Abstract
Objective
The objectives of this study were to determine the frequency of symptomatic postdiscectomy pseudocyst (PP) after endoscopic discectomy and to compare the results of surgical and conservative management of them.
Methods
Initial study participants were 1,503 cases (1,406 patients) receiving endoscopic lumbar discectomy by 23-member board of neurosurgeons from March 2003 to October 2008. All patients' postoperative magnetic resonance imaging (MRI) scans were evaluated. On the postoperative MRI, cystic lesion of T2W high and T1W low at discectomy site was regarded as PP. Reviews of medical records and radiological findings were done. The PP patients were divided into two groups, surgical and conservative management by treatment modality after PP detection. We compared the results of the two groups using the visual analogue scale (VAS) for low back pain (LBP), VAS for leg pain (LP) and the Oswestry disability index (ODI).
Results
Among 1,503 cases of all male soldiers, the MRIs showed that pseudocysts formed in 15 patients, about 1.0% of the initial cases. The mean postoperative interval from surgery to PP detection was 53.7 days. Interlaminar approach was correlated with PP formation compared with transforaminal approach (p=0.001). The mean VAS for LBP and LP in the surgical group improved from 6.5 and 4.8 to 2.0 and 2.3, respectively. The mean VAS for LBP and LP in the conservative group improved from 4.4 and 4.4 to 3.9 and 2.3, respectively. There was no difference in treatment outcome between surgical and conservative management of symptomatic PP.
Conclusion
Although this study was done in limited environment, symptomatic PP was detected at two months' postoperative period in about 1% of cases. Interlaminar approach seems to be more related with PP compared with transforaminal approach.
Keywords: Endoscopic discectomy, Herniated disc, Lumbar, Postoperative complication, Pseudocyst
INTRODUCTION
Some patients may persistent pains or relapsing radiating pain after surgery for herniated lumbar disc. Among these patients, cystic lesions of discectomy site on postoperative magnetic resonance imaging scans (MRIs) may be evident56). Symptomatic post-discectomy pseudocysts (PP) of the lumbar discs are often detected from postoperative MRI in out-patient department without any reference. However, there is limited information on their pathogenesis, natural course, and frequency. In this study, we determined the frequency of symptomatic PP after endoscopic lumbar discectomy and compared the outcomes after surgical and conservative management of PP.
MATERIALS AND METHODS
Initial study participants were 1,503 consecutive cases (1,406 patients) who received endoscopic discectomies in one military hospital from March 2003 to October 2008. All patients were young, male soldiers at the time of their operations. Mean patient age was 22.6±5.8 (18 to 55) years. A 23-member board of neurosurgeons, all of whom were military surgeons at the time, performed the 1503 operations. There was no difference of surgical carrier as a neurosurgeon.
All lesions were confirmed by radiologic findings as protruded or extruded disc materials compressing the lumbar root(s). The endoscopic discectomies were performed using the Vertebris® system (Richard Wolf, GmbH, Knittlingen, Germany). The surgical approach was based on Rutten's method42,43). Usually, interlaminar endoscopic discectomy (ILED) was performed in L5/S1 level. Transforaminal endoscopic discectomy (TFED) was performed in all other cases and some limited L5/S1 cases. Most patients received intraoperative epidural steroids at the end of their surgeries. We reviewed all the patients' medical records and radiology findings. All patients received postoperative magnetic resonance imaging scans (MRIs) within 7 days after surgery. When new symptoms occurred, follow-up MRIs were checked. Radiologically, cystic lesion of T2W high and T1W low signal intensity at discectomy site regarded as PP. The incidence of this cystic lesion was calculated and their medical records were reviewed.
PP patients were divided into two groups according to the treatment modality after PP detection, surgically treated (S) and conservatively treated (C). We compared the outcomes. Because of the limited period of military medical service, final follow up of clinical findings including the Visual Analogue Scale (VAS) for low back pain (LBP), the VAS for leg pain (LP), and the Oswestry Disability Index (ODI) were done by telephone. The paired t-test was used for the statistical analysis.
RESULTS
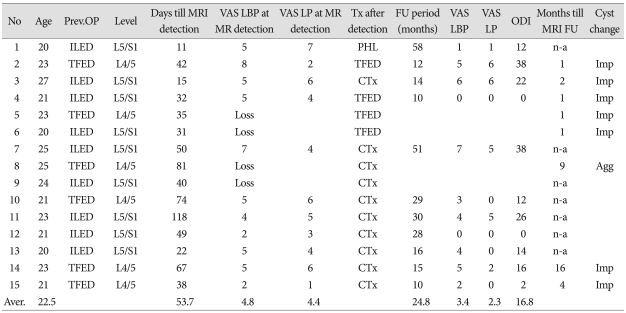
A total of 1,406 patients underwent endoscopic discectomies. Symptomatic PPs were found in 15 patients, about 1% of the initial cases. Mean age of the PP group was 22.5±2.1 years. The 15 PP patients were distributed among 11 surgeons and showed an even distribution among the surgeons involved. All disc protrusion was subligamentously constrained. There were no findings of posterior longitudinal ligament rupture on preoperative MRI. The VAS of LBP, LP and ODI before initial surgery were 3.9±1.2, 5.8±0.9 and 39.2±4.7%, respectively. The symptoms of all patients improved after surgery and aggravated. The VAS of LBP and LP at the time of PP detection with MRI were 4.8±1.9 and 4.4±1.9, respectively. After 24.8±16.5 months of mean follow up, the VAS of LBP and LP were 3.4±2.4 and 2.3±2.6, respectively. The ODI checked at last follow-up was 16.4±13.6%. The interval between discectomy and pseudocyst detection via MRI was 53.7±44.1 (11-118) days (Fig. 1, Table 1).
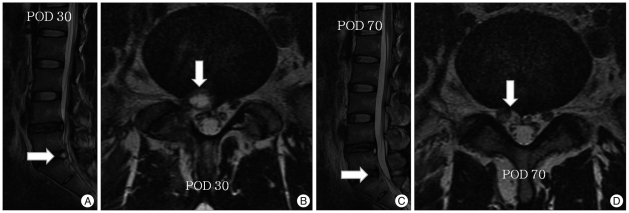
Fig. 1.
MRIs of Case 3, who underwent right L5/S1 endoscopic discectomy via interlaminar approach. A and B : Lumbar MRIs on Day 30 shows a pseudocyst (arrow) compressing the neural structures at the discectomy site. C and D : Lumbar MRIs on Day 70 shows complete resolution (arrow) of the right L5/S1 pseudocyst and epidural decompression at the right S1 root.
Table 1.
Patients with a pseudocyst after lumbar discectomy, seen on MRI during follow-up
OP : operation, MRI : magnetic resonance images, VAS : Visual Analogue Scale, LBP : low back pain, LP : leg pain, Tx : treatment, FU : follow up, ODI : Oswestry Disability Index, TFED : transforaminal endoscopic discectomy, ILED : interlaminar endoscopic discectomy, PHL : partial hemilaminectomy and discectomy, CTx : conservative treatment, BTW : between jobs, Aver : average, Imp : improved, Agg : aggravated, n-a : not available
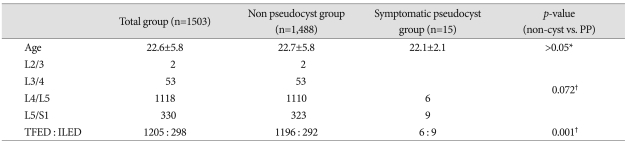
Among these 15 affected patients, 6 had discectomies at the L4-5 via transforaminal approach and 9 at the L5-S1 level via interlaminar approach. Operation levels had no significant differences with total group. However, approach trajectory of PP group, which was transforaminal or interlaminar, had significant difference with total group (p=0.001) (Table 2).
Table 2.
The result of comparison between total surgical group and postdiscectomy pseudocyst groups
PP : post-discectomy pseudocyst, TFED : transforaminal endoscopic discectomy, ILED : interlaminar endoscopic discectomy. *Statistical significances were tested by Student t-test between groups. †Statistical significances were tested by Pearson's chi-square between groups
The 15 patients divided into 2 groups according to the treatment modality after PP had been detected, surgical treatment group (S) and conservative treatment group (C). Five patients had got surgical treatment and 10 patients had got conservative treatment. In the cases of surgical treatment group (S), 1 microscopic partial hemilaminectomy and 4 transforaminal endoscopic discectomy were done. Because of lack of intraoperative image, we could not obtain specific operation finding and pathology. In the cases of endoscopic reoperation, it is not possible to tell the difference between irrigation fluid and cystic fluid. Because of limitation of visual fields according to the transforaminal approach, there were no specific operation findings except bulging posterior annulus and longitudinal ligament.
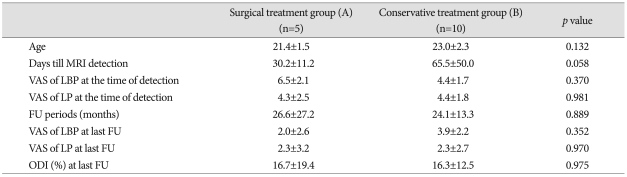
The VAS for the LBP and LP at the time of pseudocyst detection in the surgical treatment group (S) were 6.5±2.1 and 4.3±2.5, respectively. The VAS for the LBP and LP in the conservative treatment group (C) were 4.4±1.7 and 4.4±1.8, respectively. The mean follow up was 26.6±27.2 months in group (S) and 24.1±13.3 months in group (C). The VAS for the LBP, the VAS for LP and the ODI for group (S) at the last follow up were 2.0±2.6, 2.3±3.2 and 16.7±19.4, respectively. For group (C), the VAS for the LBP, the VAS for the LP and the ODI were 3.9±2.2, 2.3±2.7 and 16.3±12.5, respectively. There was no difference in the treatment outcome between groups (S) and (C). (Table 3)
Table 3.
Comparison of treatment results between the surgical treatment group (A) and the conservative treatment group (B)
MRI : magnetic resonance images, VAS : visual analogue scale, LBP : low back pain, LP : leg pain, FU : follow up, ODI : Oswestry disability index
There was no recurrent PP after surgical treatment. In cases of conservative group, the PPs decreased in 3 cases on the follow-up MRI (Fig. 1, Table 1). However, one caes showed aggravated PP in the MRI checked 9 months after surgery
DISCUSSION
There has been little information on post-discectomy pseudocysts (PP)56). However, with the development of diagnostic Park performance, it is speculated that PPs will be more frequently detected than the past. The PP differs from juxtafacet, perineural, and ganglion cysts in that it develops over a relatively short interval after a discectomy and the cyst is in communication with the intervertebral disc. PP resembles a cyst of the disc, as several previous studies have described20,28,33). However, PP is different from a cyst of the disc in that PP has an incomplete cystic wall, as suggested by its name56).
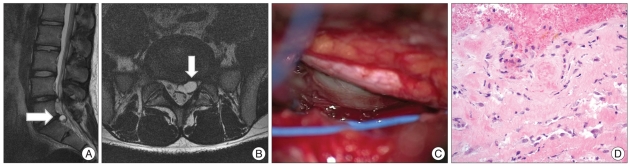
The cytological and pathologic findings with regard to one PP (not included in this study) showed many RBCs, with some macrophages, and soft fibrotic tissue with inflammatory changes. Surgery on this PP revealed that the cystic wall, located around the posterior longitudinal ligament previously operated upon, was compressing the corresponding root; this was also visible in MRIs (Fig. 2).
Fig. 2.
Case illustration of symptomatic PP, detected 5 months after endoscopic discectomy via the interlaminar approach (used with the permission of Dr. Hoon Kim). A and B : A 17 mm cystic mass, between dura and posterior longitudinal ligament, at L5/S1-level compressing the left S1 root. C : Intraoperative finding shows cystic mass beneath left S1 root being compressed. D : Microscopic view of cystic wall shows fibrous tissue with some inflammatory cells, indicating an inflammatory reaction with some hemorrhages.
An April 2010 PubMed search for "lumbar disc," "discectomy," or "complication" yielded no reports on PP. Most of the published literature is on lumbar discectomy complications, such as postoperative wound hematoma, neuronal injury (including postoperative dysethesia), recurrent herniation, postoperative instability, wrong level of exposure, arachnoiditis, infection, incidental durotomy (including its long term sequelae), and pseudomeningoceles1,2,5,9,18,26,35,38-40,47,49,51,53,54). In addition, there have been case reports of rare complications after lumbar discectomy, such as development of an arteriovenous fistula, major vessel injury, epidural fibrosis, ureteral injury, compartment syndrome with acute renal failure, iliac artery injury, intradural disc migration, bowel injury, septicemia, symptomatic pneumorachis, instrument failure, postoperative radicular neuroma, Ogilvie's syndrome, and reflex sympathetic dystrophy3,4,10,12,13,15-17,19,21,22,34,36,37,41,44,45,48,52).
In reports on cases subsequent to full endoscopic discectomy, published complications have included recurrent disc herniation on the same side, incomplete removal of a ruptured disc, infection, neuronal injury (including sensory changes), dural tears, vascular injury, psoas hematoma, and sympathetically mediated pain6-8,11,14,23-27,29,32,35,42,43,46,55).
In this study, symptomatic PP occurred in about 1% of patients after endoscopic discectomy and three cases treated by conservative manage showed decreased cyst size. We believe this is reason why there was little literature about PPs.
Fortunately, we found one report of two cases of 'postoperative annular pseudocyst'. In this report, 60-year-old man and 38-year-old man presented postoperative annular pseudocyst at L4/5 and 5/S1on the MRI checked 13 months and 14 months after hemilaminectomy and discectomy, respectively. Their recurrent symptoms were developed 1 month and 8 months after initial surgery. Sixty-year-old man received conservative management and 38-year-old man received needle aspiration and steroid injection. Comparing with this report, the period from surgery to PP detection in this study, 54 days, seemed to be too short. We thought the difference of insurance system between two countries made this different result.
Pathogenesis of PP is likely associated with inflammation of the connective tissue at the procedure site, resulting in the pseudocyst. In particular, postoperative inflammatory reaction of posterior longitudinal ligament (PLL) and annulus complex were supposed to be related with PP formation56). In this study, the result of surgical trajectory that thought be related with PP support this supposition. Also, contrary to the transforaminal approach, the interlaminar approach expose more PLL and during endoscopic surgery, heat from radiofrequency (RF) cautery or laser coagulation can cause inflammation. Although irrigation is used throughout such surgery, previous reports on cancer treatment have revealed that the intraoperative RF thermal injury can be significant30,31,50). If the pseudocyst's internal space connects with the epidural or extraforaminal space, there are no massive effects or clinical symptoms such as low back pain and/or leg pain. Without a connection between the two spaces, the pseudocyst can be enlarged which may compress the neuronal structures until the inflammation subsides.
As mentioned above, there was one patient experienced spontaneous regression 70 days after surgery. Two patients showed decreased PP on MRI follow-up. Furthermore, the result of conservative treatment and surgical treatment were not different. However, Young recommended that percutaneous aspiration and steroidal injection may represent a potential therapy for PP56). Unfortunately, one of our patients showed aggravated PP on the MRI 9 months after surgery. In the cases of Young, the PP detected 13 and 14 months after surgery. Considering these data, we recommend non-surgical treatments initially rather than surgery, because there will be possibility of spontaneous regression of PP.
All patients in this study were young, adult males, which are thought to be the limitation. However, in some respects, this homogeneity strengthens the study. On the other hand, there is a possibility that PP may be prone to occur predominantly in young intervertebral discs or in males. Thus, further studies with a large mixed population are required to verify the pathogenesis and natural course of PP.
CONCLUSION
Although there are limitations in this study, the results of this study showed that in about 1% of endoscopic lumbar discectomy patients, symptomatic post-discectomy pseudocysts (PP) were detectable via MRI within 2 months. The surgical trajectory of endoscope seems to be related with the formation of PP. Further reports and studies are required to reveal PP's pathogenesis and natural course.
Acknowledgements
Personally, I would like to appreciate 22 neurosurgeons used to be military neurosurgeons in one military hospital from 2003 to 2008 (Doo Sik Kong, Ji Ha Kim, Chi Heon Kim, Hyung Suk Kim, Kyung-Yoon Moon, Jun Hong Min, Kwan Woong Park, Jin Young Park, Jae Seung Bang, Keun Soo Won, Eun Sang Lee, Hae Il Lee, Hyun Wook Lee, Sang Ho Cheon, Hyo Chul Cheon, Byung Wook Chung, Young Hyun Cho, Yong Jun Jin, Yuol Choi, Hwan Young Choi, In Bo Han and Won Jin Hong).
References
- 1.Babar S, Saifuddin A. MRI of the post-discectomy lumbar spine. Clin Radiol. 2002;57:969–981. doi: 10.1053/crad.2002.1071. [DOI] [PubMed] [Google Scholar]
- 2.Beldzinski P, Stempniewicz M, Sloniewski P. Posterior lumbar interbody fusion of the lumbo-sacral spine - treatment outcomes. Ortop Traumatol Rehabil. 2004;6:288–292. [PubMed] [Google Scholar]
- 3.Caner H, Bavbek M, Albayrak A, Altinörs TC. Ogilvie's syndrome as a rare complication of lumbar disc surgery. Can J Neurol Sci. 2000;27:77–78. doi: 10.1017/s0317167100052033. [DOI] [PubMed] [Google Scholar]
- 4.Chang CP, Lee WS, Lee SC. Left internal iliac artery and vein tear during microendoscopic lumbar discectomy - a case report. Minim Invasive Ther Allied Technol. 2006;15:155–158. doi: 10.1080/13645700600771686. [DOI] [PubMed] [Google Scholar]
- 5.Chang SS, Fu TS, Liang YC, Lia PL, Niu CC, Chen LH, et al. Results of microendoscopic discectomy performed in the 26 cases with a minimum 3 years follow-up. Chang Gung Med J. 2009;32:89–97. [PubMed] [Google Scholar]
- 6.Choi G, Lee SH, Raiturker PP, Lee S, Chae YS. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006;58:ONS59–ONS68. doi: 10.1227/01.neu.0000192713.95921.4a. discussion ONS59-ONS68. [DOI] [PubMed] [Google Scholar]
- 7.Choi G, Lee SH, Bhanot A, Raiturker PP, Chae YS. Percutaneous endoscopic discectomy for extraforaminal lumbar disc herniations : extraforaminal targeted fragmentectomy technique using working channel endoscope. Spine (Phila Pa 1976) 2007;32:E93–E99. doi: 10.1097/01.brs.0000252093.31632.54. [DOI] [PubMed] [Google Scholar]
- 8.Choi G, Lee SH, Lokhande P, Kong BJ, Shim CS, Jung B, et al. Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope. Spine (Phila Pa 1976) 2008;33:E508–E515. doi: 10.1097/BRS.0b013e31817bfa1a. [DOI] [PubMed] [Google Scholar]
- 9.Cole JS, 4th, Jackson TR. Minimally invasive lumbar discectomy in obese patients. Neurosurgery. 2007;61:539–544. doi: 10.1227/01.NEU.0000290900.23190.C9. discussion 544. [DOI] [PubMed] [Google Scholar]
- 10.Coskun E, Süzer T, Topuz O, Zencir M, Pakdemirli E, Tahta K. Relationships between epidural fibrosis, pain, disability, and psychological factors after lumbar disc surgery. Eur Spine J. 2000;9:218–223. doi: 10.1007/s005860000144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ditsworth DA. Endoscopic transforaminal lumbar discectomy and reconfiguration : a postero-lateral approach into the spinal canal. Surg Neurol. 1998;49:588–597. doi: 10.1016/s0090-3019(98)00004-4. discussion 597-588. [DOI] [PubMed] [Google Scholar]
- 12.Domsky R, Goldberg ME, Hirsh RA, Scaringe D, Torjman MC. Critical failure of a percutaneous discectomy probe requiring surgical removal during disc decompression. Reg Anesth Pain Med. 2006;31:177–179. doi: 10.1016/j.rapm.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Erman T, Tuna M, Göçer AI, Idan F, Akgül E, Zorludemir S. Postoperative radicular neuroma. Case report. Neurosurg Focus. 2001;11:ecp. doi: 10.3171/foc.2001.11.5.9. [DOI] [PubMed] [Google Scholar]
- 14.Frank E. Endoscopically assisted open removal of laterally herniated lumbar discs. Surg Neurol. 1997;48:430–433. doi: 10.1016/s0090-3019(97)00286-3. discussion 433-434. [DOI] [PubMed] [Google Scholar]
- 15.Gazzeri R, Galarza M, Neroni M, Esposito S, Alfieri A. Fulminating septicemia secondary to oxygen-ozone therapy for lumbar disc herniation : case report. Spine (Phila Pa 1976) 2007;32:E121–E123. doi: 10.1097/01.brs.0000254125.85406.6e. [DOI] [PubMed] [Google Scholar]
- 16.Grane P. The postoperative lumbar spine. A radiological investigation of the lumbar spine after discectomy using MR imaging and CT. Acta Radiol Suppl. 1998;414:1–23. [PubMed] [Google Scholar]
- 17.Hekal IA, Mohsen T, Nabeeh A. Ureteric injury after lumbosacral discectomy : a case report and review of the literature. J Trauma. 2008;64:1387–1391. doi: 10.1097/TA.0b013e31816bbe4c. [DOI] [PubMed] [Google Scholar]
- 18.Hoogland T, van den Brekel-Dijkstra K, Schubert M, Miklitz B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation : a prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976) 2008;33:973–978. doi: 10.1097/BRS.0b013e31816c8ade. [DOI] [PubMed] [Google Scholar]
- 19.Houten JK, Frempong-Boadu AK, Arkovitz MS. Bowel injury as a complication of microdiscectomy : case report and literature review. J Spinal Disord Tech. 2004;17:248–250. doi: 10.1097/00024720-200406000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Hwang JH, Park IS, Kang DH, Jung JM. Discal cyst of the lumbar spine. J Korean Neurosurg Soc. 2008;44:262–264. doi: 10.3340/jkns.2008.44.4.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inamasu J, Guiot BH. Vascular injury and complication in neurosurgical spine surgery. Acta Neurochir (Wien) 2006;148:375–387. doi: 10.1007/s00701-005-0669-1. [DOI] [PubMed] [Google Scholar]
- 22.Jeon SH, Lee SH, Choi WC. Iliac artery perforation following lumbar discectomy with microsurgical carbon dioxide laser : a report of a rare case and discussion on the treatment. Spine (Phila Pa 1976) 2007;32:E124–E125. doi: 10.1097/01.brs.0000254078.88358.33. [DOI] [PubMed] [Google Scholar]
- 23.Kambin P. Arthroscopic microdiscectomy. Arthroscopy. 1992;8:287–295. doi: 10.1016/0749-8063(92)90058-j. [DOI] [PubMed] [Google Scholar]
- 24.Kambin P, Cohen LF. Arthroscopic microdiscectomy versus nucleotomy techniques. Clin Sports Med. 1993;12:587–598. [PubMed] [Google Scholar]
- 25.Kim HS, Ju CI, Kim SW, Kim JG. Endoscopic transforaminal suprapedicular approach in high grade inferior migrated lumbar disc herniation. J Korean Neurosurg Soc. 2009;45:67–73. doi: 10.3340/jkns.2009.45.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kotil K, Akcetin M, Bilge T. A minimally invasive transmuscular approach to far-lateral L5-S1 level disc herniations : a prospective study. J Spinal Disord Tech. 2007;20:132–138. doi: 10.1097/01.bsd.0000211268.43744.2a. [DOI] [PubMed] [Google Scholar]
- 27.Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir (Tokyo) 2008;48:383–388. doi: 10.2176/nmc.48.383. discussion 388-389. [DOI] [PubMed] [Google Scholar]
- 28.Lee HK, Lee DH, Choi CG, Kim SJ, Suh DC, Kahng SK, et al. Discal cyst of the lumbar spine : MR imaging features. Clin Imaging. 2006;30:326–330. doi: 10.1016/j.clinimag.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 29.Lee S, Kim SK, Lee SH, Kim WJ, Choi WC, Choi G, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation : classification of disc migration and surgical approaches. Eur Spine J. 2007;16:431–437. doi: 10.1007/s00586-006-0219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lencioni R, Cioni D, Donati F, Bartolozzi C. Combination of interventional therapies in hepatocellular carcinoma. Hepatogastroenterology. 2001;48:8–14. [PubMed] [Google Scholar]
- 31.Llovet JM. Updated treatment approach to hepatocellular carcinoma. J Gastroenterol. 2005;40:225–235. doi: 10.1007/s00535-005-1566-3. [DOI] [PubMed] [Google Scholar]
- 32.Mayer HM, Brock M. Percutaneous endoscopic discectomy : surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–225. doi: 10.3171/jns.1993.78.2.0216. [DOI] [PubMed] [Google Scholar]
- 33.Nabeta M, Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T. Discal cysts of the lumbar spine. Report of five cases. J Neurosurg Spine. 2007;6:85–89. doi: 10.3171/spi.2007.6.1.17. [DOI] [PubMed] [Google Scholar]
- 34.Nam TK, Park SW, Shim HJ, Hwang SN. Endovascular treatment for common iliac artery injury complicating lumbar disc surgery : limited usefulness of temporary balloon occlusion. J Korean Neurosurg Soc. 2009;46:261–264. doi: 10.3340/jkns.2009.46.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nellensteijn J, Ostelo R, Bartels R, Peul W, van Royen B, van Tulder M. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations : a systematic review of the literature. Eur Spine J. 2010;19:181–204. doi: 10.1007/s00586-009-1155-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perrot S, Ziza JM, Khalifa P, Chazerain P, Campagne JP, Le Quintrec JL. [Persistent pain following discal sciatica : reflex sympathetic dystrophy, an unusual complication to be examined. Apropos of 4 cases] Rev Rhum Mal Osteoartic. 1992;59:745–747. [PubMed] [Google Scholar]
- 37.Prabhakar H, Bithal PK, Dash M, Chaturvedi A. Rupture of aorta and inferior vena cava during lumbar disc surgery. Acta Neurochir (Wien) 2005;147:327–329. doi: 10.1007/s00701-004-0405-2. [DOI] [PubMed] [Google Scholar]
- 38.Ramirez LF, Thisted R. Using a national health care data base to determine surgical complications in community hospitals : lumbar discectomy as an example. Neurosurgery. 1989;25:218–225. doi: 10.1097/00006123-198908000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Ramirez LF, Thisted R. Complications and demographic characteristics of patients undergoing lumbar discectomy in community hospitals. Neurosurgery. 1989;25:226–230. doi: 10.1097/00006123-198908000-00012. discussion 230-231. [DOI] [PubMed] [Google Scholar]
- 40.Rocca A, Turtas S, Pirisi A, Agnetti V. Iatrogenic lumbar pseudomeningocele. Zentralbl Neurochir. 1986;47:311–315. [PubMed] [Google Scholar]
- 41.Rovlias A, Pavlakis E, Kotsou S. Symptomatic pneumorachis associated with incidental durotomy during microscopic lumbar disc surgery. Case report. J Neurosurg Spine. 2006;5:165–167. doi: 10.3171/spi.2006.5.2.165. [DOI] [PubMed] [Google Scholar]
- 42.Ruetten S, Komp M, Godolias G. A New full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6-mm endoscopes : prospective 2-year results of 331 patients. Minim Invasive Neurosurg. 2006;49:80–87. doi: 10.1055/s-2006-932172. [DOI] [PubMed] [Google Scholar]
- 43.Ruetten S, Komp M, Merk H, Godolias G. Use of newly developed instruments and endoscopes : full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine. 2007;6:521–530. doi: 10.3171/spi.2007.6.6.2. [DOI] [PubMed] [Google Scholar]
- 44.Santos E, Peral V, Aroca M, Hernández Lezana A, Serrano FJ, Vilacosta I, et al. Arteriovenous fistula as a complication of lumbar disc surgery : case report. Neuroradiology. 1998;40:459–461. doi: 10.1007/s002340050624. [DOI] [PubMed] [Google Scholar]
- 45.Sarliève P, Delabrousse E, Clair C, Hussein HH, Schmitt C, Kastler B. Intradural disc herniation with cranial migration of an excluded fragment. Clin Imaging. 2004;28:170–172. doi: 10.1016/S0899-7071(03)00147-5. [DOI] [PubMed] [Google Scholar]
- 46.Savitz MH, Doughty H, Burns P. Percutaneous lumbar discectomy with a working endoscope and laser assistance. Neurosurg Focus. 1998;4:e9. doi: 10.3171/foc.1998.4.2.12. [DOI] [PubMed] [Google Scholar]
- 47.Saxler G, Krämer J, Barden B, Kurt A, Pförtner J, Bernsmann K. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine (Phila Pa 1976) 2005;30:2298–2302. doi: 10.1097/01.brs.0000182131.44670.f7. [DOI] [PubMed] [Google Scholar]
- 48.Smuck M, Benny B, Han A, Levin J. Epidural fibrosis following percutaneous disc decompression with coblation technology. Pain Physician. 2007;10:691–696. [PubMed] [Google Scholar]
- 49.Stolke D, Sollmann WP, Seifert V. Intra- and postoperative complications in lumbar disc surgery. Spine (Phila Pa 1976) 1989;14:56–59. doi: 10.1097/00007632-198901000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Tacke J, Mahnken AH, Günther RW. [Percutaneous thermal ablation of renal neoplasms] Rofo. 2005;177:1631–1640. doi: 10.1055/s-2005-858819. [DOI] [PubMed] [Google Scholar]
- 51.Tasdemiroğlu E, Sengöz A, Bagatur E. Iatrogenic spondylodiscitis. Case report and review of literature. Neurosurg Focus. 2004;16:ECP1. [PubMed] [Google Scholar]
- 52.Torun F, Tuna H, Deda H. Abdominal vascular injury during lumbar disc surgery : report of three cases. Ulus Travma Acil Cerrahi Derg. 2007;13:165–167. [PubMed] [Google Scholar]
- 53.Vogelsang H, Stolke D. [Pseudomeningoceles--a rare complication following lumbar intervertebral disk operations] Neurochirurgia (Stuttg) 1984;27:73–77. doi: 10.1055/s-2008-1053733. [DOI] [PubMed] [Google Scholar]
- 54.Wiese M, Krämer J, Bernsmann K, Ernst Willburger R. The related outcome and complication rate in primary lumbar microscopic disc surgery depending on the surgeons experience : comparative studies. Spine J. 2004;4:550–556. doi: 10.1016/j.spinee.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 55.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation : surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722–731. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 56.Young PM, Fenton DS, Czervionke LF. Postoperative annular pseudocyst : report of two cases with an unusual complication after microdiscectomy, and successful treatment by percutaneous aspiration and steroid injection. Spine J. 2009;9:e9–e15. doi: 10.1016/j.spinee.2007.12.013. [DOI] [PubMed] [Google Scholar]