Abstract
We report a case of pedicle screw loosening treated by modified transpedicular screw augmentation technique using polymethylmethacrylate (PMMA), which used the anchoring effect of hardened PMMA. A 56-year-old man who had an L3/4/5 fusion operation 3 years ago complained of continuous low back pain after this operation. The computerized tomography showed a radiolucent halo around the pedicle screw at L5. We augmented the L5 pedicle screw with modified pedicle screw augmentation technique using PMMA and performed an L3/4/5 pedicle screw fixation without hook or operation field extension. This modified technique is a kind of transpedicular stiffness augmentation using PMMA for the dead space around the loosed screw. After filling the dead space with 1-2 cc of PMMA, we inserted a small screw. Once the PMMA hardened, we removed the small screw and inserted a thicker screw along the existing screw threading to improve the pedicle screws' pullout strength. At 10 months' follow-up, x-ray showed strong fusion of L3/4/5. The visual analogue scale (VAS) of his back pain was improved from 9 to 5. This modified transpedicular screw augmentation with PMMA using anchoring effect is a simple and effective surgical technique for pedicle screw loosening. However, clinical analyses of long-term follow-up and biomechanical studies are needed.
Keywords: Instrument failure, Osteoporosis, Pedicle screw loosening, PMMA, Pseudoarthrosis, Surgical technique
INTRODUCTION
Pedicle screw fixation is very useful surgical technique used in spinal fusions and fixations. However, according to reports, pedicle screw loosening is associated with a relatively high rate of complications. There is a distinct lack of surgical techniques that can overcome the pedicle screw loosening5). The pedicle screw offers no advantage once the screw has loosened, often resulting in the need to consider further surgery, such as the potentially adverse operations of extension and/or hook insertion17). Recently, the authors treated one patient of pseudoarthrosis due to pedicle screw loosening with a modified pedicle screw augmentation technique using polymethylmethacrylate (PMMA). In this report, we present the surgical technique in detail.
CASE REPORT
A 56-year-old man who had an L3/4/5 fusion operation at other hospital 3 years ago complained of continuous low back pain after this operation. He received non-surgical treatment, including pain intervention, for more than 6 consecutive months with no improvement. The result of bone mineral density (BMD) Tscore was -3.1. The computerized tomography (CT) of his spine showed a radiolucent halo around the pedicle screw at L5 (Fig. 1). We augmented the L5 pedicle screw with PMMA and performed an L3/4/5 pedicle screw fixation without hook or operation field extension. To achieve firm bone fusion, intertransverse on-lay bone graft with tri-calcium phosphate was done. The back pain of patient was decreased from visual analogue scale (VAS) 9 to5 after the operation. At 10 months' follow-up, x-ray showed strong intertransverse fusion (Fig. 1).
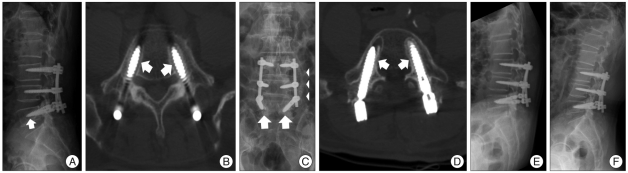
Fig. 1.
X-ray and computerized tomography (CT) of the case. A : Lateral lumbar X-ray shows a radiolucent halo around L5 pedicle screw (arrow). B : Pre-reoperative CT of the L5 pedicle showing the radiolucent halos around the screws (arrows). C : Post-reoperative anterior-posterior (AP) X-ray checked 10 months after reoperation shows the pedicle screw fixation of L3/4/5 with the intertransverse bone fusion (arrow head). Each peri-implant hollow is filled with PMMA and a new screw (arrows). D : Post-reoperative CT reveals the halos are filled with radiopaque bone cement (arrows) and new pedicle screws. E and F : flexion and extension lateral view of lumbar spine checked 10 months after reoperation showed strong fixation between instruments and vertebral bodys.
OPERATION TECHNIQUE
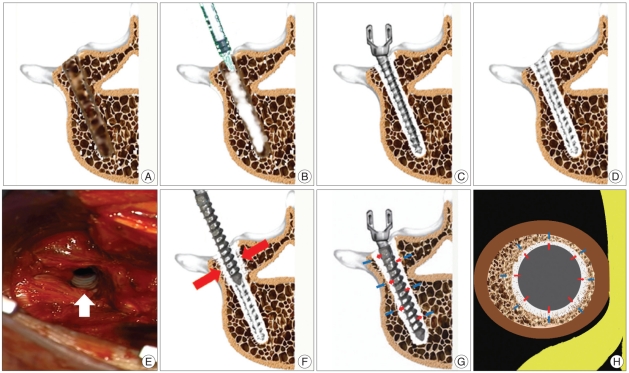
First of all, after removing the loose screw (Fig. 2A), we confirmed the empty hole's venous drain pattern using a water-soluble contrast. When the PMMA's viscosity became like toothpaste, we filled the dead space with about 1 cc of PMMA (Fig. 2B). Then, we packed PMMA in the hole, and inserted a small pilot screw, 5.5 mm in diameter (smaller than we usually use). Repeating this process 2-3 times filled the hole with PMMA, whereupon we left the small pilot screw in place (Fig. 2C). After the PMMA was hardened, the smaller pilot screw could be screwed out easily without PMMA adhesion. Then, we replaced the small pilot screw with a thicker permanent screw, usually one 6.5 mm in diameter, which we inserted into the existing internal thread (Fig. 2D-F). This process impacted the PMMA broken into the cancellous bone (anchoring effect) (Fig. 2G, H). The PMMA filled the preexisting pedicle gap, and hardened PMMA encircled the most part of the thicker permanent screw, 2011giving the pedicle screw pronounced expansile force. Thus, the PMMA anchor strengthened holding power throughout the thicker permanent screw.
Fig. 2.
Consecutive schematic illustrations of the modified transpedicular screw augmentation procedure and operation findings. A : The vacant pedicle hole after removal of the loose pedicle screw. B : The PMMA insertion process. When the PMMA's viscosity became like toothpaste, we filled the dead space with about 1 cc of PMMA. C : The inserted PMMA hardens with the small pilot screw inserted. D : The inner thread created by the small screw is presented after the small pilot screw was removed. E : Intra-operative photograph shows the inner thread (white arrow) after removing the small pilot screw. F : The cracks (red arrows), caused by inserting the thicker permanent screw, gives the screw greater holding power (anchor bolt effect). G and H : Illustrations of axial and coronal section after thicker permanent screw insertion. We suppose the thicker permanent screw has greater expansile forces (red arrows) and holding powers (blue arrows) throughout its whole surface.
DISCUSSION
Pedicle screw fixation (PSF) is an essential technique for spinal operations. From degenerative spinal diseases to deformity surgery, PSF's usefulness is wide-ranging, because it gives immediate, strong fixation after surgery2,11). PSF often causes complications. Reportedly, 17% of revision surgeries are associated with pedicle screw failure5).
Pedicle screw loosening is one of these complications, radiologically; it presents the characteristic findings of radiolucent zones around the screw. Such loosened screws are associated with decreased pullout strength and extraction torque15). A loosened pedicle screw can be regarded as a kind of instrument failure and is associated with pseudoarthrosis and back pain19).
In literatures, pedicle screw loosening has been recorded as being caused mainly by cyclic caudocephalad toggling at the bone-screw interface9,12,21). Although there is contrary opinion, BMD is assumed that related with the pedicle insertion torque and screw loosening12).
Therefore, to prevent pedicle screw loosening, we recommend meticulous screw insertion technique to prohibit toggling effect which could be occurring during screw insertion. Adding this, preoperative augmentation plan for the osteoporotic spine should be prepared. We believe that to avoid the possible cause is the best way to prevent pedicle screw loosening.
Surgeons can add a laminar hook or sub-laminar wiring to a pedicle screw insertion to prevent or treat these complications. Sometimes, recovering the situation from the instrument failure requires executing an extension of the operational level17). If strong insertion torques reduces the amount of screw loosening, a surgical technique that could create increased insertion torque in a loosened pedicle screw would rescue such screw loosening12,13).
The clinical analyses and biomechanic study about this modified transpedicular screw augmentation technique is underway. Mechanically, this modified transpedicular screw augmentation is different from conventional transpedicular screw augmentation3). This technique uses the anchoring effect of harden PMMA, which reinforces the screw insertion torque by playing just like relatively-healthy cancellous bone containing high BMD. The PMMA fills the preexisting pedicle hole, and the hardened PMMA encircles the thicker screw, which adds expansile force throughout the pedicle screw. Osteoporotic cancellous bone of pedicle can be strengthened by inserting a bigger screw into the internal thread of the PMMA anchor bolt, which surrounds the inserted screw from insertion point to screw tip. The thicker screw impacts this PMMA into the cancellous bone. Solid pedicle cortical bone and PMMA make more holding power and increasing the screw's pullout strength. A limitation of this technique is that it is indicated only for intact pedicles, because PMMA can possibly leak through a broken pedicle (Fig. 2).
There are some similarities between this transpedicular screw augmentation technique and Sugimoto's surgical technique, which uses a novel, metallic screw and bolt, with PMMA, to strengthen the pedicle screw16). However, this new transpedicular screw augmentation technique seems to be more simple and cost-effective. Furthermore, this surgical technique could be indicated not only for pedicle screws, but also for rescue screws subsequent to loosening in all similar screws, such as cervical plate screws, iliac screws, and occipito-cervical fixation screws.
Although it is not indicated for pedicle screw loosening, intra-operative vertebroplasty (VP) is another technique that, used with pedicle screw fixation, can increase pedicle screw strength and prevent pedicle screw loosening through strong fixation. PMMA VP, combined with a variable screw can achieve increased screw pullout strength1,3,4,7,8,10,14,16,18,20). This kind of pedicle screw can be used in deformity correction8). For intra-operative VP, calcium phosphate (CP) can replace the PMMA. However, CP tends to be absorbed more quickly than PMMA. Furthermore, the insertion torque of CP pedicle screw results in a weaker screw than with PMMA14). However, such a process has some weak points; chemical toxicities, thermal injury, and PMMA leakage can all occur. Although one report found no association between the amount of inserted PMMA and PMMA leakage, PMMA leakage followed intra-operative VP in 26.2% of cases. In addition, 39% of cases experienced asymptomatic anterior cement leakage4,5). In its severe form, PMMA can cause pulmonary embolism during the operation1,6). Unfortunately, larger amounts of PMMA are required for strong insertion torques7). Additionally, there is always the possibility of infection and/or bone necrosis.
Finally, there is a report comparing the pull-out strength between conventional transpedicular augmentation and kyphoplasty augmentation3). Both surgical technique improved screw fixation strength. Regardless the result of comparison, adequate surgical indication is essential for the technique, and we thought that for the pedicle screw loosening, this modified transpedicular screw augmentation would be better.
CONCLUSION
This modified transpedicular screw augmentation with PMMA using anchoring effect is a simple and effective surgical technique for pedicle screw loosening. However, clinical analyses of long-term follow-up and biomechanical studies are needed.
References
- 1.Aydogan M, Ozturk C, Karatoprak O, Tezer M, Aksu N, Hamzaoglu A. The pedicle screw fixation with vertebroplasty augmentation in the surgical treatment of the severe osteoporotic spines. J Spinal Disord Tech. 2009;22:444–447. doi: 10.1097/BSD.0b013e31818e0945. [DOI] [PubMed] [Google Scholar]
- 2.Bullmann V, Liljenqvist UR, Schmidt C, Schulte TL. [posterior operative correction of idiopathic scoliosis. Value of pedicle screws versus hooks] Orthopade. 2009;38:198–200. 202–204. doi: 10.1007/s00132-008-1370-x. [DOI] [PubMed] [Google Scholar]
- 3.Burval DJ, McLain RF, Milks R, Inceoglu S. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae : biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976) 2007;32:1077–1083. doi: 10.1097/01.brs.0000261566.38422.40. [DOI] [PubMed] [Google Scholar]
- 4.Chang MC, Liu CL, Chen TH. Polymethylmethacrylate augmentation of pedicle screw for osteoporotic spinal surgery : a novel technique. Spine (Phila Pa 1976) 2008;33:E317–E324. doi: 10.1097/BRS.0b013e31816f6c73. [DOI] [PubMed] [Google Scholar]
- 5.Frankel BM, Jones T, Wang C. Segmental polymethylmethacrylate-augmented pedicle screw fixation in patients with bone softening caused by osteoporosis and metastatic tumor involvement : a clinical evaluation. Neurosurgery. 2007;61:531–537. doi: 10.1227/01.NEU.0000290899.15567.68. discussion 537-538. [DOI] [PubMed] [Google Scholar]
- 6.Jang JS, Lee SH, Jung SK. Pulmonary embolism of polymethylmethacrylate after percutaneous vertebroplasty : a report of three cases. Spine (Phila Pa 1976) 2002;27:E416–E418. doi: 10.1097/00007632-200210010-00021. [DOI] [PubMed] [Google Scholar]
- 7.Jang JS, Lee SH, Kim KT, Kim BS, Lee WB. A biomechanical study on the pull-out strength of pedicle screw augmented with polymethylmethacrylate (PMMA) - Cadaveric study - J Korean Neurosurg Soc. 2002;31:45–49. [Google Scholar]
- 8.Lattig F. Bone cement augmentation in the prevention of adjacent segment failure after multilevel adult deformity fusion. J Spinal Disord Tech. 2009;22:439–443. doi: 10.1097/BSD.0b013e31818d6493. [DOI] [PubMed] [Google Scholar]
- 9.Law M, Tencer AF, Anderson PA. Caudo-cephalad loading of pedicle screws : mechanisms of loosening and methods of augmentation. Spine (Phila Pa 1976) 1993;18:2438–2443. doi: 10.1097/00007632-199312000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Moon BJ, Cho BY, Choi EY, Zhang HY. Polymethylmethacrylate-augmented screw fixation for stabilization of the osteoporotic spine : a three-year follow-up of 37 patients. J Korean Neurosurg Soc. 2009;46:305–311. doi: 10.3340/jkns.2009.46.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore DC, Maitra RS, Farjo LA, Graziano GP, Goldstein SA. Restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine (Phila Pa 1976) 1997;22:1696–1705. doi: 10.1097/00007632-199708010-00003. [DOI] [PubMed] [Google Scholar]
- 12.Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine (Phila Pa 1976) 2000;25:858–864. doi: 10.1097/00007632-200004010-00015. [DOI] [PubMed] [Google Scholar]
- 13.Ozawa T, Takahashi K, Yamagata M, Ohtori S, Aoki Y, Saito T, et al. Insertional torque of the lumbar pedicle screw during surgery. J Orthop Sci. 2005;10:133–136. doi: 10.1007/s00776-004-0883-3. [DOI] [PubMed] [Google Scholar]
- 14.Renner SM, Lim TH, Kim WJ, Katolik L, An HS, Andersson GB. Augmentation of pedicle screw fixation strength using an injectable calcium phosphate cement as a function of injection timing and method. Spine (Phila Pa 1976) 2004;29:E212–E216. doi: 10.1097/00007632-200406010-00020. [DOI] [PubMed] [Google Scholar]
- 15.Sandén B, Olerud C, Petrén-Mallmin M, Johansson C, Larsson S. The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. J Bone Joint Surg Br. 2004;86:457–461. doi: 10.1302/0301-620x.86b3.14323. [DOI] [PubMed] [Google Scholar]
- 16.Sugimoto Y, Tanaka M, Konishi H, Takigawa T, Nakanishi K, Misawa H, et al. Posterior spinal fusion using a pedicle nail system with polymethylmethacrylate in a paraplegic patient after vertebral collapse caused by osteoporosis. Spine J. 2009;9:e5–e8. doi: 10.1016/j.spinee.2007.10.036. [DOI] [PubMed] [Google Scholar]
- 17.Sun E, Alkalay R, Vader D, Snyder BD. Preventing distal pullout of posterior spine instrumentation in thoracic hyperkyphosis : a biomechanical analysis. J Spinal Disord Tech. 2009;22:270–277. doi: 10.1097/BSD.0b013e31816a6887. [DOI] [PubMed] [Google Scholar]
- 18.Takigawa T, Tanaka M, Konishi H, Ikuma H, Misawa H, Sugimoto Y, et al. Comparative biomechanical analysis of an improved novel pedicle screw with sheath and bone cement. J Spinal Disord Tech. 2007;20:462–467. doi: 10.1097/bsd.0b013e318030d2d6. [DOI] [PubMed] [Google Scholar]
- 19.Wetzel FT, Brustein M, Phillips FM, Trott S. Hardware failure in an unconstrained lumbar pedicle screw system. A 2-year follow-up study. Spine (Phila Pa 1976) 1999;24:1138–1143. doi: 10.1097/00007632-199906010-00014. [DOI] [PubMed] [Google Scholar]
- 20.Yazu M, Kin A, Kosaka R, Kinoshita M, Abe M. Efficacy of novel-concept pedicle screw fixation augmented with calcium phosphate cement in the osteoporotic spine. J Orthop Sci. 2005;10:56–61. doi: 10.1007/s00776-004-0862-8. [DOI] [PubMed] [Google Scholar]
- 21.Zindrick MR, Wiltse LL, Widell EH, Thomas JC, Holland WR, Field BT, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986:99–112. [PubMed] [Google Scholar]