Abstract
Background
Although fear-avoidance beliefs (FABs) have been explored in younger adults and Spanish older adults, their relationships to measures of low back pain (LBP)–related disability, overall physical health, and falling have not been investigated in older American adults.
Objective
The purpose of this study was to examine the association of FABs with self-reported disability, physical health, and falling among community-dwelling older adults with LBP in the United States.
Design
This was a cross-sectional study.
Methods
Ninety-three community-dwelling men and women with current LBP were included in this analysis. Participants completed the Fear-Avoidance Beliefs Questionnaire physical activity subscale (FABQ-PA). The modified Oswestry Disability Questionnaire (mOSW) and the Quebec Back Pain Disability Scale (QUE) were used to measure self-reported disability, and the Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire (SF-36) physical component summary (PCS) score was used to assess physical health. Participants provided demographic information and information regarding LBP duration and intensity. Linear regression models were developed using the following dependent variables: mOSW, QUE, and SF-36 PCS scores. Logistic regression was used to determine the association between high FABs and falling.
Results
For each analysis, the FABQ-PA score independently explained 3% to 6% of the variance in the LBP-related disability score and 3% of the variance in the SF-36 PCS score. For all dependent variables, the strongest contributors to explained variance were pain intensity, assistive device use, and FABQ-PA score. High FABs were associated with falling.
Limitations
Future investigations might seek a more diversified sample and utilize both qualitative and quantitative measures for assessing disability and physical health.
Conclusions
Physical activity FABs are independently associated with self-reported disability and overall physical health in older American adults with LBP. High FABs may warrant balance and falls assessment.
In older adults, low back pain (LBP) significantly affects physical function, resulting in greater difficulties with activities of daily living.1,2 Furthermore, from the 1990s to 2000s, there was an increase of greater than 100% in the prevalence of chronic LBP among people aged 65 years and older,3 but limited work has been done to understand the proliferation of LBP in this age group. In younger age groups, some authors have proposed psychosocial risk factors, such as heightened fear-avoidance beliefs (FABs), as key factors in the development and perpetuation of LBP.4,5 In older adults, the role of FABs in LBP progression remains unclear.
Fear-avoidance beliefs in older adults with LBP may be associated with increased disability, as found in younger populations. Increased FABs may be characterized by avoidance behaviors, which can lead to disability.6 In a younger cohort with LBP, Pfingsten et al7 reported that heightened LBP-related FABs motivated avoidance behaviors, resulting in poorer performance during a lower-extremity task, despite no strain to the back. Furthermore, in a cross-sectional study of younger individuals with chronic LBP, Meyer et al8 found that FABs explained a significant percentage of the variance in LBP-related disability. In a group of people with LBP followed longitudinally, FABs also were shown to predict disability after adjusting for pain variables and sociodemographic factors.9 Comparable cross-sectional and prospective studies among people aged 65 years and older are lacking but needed, given an established association between FABs and disability in younger populations.
The Fear-Avoidance Beliefs Questionnaire (FABQ) is commonly used to explore FABs. The FABQ is a measure of an individual's beliefs regarding the impact of physical activity and work on his or her LBP.10 The FABQ has been shown to correlate with measures of disability and with another measure of fear avoidance (ie, the Tampa Scale of Kinesiophobia).11,12 The FABQ comprises 2 subscales: physical activity (FABQ-PA) and work.10 In younger individuals, work-related FABs are independent risk factors for poor recovery from LBP13 and predictors of pain and pain-related disability 1 year after LBP onset.9 Work-related FABs also have been found to be predictors of impairment in physical health-related quality of life.14 In younger populations, although work-related FABs are powerful predictors of disability and physical health, physical activity FABs have not been found to be predictors of disability and physical health.15 Yet, in the older adult population, the work-related subscale may be inappropriate, given that many individuals in this population are retired and such use would disregard the measure's construct validity. Furthermore, understanding whether FABs are predictors of disability in older populations is critical, given that older adults with greater disability may require increased health care, assisted living, and social support services.
Use of the FABQ-PA may be appropriate for studying the relationship between FABs and disability in older individuals. For example, in a study of older American adults with osteoarthritis of the knee (mean age=63.9 years, SD=8.8), researchers administered a modified version of the FABQ for the knee and found that physical activity FABs were associated with self-report measures of function.16 However, Kovacs and colleagues12 found that physical activity FABs were not associated with LBP-related disability and had minimal influence on physical quality of life in Spanish older adults. These cross-sectional study results among Spanish older adults are similar to those reported in younger adult populations with LBP across cultures. Based on the equivocal results regarding FABs, the presence of cultural or generational variables cannot be discounted.
Physical activity FABs and their relationships to measures of LBP-related disability in older American adults have not been investigated. The primary purpose of this cross-sectional study was to examine the association of physical activity FABs with self-reported disability and physical health among community-dwelling older adults with LBP in the United States. We hypothesized that FABs would be independently associated with self-reported disability and overall physical health in older adults with LBP.
The secondary aim of this study was to evaluate the association of physical activity FABs with falling. Previous investigators have reported on fear of falling and its potential predictive value for future falls among older adults,17 but the association of pain-related FABs with physical activity and falling has not been explored. Given associations between FABs and pain intensity18 and the relationship between heightened pain intensity and increased falling,19 we hypothesized that high levels of FABs would be associated with greater odds of having fallen in the previous year.
Method
The participants in this study were part of a population-based survey study (Retirement Community Back Pain Study20) of independently living older adults residing in continuing care retirement communities (CCRCs). These communities provide lodging and nursing services to their residents and include a variety of living arrangements, from independent to group living. One thousand participants were actively recruited from 1 of 4 CCRCs owned by the same corporate group in Maryland and northern Virginia. Within each community, 250 potential participants were randomly selected and sent a survey questionnaire by a staff member of the CCRC, which allowed researchers to remain masked to the participants' identities. Potential participants were allotted 4 weeks for survey completion. Further details on participant recruitment and sampling procedures have been previously published.20,21
Participant data were included in this analysis if the individual was (1) at least 62 years of age, (2) reporting current LBP resulting in activity modification, and (3) able to read and understand English for survey completion. Low back pain location was defined as the region from the bottom of the rib cage to the top of the legs. Individuals with current LBP requiring activity modification were targeted, as they may represent people most likely to seek clinical services for their LBP in an outpatient setting.
Study procedures were exempt from institutional review, as the survey results could not be linked to respondents, but the study was approved by the National Institute on Aging Intramural Program (via a Clinical Investigator's Meeting) and the Research Advisory Board for the CCRCs.
Self-Report Questionnaires
Fear-Avoidance Beliefs Questionnaire.
Within the FABQ's 2 subscales, individual items are scored on a scale of 0 to 6 points. Based on the population sample, participants completed only the FABQ-PA. Within the FABQ-PA, 4 of the 5 questions are scored, for a maximal score of 24 points. Higher FABQ scores indicate a greater tendency to demonstrate avoidance of activity.14 The FABQ has established reliability in individuals under 60 years of age,10 but has not been evaluated in older adults.
Modified Oswestry Disability Questionnaire.
The Oswestry Disability Questionnaire (OSW) is an internationally known measure of LBP-related disability with established reliability and validity.22,23 The Modified Oswestry Disability Questionnaire (mOSW) is a version of the original OSW in which the sex life category is replaced with the employment/homemaking category.24 Hicks and Manal21 recently established reliability and construct validity of the mOSW in older adults with LBP. The mOSW comprises 10 items: pain, personal care, lifting, walking, sitting, standing, sleeping, social life, employment/homemaking, and traveling.24 Items are graded on a scale of 0 to 5 points, with a maximal score of 50 points. Scores are reported as percentages, with higher percentages indicating greater disability.25
Quebec Back Pain Disability Scale.
Another condition-specific measure with established psychometric properties in older adults with LBP is the Quebec Back Pain Disability Scale (QUE).21 As with the OSW, the QUE has been recognized as a LBP assessment tool with international, widespread use.22 The QUE consists of 20 items, which are descriptions of activities. Participants are asked to what extent they experience difficulty with each activity.26 A maximum score of 100 is possible, with higher scores indicating greater disability.26 In older adults with LBP, higher scores may be associated with increased functional limitations and greater pain severity.21
Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire.
The Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire (SF-36) is a comprehensive, generic questionnaire that evaluates health-related quality of life. Compared with other generic health measures, in large populations with LBP, including older adults, the SF-36 is recommended due to its minimal administration time and established psychometric properties.27,28 The questionnaire consists of 36 items, which can be summarized as 2 measures related to physical and mental health29: the physical component summary (PCS) score and the mental component summary (MCS) score. The PCS is represented by 4 domains (physical function, role limitations—physical, bodily pain, and general health), and the MCS also is represented by 4 domains (role limitations—emotional, social function, mental health, and vitality).30 Each measure has a maximum norm-based score of 100, with a score of 50 representing “average” health and higher scores indicating better health status.30
Demographics and Self-Ratings
Participants provided the following additional information: age, sex, weight, education level, assistive device use, and LBP duration. Self-ratings of LBP intensity were collected. Participants rated their current LBP using the Numeric Pain Rating Scale (NPRS), with line anchors of 0 (“no pain”) and 10 (“extremely intense pain”).31 According to a 2005 review, the NPRS has established reliability and validity.31 Participants also responded “yes” or “no” to the question: “In the past 12 months, have you fallen and landed on the floor or the ground?”
Data Analysis
All analyses were performed using PASW Statistics 18.* Descriptive analyses were performed for the entire sample, including demographic factors, pain characteristics, and self-report measures. Separate hierarchical linear regression models were developed using the following dependent variables: mOSW, QUE, and PCS scores. This approach allowed us to examine the independent contribution of FABs about LBP, above and beyond demographic and pain variables, to LBP-related disability and overall physical health among older adults.
Age, sex, weight, education level, and assistive device use were entered in the first step, followed by severity of LBP (ie, pain intensity as measured with the NPRS) and duration of LBP in the second step, and, finally, the FABQ-PA score in the third step. R2 change statistics are reported along with P values at each step of the model to demonstrate the importance of the variables added in that step. To determine the influence that order of entry into the regression models might have on the relationship between FABQ-PA score and the dependent variables, alternate hierarchical regression models were developed in which FABQ-PA score was entered first, followed by the addition of demographic variables in step 2, and pain variables in the final step.
Furthermore, for each of the dependent variables, final reduced regression models were constructed that included only those independent variables that were significantly associated with the dependent variable of interest. Standardized beta coefficients are reported for each independent variable included in the final reduced models to allow for direct comparison between the independent variables in the regression model and the dependent variable being studied. Variance inflation factors (VIFs) were calculated to determine whether there were any multicollinearity issues in any of the models. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were calculated using logistic regression to determine associations between high FABs and fall status within the previous year. Using a standard quartile approach to delineate a high level of FABs, FABQ-PA scores in the upper quartile (highest 25%) of all scores (>18 points) were classified as a high level of fear for this analysis.
Role of the Funding Source
Data collection was funded by the Intramural Research Program of the National Institute on Aging, National Institutes of Health. Preparation of the manuscript by Dr Sions and Dr Hicks was supported by R21 HD057274 (Eunice Kennedy Shriver National Institute of Child Health and Human Development). The work of Dr Hicks, a CORRT scholar, also was supported by 1K12HD055931-01 (Eunice Kennedy Shriver National Institute of Child Health and Human Development).
Results
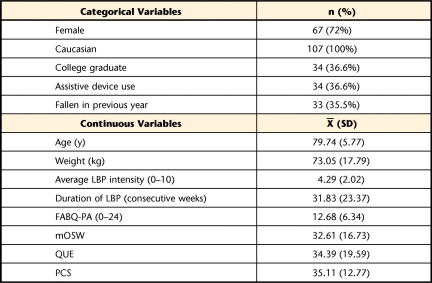
Of the 522 respondents to the initial survey, 107 had current LBP that required activity modification. Of these 107 participants, 93 (87%) had complete data for all analyses. No significant differences were found between the included and excluded participants for any demographic factors (P<.05). The mean age of the sample was 79.74 years (SD=5.77). The majority of the respondents were female, and all respondents were Caucasian. Slightly more than one third of the respondents were college graduates, used an assistive device, and had at least one fall in the previous year. Regarding duration of LBP, 62.5% of the respondents reported pain lasting longer than 12 weeks, with 51.2% of these individuals reporting pain for 52 out of 52 weeks. Mean scores on the LBP-related disability questionnaires indicated moderate disability. Further descriptive characteristics of the respondents are summarized in Table 1.
Table 1.
Descriptive Characteristics of Respondents (n=107)a
LBP=low back pain, FABQ-PA=Fear-Avoidance Beliefs Questionnaire physical activity subscale, mOSW=modified Oswestry Disability Questionnaire, QUE=Quebec Back Pain Disability Scale, PCS=physical component summary score of the Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire (SF-36).
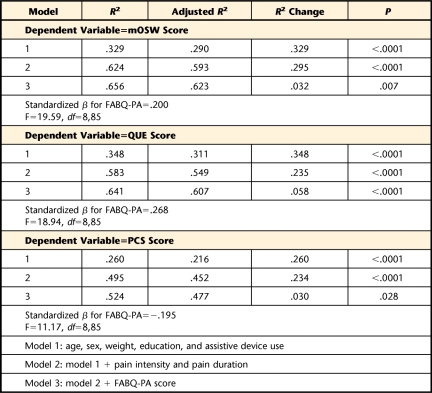
For the mOSW, the factors in model 1 (ie, age, sex, weight, education, and use of an assistive device) explained 33% of the variance (P<.0001) in LBP-related disability. The addition of pain intensity and duration in model 2 explained an additional 30% of the variance (P<.0001). After accounting for demographic factors and pain characteristics, adding FABQ-PA score explained an additional 3% of the variance in the mOSW scores (P=.007). R2 values and R2 change statistics for each model are shown in Table 2. For the QUE, the factors in model 1 explained 35% of the variance (P<.0001), and the inclusion of pain intensity and duration explained an additional 24% of the variance (P<.0001). Inclusion of FABQ-PA score in the model explained an additional 6% of the variance in the QUE scores (P<.0001). For the PCS, the factors in model 1 explained 26% of the variance (P=.0001). With the addition of model 2 variables, an additional 23% of the variance in the PCS scores was explained (P<.0001). Furthermore, when FABQ-PA score was added, an additional 3% of the variance was explained (P=.028).
Table 2.
Hierarchical Linear Regression Modeling Resultsa
FABQ-PA=Fear-Avoidance Beliefs Questionnaire physical activity subscale, mOSW=modified Oswestry Disability Questionnaire, QUE=Quebec Back Pain Disability Scale, PCS=physical component summary score of the Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire (SF-36).
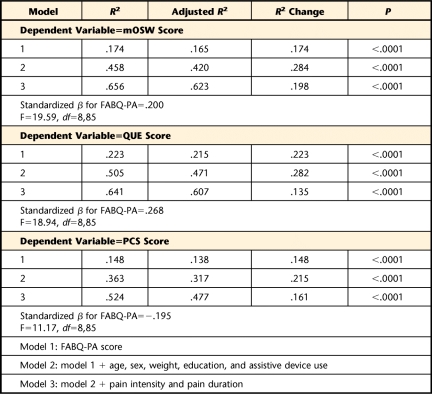
Table 3 delineates the regression model summaries for the analyses where we assessed the influence that order of entry into the regression models might have on the relationship between FABQ-PA score and the dependent variables. For the mOSW, the addition of FABQ-PA score in model 1 explained 17% of the variance (P<.0001) in LBP-related disability. The addition of demographic factors in model 2 explained an additional 28% of the variance (P<.0001). After accounting for FABQ-PA score and demographic factors, adding pain intensity and duration in the final step of the model explained an additional 20% of the variance in the mOSW scores (P<.0001). R2 values and R2 change statistics for each model are shown in Table 3. For the QUE, the addition of FABQ-PA score in model 1 explained 22% of the variance (P<.0001), and the inclusion of demographic factors explained an additional 28% of the variance (P<.0001). Inclusion of pain intensity and duration in the model explained an additional 14% of the variance in the QUE scores (P<.0001). For the PCS, the addition of FABQ-PA score explained 15% of the variance in model 1 (P<.0001). With the addition of demographic variables, an additional 22% of the variance in the PCS scores was explained (P<.0001). Finally, when pain intensity and duration were added to the model, an additional 16% of the variance in the PCS scores was explained (P<.0001).
Table 3.
Hierarchical Linear Regression Modeling Results: Alternate Order of Entrya
FABQ-PA=Fear-Avoidance Beliefs Questionnaire physical activity subscale, mOSW=modified Oswestry Disability Questionnaire, QUE=Quebec Back Pain Disability Scale, PCS=physical component summary score of the Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire (SF-36).
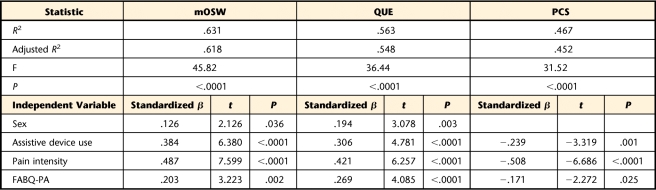
For the final reduced linear regression models (Tab. 4), assistive device use, pain intensity, and FABQ-PA score explained a significant amount of variance in mOSW, QUE, and PCS scores, whereas sex was significantly associated only with mOSW and QUE scores. The strongest predictor across all 3 models was pain intensity, followed by assistive device use, and then FABQ-PA score. The standardized beta coefficients for the FABQ-PA scores would indicate that a 1-point increase in FABQ-PA score would result in a 0.203-unit increase in mOSW score, a 0.269-unit increase in QUE score, and a 0.171-unit reduction in PCS score. For all models, the VIF indicated low likelihood of multicollinearity, with VIF values ranging from 1.02 to 1.18.
Table 4.
Reduced Final Linear Regression Models for Measures of Self-Reported Disability and Physical Healtha
FABQ-PA=Fear-Avoidance Beliefs Questionnaire physical activity subscale, mOSW=modified Oswestry Disability Questionnaire, QUE=Quebec Back Pain Disability Scale, PCS=physical component summary score of the Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire (SF-36).
Logistic regression analysis revealed that high FABs were associated with more than a 3-fold greater odds of having fallen in the previous year (OR=3.38, 95% CI=1.05–11.04).
Discussion
The primary objective of this study was to examine the relationship between FABs and self-reported disability in older American adults with LBP. As hypothesized, pain-related fear was independently associated with LBP-related disability and overall physical health, even after controlling for demographics, pain intensity, and pain duration. Although FABs were significant contributors regardless of the modeling approach used, the amount of variance explained by FABs was affected by the order of entry into the model. When FABQ-PA score was entered first in the model, regardless of the dependent variable, it explained a larger proportion of variance than when entered last, suggesting that FABQ-PA score shares variance with the other independent variables. When FABQ-PA score was entered first, there was more variance available to be explained compared with when it was entered last in the model. Most importantly, regardless of the order of entry for the independent variables, the standardized beta coefficient is the same in both models for each dependent variable, which suggests that there is no confounding and that the developed models are fairly robust.
Pain intensity and assistive device use were the strongest predictors in each of the models. Nonetheless, the FABQ-PA score helped to independently explain a small but significant percentage of the variance in scores in each self-report questionnaire, beyond what was explained by participant demographic and pain information. Thus, this study provides preliminary evidence that physical-activity FABs in older American adults with LBP may help explain LBP-related disability and overall physical health. We acknowledge that the cross-sectional nature of this study does not allow establishment of a causal relationship between FABs and future disability. However, these findings support future, prospective investigations of the fear-avoidance model in older American adults with LBP.
In younger adults, LBP-related disability has been reported to be significantly correlated to work-related FABs.15,32 For example, in a prospective study of young Americans with LBP, George et al32 found work-related FABs to be a better indicator of disability than physical activity FABs. The authors proposed that such findings may be secondary to work-related FABs having a more significant impact on perceived social role factors than physical activity FABs, ultimately affecting disability to a greater degree.32
Based on our sample, we did not assess work-related FABs because we did not believe that they would significantly affect social role or disability in these retirees. We do acknowledge that the FABQ-PA, which contains only 4 scored items, may not be sufficiently specific to optimally determine the impact of FABs on the diversified social roles of older adults (eg, primary caretaker for an ailing spouse, after-school child care provider, volunteer at a local community center). Future investigations may seek to develop a scale assessing LBP-related FABs on common societal roles of older adults.
Pain chronicity may be responsible for differing results regarding FABs and their relationships to disability and overall physical health. In a cross-sectional study of community-dwelling Spanish older adults with acute LBP, Kovacs et al33 reported clinically small effects of physical activity FABs on LBP-related disability. Although similar to the participants in our study, these Spanish older adults had acute pain,33 whereas 62.5% of our participants reported having chronic LBP. Greater duration of spinal pain is related to pain catastrophizing,34 which is an exaggerated negative “mental set” associated with pain.8 Pain catastrophizing has been linked to pain intensity and disability8 and may help explain the relationship between FABs and LBP-related disability in older American adults with chronic pain.
Ethnicity distinguishes between groups of people based on culture and behaviors, as well as biological and physical characteristics.35 Ethnicity may help explain the differences in findings between our participants and Spanish older adults.12,33 Hispanic cultural traditions view reality as unchangeable rather than capable of manipulation, which corresponds with an external locus of control style.36 Compared with other ethnic groups, Hispanics report greater pain intensities.36 Higher pain intensities have been associated with greater difficulty with functional tasks37 and decreased physical mobility.38 Pain intensity may partially mediate the relationship between FABs and disability.15 Consequently, we would expect Hispanics or Spaniards with LBP to report greater FABs, decreased physical health, and greater LBP-related disability. Nonetheless, strong relationships between FABs and disability and FABs and physical quality of life have not been found in Spanish older adults,12 likely because FABs are always viewed in the context of pain intensity and Hispanics have an external locus of control style. Future studies might further investigate the impact of ethnicity on FABs and their relationships to disability and physical health.
Understanding the impact of FABs on disability is important to health care practitioners, as using interventions that address physical activity FABs in older adults with LBP may improve outcomes related to function and physical health. Specifically, screening for physical activity FABs in older individuals with LBP may alert practitioners to FABs, allow consideration of FABs for an effective treatment plan, or prompt consultation for an interdisciplinary intervention approach. Unfortunately, although intervention strategies to address FABs in younger individuals with LBP have been tested, such strategies remain unexplored in individuals over 65 years of age. For example, in vivo exposure, which systematically incorporates movements and tasks avoided secondary to fear of pain or reinjury, has been purported to address FABs.39 In vivo exposure has demonstrated efficacy in younger individuals with chronic LBP for decreasing pain-related fear40,41 and disability.40 Our results call for prospective, longitudinal investigations evaluating FABs in older adult patient populations to better understand the impact of psychosocial state on physical rehabilitation outcomes. If FABs affect patient outcomes, similar interventional investigations of strategies to address FABs in older adults may be warranted. Such strategies ultimately may decrease LBP-related disability and improve physical health outcomes in individuals with heightened FABs.
Recently, researchers have explored the relationship between fear beliefs, avoidance behaviors, and falling in older adults. For example, Hadjistavropoulos et al17 reported fear of falling was a predictor of falling in community-dwelling older Canadian adults. Furthermore, in a similar sample of older American adults, Bertera and Bertera42 found fear of falling to be the most important factor in predicting activity avoidance. They also reported that a greater number of falls enhanced the impact of fear of falling on avoidance behaviors. However, our results are the first to document a relationship between elevated pain-related FABs and increased likelihood of a fall in older adults.
This relationship may be partially explained by the association between heightened FABs and pain intensity,18 as more severe or disabling pain is associated with higher fall rates.19 Blyth et al43 found that individuals with moderate to severe pain-related interference with daily work were more likely to report a fall or multiple falls in the previous year compared with those without pain. Furthermore, Leveille et al44 reported that older women with moderate to severe widespread pain had a greater likelihood of falling (OR=1.66, 95% CI=1.25–2.21) at follow-up compared with women with no pain or mild pain in only one musculoskeletal site. When evaluating LBP specifically, Morris et al45 found that occasional fallers (ie, those with one self-reported fall in the previous year) were more likely to have LBP (OR=1.54, 95% CI=1.10–2.16).
Given our results on FABs and fall history, it may be important to screen not only for pain intensity but also for FABs. Consider that even in the absence of LBP, age-related trunk postural changes result in inefficient balance recovery with external perturbations.46 Therefore, recognition, screening, and initiation of fall prevention treatment may be imperative in the older adult with LBP, as pain and possibly FABs are superimposed on age-related changes. If high levels of LBP-related FABs are detected, a balance or falls screening and subsequent retraining may be warranted. It is important to note that the cutoff point of >18 out of 24 on the FABQ-PA should not be used as a screening cutoff point for fall risk in older adults with LBP, as this was not the intention of our study. Future work, using a prospective design, is needed to establish a specific cutoff point that is predictive of increased fall risk. Furthermore, established and validated tools are already available to assess fall risk in the geriatric population.47,48
Although this is the first study to show associations between FABs and LBP-related disability and physical health in older American adults, there are several limitations to consider when interpreting these results. First, the study sample was predominantly well-educated, Caucasian women, limiting the generalizability of these results. Nonetheless, there is evidence to suggest that the impact of LBP-related FABs may be even greater in other populations. For example, McCracken et al49 found greater avoidance of activity and fearful thinking in African Americans with chronic pain compared with Caucasian Americans. Furthermore, Szanton et al50 recently reported that frailty odds are increased for those with lower educational levels. Underprivileged populations with poorer health status may have heightened disability scores and lower physical health status. Future studies on older minority populations with LBP may potentially implicate LBP-related FABs as even greater determinants of disability and physical health.
Second, mailed self-report questionnaires provided the data for this study. Therefore, we recognize an inability to control for proxy bias or to screen for respondent cognitive status, as well as inherent issues associated with self-report measures, such as social desirability and recall bias. We cannot be certain that a proxy did not complete the surveys. We attempted to address the possibility of bias from social desirability by ensuring confidentiality of respondents. During questionnaire completion, participants were asked to rate their current condition, except when reporting fall history, to decrease recall bias. Future investigations might consider a combination of qualitative and quantitative measures to determine disability and physical health status.
Another potential limitation of our study is the low response rate of 52% for this survey, which is not uncommon in studies of older adults. As previously described,20 we are fairly confident that the sample is representative of the larger population in these CCRCs based upon the fact that the demographics of our sample are nearly identical to the demographics of the entire population in the 4 CCRCs that were examined. Furthermore, there are some missing data (∼13%) among the participants with current LBP. The lack of differences in demographic factors between the participants with and without missing data would suggest that there is no particular source of bias causing those respondents with missing data to have incomplete data; however, the missing data should be considered as the results are interpreted.
Although FABs explain a similar percentage of the variance in self-report measures of disability and physical health among older adults, above and beyond demographics and pain factors, we acknowledge that the percentage explained, is relatively small. However, when considering the potential implications of greater disability and poorer physical health in this population (ie, increased need for physical assistance, resulting in greater resource utilization and increased economic burden), the potential to improve disability or physical health minimally may equate to clinically meaningful improvements in functional independence. Follow-up prospective studies may evaluate whether interventions that address physical activity FABs in older American adults with LBP are not only successful at improving patient functional independence but also are cost-effective.
In conclusion, this is the first study to show that physical activity FABs are independently associated with self-reported disability and overall physical health in older American adults with LBP. Among the strongest predictors of disability status are pain intensity and FABQ-PA score. Additionally, our results indicate a relationship between elevated pain-related FABs and increased likelihood of falling. Pending future research, interventions that address not only pain intensity FABs but also physical activity FABs may demonstrate efficacy in decreasing disability, improving physical health, and decreasing falls in older adults with LBP.
The Bottom Line
What do we already know about this topic?
Psychosocial risk factors, such as heightened fear-avoidance beliefs, are key factors in the perpetuation of low back pain and low back pain–related disability in younger adults, but the significance of these risk factors in older American adults remains unknown.
What new information does this study offer?
Elevated fear-avoidance beliefs were associated with greater low back pain–related disability, worse physical health, and greater odds of having fallen in older American adults.
If you're a patient, what might these findings mean for you?
When receiving treatment for low back pain, you should be aware that fear of further injury may cause you to avoid certain movements or activities, which can lead to worse outcomes in the long run. Further research will be necessary to determine whether treatment strategies designed to address elevated fear will be effective in decreasing disability, improving physical health, and decreasing falls in older adults with low back pain.
Footnotes
Both authors provided concept/idea/research design, writing, data analysis, and consultation (including review of manuscript before submission). Dr Hicks provided data collection, project management, and fund procurement.
A platform presentation of this research was given at the Combined Sections Meeting of the American Physical Therapy Association; February 17–20, 2010; San Diego, California. A poster presentation of this research was made at the Exercise and Physical Activity in Aging Conference: Blending Research and Practice (ExPAAC); July 29–31, 2010; Indianapolis, Indiana.
Data collection was funded by the Intramural Research Program of the National Institute on Aging, National Institutes of Health. Preparation of the manuscript by Dr Sions and Dr Hicks was supported by R21 HD057274 (Eunice Kennedy Shriver National Institute of Child Health and Human Development). The work of Dr Hicks, a CORRT scholar, also was supported by 1K12HD055931-01 (Eunice Kennedy Shriver National Institute of Child Health and Human Development).
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
References
- 1. Di Iorio A, Abate M, Guralnik JM, et al. From chronic low back pain to disability, a multifactorial mediated pathway: the InCHIANTI study. Spine (Phila Pa 1976). 2007;32:E809–E815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hicks GE, Simonsick EM, Harris TB, et al. Trunk muscle composition as a predictor of reduced functional capacity in the health, aging and body composition study: the moderating role of back pain. J Gerontol A Biol Sci Med Sci. 2005;60:1420–1424 [DOI] [PubMed] [Google Scholar]
- 3. Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cohen SP, Argoff CE, Carragee EJ. Management of low back pain. BMJ. 2008;337:a2718. [DOI] [PubMed] [Google Scholar]
- 5. Fritz JM, George SZ, Delitto A. The role of fear-avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain. 2001;94:7–15 [DOI] [PubMed] [Google Scholar]
- 6. Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332 [DOI] [PubMed] [Google Scholar]
- 7. Pfingsten M, Leibing E, Harter W, et al. Fear-avoidance behavior and anticipation of pain in patients with chronic low back pain: a randomized controlled study. Pain Med. 2001;2:259–266 [DOI] [PubMed] [Google Scholar]
- 8. Meyer K, Tschopp A, Sprott H, Mannion AF. Association between catastrophizing and self-rated pain and disability in patients with chronic low back pain. J Rehabil Med. 2009;41:620–625 [DOI] [PubMed] [Google Scholar]
- 9. Grotle M, Vollestad NK, Brox JI. Clinical course and impact of fear-avoidance beliefs in low back pain: prospective cohort study of acute and chronic low back pain; II. Spine (Phila Pa 1976). 2006;31:1038–1046 [DOI] [PubMed] [Google Scholar]
- 10. Waddell G, Newton M, Henderson I, et al. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168 [DOI] [PubMed] [Google Scholar]
- 11. Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80:329–339 [DOI] [PubMed] [Google Scholar]
- 12. Kovacs F, Abraira V, Cano A, et al. Fear avoidance beliefs do not influence disability and quality of life in Spanish elderly subjects with low back pain. Spine (Phila Pa 1976). 2007;32:2133–2138 [DOI] [PubMed] [Google Scholar]
- 13. Elfering A, Mannion AF, Jacobshagen N, et al. Beliefs about back pain predict the recovery rate over 52 consecutive weeks. Scand J Work Environ Health. 2009;35:437–445 [DOI] [PubMed] [Google Scholar]
- 14. Keeley P, Creed F, Tomenson B, et al. Psychosocial predictors of health-related quality of life and health service utilisation in people with chronic low back pain. Pain. 2008;135:142–150 [DOI] [PubMed] [Google Scholar]
- 15. Cai C, Pua YH, Lim KC. Correlates of self-reported disability in patients with low back pain: the role of fear-avoidance beliefs. Ann Acad Med Singapore. 2007;36:1013–1020 [PubMed] [Google Scholar]
- 16. Scopaz KA, Piva SR, Wisniewski S, Fitzgerald GK. Relationships of fear, anxiety, and depression with physical function in patients with knee osteoarthritis. Arch Phys Med Rehabil. 2009;90:1866–1873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hadjistavropoulos T, Martin RR, Sharpe D, et al. A longitudinal investigation of fear of falling, fear of pain, and activity avoidance in community-dwelling older adults. J Aging Health. 2007;19:965–984 [DOI] [PubMed] [Google Scholar]
- 18. Coudeyre E, Tubach F, Rannou F, et al. Fear-avoidance beliefs about back pain in patients with acute LBP. Clin J Pain. 2007;23:720–725 [DOI] [PubMed] [Google Scholar]
- 19. Leveille SG, Jones RN, Kiely DK, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302:2214–2221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hicks GE, Gaines JM, Shardell M, Simonsick EM. Associations of back and leg pain with health status and functional capacity of older adults: findings from the retirement community back pain study. Arthritis Rheum. 2008;59:1306–1313 [DOI] [PubMed] [Google Scholar]
- 21. Hicks GE, Manal TJ. Psychometric properties of commonly used low back disability questionnaires: are they useful for older adults with low back pain? Pain Med. 2009;10:85–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Calmels P, Bethoux F, Condemine A, Fayolle-Minon I. Low back pain disability assessment tools [in French]. Ann Readapt Med Phys. 2005;48:288–297 [DOI] [PubMed] [Google Scholar]
- 23. Vianin M. Psychometric properties and clinical usefulness of the Oswestry Disability Index. J Chiropr Med. 2008;7:161–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale [erratum in: Phys Ther. 2008;88:138–139]. Phys Ther. 2001;81:776–788 [DOI] [PubMed] [Google Scholar]
- 25. Davidson M. Rasch analysis of three versions of the Oswestry Disability Questionnaire. Man Ther. 2008;13:222–231 [DOI] [PubMed] [Google Scholar]
- 26. Reneman MF, Jorritsma W, Schellekens JM, Goeken LN. Concurrent validity of questionnaire and performance-based disability measurements in patients with chronic nonspecific low back pain. J Occup Rehabil. 2002;12:119–129 [DOI] [PubMed] [Google Scholar]
- 27. Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: introduction. Spine (Phila Pa 1976). 2000;25:3097–3099 [DOI] [PubMed] [Google Scholar]
- 28. Garratt AM, Ruta DA, Abdalla MI, et al. The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS? BMJ. 1993;306:1440–1444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ferrari R. Responsiveness of the short-form 36 and oswestry disability questionnaire in chronic nonspecific low back and lower limb pain treated with customized foot orthotics. J Manipulative Physiol Ther. 2007;30:456–458 [DOI] [PubMed] [Google Scholar]
- 30. Veresciagina K, Ambrozaitis KV, Spakauskas B. Health-related quality-of-life assessment in patients with low back pain using SF-36 questionnaire. Medicina (Kaunas). 2007;43:607–613 [PubMed] [Google Scholar]
- 31. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804 [DOI] [PubMed] [Google Scholar]
- 32. George SZ, Fritz JM, Childs JD. Investigation of elevated fear-avoidance beliefs for patients with low back pain: a secondary analysis involving patients enrolled in physical therapy clinical trials. J Orthop Sports Phys Ther. 2008;38:50–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kovacs F, Noguera J, Abraira V, et al. The influence of psychological factors on low back pain-related disability in community dwelling older persons. Pain Med. 2008;9:871–880 [DOI] [PubMed] [Google Scholar]
- 34. Demmelmaier I, Lindberg P, Asenlof P, Denison E. The associations between pain intensity, psychosocial variables, and pain duration/recurrence in a large sample of persons with nonspecific spinal pain. Clin J Pain. 2008;24:611–619 [DOI] [PubMed] [Google Scholar]
- 35. Edwards CL, Fillingim RB, Keefe F. Race, ethnicity and pain. Pain. 2001;94:133–137 [DOI] [PubMed] [Google Scholar]
- 36. Bates MS, Edwards WT, Anderson KO. Ethnocultural influences on variation in chronic pain perception. Pain. 1993;52:101–112 [DOI] [PubMed] [Google Scholar]
- 37. Weiner DK, Haggerty CL, Kritchevsky SB, et al. How does low back pain impact physical function in independent, well-functioning older adults: evidence from the Health ABC Cohort and implications for the future. Pain Med. 2003;4:311–320 [DOI] [PubMed] [Google Scholar]
- 38. Leveille SG, Guralnik JM, Hochberg M, et al. Low back pain and disability in older women: independent association with difficulty but not inability to perform daily activities. J Gerontol A Biol Sci Med Sci. 1999;54:M487–M493 [DOI] [PubMed] [Google Scholar]
- 39. Leeuw M, Goossens ME, van Breukelen GJ, et al. Exposure in vivo versus operant graded activity in chronic low back pain patients: results of a randomized controlled trial. Pain. 2008;138:192–207 [DOI] [PubMed] [Google Scholar]
- 40. Vlaeyen JW, de Jong J, Geilen M, et al. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18:251–261 [DOI] [PubMed] [Google Scholar]
- 41. Woods MP, Asmundson GJ. Evaluating the efficacy of graded in vivo exposure for the treatment of fear in patients with chronic back pain: a randomized controlled clinical trial. Pain. 2008;136:271–280 [DOI] [PubMed] [Google Scholar]
- 42. Bertera EM, Bertera RL. Fear of falling and activity avoidance in a national sample of older adults in the United States. Health Soc Work. 2008;33:54–62 [DOI] [PubMed] [Google Scholar]
- 43. Blyth FM, Cumming R, Mitchell P, Wang JJ. Pain and falls in older people. Eur J Pain. 2007;11:564–571 [DOI] [PubMed] [Google Scholar]
- 44. Leveille SG, Bean J, Bandeen-Roche K, et al. Musculoskeletal pain and risk for falls in older disabled women living in the community. J Am Geriatr Soc. 2002;50:671–678 [DOI] [PubMed] [Google Scholar]
- 45. Morris M, Osborne D, Hill K, et al. Predisposing factors for occasional and multiple falls in older Australians who live at home. Aust J Physiother. 2004;50:153–159 [DOI] [PubMed] [Google Scholar]
- 46. Tang PF, Woollacott MH. Inefficient postural responses to unexpected slips during walking in older adults. J Gerontol A Biol Sci Med Sci. 1998;53:M471–M480 [DOI] [PubMed] [Google Scholar]
- 47. Wrisley DM, Kumar NA. Functional gait assessment: concurrent, discriminative, and predictive validity in community-dwelling older adults. Phys Ther. 2010;90:761–773 [DOI] [PubMed] [Google Scholar]
- 48. Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed “Up & Go” Test. Phys Ther. 2000;80:896–903 [PubMed] [Google Scholar]
- 49. McCracken LM, Matthews AK, Tang TS, Cuba SL. A comparison of blacks and whites seeking treatment for chronic pain. Clin J Pain. 2001;17:249–255 [DOI] [PubMed] [Google Scholar]
- 50. Szanton SL, Seplaki CL, Thorpe RJ, Jr, et al. Socioeconomic status is associated with frailty: the Women's Health and Aging Studies. J Epidemiol Community Health. 2010;64:63–67 [DOI] [PMC free article] [PubMed] [Google Scholar]