Abstract
Background
Impairment-based exercise programs have yielded only small to moderate benefits in reducing pain and improving function in people with knee osteoarthritis (OA). It has previously been proposed that adding agility and perturbation training to exercise programs for people with knee OA may improve treatment effects for pain and function.
Objective
The purpose of this study was to examine the effectiveness of adding agility and perturbation techniques to standard exercise therapy compared with the standard exercise program alone for people with knee OA.
Design
This was a single-blinded randomized controlled trial.
Setting
The study was conducted in the outpatient physical therapy clinic of a large, university-based health center.
Participants
One hundred eighty-three people with knee OA (122 women, 61 men) participated.
Interventions
Participants were randomly assigned to either a group that received agility and perturbation training with standard exercise therapy or a group that received only the standard exercise program.
Measurements
The outcome measures were self-reported knee pain and function, self-reported knee instability, a performance-based measure of function, and global rating of change.
Results
Although both groups exhibited improvement in self-reported function and in the global rating of change at the 2-, 6-, and 12-month follow-up periods, there were no differences between groups on these outcomes. There was no reduction in knee pain or improvement in performance-based function in either group.
Limitations
It is possible that more-intense application of the interventions or application of the interventions to participants with knee OA who were at greater risk for falling may have yielded additive effects of the agility and perturbation training approach.
Conclusions
Both intervention groups exhibited improvement in self-reported function and the global rating of change. Our results, however, did not support an additive effect of agility and perturbation training with standard exercise therapy in our sample of individuals with knee OA. Further study is needed to determine whether there are subgroups of individuals who might achieve an added benefit with this approach.
Exercise therapy is well established as an important part of clinical management for people with knee osteoarthritis (OA).1–4 Although exercise therapy has been shown to be helpful, recent systematic reviews indicate that the effects of exercise on pain and function are moderate for people with knee OA.5,6 Based on these findings, it appears that there is room for improvement in designing OA exercise therapy programs.
Exercise therapy programs for knee OA traditionally have been impairment-based in design, focusing on impairments associated with knee OA such as lower-extremity joint motion deficits, muscle weakness, and reduced aerobic capacity.1–4 Although these programs may be effective in improving these impairments, they do not provide the individual with exposure to other challenges of motor function (eg, quick stops, turns, and changes in direction; challenges to balance; negotiating obstacles) that may be encountered during daily functional activities. Overall physical function might be further improved if individuals with knee OA were better prepared to deal with these challenges to motor function. This improvement in overall physical function might be accomplished if individuals were exposed to such challenges in motor function in conjunction with traditional impairment-based exercise therapy programs.
It also is well recognized that some people with knee OA may complain of knee instability.7–9 Patients usually describe this knee instability as “giving way” or “buckling” of the knee during activities of daily living. The prevalence of self-reported instability among people with knee OA has ranged from 11% to 44% and has been shown to be correlated with reduced functional ability.7–9 There is evidence that complaints of knee instability contribute to reduced function in people with knee OA above and beyond what is explained by impairments such as knee pain, quadriceps muscle weakness, and limited joint motion.7 This evidence may indicate that in order to enhance functional gains with exercise therapy, exercise programs should include activities that will address problems with knee instability.
Therapeutic exercise approaches have been shown to reduce complaints of knee instability in some people with anterior cruciate ligament (ACL) injury.10 These approaches included the use of lower-extremity strengthening as well as agility and perturbation training techniques. Agility training techniques involve quick stops and starts, cutting and turning, and changes in direction. Perturbation training incorporates the use of rollerboards and wobble boards to challenge balance and knee stability. The idea is that exposing individuals to activities that challenge the knee to potentially destabilizing loads during therapy may help them learn to deal with these loads when encountered in regular daily activity. Adding these types of training techniques to standard rehabilitation programs was found to be more effective in reducing dynamic knee instability (or improving dynamic stability) upon return to high-level physical activity than an impairment-based standard program in people with ACL-deficient knees.10
Given the limited effects with impairment-based exercise programs on improving physical function in knee OA, coupled with the fact that a significant proportion of people with knee OA have complaints of knee instability, we reasoned that a similar approach that was found to be effective for people with ACL-deficient knees might be modified to be beneficial for people with knee OA. In addition, even for those individuals with knee OA who did not have complaints of knee instability, agility and perturbation training techniques provide exposure to other challenges of motor function (eg, quick stops, turns, and changes in direction; challenges to balance; negotiating obstacles) that may be encountered during daily functional activities. Therefore, these techniques may be beneficial to people with knee OA by enhancing functional ability, even if they do not complain of knee instability.
Recently, we developed a supplemental approach to exercise therapy that included the use of agility and perturbation techniques in conjunction with a standard impairment-based exercise therapy program for people with knee OA.11 The program consisted of many of the same activities that were used, with modifications, in people with ACL-deficient knees. The modifications included performing agility techniques using walking-based rather than running-based activities and beginning in double-limb support rather than single-limb support for the perturbation techniques. The agility exercises focused on exposing the individual to quick stops and starts, quick turns and changes in direction, and negotiating obstacles encountered in the environment. The perturbation training involved the use of rollerboards and tiltboards to expose the individual to challenges in balance. We reported on successful implementation of this program in a case report.11 The patient in the case report had knee pain and complaints of knee instability secondary to her knee OA and had to stop playing golf and tennis. She also had difficulty climbing stairs without her knee feeling unstable. Following 12 sessions of the program, she had reduced her knee pain by 60% (pretraining score=5/10 and posttraining score=2/10 on 0–10 numeric knee pain scale), improved her Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) total score by 22% (pretraining score=27, posttraining score=21) and her WOMAC physical function score by 24% (pretraining score=17, posttraining score=13), and no longer had complaints of knee instability. She was able to return to golf and tennis. The success of this case prompted us to conduct the current study to determine whether there is an additive effect on improving function and self-reported knee stability and reducing pain by adding agility and perturbation training techniques to a therapeutic exercise program for people with knee OA.
The purpose of the current study was to formally test the effectiveness of adding agility and perturbation training to an exercise therapy program in comparison with the same exercise therapy program without agility and perturbation training for people with knee OA in a randomized clinical trial. We hypothesized that participants who received agility and perturbation training techniques in conjunction with a standard exercise therapy program would have greater improvements in physical function compared with those who received only the standard exercise program. We also hypothesized that there would be a greater proportion of participants reporting improved knee stability in the group who received the agility and perturbation training. Because previous studies have shown that exercise can help reduce pain5,6 and that pain has a strong relationship with physical function in people with knee OA, we also examined the effect of the interventions on knee pain. We hypothesized that if the agility and perturbation training program were to have an additive effect in improving function, it is likely it would also have an additive effect in reducing knee pain.
Method
Design Overview
The study was a prospective, single-blinded (testers were blinded to treatment group; treating therapists were not blinded to group but did not participate in any testing procedures) randomized controlled trial. All participants gave written informed consent prior to enrollment in the study.
Setting and Participants
The study was conducted in the Outpatient Department of Physical Therapy at the University of Pittsburgh Medical Center, Center for Sports Medicine, Pittsburgh, Pennsylvania. Participant recruitment began in October 2004, and the final data collection procedure was performed in December 2008. Participants were volunteers who were recruited from the greater Pittsburgh metropolitan area through physician offices, community flyers, newspaper advertisements, and the University of Pittsburgh Arthritis Institute Registry. All participants provided written approval from their physician to participate in the study.
Individuals were included in the study if they met the 1986 American College of Rheumatology (ACR) clinical criteria for knee OA12 and had grade II or greater Kellgren and Lawrence radiographic changes in the tibiofemoral joint.13 The 1986 ACR criteria for diagnosis of knee OA include knee pain and at least 3 of the following: age 50 years or older, morning stiffness of less than 30 minutes' duration, crepitus with active motion of the knee (eg, when squatting while weight bearing), tenderness on palpation of the bony margins of the joint, bony enlargement, and no palpable warmth.12 Individuals with patellofemoral joint radiographic changes were included provided that they had tibiofemoral radiographic changes as well. To ensure that study participants could safely participate in the training programs, individuals were excluded if they required use of an assistive device for ambulation, reported a history of 2 or more falls within the previous year, were unable to ambulate a distance of 30.5 m without an assistive device or need of a rest period, or reported severe visual problems. In addition, individuals were excluded if they had undergone total knee arthroplasty, exhibited uncontrolled hypertension, had a history of cardiovascular disease, or had neurological disorders that affected lower-extremity function.
Randomization and Interventions
To ensure a balanced assignment of participants to the 2 intervention groups, block randomization was used. To eliminate any potential biases that could occur from an investigator determining the next intervention assignment in the block sequence, the intervention assignments occurred in random block sizes of 2 and 4. In addition, randomization was stratified by the presence of unilateral versus bilateral knee OA. A set of sequentially numbered, sealed envelopes containing participant intervention assignment were created by the study statistician. Following baseline testing, the trial coordinator assigned an individual to a group based on the instructions in the next sealed envelope in sequence. The trial coordinator did not take part in any of the follow-up testing or intervention procedures.
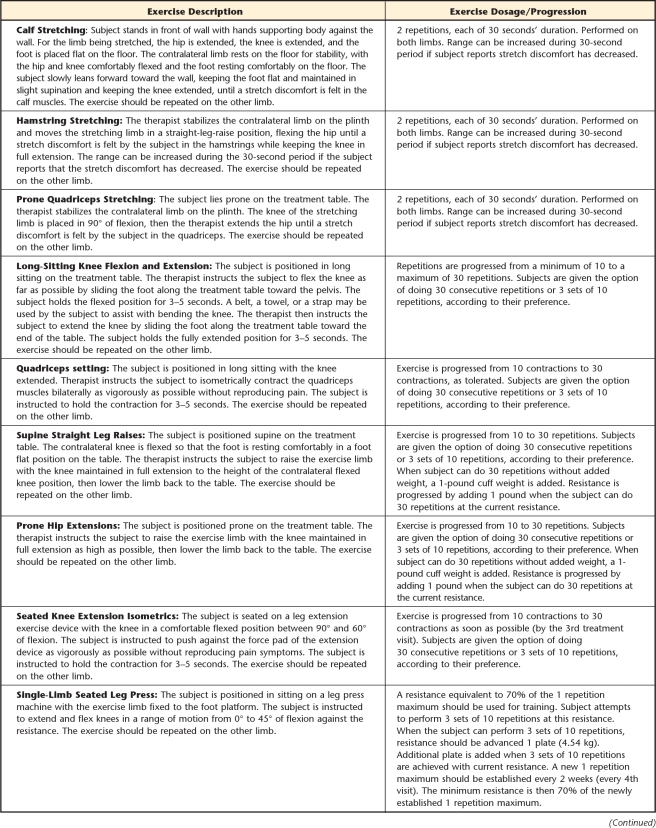
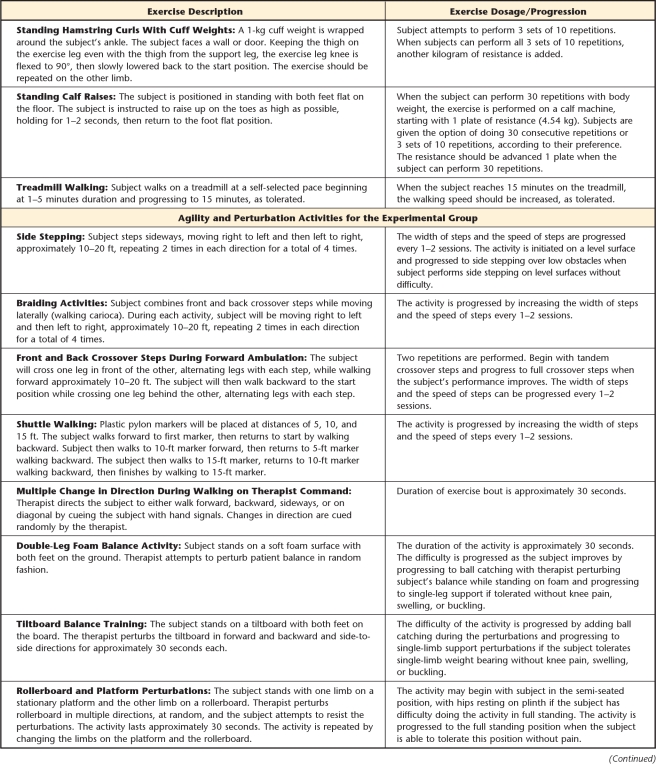
Participants were randomly assigned to 1 of 2 exercise intervention groups. Those assigned to the standard exercise group received an exercise program that included lower-extremity muscle stretching (quadriceps femoris, hamstring, and calf muscle stretching) and strengthening (quad sets, supine straight leg raises, prone hip extensions, seated isometric knee extensions, single-leg leg presses, standing hamstring curls, and standing heel raises), long-sitting knee flexion and extension range of motion, and treadmill walking. All lower-extremity exercises were performed bilaterally. This program was consistent with current published treatment recommendations for exercise programs for knee OA.1,2,4
Participants assigned to the agility and perturbation group received the same standard exercise program as the standard exercise group with the addition of agility and perturbation training techniques. The agility training techniques included side stepping, braiding (lateral stepping combined with forward and backward crossover steps), front crossover steps during forward ambulation, back crossover steps during backward ambulation, shuttle walking (forward and backward walking to and from designated markers), and a drill requiring multiple changes in direction in which the therapist provided hand signals at random to prompt the individual to change direction (forward and backward, right and left lateral steps, diagonally backward and forward) during walking. The perturbation techniques incorporated the use of foam surfaces, tiltboards, and rollerboards to expose the individual's lower limbs and body to potentially destabilizing forces. The participants attempted to maintain balance and control over the exercised lower extremity during the perturbations. Details of both of these exercise programs are provided in the Appendix.
To ensure standardization of the intervention implementation, all therapists were given one-on-one instruction in the intervention procedures by the principal investigator (G.K.F.). The therapists were provided with a booklet that included descriptions and pictures of the exercises and instructions in the progression of the exercises. The trial coordinator conducted periodic, random reviews of the participants' treatment records to ensure that they were receiving their assigned protocols and progressing programs per the protocol. The principal investigator performed a face-to-face review of the intervention programs with the therapists every 6 months.
To account for any potential effect that differences in contact time in therapy between groups may have had on treatment outcome, participants in the standard exercise group performed an arm-bike exercise activity of the upper extremities for 10 to 15 minutes. This amount of time approximated the time it took for participants in the agility and perturbation group to complete the agility and perturbation training activities. Participants were to complete 12 supervised sessions of their respective program in a 6- to 8-week period, depending upon their scheduling constraints.
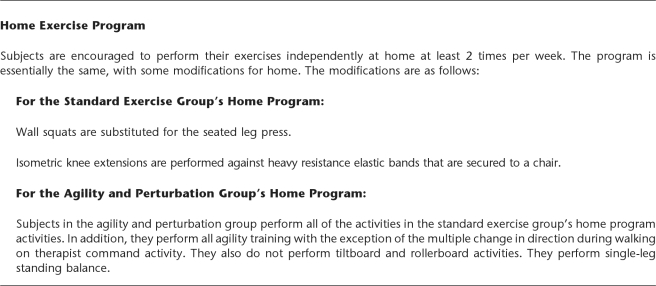
During the supervised exercise sessions, therapists began instructing participants in the home exercise activities so that they would be independent in this program by the end of the supervised therapy period of the study. The content of the home exercise program for the standard exercise group was similar to that of the program they received during the supervised sessions, with some modifications. Because they would not have a leg press machine in their homes, wall squat exercises were substituted for the leg press exercise. Although a 1-repetition maximum resistance used in the leg press exercise could not be directly translated to the wall squat, most participants had been lifting about half of their body weight during the leg press exercise, so we were confident that the wall squats were providing resistance similar to that of the leg press. Participants were provided with cuff weights to perform the straight leg raises, hip extensions, and hamstring curls at home. For the isometric knee extensions, they were provided with heavy-resistance Thera-Band* (Gold color) and instructed how to attach it to a chair in order to perform an isometric knee extension exercise.
Participants in the agility and perturbation group performed all of the same standard home program exercises as those in the standard exercise group. In addition, they performed all agility exercises with the exception of the activity involving multiple changes in direction during walking on therapist command. They also did not perform tiltboard and rollerboard activities because we could not provide them with this equipment for home use and there would be safety concerns in performing these activities without supervision. As an alternative, they were instructed to perform a single-leg standing balance exercise on level surfaces and carpeting. Participants in both groups also were encouraged to continue a walking program of at least 30 minutes per day at least 3 days a week for the home program. They were encouraged to perform all prescribed home exercises at least 2 times per week. We monitored their home program participation through the 6-month follow-up period. After this period, participants were encouraged to continue the program, but further monitoring was not performed.
A number of steps were taken to encourage adherence to the home exercise program. Participants were provided with a binder containing descriptions and pictures of their home exercises. Exercise diary checklists were provided to the participants so that they could record the amount of exercise they performed each week. These diaries were to be returned at each follow-up visit through the 6-month follow-up visit. Participants were provided a small monetary reward for returning their exercise diaries at the follow-up visit. In order to prevent any bias from participants forging their diaries to receive the reward, we instructed them that they would be paid for returning the diary regardless of whether the form was complete and that we only wanted to monitor how much they actually did their exercise program. There would be no penalty for incomplete forms. Participants also came in to the clinic for a face-to-face visit with the study coordinator for a review of the home exercise program 4 months post-randomization. This visit was to ensure that participants were performing their prescribed exercise program properly and to assist them in troubleshooting any problems with the home program. No outcomes were tested at this 4-month visit. Finally, the trial coordinator conducted monthly telephone contacts to remind participants to perform their exercises and complete their exercise diaries and to assist in troubleshooting any difficulties with the home program. This multistep approach has been shown to improve adherence to exercise programs14 and was implemented through the 6-month follow-up period.
Outcome Measures
Testing was performed at baseline and at 2, 6, and 12 months following randomization. Self-report measurements were taken at all time points. The physical performance measurements were taken at baseline and at the 2- and 6-month time points. Testers were blinded from knowledge of participants' group assignments. The participants were not informed of the specific group to which they were assigned. They only knew that they were randomly assigned to 1 of 2 exercise approaches. Although the treating therapists could not be blinded from the participants' group assignments, they were not involved in any of the study testing procedures and remained blinded from test results.
Primary outcome measure.
The WOMAC total score was the primary outcome measure for the study. The WOMAC is a disease-specific measure of pain, stiffness, and physical function for individuals with knee OA. The WOMAC comprises 5 items related to pain, 2 items related to stiffness, and 17 items related to physical function. Each item is scored on a 5-point Likert scale. The 0 to 4 Likert version (version 3.1) of the WOMAC was used in this study. The reliability and validity of WOMAC scores have been established.15–17 We also analyzed the WOMAC physical function subscale scores separately from the total scores to ensure that the pain and stiffness components in the WOMAC total score did not mask the potential effects on physical function.
Secondary outcome measures.
Secondary outcome measures were: self-reported knee instability, self-reported knee pain, global rating of change (GRC) score, and Get Up and Go Test (GUAG) score.
Participants rated the severity of knee instability on a 0 to 5 numeric scale in response to the query: “To what degree does giving way, buckling, or shifting of the knee affect your level of daily activity?” The ratings were as follows: 5=“I do not have the symptom”; 4=“I have the symptom, but it does not affect daily activity”; 3=“the symptom affects my activity slightly”; 2=“the symptom affects my activity moderately”; 1=“the symptom affects my activity severely”; and 0=“the symptom prevents me from all daily activities.” This self-report rating of knee instability was taken from the Knee Outcome Survey—Activities of Daily Living Scale.18 The test-retest reliability of this self-report rating of knee instability on 50 individuals with a variety of knee pathologies, including knee OA, was estimated using an intraclass correlation coefficient (ICC [2,1]=.72). Because few participants rated their instability as 0 or 1, we collapsed the ratings into a dichotomous variable. Participants were classified as “unstable” if their knee instability rating was severe enough to affect their activity (ie, ≤3). They were classified as “stable” if the knee instability rating did not affect their activity (ie, ≥4).
Participants rated the worst knee pain they experienced in the 24 hours prior to testing using an 11-point numeric pain rating scale, with 0 representing “no pain” and 10 representing “the worst pain imaginable.” Numeric rating scales have been found to be reliable and valid for measuring clinical pain.19,20
A GRC score was obtained from each participant at the 2-, 6-, and 12-month time points. The GRC is a 15-item scale in which individuals rate the degree to which their knee condition has changed from the time treatment was initiated to the present.21 For example, a rating of 1 corresponds to the phrase “a very great deal better,” 8 corresponds to the phrase “about the same,” and 15 corresponds to the phrase “a very great deal worse.”
The GUAG was used as a performance-based measure of function. To perform this test, participants were seated on a standard-height chair with armrests. On the command “go,” they stood up and walked as fast as possible along a level, unobstructed distance of 15.2 m. A stopwatch was used to measure the length of time it took to complete the task. We have demonstrated intrarater (ICC=.95) and interrater (ICC=.98) test-retest reliability in our laboratory for the GUAG.22 The minimum detectable change was 1.2 seconds.22
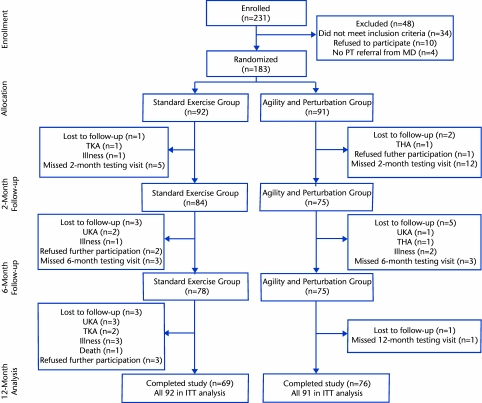
Assessment of Potential Covariates
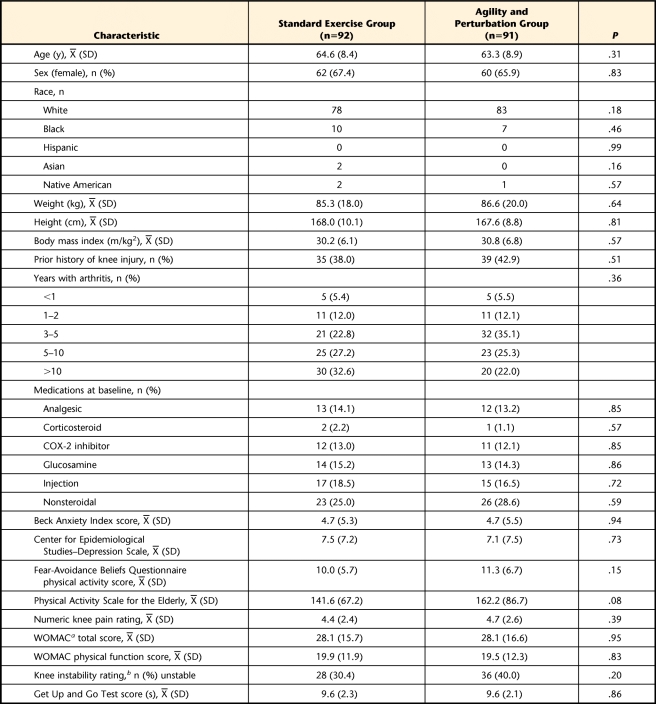
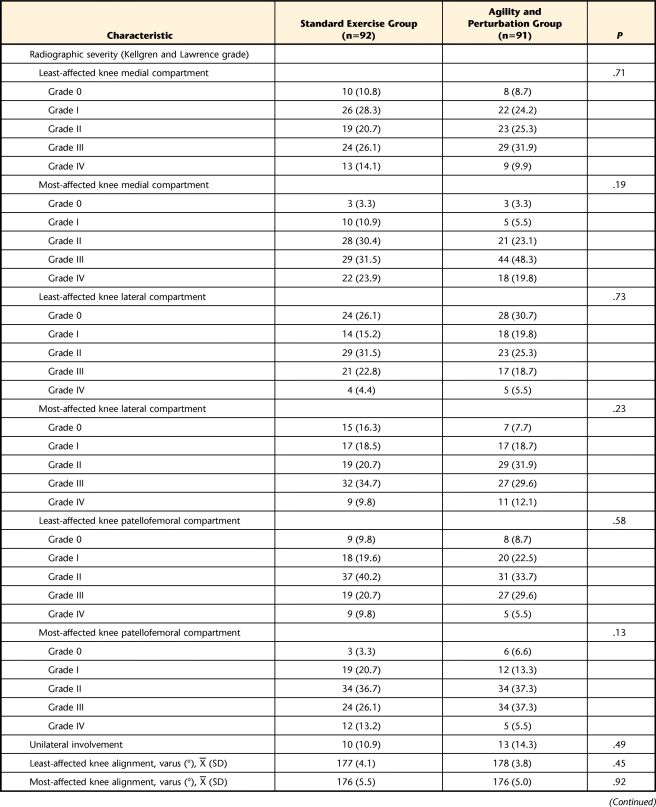
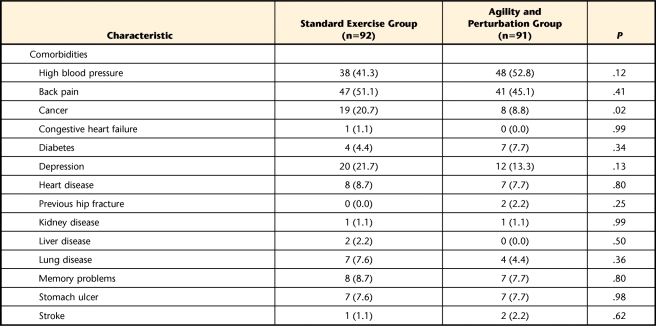
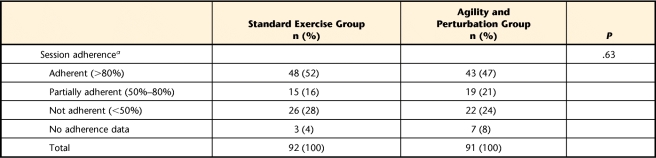
In order to account for any potential covariates that might need to be controlled in the final analysis, we compared potential differences between groups on a number of variables that could influence treatment outcome. These variables included age, sex, race, height, weight, body mass index, years with a diagnosis of knee OA, medications, anxiety (measured using the Beck Anxiety Index23), depression (measured using the Center for Epidemiological Studies—Depression Scale24), fear of physical activity (measured using the Fear-Avoidance Beliefs Questionnaire physical activity subscale, modified for the knee25,26), and physical activity (measured using the Physical Activity Scale for the Elderly27) (Tab. 1). In addition, radiographic severity of knee OA (using the standing fixed knee flexion view for the tibiofemoral joint and Merchant view for the patellofemoral joint),13 knee alignment (using the long cassette radiographic view), comorbidities, serious adverse events, number of dropouts, and adherence to the home exercise program were assessed (Tabs. 2 and 3, Fig.1).
Table 1.
Baseline Characteristics by Treatment Group
a WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index.
b ≤3=unstable, ≥4=stable.
Table 2.
Baseline Characteristics by Treatment Group: Radiographic Severity and Comorbiditiesa
Values represent number of participants (%), unless otherwise indicated.
Table 3.
Home Exercise Adherence by Group
a Based on the percentage of expected home exercise sessions to complete during the follow-up period. The expectation was 2 sessions per week over a 16-week follow-up period, totaling 32 sessions.
Figure 1.
CONSORT diagram of study enrollment and participation. PT=physical therapy, TKA=total knee arthroplasty, THA=total hip arthroplasty, UKA=unicompartmental knee arthroplasty, ITT=intention to treat.
Sample Size
To estimate the sample size required for the study, based on preliminary observations in our clinic of people with knee OA undergoing exercise therapy and those who had received agility and perturbation training as part of the exercise program, we assumed an 8-point difference in the mean between groups with a common standard deviation of 18 points on the WOMAC, with a .05 level of significance and a 2-sided alternative hypothesis. This estimate translates into an effect size of approximately 0.44. This effect size would be considered a moderate treatment effect between groups, and we believed it would be reasonable if adding the additional agility and perturbation training to existing exercise therapy programs was to be worth the extra time and effort. Our analysis indicated a sample size of 168 participants (84 per group) would yield approximately 80% power to detect a difference of 8 in the mean WOMAC scores at the 1-year endpoint. We anticipated that approximately 30% of the participants might either fail initial screening or drop out; therefore, we needed to enroll 240 participants (120 per group) to account for this loss.
Data Analysis
Summary statistics are presented as means (±SD) for continuous variables and as percentages for discrete variables. Parametric and nonparametric analysis-of-variance methods and chi-square tests were used to compare the baseline clinical and demographic characteristics, treatment features, rates of side effects and serious adverse events (injuries or symptoms associated with the interventions or testing procedures that required referral to a physician for evaluation or intervention), and adherence to home exercise between treatment groups (Tabs. 1, 2, and 3).
All outcome analyses were conducted according to the intention-to-treat (ITT) principle. Regression models (linear for continuous measures and logistic for discrete measures) were used to determine whether there was an independent treatment effect on the outcome variables at the 12-month follow-up assessment, adjusting for those baseline characteristics that differed between treatment groups. At the 12-month assessment, data for participants with missing scores were imputed using the last observation carried forward approach. To determine whether this imputation approach affected study results, we conducted sensitivity analyses. The analyses were replicated using multiple imputation. Consistent findings indicated that the results were not affected by this approach to missing data. Generalized estimating equation longitudinal models were used to model the association of treatment on the outcomes over the course of the follow-up period. We adjusted the models for the incidence of cancer, as it was significantly different between groups at baseline. We also adjusted the models for the Physical Activity Scale for the Elderly score because although not statistically significant, the group mean differences appeared to approach significance. Furthermore, we adjusted for the most-affected knee medial compartment and patellofemoral compartment radiographic severity because, although not statistically significant, there did appear to be some difference between the groups on these variables and previous research indicated that radiographic severity might affect the outcome of exercise therapy.28 No adjustment for multiple tests was implemented for secondary endpoints, so the results should be interpreted accordingly.
Role of the Funding Source
This study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (grant 1-R01-AR048760). The views contained in this publication are those of the grantees and do not necessarily reflect those of the funding agency.
Results
Two hundred thirty-one participants were enrolled in the study. Forty-eight participants were not randomized to a treatment group, as they did not meet the study inclusion criteria during screening procedures (Fig. 1). Therefore, 183 participants were randomized to a treatment group. The characteristics of these participants, by group, are shown in Tables 1 and 2. There were no differences between groups for any demographic variables or potential covariates, with the exception of history of cancer in the list of comorbidities. The standard exercise group had significantly more participants with a history of cancer than the agility and perturbation group (Tab. 2). There were no adverse events resulting from participation in the study reported by participants in either group.
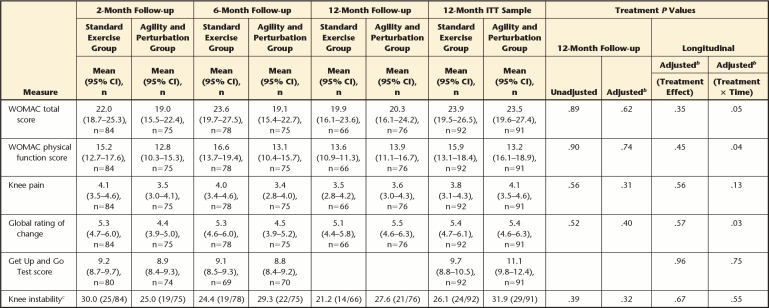
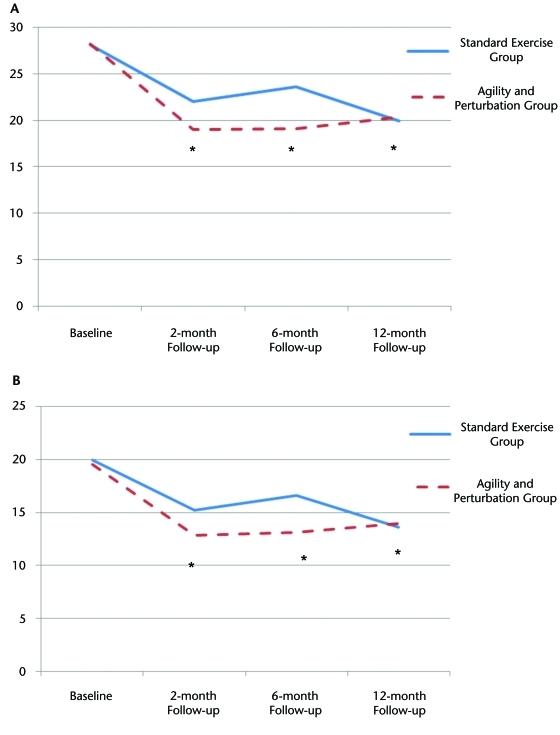
Table 4 provides the mean outcome scores for each group at each time point, the results of the ITT analysis, and the treatment × time interaction for each outcome variable. The longitudinal ITT analysis indicated that there were no differences between treatment groups for any of the outcome measures at the 1-year endpoint. The significant treatment × time interaction results shown in Table 4 indicate there was some improvement in both groups from baseline, with the agility and perturbation group exhibiting slightly more improvement than the standard exercise group in WOMAC total and physical function scores and GRC scores in the early follow-up period. However, these differences disappeared by the 1-year endpoint. We have provided a plot of the WOMAC total and physical function scores over the follow-up periods to illustrate this interaction (Fig. 2). There were no changes in knee pain or GUAG scores within the groups. There also was no significant change in the proportion of participants who had knee instability within the groups.
Table 4.
Outcome Measures by Treatment Group at Each Time Point With Intention-to-Treat (ITT) Analysisa
95% CI=95% confidence interval, WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index.
b Adjusted for incidence of cancer, Physical Activity Scale for the Elderly score, most-affected knee medial and patellofemoral compartments radiographic severity.
c Reported as percentage of participants with knee instability (≤3 on the knee instability rating scale).
Figure 2.
Plot of Western Ontario and McMaster Universities Osteoarthritis Index total (A) and physical function (B) scores at each time point. Asterisk indicates both groups' scores were significantly different from their respective baseline scores (P<.01).
Discussion
Our results indicate that although both groups exhibited some modest improvements in outcome measures, there were no significant differences between the intervention groups. Although we did find a significant interaction indicating that the agility and perturbation group improved slightly more than the standard exercise group at early time points, post hoc testing of the simple between-group effects were not significant. A 17% to 22% change in WOMAC scores from baseline has been reported to be clinically meaningful.29 By converting our change scores for each group to percentages of change in WOMAC scores, we found that changes for each group either were within or exceeded this range at most time points (2 months: standard exercise group=21%, agility and perturbation group=32%; 6 months: standard exercise group=16%, agility and perturbation group=32%; 12 months: standard exercise group=29%, agility and perturbation group=28%). Likewise, the percentage of change from baseline in WOMAC physical function scores was within or exceeded this range (2 months: standard exercise group=24%, agility and perturbation group=34%; 6 months: standard exercise group=17%, agility and perturbation group=33%; 12 months: standard exercise group=32%, agility and perturbation group=29%). Post hoc pair-wise comparisons on the per protocol data using a Bonferroni correction indicated that the within-group changes from baseline in the WOMAC total and physical function scores were significant (P<.01) for both groups (Fig. 2). The GRC scores also exhibited moderate improvements for each group (5=somewhat better to 4=moderately better) at all 3 follow-up time points. There were only slight improvements in knee pain (0.3 to 1.0) and in GUAG scores (0.3 to 0.5 seconds) in both groups, and we would not consider these changes to be clinically meaningful. Likewise, there were only slight within-group improvements in the proportion of participants reporting knee instability from baseline to the follow-up periods. The results do not support an additive effect of agility and perturbation training techniques to a standard exercise therapy program in our sample of participants with knee OA.
We are aware of only one other study that examined the effectiveness of a similar training program that included balance and agility exercises in people with knee OA. Diracoglu et al30 compared the effectiveness of “kinesthetic and balance training” plus strengthening exercises versus only strengthening exercise in 60 female participants. The participants received 24 sessions of their respective interventions over an 8-week period. Outcome was measured at the end of the 8-week period. Similar to our study, although both groups improved, there was no difference in WOMAC scores.30 Diracoglu et al did report that WOMAC physical function scores were statistically better in the kinesthesia group; however, the actual difference was on the order of 0.7 points, which, in our opinion, does not seem clinically meaningful. They also reported greater improvements in scores on the Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire (SF-36) physical function, role limitations (physical), and vitality (energy or fatigue) subscales. The kinesthesia group also had significantly faster times on the 10-Meter Walking Test (0.68 seconds faster) following treatment, but it is unclear whether this finding represents a clinically meaningful difference. Participants in Diracoglu and colleagues' study received twice as many treatment sessions as our participants received and in a shorter time frame. It may be possible that if we had administered a greater number of treatment sessions in a shorter period of time, we might have detected significant differences between our intervention groups.
Our initial sample size estimate indicated that we needed 168 participants (84 per group) to have sufficient statistical power, and as we had anticipated a 30% initial screening failure or dropout rate, we indicated we would enroll 240 participants. We did not meet the target enrollment, as we enrolled only 231 participants due to limitations in funding. At the 1-year endpoint, we had complete data on 143 participants. However, because we used an ITT analysis, we used a last score carried forward approach to handle missing data, so the analysis included data from 183 participants at the 1-year endpoint, which is well over the initial sample size estimate. We performed a sensitivity analysis using multiple imputation to verify our ITT approach. In addition, the relatively small difference in means between groups indicates that we probably did have sufficient power to conclude that the groups were not different on our outcome measures.
In developing the agility and perturbation training program, we had hypothesized that exposing participants to challenging movement problems, including challenges to knee stability, balance, quick changes in direction, quick stops and starts, and so on, would better prepare them for dealing with these types of movement problems during daily function. This logic may have been reasonable and appeared to have worked in younger, athletic individuals with ACL injuries.10 However, in older individuals with knee OA, the daily challenges to balance and requirements for agility may not be as intense or as frequent as those encountered by younger, athletic people. Therefore, adding agility and perturbation training techniques to exercise programs may not have as dramatic an effect on knee stability and general function in older individuals with knee OA as had previously been observed for younger, athletic individuals. It may be true that some of our participants engaged in higher-level activity where challenges to balance and agility may occur, but perhaps the majority of them did not.
Another potential limitation is that we had excluded participants who were already known to be at risk for falling and those who required assistive devices for ambulation. It is possible that these individuals might benefit more from the agility and perturbation training than from a standard exercise program. Further study is warranted to determine whether adding agility and perturbation training techniques for people with knee OA who are also at risk for falling may have an additive effect on improving function in those individuals.
Another potential problem is that our outcome measures may not have been sufficiently sensitive in capturing aspects of physical function that might be more influenced by agility and perturbation training. For example, the WOMAC does not include items that directly incorporate higher-level activities requiring balance and agility skills. In addition, we had only one performance-based measure of function. If other types of performance-based measures of function had been used, we might have found differences between our intervention groups. For example, in a recently completed feasibility study including participants with total knee arthroplasty, we found that single-limb stance time (a measure of balance) and self-selected gait speed improved in participants who received the same agility and perturbation training techniques compared with those who received a standard exercise program.31
The fact that there were only slight changes in knee pain from baseline in both groups most likely also played a role in dampening any beneficial effects of adding agility and perturbation training to exercise programs to improve physical function. A strong relationship between pain and function is well established in people with knee OA, and it would not be surprising that differences in physical function would not be observed if there were not significant differences in knee pain following treatment.
In both groups, we had responders and nonresponders to treatment. It may be that the addition of agility and perturbation training techniques are advantageous for some and not really helpful, or perhaps harmful, for others. In order to improve the precision of decision making, it would be helpful to determine whether there are patient characteristics that could be measured at baseline that would help determine who is likely to benefit from adding agility and perturbation training techniques to exercise programs and who is not likely to benefit. This effort was beyond the scope of our study, but we are currently examining our data to determine whether we can identify baseline predictors of treatment response for both of our intervention groups.
Conclusion
Although both intervention groups exhibited some moderate improvements in self-reported outcome measures, there was no additive benefit from including agility and perturbation training techniques in a standard exercise program for our participants with knee OA. The use of other outcome measures (eg, more variety of performance-based physical function measures, balance, proprioception) or application of the interventions to subgroups of people with knee OA who also have problems with balance may be needed to observe an additive effect. Future study also is needed to determine whether baseline clinical measures could be used to identify individuals who may benefit from adding agility and perturbation training techniques to exercise therapy programs for people with knee OA.
The Bottom Line
What do we already know about this topic?
Agility and perturbation training, when added to standard exercise programs, has helped improve the outcome for young athletes who sustained an anterior cruciate ligament injury. One case report suggests that this approach also might improve the effects of therapeutic exercise in a person with knee osteoarthritis.
What new information does this study offer?
This study tested whether adding agility and perturbation training to a standard exercise program could provide additional improvements in function and knee stability in patients with knee osteoarthritis. Although participants in both groups appeared to improve in self-reported physical function, there did not appear to be an additive effect of the agility and perturbation training program.
If you're a patient, what might these findings mean for you?
If you have knee osteoarthritis, adding agility and perturbation training techniques to your therapeutic exercise program may or may not increase the benefits of therapy. More work is needed to determine which patients may benefit from this approach.
Appendix.
Appendix.
Exercise Therapy Proceduresa
a Reprinted with permission and with modifications from: Scopaz KA, Piva SR, Gil AB, et al. Effect of baseline quadriceps activation on changes in quadriceps strength after exercise therapy in subjects with knee osteoarthritis. Arthritis Rheum. 2009;61:951–957.
Footnotes
Dr Fitzgerald, Dr Piva, Dr Wisniewski, Dr Oddis, and Dr Irrgang provided concept/idea/research design. Dr Fitzgerald, Dr Piva, Dr Wisniewski, and Dr Irrgang provided writing. Dr Gil and Dr Oddis provided data collection. Dr Gil and Dr Wisniewski provided data analysis. Dr Fitzgerald, Dr Piva, and Dr Gil provided project management. Dr Fitzgerald provided fund procurement. Dr Oddis provided participants. Dr Fitzgerald and Dr Irrgang provided institutional liaisons. Dr Piva and Dr Gil provided clerical support. Dr Gil, Dr Wisniewski, Dr Oddis, and Dr Irrgang provided consultation (including review of manuscript before submission).
This study was approved by the University of Pittsburgh Institutional Review Board.
This study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (grant 1-R01-AR048760).
Clinical trial registration number: NCT00078624.
The Hygenic Corp, 1245 Home Ave, Akron, OH 44310-2575.
References
- 1. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum. 2000;43:1905–1915 [DOI] [PubMed] [Google Scholar]
- 2. Jordan KM, Arden NK, Doherty M, et al. EULAR Recommendations 2003; an evidence-based approach to the management of knee osteoarthritis: report of a task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62:1145–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ottawa Panel Evidence-Based Clinical Practice Guidelines for Therapeutic Exercises and Manual Therapy in the Management of Osteoarthritis. Phys Ther. 2005;85:907–971 [PubMed] [Google Scholar]
- 4. Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16:137–162 [DOI] [PubMed] [Google Scholar]
- 5. Fransen M, McConnell S, Bell M. Exercise for osteoarthritis of the hip or knee. Cochrane Database Syst Rev. 2003;3:CD004286. [DOI] [PubMed] [Google Scholar]
- 6. Jamtvedt G, Dahm KT, Christie A, et al. Physical therapy interventions for patients with osteoarthritis of the knee: an overview of systematic reviews. Phys Ther. 2008;88:123–136 [DOI] [PubMed] [Google Scholar]
- 7. Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51:941–946 [DOI] [PubMed] [Google Scholar]
- 8. Felson DT, Niu J, McClennan C, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147:534–540 [DOI] [PubMed] [Google Scholar]
- 9. Schmitt LC, Fitzgerald GK, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Phys Ther. 2008;88:1506–1516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in non-operative anterior cruciate ligament rehabilitation programs for physically active individuals. Phys Ther. 2000;80:128–140 [PubMed] [Google Scholar]
- 11. Fitzgerald GK, Childs JD, Ridge TM, Irrgang JJ. Agility and perturbation training for a physically active individual with knee osteoarthritis. Phys Ther. 2002;82:372–382 [PubMed] [Google Scholar]
- 12. Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis; classification of osteoarthritis of the knee: Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–1049 [DOI] [PubMed] [Google Scholar]
- 13. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jette AM, Rooks D, Lachman M, et al. Home-based resistance training: predictors of participation and adherence. Gerontologist. 1998;38:412–421 [DOI] [PubMed] [Google Scholar]
- 15. Bellamy N, Watson-Buchanan WW, Goldsmith CH, Campbell J. Validation study of WOMAC: a health status instrument for measuring clincically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840 [PubMed] [Google Scholar]
- 16. Bellamy N, Kean WF, Buchanan WW, et al. Double blind randomized controlled trial of sodium meclofenamate (Meclomen) and diclofenac sodium (Voltaren): post validation reapplication of the WOMAC osteoarthritis index. J Rheumatol. 1992;19:153–159 [PubMed] [Google Scholar]
- 17. Hawker G, Melfi C, Paul J, et al. Comparison of a generic (SF-36) and disease-specific (WOMAC) (Western Ontario and McMaster Universities Osteoarthritis Index) instrument in the measurement of outcomes after knee replacement surgery. J Rheumatol. 1995;22:1193–1196 [PubMed] [Google Scholar]
- 18. Irrgang JJ, Snyder-Mackler L, Wainner RS, et al. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132–1145 [DOI] [PubMed] [Google Scholar]
- 19. Jensen MP, Miller L, Fisher LD. Assessment of pain during medical procedures: a comparison of three scales. Clin J Pain. 1998;14:343–349 [DOI] [PubMed] [Google Scholar]
- 20. Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999;79:231–252 [DOI] [PubMed] [Google Scholar]
- 21. Jaeschke R, Singer J, Guyatt GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–415 [DOI] [PubMed] [Google Scholar]
- 22. Piva SR, Fitzgerald GK, Irrgang JJ, et al. Get up and go test in patients with knee osteoarthritis. Arch Phys Med Rehabil. 2004;85:284–289 [DOI] [PubMed] [Google Scholar]
- 23. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psych. 1988;56:893–897 [DOI] [PubMed] [Google Scholar]
- 24. Radloff LS. The CES-D scale: a self-report depression scale for research in a general population. Appl Psychol Meas. 1977;1:385–401 [Google Scholar]
- 25. van Baar ME, Dekker J, Oostendorp RA, et al. The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee; a randomized clinical trial. J Rheumatol. 1998;25:2432–2439 [PubMed] [Google Scholar]
- 26. Scopaz KA, Piva SR, Wisnewski S, Fitzgerald GK. Relationships of fear, anxiety, and depression with physical function in patients with knee osteoarthritis. Arch Phys Med Rehabil. 2009;90:1866–1873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162 [DOI] [PubMed] [Google Scholar]
- 28. Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. J Rheumatol. 2001;28:156–164 [PubMed] [Google Scholar]
- 29. Angst F, Aeschlimann A, Michel BA, Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol. 2002;29:131–138 [PubMed] [Google Scholar]
- 30. Diracoglu D, Aydin R, Baskent A, Celik A. Effects of kinesthesia and balance exercises in knee osteoarthritis. J Clin Rheumatol. 2005;11:303–310 [DOI] [PubMed] [Google Scholar]
- 31. Piva SR, Gil AB, Almeida GJ, et al. A balance exercise program appears to improve function for patients with total knee arthroplasty: a randomized clinical trial. Phys Ther. 2010;90:880–894 [DOI] [PMC free article] [PubMed] [Google Scholar]