO, and the Cochrane Database of Systematic Reviews. Over 40 search terms were employed alone and/or in various combinations, including behavior and behavior mechanisms; communication barriers; computer-assisted instruction; disadvantaged; health education; healthcare disparities; Internet; minority health; motivation; patient education; patient participation; physician-patient relations; poverty; prejudice; stereotyping; tailored health information; therapy-computer assisted; and vulnerable populations. Several hundred potentially relevant articles were retrieved and screened by one of the authors (AJ). Additional articles were located via manual review of citation lists of retrieved articles. Articles of greatest relevance to one or more issues germane to the consideration of disparity-reduction by tailored IMCPs were read in detail by one or more of the authors and included in the review.
3. Tailored health information: definition and key concepts
Tailoring aims to personalize health information. An example of the simplest form of tailoring is sending a reminder letter to a 65 year old woman that addresses her by name and states “You are due for your yearly mammogram.” Even such minimally tailored approaches tend to be more effective than generic prompts, such as sending a non-personalized letter that states “All women between 50 and 70 should have a yearly mammogram.”11
However, health messages tailored to the status of psychological variables known to influence health behaviors are even more powerful than minimally tailored interventions in improving health behaviors, including those related to cancer screening, healthy eating, and smoking.1 Ideal variables for tailoring meet two criteria. First, they are associated with (and preferably are known to mediate)12 the health behaviors of interest. Second, there is a range of baseline values for the variable in the group who will receive the intervention.13 The latter condition is important because when there is little variability in baseline variable status, a group targeted intervention that addresses modal attributes of the group would likely be more efficient, since targeted interventions avoid the step of having to identify characteristics tailored to the individual. Section 4.1 presents examples of variables commonly employed in prior tailoring interventions that meet these two criteria.
4. Ways in which tailored IMCPs may positively influence health behavior
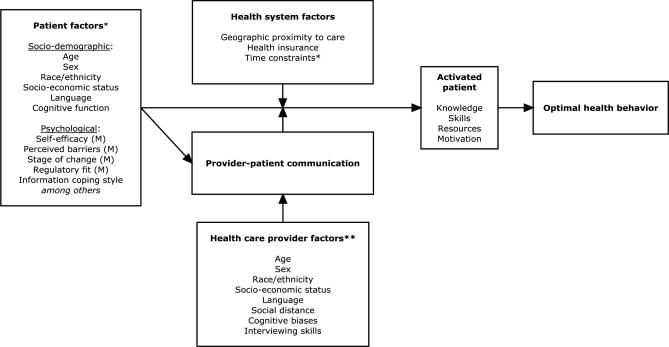
The Figure outlines a theoretical model delineating how psychologically tailored IMCPs may influence patient, provider, interpersonal, and health system factors to optimize health behaviors. The model builds on prior theories and research relevant to health behavior, including Social Cognitive Theory,14 the Expanded Health Belief Model,15 information coping styles,16 regulatory fit theory,17 and patient activation.18–22 Patient factors are viewed as the primary mediators12 of health behaviors, considered within two overlapping clusters: salience and mutability. Salience refers to tailoring factors affecting the relevance of messages to the individual. Mutability refers to tailoring factors that, in addition, tailored information aims to enhance. The ultimate goal of both salience and mutability tailoring is to improve health behaviors.
Figure.
Theoretical model of factors influencing patient activation and health behavior.
* = Factors that can be directly addressed with tailored patient health information
** = Factors for which adverse effects on behavior may be indirectly addressed or “buffered” with tailored patient health information
M = Mutable factors that tailored health information can enhance.
By contrast, provider factors, operating through provider-patient communication, are viewed as moderators.12 Similarly, health system factors are also moderators, influencing both patients and provider-patient communication. The final common pathway is an activated patient, primed with the requisite knowledge and necessary skills, resources, and motivation to pursue optimal health behaviors (that is, behaviors associated with better health outcomes). The Figure also illustrates selected patient, provider, and health system factors upon which psychologically tailored IMCPs may have salutary effects. The status of each factor tends to be least favorable among disadvantaged patients, who are also most likely to experience health disparities, indicating the potential for tailored IMCPs to reduce disparities.
Our notion of an activated patient draws on the concept of patient activation developed by prior authors, especially Kaplan and Greenfield18, 19, 22 and more recently Hibbard and colleagues.20, 21 However, in the context of our model, activation is considered to be specific to the health behavior being addressed, whereas most prior research has approached activation as a general behavioral state.18–22 This is because Social Cognitive Theory and research suggest self-efficacy – a key construct in our model – is health behavior specific.23 In other words, it would not be unusual for a woman to simultaneously have high self-efficacy for quitting smoking, low self-efficacy for taking daily medications for diabetes, and intermediate self-efficacy for undergoing screening mammography. Thus, her levels of activation for pursuing each of these health behaviors would also be expected vary.
4.1. Psychological tailoring via IMCPs
There are two fundamental goals of psychologically tailored interventions, and both are commonly pursued within a single intervention.6, 24 One goal is to maximize the perceived salience or “fit” of information to the individual. Such an approach is particularly relevant when health information is being tailored to largely immutable psychological characteristics. For example, in a tailored intervention to increase mammography screening, different message variants might be created for people with different styles of coping with information.16 One variant might be created for “monitors,” that is, people who prefer more information and respond more favorably to reassuring messages (“Getting a yearly mammogram is easy to do and can protect your health.”). Another variant might be for “blunters,” who desire less information and are motivated to act by more intense messages framed in terms of health threats (“Women who don't get yearly mammograms are more likely to die from breast cancer!”). Finally, a neutral variant might be created for people falling between these extremes (“Annual mammograms save lives.”). In each case, the aim is not to change recipients' information coping style but to provide information in a way that matches their style. In tailored IMCPs, media hyperlinks and other navigational tools can also be exploited to allow individuals to self-tailor the type and level (depth and breadth) of information they receive regarding topics.
A second goal of tailoring is to favorably influence the status of mutable psychological characteristics that mediate health behavior. For example, in a smoking cessation intervention, variants of a message might be tailored to different levels of self-efficacy for quitting. The aim of a low self-efficacy variant might be to bolster self-efficacy for quitting by using encouraging language and pointing out commonalities with other healthy behaviors the recipient has previously achieved (e.g. daily tooth brushing, healthy eating). By contrast, a high self-efficacy variant might briefly congratulate the recipient for being confident in their ability to quit and suggest they may be ready to pick a quit date.
Beyond delineating the two fundamental goals of tailoring, the preceding examples illustrate that the design of psychologically tailored messages is typically informed by one or more partially overlapping theoretical models relevant to health behavior. For example, the Expanded Health Belief Model, the Transtheoretical Model, and Social Cognitive Theory each suggest that self-efficacy for implementing a given health behavior is a key determinant of success in achieving the behavior.14, 15, 25 An individual's self-efficacy derives from several sources, including previous performance accomplishments, vicarious experiences, and verbal persuasion.23 Thus, in a tailored intervention to encourage colorectal cancer screening, an individual's self-efficacy for screening might be bolstered by: (1) asking about and congratulating them on successes with the same (e.g. prior colorectal cancer screening) or similar (e.g. mammography screening) health behaviors; (2) pointing out that many people much like them successfully undergo screening each year; (3) characterizing and providing tailored practical suggestions for overcoming perceived barriers to screening; and (4) using appropriately positive language (e.g. “For all these reasons, we are confident you have what it takes to be screened!”). Note that self-efficacy is used here as but one illustrative example; several other psychological variables have been commonly employed in tailored interventions, particularly stage of readiness for behavior change.1, 24
Regardless of the tailoring variables employed, persuasive messages have the most impact on behavior when subjects attend closely and objectively to message content. This is most likely to occur when they are interested in the issue at hand and perceive it to be personally salient.26 High personal salience is achieved in tailored interventions in general by first eliciting the patient's knowledge, concerns, preferences, and barriers related to a given health topic using the computerized tailoring questionnaire, and then providing information tailored to these and other relevant personal factors. Even when only a few tailoring variables are employed, the capacity for maximizing personal salience is vast due to the number of possible combinations of responses. One tailored smoking cessation intervention, which employed only a handful of tailoring variables, was capable of generating almost half a million tailored message variants.27
Providing tailored information in the form of carefully chosen images may also improve salience. Even when people are not initially motivated to attend to a health message, they may be influenced by cues like perceived source credibility and media characteristics such as interactivity,28 the latter a particular strength of IMCPs. For example, the perceived salience of information about a health topic might be enhanced by ensuring that some of the patient testimonial video clips presented in an IMCP feature individuals whose race and ethnicity are concordant with those of each user.
5. Tailored IMCPs and health disparities: Rationale and preliminary evidence
The research and theories discussed thus far support the use of psychologically tailored interventions in general, but do they suggest greater use of psychologically tailored IMCPs would be likely to help mitigate health disparities? We believe the answer is “yes.” Lack of foresight and planning when introducing new health technologies could lead to worsening health disparities.29–31 However, when new technologies are made accessible to disadvantaged individuals32, 33 – in other words, when they are designed and deployed in a manner that accounts for their personal and social characteristics – new health technologies do not generally worsen and may at times lessen health disparities.34–39 In the next sections, we present theoretical and preliminary research support for the notion that psychologically tailored IMCPs could lessen health disparities.
5.1. Effects of tailored interventions on psychological mediators of health behavior among the disadvantaged
The statuses of many psychological variables that mediate health behaviors, such as self-efficacy, tend to be less favorable among poor, minority, and less healthy individuals than among others.40–42 Such individuals also tend to view standard patient education as largely irrelevant to their unique perspectives and needs.43 Thus, disadvantaged individuals may have more to gain from psychologically tailored information than others, suggesting the potential for reduction in disparities with this approach assuming equitable access to tailored IMCPs is assured (an issue addressed in Section 7.3).
One randomized controlled trial (RCT) suggested psychologically tailored interventions can help to mitigate health disparities, comparing the effects of computer-generated, printed mammography letters tailored to stage of readiness with the effects of non-tailored letters.44 Letter type was statistically significantly associated with optimal stage of readiness movement among black but not white women. Black women also indicated significantly more interest in the content of tailored versus non-tailored letters. We found no other published studies have examining the effects of computer-assisted tailoring of health information on race/ethnicity- or socioeconomically-based health disparities. However, a RCT of a personalized nurse coaching intervention found that the intervention was associated with elimination of a baseline disparity in cancer pain control between whites and minorities, suggesting the potential for personally tailored interventions to reduce disparities.45
Several other studies provided psychologically tailored information to minority and poor individuals, but none examined effects on health disparities, and only some employed IMCPs to deliver the tailored information.8, 13, 46–48 Nonetheless, taken together, their results indicate that psychologically tailored interventions are viewed as useful by disadvantaged individuals, and can favorably influence psychological mediators of health behavior and actual health behaviors among such individuals.8, 13, 46–48
5.2. Effects on quality of communication with health care providers
Many studies have documented suboptimal communication between health care providers and minority, less educated, and poor patients.49–52 While the issues that limit provider/patient communication are not unique to disadvantaged individuals, they limit communication to the greatest degree among such individuals,53 and therefore contribute to disparities.
Language barriers significantly impair communication with health care providers in many individuals. In the 2000 United States census, 8.1% of the population aged 5 and older indicated speaking English less than “very well,”54 with 38% of older Latino adults and 41% of older Asian adults indicating they spoke little or no English.55 Given that most health care providers in industrialized nations are unable to speak the languages primarily spoken by many of their disadvantaged patients, that access to certified medical interpreters is poor in most health care settings, and that use of untrained interpreters such as family members is fraught with problems, language constitutes one of the most significant barriers to optimal health care communication.56
For minority patients recently immigrated to industrialized countries, culturally-related differences in health beliefs, deference to authority, and mistrust of the health care system are superimposed upon the inherent power imbalance between patients and health care providers, creating further barriers to communication.50, 52 Minorities and less affluent individuals also have significantly lower average levels of education, general literacy, and health literacy than others,57 creating further communication impediments. Finally, among older disadvantaged individuals, sensory impairments, such as vision and hearing limitations, and cognitive impairment are common, and these issues also hinder communication.58 Each of these communication barriers is independently associated with health disparities.55, 57 Cumulatively, they result in a considerable social distance between disadvantaged patients and their health care providers.59
Tailored information delivered via IMCPs could help to address each of the aforementioned provider-patient communication barriers,60 reducing the large social distance between disadvantaged patients and their providers and, in turn, lessening health disparities. Tailored IMCPs can be offered in any language, and designed so users can self-select the language in which they prefer to review materials, thereby overcoming language barriers. On-screen text and narrated information in IMCPs can be presented at the appropriate reading and medical terminology sophistication levels for low education and low literacy individuals. IMCPs can also deliver tailored information via multiple sensory channels, including via on screen text, pictures, animations, sound files, and video clips, further helping to circumvent sensory and literacy impairments. Finally, with input from members of the intended audience, as well as content experts, personally tailored information can even be developed to help overcome provider-patient cultural, generational, and power differences. While health care providers might be trained to simplify the language they use in communicating with disadvantaged individuals, and to use interviewing techniques to elicit and explore cultural, generational, and power differences, it is exceedingly difficult for providers to implement these strategies widely and consistently in practice.
5.3. Effects on health care provider factors such as cognitive biases
Research suggests that clinicians' diagnostic and therapeutic decision making can vary by clinically irrelevant patient characteristics, such as race or ethnicity, age, and gender, and that this variation contributes to health disparities.51, 61–66 Specifically, health care providers may act based on cognitive biases regarding disadvantaged individuals,67 resulting in ineffective communication, questionable clinical decisions, and ultimately suboptimal care.68 Such cognitive biases are wide spread69 and largely automatic and unconscious, and therefore operative even in well-intentioned providers who are motivated to be non-prejudiced, potentially explaining “the strange juxtaposition of egalitarian attitudes and discriminatory behavior” prevalent in current medical practice.62
In theory, health care providers could be trained to recognize and avoid acting on such biases. Greater efforts to attract and select medical students less likely to be biased toward vulnerable populations, including efforts to increase recruitment of minority students, could also help to address this problem. Yet such interventions are challenging to design and implement broadly, and would require considerable time to achieve noticeable effects on disparities. Creating unbiased psychologically tailored IMCPs may be more quickly achieved. Materials can be carefully developed in advance with input from target audience members and experts in cross-cultural communication,13 and are relatively easy to reproduce and disseminate. At a minimum, routinely providing minority, low education, and poor adults with such materials before interactions with health care providers would complement other promising approaches to overcoming provider-related barriers to communication, helping to “level the playing field” in at least two ways. First, such an approach might help to “buffer” some of the effects of suboptimal health care provider communication by providing unbiased, tailored information directly to patients. Second, such an approach might indirectly lead to better provider interpersonal behaviors (e.g. less biased, more personalized care) during encounters, due to prompts by activated patients. Studies examining the effects of patient requests on physician behavior via audio recordings of provider-patient encounters suggest both mechanisms might be operative.70, 71 However, these studies did not specifically examine the effects of tailored interventions on office encounter processes.
5.4 Overcoming time constraints
All of the aforementioned barriers to optimal communication between disadvantaged patients and their providers play out within the context of brief outpatient primary care office visits, in which most health care is delivered.72 Primary care office visits typically feature crowded agendas, with multiple issues competing for providers' time. One audiotape study found that on average about five minutes was spent on the main topic of primary care office visits, while other topics received about one minute each.73 Primary care office visit time constraints may disproportionately impact on disadvantaged people, contributing to disparities in care. Many disadvantaged individuals have multiple complex needs,74 and dealing with these needs during brief outpatient visits places a high cognitive demand on providers – the very circumstance in which they may be most likely to act on unconscious cognitive biases they harbor regarding disadvantaged groups.75
Wider provision of personally tailored information to disadvantaged individuals could help to remedy this situation, effectively expanding the reach of the patient-provider encounter in both space and time. Imagine a patient interested in discussing colorectal cancer screening during a primary care office visit in which there are multiple other issues to discuss. If the patient has little knowledge of colorectal cancer screening, the discussion is likely to be time consuming, starting from “square one” (e.g. who is eligible, what are the available tests), and only then moving to more behaviorally-relevant issues such as identifying and addressing perceived barriers to screening. If the patient had the opportunity to use an psychologically tailored colorectal cancer screening IMCP in the office waiting room before the appointment, then the discussion during the visit might be both shorter and more productive, focusing first on quickly answering any remaining fundamental questions and then on negotiating an individualized plan for screening.
6. Tailored IMCPs and patient activation
In the prior section of this review, we delineated ways in which personally tailored interventions can favorably influence patient, provider, and health system factors. The cumulative anticipated effect of these influences would be an activated patient: one primed with the requisite knowledge, skills, resources, and motivation to pursue optimal health behaviors (Figure). Currently a relatively high proportion of disadvantaged individuals state a preference for less participatory care.76, 77 While this could in part reflect conscious, well-informed preferences, it seems more likely that the factors identified in the Figure (e.g. suboptimal status of psychological factors like self-efficacy, along with cultural norms, experiences, expectations, language barriers, provider cognitive biases, encounter time constraints, and other issues) probably combine to decrease disadvantaged individuals' participation in care.77, 78 By engaging disadvantaged individuals in the health care process, tailored IMCPs are likely to encourage more favorable beliefs about the value of being an active participant in ones own care.
7. Recommendations for future research
While the forgoing literature review suggests IMCPs hold promise as tools for mitigating health disparities, it also clearly indicates a pressing need for empirical studies examining the utility of IMCPs in this regard. In the final section of this review, we propose a research agenda for studying the effects of tailored IMCPs on disparities.
7.1. Adequately design and power studies to examine the effects of tailored interventions on health disparities
To our knowledge, no RCTs have been published that were designed and powered to examine the effects of any interventions on health disparities, including tailored interventions.3 The most rigorous way of demonstrating the disparity-reducing potential of an intervention would involve detecting a statistically significant interaction between the disparity and the effect of the intervention in a RCT. To support such interaction analyses, randomization within the intervention and control groups must be stratified by the relevant socio-demographic characteristics. For example, to examine the potential of a tailored IMCP to eliminate disparities in completion of colorectal cancer screening between Hispanic and non-Hispanic white individuals in a RCT, stratified randomization of individuals by ethnicity (Hispanic or not) into both the experimental and control arms of would need to occur. In such studies, attaining adequate statistical power to detect interactions between the disparity and the intervention effect requires sample sizes about four times larger than those needed to detect the main effect of the intervention.3 The high costs entailed by attempting to recruit large study samples could in some circumstances preclude conducting disparities-focused tailored IMCP studies, at least within the limits of current grant funding mechanisms.
A less definitive but perhaps more pragmatic approach, because it would require somewhat smaller sample sizes than the interaction approach, may be to conduct equivalence analyses of data from stratified RCTs, where the effects of a tailored IMCP intervention in a group experiencing a particular health disparity are compared with those in a group not experiencing the disparity.3 In this approach, researchers define, a priori, a minimal clinically important difference (MCID) between groups on the outcome of interest, proposing, in effect, that differences equal to or smaller than the MCID are likely to be clinically unimportant or trivial. If in the subsequent RCT the difference in the outcome between the group currently experiencing a disparity in that outcome in society and the group not currently experiencing the disparity is less than or equal to the pre-specified MCID, it implies the intervention has the potential to eliminate the disparity. While the equivalence analysis approach requires a smaller sample size than interaction analysis, it is also a less rigorous methodology. Furthermore, defining the MCID is often a contentious process, since for most outcome measures no universally agreed upon threshold exists.
7.2. Explore the utility of various psychological tailoring variables
Although prior tailored intervention studies have generally focused on a relatively small grouping of psychological variables, a number of other constructs appear ripe for exploration. One of the most promising, regulatory fit, is discussed as an illustrative example here.
Regulatory fit describes a situation where a person behaves in a manner that matches or “fits” their current motivational state.17 It lends itself to tailoring of health information that addresses both the salience of messages to an individual and the mutability of motivational states affecting message effectiveness (see Figure). For example, in a patient with diabetes, seeking to achieve ideal serum glycosylated hemoglobin levels is a gain-oriented motivation and is a regulatory fit with behaving in an eager (or advancement, accomplishment, and aspiration-oriented) manner – e.g. trying out new foods or creating low-calorie recipes. By contrast, behaving in a vigilant (or protection, safety, and responsibility-oriented) manner – e.g. focusing on maintaining the prescribed behavioral pattern of taking one's oral hypoglycemic medications - is a non-fit. When experiencing regulatory fit, individuals are more motivated to complete their goals79 and are better able to resist temptation.80 Moreover, behaving can be considered in a broad sense, so that even reading a paragraph framed in a manner that matches (rather than disrupts) the individual's motivation creates a regulatory fit experience and causes people to find messages to be more salient and persuasive.81 Regulatory fit is also known to enhance cognition and both mental and physical performance,82, 83 intensify evaluative experiences,84 and help people to “feel right” about what they are doing.85
In the health care domain, regulatory fit tailoring manipulations have been shown to increase participation in physical fitness activities86 and increase fruit and vegetable intake.87 Another set of studies correlated regulatory fit experience with health care-taking behaviors and readiness to participate in cancer screening,88 while other research manipulated regulatory fit to increase healthy food choice and compliance with other health related suggestions.89 Importantly, a regulatory fit mechanism was found to mediate cultural differences in adherence to a persuasive message about flossing.90 If disadvantaged groups routinely experience a non-fit in health related persuasive messages, it could account for lower implementation of optimal health behaviors in these groups, suggesting a potential role for tailoring of message to regulatory fit in reducing disparities. More research exploring this line of inquiry is needed.
7.3. Study the effects of potential barriers to tailored IMCP implementation, and strategies for overcoming those barriers
If not thoughtfully examined and addressed, several issues could limit the impact of tailored IMCPs on health disparities. A number of “digital divides” currently exist that sort along racial/ethnic and socio-demographic lines. For example, only 57% of African-Americans currently report regularly using the Internet, compared with 70% of whites,91 and only 29% of non-high school graduates have Internet access, versus 61% of high school and 89% of college graduates.92 The “graying” of the population also represents a potential challenge to wider use of tailored IMCPs as disparity-reducing tools. Encouragingly, preliminary studies suggest older adults generally enjoy, are interested in, and can benefit from thoughtfully designed computerized health information systems,93, 94 including tailored IMCPs.4, 9, 95, 96 However, no carefully designed, adequately powered RCTs have examined the effectiveness of tailored IMCPs among older disadvantaged adults, who tend to have relatively low computer use confidence and skills58 and relatively high rates of sensory and cognitive impairment,97 all of which can impair computer use.
Nonetheless, such potential barriers to tailored IMCP use in disadvantaged adults might be largely overcome with careful attention to design and deployment. For example, to help overcome digital divide issues, individuals without home computer access can be provided with computers loaded with tailored IMCPs for use in office waiting areas prior to doctors' visits.6 Likewise, to help overcome vision, hearing, and cognitive barriers prevalent among older disadvantaged people, tailored IMCP designers and programmers can strive to develop simple programs navigable via touch screen or other user-friendly interfaces; employ larger fonts; and offer optional audio narration of text. Such measures represent good basic principles for designing computer programs for any audience, but are even more important for older adults.58 To help address these barriers, investigators may also need to consider including human assistants or chaperones in IMCP study protocols.
7.4. Study how personally tailored interventions can be optimally packaged for use in daily practice
The majority of care is delivered in primary care offices, and this is particularly true for minority and disadvantaged adults.98, 99 Furthermore, it is unlikely that patients or practitioners have the time to hunt for dozens of different tailored IMCPs, each offered in a different platform and focused on a different health issue and patient group. Thus, future research regarding tailored IMCPs and health disparities must consider optimal ways of packaging these tools for use in primary care.
Two different and complementary packaging approaches appear worthy of exploration in future studies. The first involves studying the effects of interventions which tailor health information to the status of “high bang for buck” psychological constructs. For example, as noted previously, the concept regulatory fit is not unique to any particular health behavior or problem per se, but rather extends across and has potential relevance to myriad behaviors and issues. Thus, an IMCP providing regulatory fit-tailored information about a variety of health problems could bolster adherence to multiple treatment regimens simultaneously, improving overall health. Such an approach would be expected to disproportionately benefit the disadvantaged, who tend to have higher medical co-morbidity and complexity.
The second potential approach to efficient packaging of tailored IMCPs involves bundling problem-focused modules together within single access point “triage and delivery” computer programs. Such programs might feature an intake questionnaire assessing a patient's status in regard to the most common and important health issues (e.g. mental health, substance abuse, cardiovascular risk, and preventive care); might provide tailored feedback regarding the patient's status in regard to each issue; and might provide tailored information to help the patient prioritize which IMCP modules to view, and which problems to address first with their health care providers.
A final unexplored packaging issue is how best to integrate tailored IMCPs into existing primary care delivery processes. Seamlessly incorporating the tools into electronic clinical information and communication systems is an obvious high priority task. However, a broader view considering other important logistical issues is warranted, including but not limited to: The optimal times and places for patients to view tailored IMCPs; whether primary care providers should receive reports with key findings of tailoring questionnaires competed by their patients; and whether other health care team members (e.g. medical assistants, front desk staff) could facilitate effective patient use of the tools.
7.5. Examine the feasibility, optimal design, and effects of longitudinal tailored interventions
Prior studies of personally tailored information have involved one time or very brief interventions, the behavioral effects of which generally diminish within a year or less. Although multiple exposure tailored interventions would clearly entail greater logistical difficulties and expense, they represent an attractive potential alternative or complement to human-delivered longitudinal interventions. Tailored IMCPs inherently remain standardized across different locations and over time. In contrast, human-delivered personalized interventions, while having the theoretical advantage of being infinitely “tailorable” on the fly, are vulnerable to unintended inconsistency and temporal drift in content, some of which may arise due to unconscious cognitive biases among individuals delivering the interventions toward minority, low education, and poor recipients. As discussed previously, such biases are prevalent even among people who strive to avoid prejudice and can lead to suboptimal communication. While unintended variation and temporal drift in human-delivered interventions can be reduced with careful planning, it is a daunting challenge, requiring considerable logistical effort and financial resources.100
7.6. Study the effects of personally tailored interventions on provider-patient communication
As mentioned previously, no direct observation studies have examined whether patient use of tailored interventions can “buffer” the effects of or correct certain health care provider-related (e.g. cognitive biases) and health-system related (e.g. lack of time) deficits that lead to suboptimal patient/provider communication and contribute to health disparities. Such studies should be a future priority, since greater understanding may help to guide efforts to strengthen the effects of such interventions.
8. Conclusion
This review has delineated only selected, pressing research gaps regarding the potential effects of tailored interventions delivered via IMCPs on health disparities. A number of other important unanswered research questions remain. It must also be emphasized that not all health disparities can be addressed with tailored IMCPs, particularly disparities resulting from reduced access to health care. Further, tailored information may be less effective for health interventions that are very strongly provider driven, such as cardiovascular interventions and surgical procedures - though even in this instance, patient activation might have salutary effects. Ultimately, the tailored IMCP is most optimally viewed as one of a number of highly promising tools for mitigating health disparities.
Acknowledgments
Funding for this research was provided by National Cancer Institute grant no. 1R01CA131386-01A1 (Jerant). The funder had no role in the study design; collection, analysis and interpretation of data; writing of the report; nor in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest The authors are aware of no conflict of interest arising from this work.
References
- [1].Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133:673–93. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- [2].Agency for Healthcare Research and Quality . National healthcare disparities report. AHRQ; Rockville, MD: 2009. AHRQ Publication No. 09-0002. [Google Scholar]
- [3].Franks P, Fiscella K. Reducing disparities downstream: prospects and challenges. J Gen Intern Med. 2008;23:672–7. doi: 10.1007/s11606-008-0509-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Barnabei VM, O'Connor JJ, Nimphius NM, Vierkant RA, Eaker ED. The effects of a web-based tool on patient-provider communication and satisfaction with hormone therapy: a randomized evaluation. J Womens Health (Larchmt) 2008;17:147–58. doi: 10.1089/jwh.2007.0369. [DOI] [PubMed] [Google Scholar]
- [5].Bodurtha J, Quillin JM, Tracy KA, Borzelleca J, McClish D, Wilson DB, Jones RM, Quillin J, Bowen D. Mammography screening after risk-tailored messages: the women improving screening through education and risk assessment (WISER) randomized, controlled trial. J Womens Health (Larchmt) 2009;18:41–7. doi: 10.1089/jwh.2007.0703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Jerant A, Kravitz RL, Rooney M, Amerson S, Kreuter M, Franks P. Effects of a tailored interactive multimedia computer program on determinants of colorectal cancer screening: a randomized controlled pilot study in physician offices. Patient Educ Couns. 2007;66:67–74. doi: 10.1016/j.pec.2006.10.009. [DOI] [PubMed] [Google Scholar]
- [7].Kroeze W, Oenema A, Campbell M, Brug J. Comparison of use and appreciation of a print-delivered versus CD-ROM-delivered, computer-tailored intervention targeting saturated fat intake: randomized controlled trial. J Med Internet Res. 2008;10:e12. doi: 10.2196/jmir.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].McDaniel AM, Casper GR, Hutchison SK, Stratton RM. Design and testing of an interactive smoking cessation intervention for inner-city women. Health Educ Res. 2005;20:379–84. doi: 10.1093/her/cyg135. [DOI] [PubMed] [Google Scholar]
- [9].Nyman SR, Yardley L. Web-site-based tailored advice to promote strength and balance training: an experimental evaluation. J Aging Phys Act. 2009;17:210–22. doi: 10.1123/japa.17.2.210. [DOI] [PubMed] [Google Scholar]
- [10].Oenema A, Tan F, Brug J. Short-term efficacy of a web-based computer-tailored nutrition intervention: main effects and mediators. Ann Behav Med. 2005;29:54–63. doi: 10.1207/s15324796abm2901_8. [DOI] [PubMed] [Google Scholar]
- [11].Stone EG, Morton SC, Hulscher ME, Maglione MA, Roth EA, Grimshaw JM, Mittman BS, Rubenstein LV, Rubenstein LZ, Shekelle PG. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136:641–51. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- [12].Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–83. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- [13].Kreuter MW, Haughton LT. Integrating culture into health information for African American women. Am Behav Sci. 2006;49:794–811. [Google Scholar]
- [14].Bandura A. Social foundations of thought and action: a social cognitive theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- [15].Janz NK, Champion VL, Strecher VJ. The health belief model. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: theory, research, and practice. 3rd ed. Jossey-Bass; San Francisco, CA: 2002. [Google Scholar]
- [16].Miller SM. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer. 1995;76:167–77. doi: 10.1002/1097-0142(19950715)76:2<167::aid-cncr2820760203>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- [17].Higgins ET. Making a good decision: Value from fit. Amer Psychologist. 2000;55:1217–30. [PubMed] [Google Scholar]
- [18].Greenfield S, Kaplan S, Ware JE. Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med. 1985;102:520–8. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- [19].Greenfield S, Kaplan SH, Ware JE, Yano EM, Frank HJL. Patient participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- [20].Hibbard JH, Greene J, Becker ER, Roblin D, Painter MW, Perez DJ, Burbank-Schmitt E, Tusler M. Racial/ethnic disparities and consumer activation in health. Health Aff (Millwood) 2008;27:1442–53. doi: 10.1377/hlthaff.27.5.1442. [DOI] [PubMed] [Google Scholar]
- [21].Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39:1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kaplan SH, Greenfield S, Ware JE. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–27. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- [23].Bandura A. Self-efficacy: the exercise of control. Freeman; New York: 1997. [Google Scholar]
- [24].Albada A, Ausems MG, Bensing JM, van Dulmen S. Tailored information about cancer risk and screening: A systematic review. Patient Educ Couns. 2009;77:155–71. doi: 10.1016/j.pec.2009.03.005. [DOI] [PubMed] [Google Scholar]
- [25].Prochaska JM, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: theory, research, and practice. 3rd ed. Jossey-Bass; San Francisco, CA: 2002. [Google Scholar]
- [26].Stiff JB. Cognitive processing of persuasive message cues: a meta-analytic review of the effects of supporting information on attitudes. Commun Monogr. 1986;53:75–89. [Google Scholar]
- [27].Schumann A, John U, Ulbricht S, Ruge J, Bischof G, Meyer C. Computer-generated tailored feedback letters for smoking cessation: theoretical and empirical variability of tailoring. Int J Med Inform. 2008;77:715–22. doi: 10.1016/j.ijmedinf.2008.03.001. [DOI] [PubMed] [Google Scholar]
- [28].Petty RE, Cacioppo JT. Communication and persuasion: central and peripheral routes to attitude change. Springer-Verlag; New York: 1986. [Google Scholar]
- [29].Fenton JJ, Tancredi DJ, Green P, Franks P, Baldwin LM. Persistent racial and ethnic disparities in up-to-date colorectal cancer testing in medicare enrollees. J Am Geriatr Soc. 2009;57:412–8. doi: 10.1111/j.1532-5415.2008.02143.x. [DOI] [PubMed] [Google Scholar]
- [30].Miech RA, Kim J, McConnell C, Hamman RF. A growing disparity in diabetes-related mortality U.S. trends, 1989–2005. Am J Prev Med. 2009;36:126–32. doi: 10.1016/j.amepre.2008.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Mattke S, Martorell F, Sharma P, Malveaux F, Lurie N. Quality of care for childhood asthma: estimating impact and implications. Pediatrics. 2009;123(Suppl 3):S199–204. doi: 10.1542/peds.2008-2233K. [DOI] [PubMed] [Google Scholar]
- [32].Chang VW, Lauderdale DS. Fundamental cause theory, technological innovation, and health disparities: The case of cholesterol in the era of statins. Journal of Health and Social Behavior. 2009;50:245–60. doi: 10.1177/002214650905000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Goldman DP, Lakdawalla DN. A theory of health disparities and medical technology. [Accessed May 15, 2010];Contributions to Economic Analysis & Policy. 2005 http://works.bepress.com/dana_goldman/7.
- [34].Shapiro S, Venet W, Strax P, Venet L, Roeser R. Prospects for eliminating racial differences in breast cancer survival rates. Am J Public Health. 1982;72:1142–5. doi: 10.2105/ajph.72.10.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Five-year findings of the hypertension detection and follow-up program. II. Mortality by race-sex and age. Hypertension Detection and Follow-up Program Cooperative Group. JAMA. 1979;242:2572–7. doi: 10.1001/jama.1979.03300230028022. [DOI] [PubMed] [Google Scholar]
- [36].Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? Proc Natl Acad Sci U S A. 2002;99:10929–34. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Smith JL, Rost KM, Nutting PA, Elliott CE, Dickinson LM. Impact of ongoing primary care intervention on long term outcomes in uninsured and insured patients with depression. Med Care. 2002;40:1210–22. doi: 10.1097/00005650-200212000-00008. [DOI] [PubMed] [Google Scholar]
- [38].Wells K, Sherbourne C, Schoenbaum M, Ettner S, Duan N, Miranda J, Unutzer J, Rubenstein L. Five-year impact of quality improvement for depression: results of a group-level randomized controlled trial. Arch Gen Psychiatry. 2004;61:378–86. doi: 10.1001/archpsyc.61.4.378. [DOI] [PubMed] [Google Scholar]
- [39].Szilagyi PG, Schaffer S, Shone L, Barth R, Humiston SG, Sandler M, Rodewald LE. Reducing geographic, racial, and ethnic disparities in childhood immunization rates by using reminder/recall interventions in urban primary care practices. Pediatrics. 2002;110:e58. doi: 10.1542/peds.110.5.e58. [DOI] [PubMed] [Google Scholar]
- [40].Kempen GI, Jelicic M, Ormel J. Personality, chronic medical morbidity, and health-related quality of life among older persons. Health Psychol. 1997;16:539–46. doi: 10.1037//0278-6133.16.6.539. [DOI] [PubMed] [Google Scholar]
- [41].Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29:823–9. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- [42].Carpenter V, Colwell B. Cancer knowledge, self-efficacy, and cancer screening behaviors among Mexican-American women. J Cancer Educ. 1995;10:217–22. doi: 10.1080/08858199509528377. [DOI] [PubMed] [Google Scholar]
- [43].Williams JH, Auslander WF, de Groot M, Robinson AD, Houston C, Haire-Joshu D. Cultural relevancy of a diabetes prevention nutrition program for African American women. Health Promot Pract. 2006;7:56–67. doi: 10.1177/1524839905275393. [DOI] [PubMed] [Google Scholar]
- [44].Skinner CS, Strecher VJ, Hospers H. Physicians' recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1994;84:43–9. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Kalauokalani D, Franks P, Oliver JW, Meyers FJ, Kravitz RL. Can patient coaching reduce racial/ethnic disparities in cancer pain control? Secondary analysis of a randomized controlled trial. Pain Med. 2007;8:17–24. doi: 10.1111/j.1526-4637.2007.00170.x. [DOI] [PubMed] [Google Scholar]
- [46].Schillinger D, Hammer H, Wang F, Palacios J, McLean I, Tang A, Youmans S, Handley M. Seeing in 3-D: examining the reach of diabetes self-management support strategies in a public health care system. Health Educ Behav. 2008;35:664–82. doi: 10.1177/1090198106296772. [DOI] [PubMed] [Google Scholar]
- [47].Weng HH, Kaplan RM, Boscardin WJ, Maclean CH, Lee IY, Chen W, Fitzgerald JD. Development of a decision aid to address racial disparities in utilization of knee replacement surgery. Arthritis Rheum. 2007;57:568–75. doi: 10.1002/art.22670. [DOI] [PubMed] [Google Scholar]
- [48].van Stralen MM, de Vries H, Mudde AN, Bolman C, Lechner L. Efficacy of two tailored interventions promoting physical activity in older adults. Am J Prev Med. 2009;37:405–17. doi: 10.1016/j.amepre.2009.07.009. [DOI] [PubMed] [Google Scholar]
- [49].Levinson W, Hudak PL, Feldman JJ, Frankel RM, Kuby A, Bereknyei S, Braddock C., 3rd “It's not what you say …”: racial disparities in communication between orthopedic surgeons and patients. Med Care. 2008;46:410–6. doi: 10.1097/MLR.0b013e31815f5392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Diette GB, Rand C. The contributing role of health-care communication to health disparities for minority patients with asthma. Chest. 2007;132:802S–9S. doi: 10.1378/chest.07-1909. [DOI] [PubMed] [Google Scholar]
- [51].Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–90. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Schouten BC, Meeuwesen L. Cultural differences in medical communication: a review of the literature. Patient Educ Couns. 2006;64:21–34. doi: 10.1016/j.pec.2005.11.014. [DOI] [PubMed] [Google Scholar]
- [53].Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O'Malley K, Petersen LA, Sharf BF, Suarez-Almazor ME, Wray NP, Street RL., Jr. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med. 2003;18:146–52. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Shin HB, Bruno R. Language use and English-speaking ability. 2000:2003. [Google Scholar]
- [55].Yeo G. How will the U.S. healthcare system meet the challenge of the ethnogeriatric imperative? J Am Geriatr Soc. 2009;57:1278–85. doi: 10.1111/j.1532-5415.2009.02319.x. [DOI] [PubMed] [Google Scholar]
- [56].Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62:255–99. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- [57].Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. 2009;7:204–11. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Redish J, Chisnell D. Designing Web sites for older adults: A review of recent research. American Association of Retired Persons; Washington, D.C.: 2004. [Google Scholar]
- [59].Saha S. The relevance of cultural distance between patients and physicians to racial disparities in health care. J Gen Intern Med. 2006;21:203–5. doi: 10.1111/j.1525-1497.2006.0345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].The state of aging and health in America, 2007. Centers for Disease Control and Prevention and the Merck Company Foundation; Whitehouse Station, NJ: 2007. [Google Scholar]
- [61].Burgess DJ, Crowley-Matoka M, Phelan S, Dovidio JF, Kerns R, Roth C, Saha S, van Ryn M. Patient race and physicians' decisions to prescribe opioids for chronic low back pain. Soc Sci Med. 2008;67:1852–60. doi: 10.1016/j.socscimed.2008.09.009. [DOI] [PubMed] [Google Scholar]
- [62].Burgess DJ, Fu SS, van Ryn M. Why do providers contribute to disparities and what can be done about it? J Gen Intern Med. 2004;19:1154–9. doi: 10.1111/j.1525-1497.2004.30227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22:882–7. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Cooper LA, Beach MC, Johnson RL, Inui TS. Delving below the surface. Understanding how race and ethnicity influence relationships in health care. J Gen Intern Med. 2006;21(Suppl 1):S21–7. doi: 10.1111/j.1525-1497.2006.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Ghods BK, Roter DL, Ford DE, Larson S, Arbelaez JJ, Cooper LA. Patient-physician communication in the primary care visits of African Americans and whites with depression. J Gen Intern Med. 2008;23:600–6. doi: 10.1007/s11606-008-0539-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Denberg TD, Kim FJ, Flanigan RC, Fairclough D, Beaty BL, Steiner JF, Hoffman RM. The influence of patient race and social vulnerability on urologist treatment recommendations in localized prostate carcinoma. Med Care. 2006;44:1137–41. doi: 10.1097/01.mlr.0000233684.27657.36. [DOI] [PubMed] [Google Scholar]
- [67].Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46:678–85. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- [68].Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22:1231–8. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians' implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20:896–913. doi: 10.1353/hpu.0.0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Epstein RM, Shields CG, Franks P, Meldrum SC, Feldman M, Kravitz RL. Exploring and validating patient concerns: relation to prescribing for depression. Ann Fam Med. 2007;5:21–8. doi: 10.1370/afm.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Young HN, Bell RA, Epstein RM, Feldman MD, Kravitz RL. Physicians' shared decision-making behaviors in depression care. Arch Intern Med. 2008;168:1404–8. doi: 10.1001/archinte.168.13.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Green LA, Fryer GE, Jr., Yawn BP, Lanier D, Dovey SM. The ecology of medical care revisited. N Engl J Med. 2001;344:2021–5. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- [73].Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42:1871–94. doi: 10.1111/j.1475-6773.2006.00689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Fiscella K, Epstein RM. So much to do, so little time: care for the socially disadvantaged and the 15-minute visit. Arch Intern Med. 2008;168:1843–52. doi: 10.1001/archinte.168.17.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Burgess DJ. Are providers more likely to contribute to healthcare disparities under high levels of cognitive load? How features of the healthcare setting may lead to biases in medical decision making. Med Decis Making. 2009;30:246–57. doi: 10.1177/0272989X09341751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Murray E, Pollack L, White M, Lo B. Clinical decision-making: Patients' preferences and experiences. Patient Educ Couns. 2007;65:189–96. doi: 10.1016/j.pec.2006.07.007. [DOI] [PubMed] [Google Scholar]
- [77].Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20:531–5. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Smith SK, Dixon A, Trevena L, Nutbeam D, McCaffery KJ. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc Sci Med. 2009;69:1805–12. doi: 10.1016/j.socscimed.2009.09.056. [DOI] [PubMed] [Google Scholar]
- [79].Spiegel S, Grant-Pillow H, Higgins ET. How regulatory fit enhances motivational strength during goal pursuit. Eur J Soc Psychol. 2004;34:39–54. [Google Scholar]
- [80].Freitas AL, Liberman N, Higgins ET. Regulatory fit and resisting temptation during goal pursuit. J Exp Soc Psychol. 2002;38:291. [Google Scholar]
- [81].Cesario J, Grant H, Higgins ET. Regulatory fit and persuasion: transfer from “feeling right”. J Pers Soc Psychol. 2004;86:388–404. doi: 10.1037/0022-3514.86.3.388. [DOI] [PubMed] [Google Scholar]
- [82].Keller J, Bless H. Regulatory fit and cognitive performance: the interactive effect of chronic and situationally induced self-regulatory mechanisms on test performance. Eur J Soc Psychol. 2006;36:393–405. [Google Scholar]
- [83].Plessner H, Unkelbach C, Memmert D, Baltes A, Kolb A. Regulatory fit as a determinant of sport performance: how to succeed in a soccer penalty-shooting. Psychol Sport Exerc. 2009;10:108–15. [Google Scholar]
- [84].Idson LC, Liberman N, Higgins ET. Imagining how you'd feel: the role of motivational experiences from regulatory fit. Pers Soc Psychol Bull. 2004;30:926–37. doi: 10.1177/0146167204264334. [DOI] [PubMed] [Google Scholar]
- [85].Camacho CJ, Higgins ET, Luger L. Moral value transfer from regulatory fit: what feels right is right and what feels wrong is wrong. J Pers Soc Psychol. 2003;84:498. [PubMed] [Google Scholar]
- [86].Latimer AE, Rivers SE, Rench TA, Katulak NA, Hicks A, Hodorowski JK, Higgins ET, Salovey P. A field experiment testing the utility of regulatory fit messages for promoting physical activity. J Exp Soc Psychol. 2008;44:826–32. doi: 10.1016/j.jesp.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Latimer AE, Williams-Piehota P, Katulak NA, Cox A, Mowad L, Higgins ET, Salovey P. Promoting fruit and vegetable intake through messages tailored to individual differences in regulatory focus. Ann Behav Med. 2008;35:363–9. doi: 10.1007/s12160-008-9039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Uskul AK, Keller J, Oyserman D. Regulatory fit and health behavior. Psychol Health. 2008;23:327–46. doi: 10.1080/14768320701360385. [DOI] [PubMed] [Google Scholar]
- [89].Hong JW, Lee AY. Be fit and be strong: Mastering self-regulation through regulatory fit. J Consum Res. 2008;34:682–95. [Google Scholar]
- [90].Uskul AK, Sherman DK, Fitzgibbon J. The cultural congruency effect: Culture, regulatory focus, and the effectiveness of gain- vs. loss-framed health messages. JExpSocPsychol. 2009;45:535–41. [Google Scholar]
- [91].Horrigan J. Wireless Internet use. Pew Internet & American Life Project; Washington, D.C.: 2009. [Accessed June 1, 2010]. http://www.pewinternet.org/~/media//Files/Reports/2009/Wireless-Internet-Use.pdf. [Google Scholar]
- [92].Fox S. Digital divisions. Pew Internet & American Life Project; Washington, D.C.: 2005. [Accessed May 27, 2010]. http://www.pewinternet.org/~/media//Files/Reports/2005/PIP_Digital_Divisions_Oct_5_2005.pdf.pdf. [Google Scholar]
- [93].van Gerven PWM, Paas F, Van Merrienboer JJG, Hendriks M, Schmidt HG. The efficiency of multimedia learning into old age. Br J Educ Psychol. 2003;73:489–505. doi: 10.1348/000709903322591208. [DOI] [PubMed] [Google Scholar]
- [94].Jimison H, Gorman P, Woods S, Nygren P, Walker M, Norris S, Hersh W. Barriers and drivers of health information technology use for the elderly, chronically ill, and underserved. Evid Rep Technol Assess (Full Rep) 2008:1–1422. [PMC free article] [PubMed] [Google Scholar]
- [95].Sweeney MA, Chiriboga DA. Evaluating the effectiveness of a multimedia program on home safety. Gerontologist. 2003;43:325–34. doi: 10.1093/geront/43.3.325. [DOI] [PubMed] [Google Scholar]
- [96].Mahoney DF, Tarlow BJ, Jones RN, Sandaire J. Effects of a multimedia project on users' knowledge about normal forgetting and serious memory loss. J Am Med Inform Assoc. 2002;9:383–94. doi: 10.1197/jamia.M1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, Burke JR, Hurd MD, Potter GG, Rodgers WL, Steffens DC, McArdle JJ, Willis RJ, Wallace RB. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med. 2008;148:427–34. doi: 10.7326/0003-4819-148-6-200803180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Cook NL, Ayanian JZ, Orav EJ, Hicks LS. Differences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary care. Circulation. 2009;119:2463–70. doi: 10.1161/CIRCULATIONAHA.108.825133. [DOI] [PubMed] [Google Scholar]
- [99].Hayanga AJ, Waljee AK, Kaiser HE, Chang DC, Morris AM. Racial clustering and access to colorectal surgeons, gastroenterologists, and radiation oncologists by African Americans and Asian Americans in the United States: a county-level data analysis. Arch Surg. 2009;144:532–5. doi: 10.1001/archsurg.2009.68. [DOI] [PubMed] [Google Scholar]
- [100].Baer JS, Ball SA, Campbell BK, Miele GM, Schoener EP, Tracy K. Training and fidelity monitoring of behavioral interventions in muti-site addictions research: A review. Drug Alcohol Depend. 2007;87:107–18. doi: 10.1016/j.drugalcdep.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]