Abstract
A 34-year-old female patient was presented with leg and hip pain for 6 months as well as voiding difficulty for 1 year. Magnetic resonance imaging revealed a well-demarcated mass lesion at L2-3. The mass was hypo-intense on T1- and T2-weighted images with homogeneous gadolinium enhancement. Surgery was performed with the presumptive diagnosis of intradural extramedullary meningioma. Complete tumor removal was possible due to lack of dural adhesion of the tumor. Histologic diagnosis was clear cell meningioma, a rare and newly included World Health Organization classification of meningioma usually affecting younger patients. During postoperative 2 years, the patient has shown no evidence of recurrence. We report a rare case of cauda equina clear cell meningioma without any dural attachment.
Keywords: Clear cell meningioma, Spinal meningioma, World Health Organization classification, Younger patients, Cauda equina
INTRODUCTION
Clear cell meningioma is a very rare histological type of meningioma that is included in the World Health Organization (WHO) classification as a peculiar variant affecting younger patients10,14,24,25). Clear cell meningiomas have been reported in only 0.2% of meningioma cases and have a more aggressive and complicated course due to their histological nature and anatomical locations25). Most meningiomas are attached to the dura mater and very seldomly they grow without dural attachment. To the best of our knowledge, only several cases of intraspinal non-dura based clear cell meningioma have been reported2,5,17,19,20). In this article, we present an unusual case of intraspinal clear cell meningioma characterized by the absence of dural attachment.
CASE REPORT
A 34-year-old female patient was admitted with complaints of pain in her lower limbs and both hips for 6 months and voiding difficulty for 1 year. She had also experienced numbness in her lower limbs. Her symptoms worsened over time. One year prior to admission, she visited a local obstetrics and gynecology clinics complaining voiding difficulty and was treated conservatively under the diagnosis of cystitis without any symptomatic improvement. Physical examination revealed non-specific 71findings. The motor power of her lower limbs was normal, and rectal examination revealed normal anal tone.
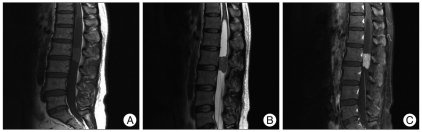
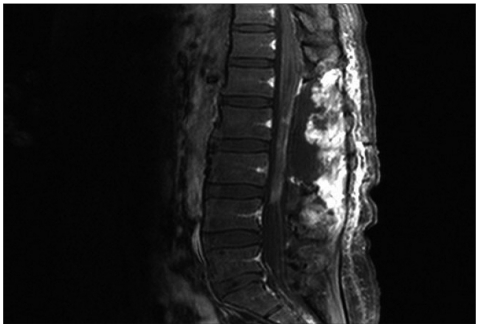
Magnetic resonance (MR) imaging showed a well-demarcated 1.5×1.9×2.9 cm sized mass lesion at L2-3. The mass was hypo- intense on T1- and T2-weighted images with homogeneous gadolinium enhancement. There was also a cystic lesion within the spinal cord on the cranial side of the mass at T12-L2. The cyst was isointense to the cerebrospinal fluid and was diagnosed to be tumor associated syrinx (Fig. 1). Myelography of the lumbar spine revealed obstruction of contrast flow due to the intradural mass. Operation was conducted with the presumptive diagnosis of intradural extramedullary meningioma. An L1-3 laminectomy and intradural exposure revealed a yellowish pink, well-encapsulated, elliptical mass of firm consistency. The tumor was found to be draped by and adhered to the nerve roots at its upper pole near the conus medullaris and cauda equina at its lower pole without dural attachment. However, the tumor was successfully dissected from the nerve roots and removed completely. The patient recovered uneventfully after the operation. The postoperative MR imaging showed no residual tumor with marked reduction of the syrinx. All of the patient's preoperative symptoms improved after surgery.
Fig. 1.
Sagittal magnetic resonance imaging shows a well-demarcated mass lesion at L2-3. The mass lesion is hypo-intense on T1-weighted (A) and T2-weighted (B) images and shows homogenous enhancement with gadolinium (C). There is a cystic lesion within the spinal cord on the cranial side of the mass at T12-L2. The cyst is iso-intense with cerebrospinal fluid (A, B and C).
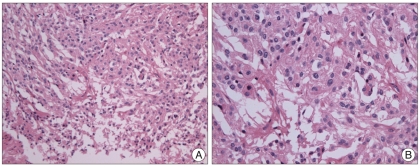
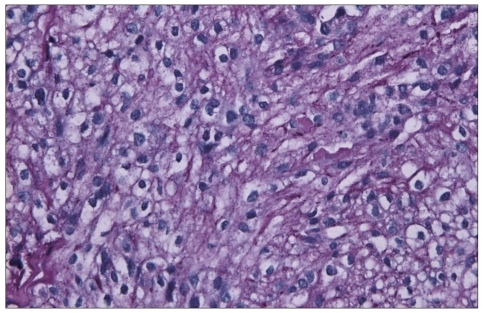
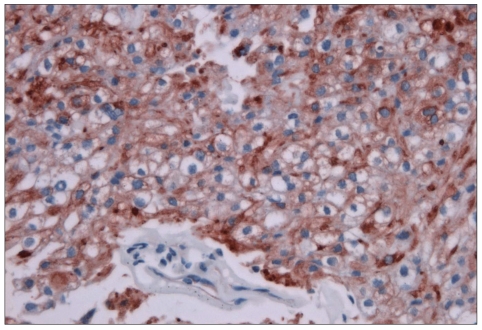
The histology of the tumor showed patternless sheets of polygonal cells with clear glycogen-rich cytoplasm and small clusters of cells in a meningothelial pattern with whorl formation (Fig. 2). A Periodic acid-Schiff (PAS) stain showed a positive reaction in the cytoplasm of tumor cells containing glycogen (Fig. 3). Tumor cells were stained positive for vimentin (Fig. 4) and epithelial membrane antigen (EMA). These findings were compatible with the diagnosis of clear cell meningioma. Postoperatively, the patient's symptoms were dramatically alleviated. Adjuvant therapy was not performed. The postoperative one-year follow-up MR imaging showed no evidence of tumor recurrence (Fig. 5). The patient has not had any complaints or neurological symptoms for two years.
Fig. 2.
Photomicrograph showing patternless sheets of polygonal cells with clear glycogen-rich cytoplasm and small clusters of cells in a meningothelial pattern with whorl formation (A, H&E ×200) (B, H & E ×400).
Fig. 3.
Photomicrograph of Periodic acid-Schiff stain showing positive reactions in the cytoplasm of tumor cells containing glycogen (×400).
Fig. 4.
Tumor cells staining positive for vimentin (×400).
Fig. 5.
Postoperative (1 year after surgery) magnetic resonance imaging shows reduction of the previously dilated central spinal canal and no residual tumor.
DISCUSSION
Zorludemir et al.25) described clear cell meningioma as a distinct variant of meningioma for the first time in 1995. Scheithauer23) described its histologic and ultrastructural features. Although it is a benign variant of meningioma22), it is found to recur relatively frequently and even metastasize1); this behavior resulted in a change in its WHO classification from grade I to grade II10).
The proportion of spinal to total meningiomas is higher for clear cell meningiomas (45%) than for other meningiomas (the highest being 20% of the reported cases)19). They also tend to present at younger ages1,13) and occur in the lower thoracic, lumbar or lumbosacral region. Heth et al.6) believed that a family history might be a risk factor for this type of meningioma.
Histologically, clear cell meningioma contains sheets of clear, glycogen-rich (Periodic acid-Schiff positive, diastase-labile), polygonal cells forming only a few vague whorls25). Its abundant glycogen is what gives the name, "clear cell," to this particular type of meningioma20). Whorl formation is histologic feature in the differentiation of clear cell meningioma from a metastatic deposit of so-called clear cell carcinoma, including renal cell carcinoma, which is negative or very weakly positive for vimentin. Microcystic meningioma should also be distinguished from clear cell meningioma, among other variants of meningioma25). Although both tumors have a clear appearance, microcystic meningioma has clear extracellular spaces of varying size that contain pale fluid, whereas the clear cytoplasm of clear cell meningioma is relatively uniform and contains abundant glycogen25).
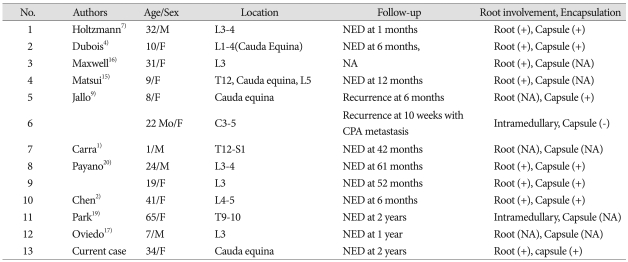
The imaging features of clear cell meningiomas do not differ from those of other common types of meningiomas3). Spinal clear cell meningioma usually occurs as an intradural extramedullary tumor with fairly homogeneous contrast enhancement3). Some cases show foraminal extension lacking dural attachment, just like schwannomas2). Even an intramedullary clear cell meningioma has been reported19). Because of radiologic and gross morphologic similarities between the spinal meningiomas and other intradural extramedullary spinal tumors including schwannomas, neurofibromas, paragangliomas and myxopapillary ependymomas, accurate histological diagnosis is improtant20). It is noteworthy that some clear cell meningiomas are not attached to the dura but to the neural sheath, as in the present case. Twelve such non dura-based intraspinal clear cell meningioma have been reported to date (Table 1).
Table 1.
Summary of cases with non-dura based intraspinal clear cell meningiomas in the literature
CPA : cerebellopontine angle, NA : not available, NED : no evidence of disease, Root (+) : adhesion to nerve root confirmed in the literature, Capsule (+) : existence of capsule confirmed in the literature
Because of the rarity of this type of meningioma, it was difficult for us to draw conclusive methods of treatment, especially in regard to radiotherapy. Another problem with treatment planning is that there has been discrepancies between histological findings and prognosis, showing no histologic features having prognostic significance18). Total surgical removal is the goal of treatment3). Subtotal resection is likely to have recurrence or progression21). Statistically, the role of radiotherapy has not been proven to be effective, but there has been a tendency towards a lower recurrence rate after postoperative radiotherapy3). On the other hand, some authors have suggested that radiotherapy should be performed only after partial resection or at recurrence11,12). In young children with clear cell meningioma, in particular, Carra et al.1) have suggested a reasonably aggressive surgical approach at diagnosis whenever possible, followed by meticulous follow-up in consideration of the potential serious late effects of radiotherapy.
The recurrence rate of clear cell meningioma is reported to be 42-61% in operative cases3,9,20,25). Intraspinal clear cell meningioma is associated with a lower rate of recurrence than the intracranial variant8). Of the patients described in the literature who had no recurrences, all had undergone gross-total resection3). The follow-up plan should include imaging of the entire neuroaxis for possible metastasis3).
CONCLUSION
Intraspinal clear cell meningioma is an uncommon WHO grade II meningioma with high recurrence rate in cases of partial removal. We report a rare case of cauda equina clear cell meningioma without dural attachment, which was successfully treated by gross total resection.
Acknowledgements
This was supported for two years by Pusan National University Research Grant.
References
- 1.Carra S, Drigo P, Gardiman M, Perilongo G, Rigobello L. Clear-cell meningioma in a 22-month-old male : a case report and literature review. Pediatr Neurosurg. 2001;34:264–267. doi: 10.1159/000056035. [DOI] [PubMed] [Google Scholar]
- 2.Chen MH, Chen SJ, Lin SM, Chen MH. A lumbar clear cell meningioma with foraminal extension in a renal transplant recipient. J Clin Neurosci. 2004;11:665–667. doi: 10.1016/j.jocn.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 3.Dhall SS, Tumialán LM, Brat DJ, Barrow DL. Spinal intradural clear cell meningioma following resection of a suprasellar clear cell meningioma. Case report and recommendations for management. J Neurosurg. 2005;103:559–563. doi: 10.3171/jns.2005.103.3.0559. [DOI] [PubMed] [Google Scholar]
- 4.Dubois A, Sevely A, Boetto S, Delisle MB, Manelfe C. Clear-cell meningioma of the cauda equina. Neuroradiology. 1998;40:743–747. doi: 10.1007/s002340050676. [DOI] [PubMed] [Google Scholar]
- 5.Epstein NE, Drexler S, Schneider J. Clear cell meningioma of the cauda equina in an adult: case report and literature review. J Spinal Disord Tech. 2005;18:539–543. doi: 10.1097/01.bsd.0000173314.98401.b5. [DOI] [PubMed] [Google Scholar]
- 6.Heth JA, Kirby P, Menezes AH. Intraspinal familial clear cell meningioma in a mother and child. Case report. J Neurosurg. 2000;93:317–321. doi: 10.3171/spi.2000.93.2.0317. [DOI] [PubMed] [Google Scholar]
- 7.Holtzman RN, Jormark SC. Nondural-based lumbar clear cell meningioma. Case report. J Neurosurg. 1996;84:264–266. doi: 10.3171/jns.1996.84.2.0264. [DOI] [PubMed] [Google Scholar]
- 8.Jain D, Sharma MC, Sarkar C, Suri V, Garg A, Singh M, et al. Clear cell meningioma, an uncommon variant of meningioma : a clinicopathologic study of nine cases. J Neurooncol. 2007;81:315–321. doi: 10.1007/s11060-006-9237-7. [DOI] [PubMed] [Google Scholar]
- 9.Jallo GI, Kothbauer KF, Silvera VM, Epstein FJ. Intraspinal clear cell meningioma : diagnosis and management : report of two cases. Neurosurgery. 2001;48:218–221. doi: 10.1097/00006123-200101000-00042. discussion 221-212. [DOI] [PubMed] [Google Scholar]
- 10.Kleihues P, Burger PC, Scheithauer BW. The new WHO classification of brain tumours. Brain Pathol. 1993;3:255–268. doi: 10.1111/j.1750-3639.1993.tb00752.x. [DOI] [PubMed] [Google Scholar]
- 11.Kolluri VR, Reddy DR, Reddy PK, Naidu MR, Rao SB, Sumathi C. Meningiomas in childhood. Childs Nerv Syst. 1987;3:271–273. doi: 10.1007/BF00271821. [DOI] [PubMed] [Google Scholar]
- 12.Leibel SA, Wara WM, Sheline GE, Townsend JJ, Boldrey EB. The treatment of meningiomas in childhood. Cancer. 1976;37:2709–2712. doi: 10.1002/1097-0142(197606)37:6<2709::aid-cncr2820370621>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 13.Liu PI, Liu GC, Tsai KB, Lin CL, Hsu JS. Intraspinal clear-cell meningioma : case report and review of literature. Surg Neurol. 2005;63:285–288. doi: 10.1016/j.surneu.2004.03.013. discussion 288-289. [DOI] [PubMed] [Google Scholar]
- 14.Louis DN, Scheithauer BW, Budka H, von Deimling A, Kepes JJ. Meningiomas. In: Kleihues P, Cavenee WK, editors. Pathology and Genetics of Tumors of the Nervous System. Lyon: International Agency for Research on Cancer Press; 2000. pp. 176–184. [Google Scholar]
- 15.Matsui H, Kanamori M, Abe Y, Sakai T, Wakaki K. Multifocal clear cell meningioma in the spine : a case report. Neurosurg Rev. 1998;21:171–173. doi: 10.1007/BF02389326. [DOI] [PubMed] [Google Scholar]
- 16.Maxwell M, Shih SD, Galanopoulos T, Hedley-Whyte ET, Cosgrove GR. Familial meningioma : analysis of expression of neurofibromatosis 2 protein Merlin. Report of two cases. J Neurosurg. 1998;88:562–569. doi: 10.3171/jns.1998.88.3.0562. [DOI] [PubMed] [Google Scholar]
- 17.Oviedo A, Pang D, Zovickian J, Smith M. Clear cell meningioma : case report and review of the literature. Pediatr Dev Pathol. 2005;8:386–390. doi: 10.1007/s10024-005-0119-3. [DOI] [PubMed] [Google Scholar]
- 18.Park HC, Sohn MJ, Kim EY, Han HS, Park HS. Spinal clear cell meningioma presented with progressive paraparesis in infancy. Childs Nerv Syst. 2000;16:607–610. doi: 10.1007/PL00007302. [DOI] [PubMed] [Google Scholar]
- 19.Park SH, Hwang SK, Park YM. Intramedullary clear cell meningioma. Acta Neurochir (Wien) 2006;148:463–466. doi: 10.1007/s00701-005-0695-z. [DOI] [PubMed] [Google Scholar]
- 20.Payano M, Kondo Y, Kashima K, Daa T, Yatsuka T, Kida H, et al. Two cases of nondura-based clear cell meningioma of the cauda equina. APMIS. 2004;112:141–147. doi: 10.1111/j.1600-0463.2004.apm1120209.x. [DOI] [PubMed] [Google Scholar]
- 21.Pimentel J, Fernandes A, Pinto AE, Fonseca I, Moura Nunes JF, Lobo Antunes J. Clear cell meningioma variant and clinical aggressiveness. Clin Neuropathol. 1998;17:141–146. [PubMed] [Google Scholar]
- 22.Prinz M, Patt S, Mitrovics T, Cervos-Navarro J. Clear cell meningioma: report of a spinal case. Gen Diagn Pathol. 1996;141:261–267. [PubMed] [Google Scholar]
- 23.Scheithauer BW. Tumors of the meninges: proposed modifications of the World Health Organization classification. Acta Neuropathol. 1990;80:343–354. doi: 10.1007/BF00307686. [DOI] [PubMed] [Google Scholar]
- 24.Shiraishi K. Glycogen-rich meningioma. Case report and short review. Neurosurg Rev. 1991;14:61–64. doi: 10.1007/BF00338195. [DOI] [PubMed] [Google Scholar]
- 25.Zorludemir S, Scheithauer BW, Hirose T, Van Houten C, Miller G, Meyer FB. Clear cell meningioma. A clinicopathologic study of a potentially aggressive variant of meningioma. Am J Surg Pathol. 1995;19:493–505. [PubMed] [Google Scholar]