Abstract
Background
Remodeling of the mitral annulus may contribute to progression of mitral regurgitation (MR). In patients with moderate to severe mitral regurgitation short term treatment with a β-blockers has been shown to increase left ventricular end diastolic and end systolic volume and this could deleteriously increase mitral valve annular dimensions. The objective of this study was to quantify the effects of a short duration of β-blocker treatment on mitral annular dimensions and dynamics in patients with mitral regurgitation due to primary degenerative valve disease.
Methods and Results
Twenty-five patients with moderate to severe degenerative MR and normal left ventricular systolic function were studied in a double blind crossover experiment using a β1-selective adrenergic blocker and placebo administered for 14±3days. Cardiac magnetic resonance images were acquired after each treatment period to quantify mitral annular dimensions. At end diastole (ED) there was no change in annular area (1659±331 vs 1632±299mm2, P<0.19), annular perimeter (154.3±16.4 vs 152±13.9mm, P<0.13), septal-lateral dimension(38.0±5mm vs 39.0±4.5mm, P<0.15), nor annular height (9.8±3.8 vs 9.5±2.5mm, P<0.53). β-blockade resulted in significant ED decreases in commissure-commissure (CC) dimension (48.9 ± 4.6mm vs 47.2 ± 4.0mm P<0.01) and eccentricity (1.3 ± 0.2 vs 1.2 ± 0.1 P<0.01). At end systole (ES), ß-blockade conferred a small, but significant decrease in annular perimeter (161.0±19.3 vs 156.8±16.9mm, P<0.04) and eccentricity (1.2±0.1 vs 1.1±0.1 P<0.02) and the SL dimension significantly increased (41.5±5.7 vs 43.0±5.3mm, P<0.03). CC, annular area, and annular height at ES were not significantly different.
Conclusions
Despite significant increases in LVEDV and LVESV, short-term β-blocker treatment of patients with moderate to severe mitral regurgitation reduced or preserved all mitral annular dimensions, except SL at ES.
Keywords: mitral valve regurgitation, β-blockers, annular geometry, mitral valve annulus
Introduction
Primary mitral regurgitation (MR), which is usually caused by myxomatous degeneration of the mitral valve (MV) leaflets, leads to a progressive increase in left ventricular (LV) volume. Eventually this may result in LV dysfunction and heart failure. Current guidelines recommend mitral valve repair or replacement in patients with chronic severe MR who have symptoms or evidence of LV dysfunction1. Surgery may also be considered in asymptomatic patients with normal LV function who have a repairable valve because of a high risk of disease progression and adverse outcomes1. However, many asymptomatic patients with moderate to severe mitral regurgitation are not referred for early surgery and in these patients a medical treatment, which reduces the risk of disease progression, would be beneficial. The clinical management of patients with chronic primary MR, however, remains contentious2, 3.
In a retrospective observational study by Varadarajan et al. of 895 patients with severe ischemic or non-ischemic mitral valve regurgitation and a normal LV ejection fraction mortality was lower for patients treated with a β-blocker. This benefit might be related to a favorable effect of the β-blocker on LV function, as observed in patients with heart failure. Alternatively, β-blockers could influence the progression of mitral regurgitation.
Mitral valve annular dilation is one cause of the progression of MR severity. In patients with non-ischemic dilated cardiomyopathy, mild to moderate heart failure and severe MR surgical ring annuloplasty results in reverse left ventricular remodeling4. No similar data are currently available in patients with primary MR. In patients with heart failure beta-blockers reduce the severity of mitral regurgitation probably by a favorable effect on LV remodeling. In a previous report5 we described the effects of short-term treatment with a ß-blocker in patients with moderate to severe mitral regurgitation and normal LV function. In that study ß-blockers reduced LV work and mitral regurgitant volume per minute, but mitral regurgitant volume per beat did not change. ß-blockers, however, also increased LVEDV and LVESV, which because of annular-ventricular continuity could have an adverse effect on mitral annular dimensions. The impact of ß-blockers on mitral valve annular dimensions and dynamics in patients with degenerative mitral valve regurgitation is uncertain. If ß-blockers were to significantly reduce or preserve annular dimensions in patients with primary MR and consequently reduce the severity or progression of MR, then the effect may be to postpone the need for invasive surgical repair.
The objective of this work was to quantify the short-term effects of the ß1-adrenergic receptor blocker metoprolol on MV annular dimensions and dynamics in patients with degenerative mitral valve disease and chronic MR. We hypothesize that in patients with MR, acute treatment with ß-blockers will decrease annular dimensions despite an increase in LVEDV and LVESV.
Methods
Patient population
Patients were recruited if they had moderate to severe mitral regurgitation without NYHA class III or IV symptoms for heart failure. Mitral regurgitation in all patients was caused by primary degenerative disease. Two subjects had anterior leaflet, 14 posterior leaflet, and 9 bileaflet prolapse. Eleven subjects had a flail or partial flail mitral leaflet. All patients had normal LV function defined as an ejection fraction >55% determined by a 2D echocardiography screening exam. MR grade was characterized by either vena contracta width >3mm, regurgitant volume >30mL/beat and/or an effective regurgitant orfice >0.2cm2 on Doppler echocardiography. Exclusion criteria included previous myocardial infarction, renal or respiratory disease, any other valvular disease, or contraindication to β-blocker treatment. This study was approved by the local institutional ethics committee and each participant provided written informed consent5.
A total of 25 patients were enrolled. Demographics, history, hemodynamics, and global LV functional characteristics were previously reported5. The mean age of participants was 61±10 years; the majority of whom were male (21). The average body mass index was 25.8±3.8. Twelve (48%) had a history of hypertension and 11 (44%) were on ACE inhibiting medication. All patients were in normal sinus rhythm. The majority of patients (18) were asymptomatic but seven had NYHA class IIa symptoms.
Study design
Enrolled patients were studied in a double blind crossover experiment using the β1-selective adrenergic blocker metoprolol. Complete study details are described in Stewart et al5. Briefly, patients were randomly assigned to two groups – ß-blocker treatment (BB) and placebo (PL). Each group received their respective treatments for 14±3days and, following a washout period of 2–14 days, changed their medications from PL to BB or vice versa5. After each treatment period a clinical assessment, ECG, and cardiac magnetic resonance imaging (MRI) exam were performed. No treatment order effects were observed and all other medications remained unchanged during the trial.
Image acquisition
Cardiac MRI exams were performed on a 1.5T Siemens (Erlangen, Germany) Avanto scanner. Long axis views were obtained in six radially prescribed slices centered about the MV and passing through the apex (separated by 30°) using a breath held, gated, balanced steady-state free precession (TruFISP) sequence (TE/ TR=1.6/3.2ms; 30ms temporal resolution; 6mm slice thickness; 360mm FOV; 256×208 matrix; ~25 cine frames). A stack of short axis slices spanning from the valve plane to the ventricular apex was also acquired. Standard functional data derived from the short axis views and phase contrast data have been previously reported5.
Data analysis
End diastolic (ED) and end systolic (ES) cardiac phases were identified as coincident with mitral valve closure (ED) and aortic valve closure (ES) from the long axis images. Two MV annular points where the valve leaflet attaches to the wall were identified in each long axis view at ED and custom non-rigid registration software automatically tracked the remaining points through all phases of the cardiac cycle6 (Figure 1A). Image features were automatically tracked throughout the cardiac cycle by finding the optimal non-linear warp between successive frames based on a pixel sum-of-squared-differences metric6. This software has been validated for tracking epicardial and endocardial left ventricular contours for the assessment of left ventricular wall mass and volumes.
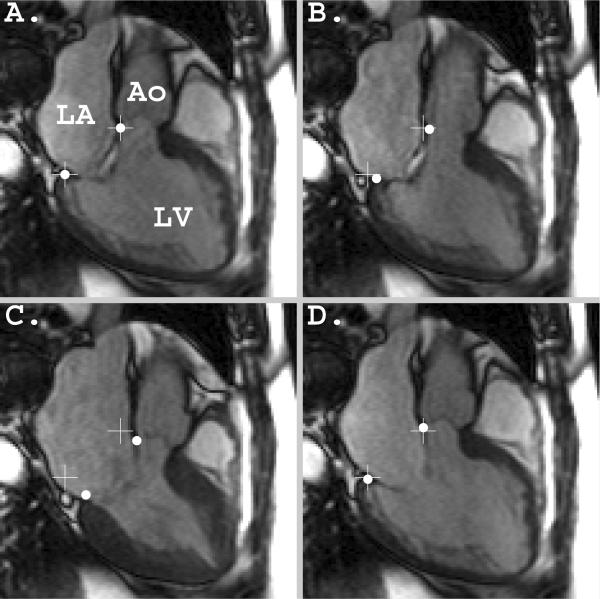
Figure 1.
Demonstration of typical image quality and automatic tracking results. Points were expertly chosen at ED when the mitral and aortic valve closed (A), then automatically propagated to all cardiac phases including the aortic valve opening (B), aortic valve closure (C), and mitral valve opening (D). The white hash marks (+) indicate the expertly chosen annular points at ED and are shown in each frame to provide a motion reference.
Validation of the custom non-rigid registration software for tracking mitral annular points was performed for the first time as part of this study. Bland-Altman analysis was used to assess the quality of the automatic tracking of mitral valve points7. An expert observer (DBE) identified two mitral annular points in both the ED and ES images in each of the six long-axis views and custom software recorded the two-dimensional image pixel coordinates. The ED points were used as an input to the automatic tracking software, which returned an estimate of the annular points at ES (ES_EST). Similarly, the hand picked ES points were used as inputs to the automatic tracking software to estimate the position of the annular points at ED (ED_EST). The three-dimensional scanner coordinates of each point were projected onto a local radial and longitudinal coordinate system. The longitudinal direction was defined as a unit vector pointing along an axis from the left ventricular apex to the centroid of the mitral valve. The radial direction was defined as a unit vector pointing from each annular point along a direction orthogonal to the longitudinal direction. The difference (ED-ED_EST and ES-ES_EST) and the average (mean of ED and ED_EST and the mean of ES and ES_EST) of the recorded radial and longitudinal coordinate results obtained by the expert and the automatic tracking software were used to construct Bland-Altman figures to calculate the bias and the limits of agreement (95% confidence intervals). A second observer (CGF) also identified two mitral annular points in the ED images in each of the six long-axis views in order to provide estimates of inter-observer variability.
Each of the twelve identified points on the mitral valve annulus at ED and ES were converted from image coordinates to scanner coordinates in order to create a three-dimensional model of the annulus at each cardiac phase. The model was created independently for each cardiac phase using a cubic interpolating (non-smoothing) spline that incorporated each of the twelve annular points. Annular perimeter was measured by summing the distance between densely spaced points along the spline. Annular area was calculated by summing the area of small triangles that adjacent points along the annular spline made with the centroid of the annulus.
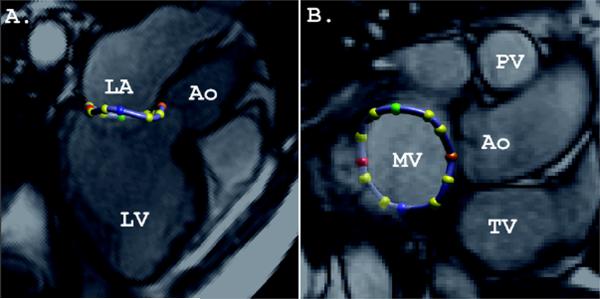
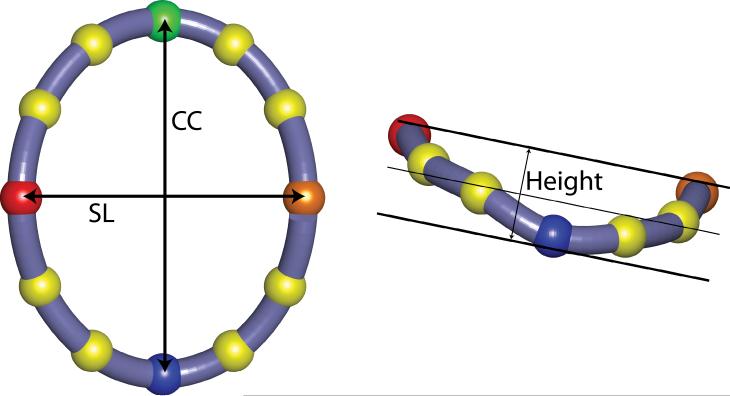
Figure 2 shows an example model of the mitral annulus with labeled anatomical points. The most superior point nearest the aorto-mitral juncture was identified as the saddlehorn (SH). A short axis image at the level of the mitral valve plane was used to identify mitral annular points nearest the anterior (ACOM) and posterior (PCOM) mitral valve commissures. The commissure-commissure axis was defined as a line from the ACOM to the PCOM. The point on the annulus opposite the SH point along a line perpendicular to the commissure-commissure axis was defined as the cantle (CA). The septal-lateral (SL) and commissure-commissure (CC) dimensions were measured as the Euclidean distance from SH to CA and PCOM to ACOM respectively. Mitral annular eccentricity was calculated as the ratio of CC to SL (Figure 3).
Figure 2.
The mitral annular model at end-diastole (ED) shown intersecting a semi-transparent long axis (A) and semi-transparent short axis (B) cine images. Note, the short axis image plane is not co-planar with the mitral annular plane, therefore it intersects the model of the annulus. Ao – aortic valve; MV – mitral valve; PV – pulmonary valve; and TV – tricuspid valve. Saddle horn – orange; cantle – red; anterior commissure – green; posterior commissure – blue.
Figure 3.
Model of the mitral annulus with labeled anatomical dimensions (SL – septal-lateral diameter, CC – commisure-commisure diameter, Height – mitral annular height, red – saddle horn, blue – anterior commisure, green – posterior commisure, orange – cantle). The thin line is the best-fit plane to the annular markers and is used for measuring annular height.
In order to estimate the mitral annular height a plane was fitted using linear least-squares regression to the twelve markers at each cardiac phase. The mitral annular height was defined as the sum of the perpendicular distance from the saddlehorn (most superior point) to the fit-plane plus the perpendicular distance from the most inferior marker to the fit-plane (Figure 3).
In order to compare ß-blocker induced changes in mitral annular dimensions (SL and CC) to the corresponding changes in LV dimensions, the LV diameter along the SL and CC axes was extracted at ED and ES at a level one-third below the base of the heart. Correlation coefficients at ED and ES were calculated between annular and ventricular SL and CC changes (BB-PL). The correlation coefficient between each mitral annular geometric measure and mitral regurgitant volume per minute were also calculated. Lastly, the correlation between the change in regurgitant volume per minute (PL-BB) and PL mitral regurgitant volume per minute was calculated.
The dynamic data for each measured parameter was temporally resampled with interpolating splines during the diastolic and systolic intervals to facilitate comparison of events between patients despite a range of patient heart rates. The data for each subject and each measure between aortic valve closure (beginning of diastole) and mitral valve closure (end diastole) were resampled to the first one-third of the cardiac cycle and data between mitral valve closure (beginning of systole) and aortic valve closure (end systole) were resampled to the remaining two-thirds of the cardiac cycle.
Statistical results for each of the measured variables and the within subject differences (Δ) are reported as mean±SD. Two-tailed paired t-tests were used to identify the statistical differences in annular dimensions and dynamics between PL and BB treatment groups. P<0.05 was considered statistically significant. Intra- and inter-observer coefficients of variation (standard deviation of the differences divided by the mean of the measures) were calculated for each parameter.
Results
Image quality and point tracking
Figure 1 provides examples of the images acquired and analyzed for the study. All fifty examinations resulted in high-quality images that were acceptable for automatic quantitative image processing and clinical evaluation. Figure 1 also demonstrates the quality and accuracy of the automatic feature tracking software wherein expertly selected points at ED (Figure 1A) are seen to track the mitral valve annular motion during the cardiac cycle. Figure 2 shows the mitral annular model created from the mitral annular points in a long axis view (Figure 2A) and a short axis view at the level of the valves (Figure 2B) and demonstrates good agreement between the observed mitral annular positions in the images.
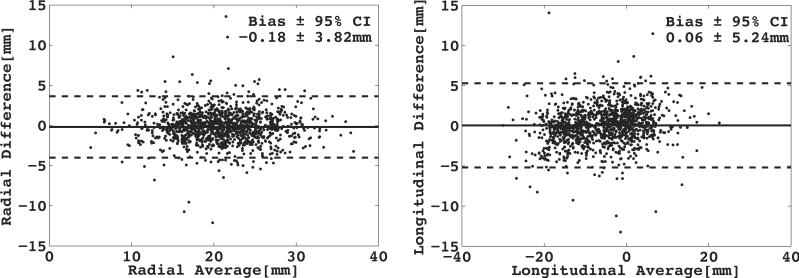
The results of Bland-Altman analysis are shown in Figure 4. Bland-Altman analysis of annular points chosen by an expert and those automatically identified by non-rigid registration software shows a bias of −0.2±1.9mm in the radial direction and 0.1±2.7mm in the longitudinal direction. Note, the limits of agreement (i.e. variance of the bias) are reported as the 95% confidence interval. The inter-observer coefficient of variation for the inter- and intra-observer comparison was 5–8% for all measured variables, except annular height (37%).
Figure 4.
Bland-Altman plots demonstrate the excellent agreement between expertly chosen and automatically tracked mitral annular points. The bias and limits of agreement (95% confidence intervals, CI) are shown for both the radial coordinate (left) and the longitudinal coordinate (right).
Effects of β-blocker treatment on LV function
As previously reported5, two-weeks of ß-blocker treatment resulted in significant chronotropic and inotropic effects; heart rate was decreased (65±10 vs 55±7 beats per minute, P<0.0001) and systolic blood pressure was decreased (138±18 vs 123±14 mmHg, P<0.0001). Furthermore, administration of ß-blockers resulted in significant increases in LVESV (81±21 vs 85±21 mL, P<0.01) and LVEDV (229±50 vs 235±48 mL, P<0.003) and a significant increase in forward stroke volume (89±21 vs 94±20 mL, P<0.03). LV ejection fraction and regurgitant volume did not change significantly.
Effects of β-blocker treatment on annular dimensions
Mitral annular dimensions at ED and ES are reported in the Table. At ED, annular area (16.6±3.3 vs 16.3±3.0mm2, P<0.19), annular perimeter (154.3±16.4 vs 152±13.9mm, P<0.13), SL (38.0±5mm vs 39.0±4.5mm, P<0.15) and annular height (9.8±3.8 vs 9.5±2.5mm, P<0.53) did not increase after two-week administration of ß-blockers. β-blocker administration did result in significant end diastolic decreases in CC (48.9 ± 4.6mm vs 47.2 ± 4.0mm P<0.01) and eccentricity (1.3 ± 0.2 vs 1.2 ± 0.1 P<0.01).
Table.
| Placebo | β-Blocker | Δ | P-value | ||
|---|---|---|---|---|---|
| End Diastole | Septal-Lateral [SL] (mm) | 38.0 ± 5.0 | 39.0 ± 4.5 | 1.0±3.2 | 0.15 |
| Commisure-Commisure [CC] (mm) | 48.9 ± 4.6 | 47.2 ± 4.0 | −1.7±3.2 | 0.01* | |
| Perimeter (mm) | 154.3 ± 16.4 | 152.0 ± 13.9 | −2.3±7.2 | 0.13 | |
| Area (cm) | 16.6 ± 3.3 | 16.3 ± 3.0 | −0.3±1.0 | 0.19 | |
| Annular Height (mm) | 9.8 ± 3.8 | 9.5 ± 2.5 | −0.3±3.5 | 0.53 | |
| Eccentricity (CC/SL) | 1.3 ± 0.2 | 1.2 ± 0.1 | −0.1±0.1 | 0.01* | |
| End Systole | Septal-Lateral [SL] (mm) | 41.5 ± 5.7 | 43.0 ± 5.3 | 1.5±3.1 | 0.03* |
| Commisure-Commisure [CC] (mm) | 47.5 ± 4.8 | 45.9 ± 5.2 | −1.6±4.3 | 0.08 | |
| Perimeter (mm) | 161.0 ± 19.3 | 156.8 ± 16.9 | −4.1±9.6 | 0.04* | |
| Area (cm) | 18.1 ± 3.7 | 17.5 ± 3.7 | −0.5±1.3 | 0.06 | |
| Annular Height (mm) | 11.5 ± 4.5 | 10.9 ± 3.0 | −0.6±4.3 | 0.33 | |
| Eccentricity (CC/SL) | 1.2 ± 0.1 | 1.1 ± 0.1 | −0.1±0.2 | 0.02* |
Mitral valve annular dimensions (mean±SD). The mean and standard deviation of each measure and the within-subject differences (Δ) are shown.
P≤0.05
At ES, ß-blockade conferred a significant decrease in annular perimeter (161.0±19.3 vs 156.8±16.9mm, P<0.04) and eccentricity (1.2±0.1 vs 1.1±0.1 P<0.02) relative to PL. The SL dimension significantly increased in BB at ES (41.5±5.7 vs 43.0±5.3mm, P<0.03). CC (47.5 ± 4.8 vs 45.9 ± 5.2, P<0.08), annular area (18.1 ± 3.7 vs 17.5 ± 3.7, P<0.06), and annular height (11.5 ± 4.5 vs 10.9 ± 3.0, P<0.33) also decreased at ES, but none were statistically significant.
The correlation coefficient (R) between the change in mitral annular SL and left ventricular SL diameter at end diastole was −0.61, whereas the correlation coefficient for end systole was −0.26. Correlation coefficients for the CC dimension were 0.33 and 0.02 for end diastole and end systole respectively. The correlation coefficient between each mitral annular geometric measure and mitral regurgitant volume per minute were all less than less than 0.5 or greater than −0.5 at both ED and ES. The correlation coefficient between the change in mitral regurgitant volume per minute and PL mitral regurgitant volume per minute was 0.71.
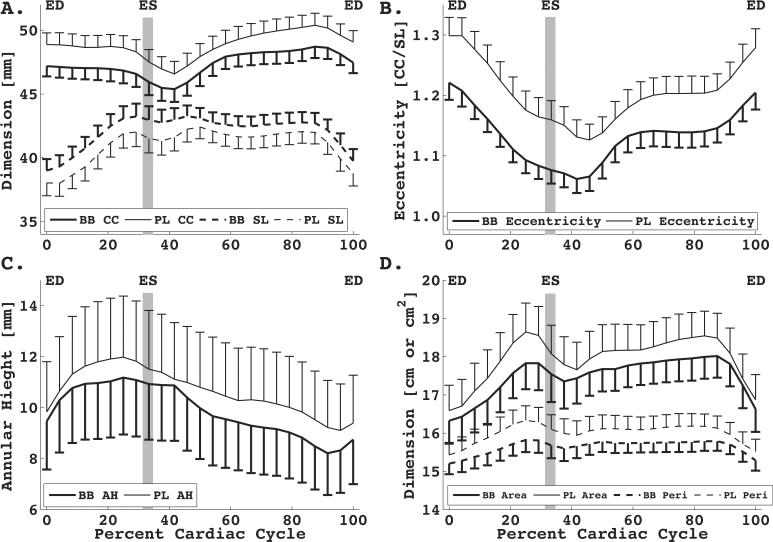
Effects of β-blocker treatment on annular dynamics
Figure 5 graphically depicts the effect of β-blockade on dynamic changes in annular dimensions throughout the cardiac cycle. SL is increased and CC is decreased for all time points for BB compared to PL (Figure 5A), which resulted in an overall decrease in eccentricity (CC/SL) for all cardiac phases (Figure 5B). Mitral annular height is decreased (Figure 5C), mitral annular perimeter is decreased (Figure 5D), and mitral annular area is decreased (Figure 5D) in BB compared to PL for all cardiac phases, but these differences were not statistically significant. A movie file depicting the mitral annular motion derived from the acquired data is available as an on-line supplement.
Figure 5.
Mitral valve annular dynamics in patients on placebo (PL) and β-blocker (BB) treatment during each phase of the cardiac cycle. In general, commisure-commisure (CC) dimensions and annular eccentricity, height, perimeter, and area significantly decreased or remained the same at each point in the cardiac cycle. The annular septal-lateral (SL) dimension was observed to increase. Data have been resampled to a standard systolic and diastolic interval across all patients to account for a range of heartrates. Errorbars (1 SD) are one-sided for clarity.
Discussion
In this study of asymptomatic or mildly symptomatic patients with moderate to severe primary mitral regurgitation of a myxomatous origin changes in mitral annular dimensions and dynamics with beta-blockers were evaluated from cardiac magnetic resonance images using a novel non-rigid registration automatic point-tracking procedure and a computer model of the annulus. Short-term treatment with ß-blockers reduced or preserved all mitral annular dimensions, except SL at ES. Increases in mitral annular dimensions may result in failure of the mitral valve leaflets to coapt completely leading to worsening of MR. Therefore treatment with a beta-blocker may preserve or reduce mitral annular dimensions, and this may improve long-term outcomes of patients with chronic moderate and severe MR8.
β-Blocker treatment effects on annular geometry
In this same patient cohort, Stewart et al.9 showed that ß-blocker treatment significantly increased LVEDV and LVESV, a finding which is corroborated by Nemoto et al.10 in a canine model of MR, which also included administration of ACE inhibitors. However, mitral annular dimensions in these patients remained the same or decreased, except SL at ES, with short-term β-blockade treatment. The absence of significant increases in CC, annular perimeter, annular area, and eccentricity upon ß-blocker treatment may indicate a favorable long-term result for these patients.
Chronic ischemic MR is characterized by increases in the SL dimension. In contrast in “pure” MR from a surgically created hole on the posterior mitral valve leaflet the primary change was increase in the CC dimension11. Increased annular flattening has also been associated with increased MR. However, Nguyen found no change in saddle shape geometry as measured by annular height, in their “pure” MR model11. In the current study, the decrease in CC with no change in annular height is consistent with reversing or preventing the pathologic changes seen in the “pure” MR model. β-blockers may therefore ameliorate or limit adverse remodeling of the annulus, which may be expected from volume overload as a consequence of MR alone.
In a canine model of chronic mitral regurgitation Young et al.12 used MRI to observe that the predominant mode of ventricular geometric remodeling was a shift of the septal wall away from the LV centroid into the right ventricle. Hence, increases in LVEDV in chronic MR lead to septal-lateral ventricular dilation. This predominant septal-lateral shift of the LV geometry may be exacerbated by ß-blockers, which increase LVEDV and, by coupling to the mitral annulus, result in SL annular dilation. Therefore, change in LV volumes may have a greater impact on the SL dimension compared to other annular dimensions.
The increase in LVEDV and LVESV in patients treated with ß-blockers in this study has been observed by others and is consistent with ß-blockade use10. The increases in SL at ES may arise from the observed increase in LVESV, but may not be sufficient to cause deleterious mitral annular remodeling, because mitral annular perimeter decreased, mitral annular area was unchanged and mitral regurgitation per minute decreased. However, further studies are needed to determine whether these short-term effects are maintained with long-term ß-blocker treatment.
Another explanation for the increase in SL dimension could be differential effect of ß-blockers on the fibrous and muscular annulus. The chronotropic and inotropic effects of ß-blockers should increase the muscular annular length with concomitant increases in the LVEDV, but may have a limited effect on the fibrous annulus, thereby tethering any potential increases in CC. Because the mitral annular perimeter is unchanged at ED and decreases at ES, the CC dimension is constrained to shorten while the SL dimension increases leading to a significant decrease in annular eccentricity. Changes in mitral annular SL dimension at the annular level as a consequence of ß-blocker treatment were moderately positive-correlated with SL dimensional changes of the LV at end diastole, but changes in SL at ES and changes in CC and ED and ES were not correlated. Decreases in mitral regurgitant volume per minute do not likely occur as a consequence of changes in mitral annular geometry, but rather as a consequence of inotropic and chronotropic effects. Lastly, a correlation was not established between mitral annular geometry and mitral regurgitant volume per minute. Note that patients with greater regurgitant volume per minute while on placebo exhibited greater decreases in mitral regurgitant volume per minute when on ß-blockers. Therefore, decreases in mitral regurgitant volume per minute likely occur as a consequence of inotropic and chronotropic effects, rather than remodeling of the mitral annulus and appear to have a larger effect on patients with greater mitral regurgitant volumes per minute.
Our findings indicate that decreases in eccentricity (CC/SL) may be the most sensitive indicator of changes to mitral annular geometry because of the consistent decrease at both ED and ES. Note that Mahmood et al.13 used three-dimensional echocardiography to measure changes in mitral annular circularity index (equivalent to the inverse of the annular eccentricity reported herein) as a consequence of valve repair using. From their results we can ascertain that mitral annular eccentricity increases from 1.0 to 1.2 in myoxmatous mitral valve disease after repair with a Carpentier-Edwards physio annuloplasty ring. Therefore, the ß-blocker induced changes in eccentricity are about half those induced by a surgical repair. A correlation between changes in eccentricity and mitral regurgitant volume per minute, however, could not be established. The benefit, if any, of a decrease in eccentricity to the patient remains to be established.
Mitral annular eccentricity values derived from the work of Nguyen et al in a chronic nonischemic MR sheep model increase at both ED and ES compared to their control group11. Hence, increases in eccentricity are associated with deleterious mitral annular remodeling. In our patient cohort, ß-blockers conferred a decrease in eccentricity at both ED and ES, which suggests a therapeutic benefit to the patients.
Currently, there are no published reports on how medical treatment with ß-blockers effects annular height measurements in humans. A decrease in annular height is generally associated with annular flattening and flattening perpetuates MR14, 15. In this study annular height did not change significantly with short-term ß-blocker treatment, but further studies are needed to evaluate longer-term effects.
β-Blocker treatment effects on annular dynamics
Using custom non-rigid registration automatic feature tracking software6, we computed annular dimensions throughout the cardiac cycle from expertly selected seed points at ED. As shown in Figure 5 the annular changes during all time points in the cardiac cycle were consistent with the quantitative analysis performed at ED and ES (Table). In general, commissure-commissure (CC) dimensions and annular eccentricity, height, perimeter, and area significantly decreased or remained the same at each point in the cardiac cycle. The annular septal-lateral (SL) dimension was observed to increase. The mean curves in ß-blocker treated patients for each measure of annular dynamics remain consistently below the respective curves for the placebo treated patients, whereas the dynamic measures of SL are consistently increased on ß-blocker compared to placebo. At no point in the cardiac cycle do the mean curves cross for any measure.
Quantitative image analysis
Image quality was suitable for automatic tracking of mitral annular points using custom non-rigid registration software. The software reduced the time spent quantitatively analyzing images by significantly reducing the need for user input, while maintaining sufficient accuracy for quantitative comparisons. On average, the difference between mitral annular points chosen by an expert and those defined by the tracking software was less than a tenth of a millimeter, thereby resulting in sub-pixel agreement. The automatic tracking software does not appear to significantly bias the location of the mitral valve annulus when compared to expertly chosen points. Furthermore, the coefficients of variation for intra- and inter-observer comparisons were low, except for annular height.
The recent advent of three-dimensional echocardiography makes available another means for studying the mitral valve, both transesophageal16 and transthoracic17 echocardiography looks promising. The MRI method reported herein for acquiring quantitative measures of mitral annular dimensions and dynamics, however, has the advantage of automated frame-to-frame point tracking, higher temporal resolution, and no required tranesophageal probe, when compared to three-dimensional echocardiography.
Limitations
This study evaluated the effects of 2 weeks of treatment with ß-blockers on the mitral annulus, but LV remodeling usually occurs over several months. Therefore longer-term studies are needed to confirm whether the observed effects of β-blocker treatment on mitral annular dimensions persist over time. In addition the mitral valve annulus may remodel with a different time course and to a different degree than the ventricular myocardium. Furthermore, the patient's response to ß-blockers may be different based on the severity and/or etiology of MR. This study, however, is too small to allow reliable sub-group analysis. Long-term studies are also needed to determine the clinical significance of the observed changes in mitral annular geometry and their influence on long-term clinical outcomes. Lastly, examining mitral annular dimensions and dynamics subsequent to the cessation of the ß-blocker regiment would confirm whether or not the measures returned to baseline.
Conclusions
Short-term β-blocker treatment in patients with moderate to severe mitral regurgitation reduced or preserved all mitral annular dimensions, except SL at ES, even though LVEDV and LVESV increased. This favorable effect of β-blockade on mitral annular dimensions, if maintained with long-term treatment, combined with negative inotropic and chronotropic effects may reduce the progression of chronic mitral regurgitation.
Supplementary Material
Acknowledgments
Sources of Funding The authors gratefully acknowledge research support from NIH/NHLBI Grant K99-R00 HL-087614 (to D.B.E.), grants from the Auckland Medical Research Foundation, and the Green Lane Research and Education Trust, Auckland, New Zealand.
Footnotes
Disclosures None.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Jr., Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT, O'Rourke RA, Otto CM, Shah PM, Shanewise JS. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e1–142. doi: 10.1016/j.jacc.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Enriquez-Sarano M, Thoralf MS. Early Surgery Is Recommended for Mitral Regurgitation. Circulation. 2010;121:804–812. doi: 10.1161/CIRCULATIONAHA.109.868083. [DOI] [PubMed] [Google Scholar]
- 3.Gillam LD, Schwartz A. Is early surgery recommended for mitral regurgitation? Circulation. 2010;121:813–821. doi: 10.1161/CIRCULATIONAHA.109.868083. [DOI] [PubMed] [Google Scholar]
- 4.Westenberg JJ, van der Geest RJ, Lamb HJ, Versteegh MI, Braun J, Doornbos J, de Roos A, van der Wall EE, Dion RA, Reiber JH, Bax JJ. MRI to evaluate left atrial and ventricular reverse remodeling after restrictive mitral annuloplasty in dilated cardiomyopathy. Circulation. 2005;112(9 Suppl):I437–442. doi: 10.1161/CIRCULATIONAHA.104.525659. [DOI] [PubMed] [Google Scholar]
- 5.Stewart RA, Raffel OC, Kerr AJ, Gabriel R, Zeng I, Young AA, Cowan BR. Pilot study to assess the influence of beta-blockade on mitral regurgitant volume and left ventricular work in degenerative mitral valve disease. Circulation. 2008;118:1041–1046. doi: 10.1161/CIRCULATIONAHA.108.770438. [DOI] [PubMed] [Google Scholar]
- 6.Li B, Young AA, Cowan BR. GPU accelerated non-rigid registration for the evaluation of cardiac function. Med Image Comput Comput Assist Interv Int Conf Med Image Comput Comput Assist Interv. 2008;11(Pt 2):880–887. doi: 10.1007/978-3-540-85990-1_106. [DOI] [PubMed] [Google Scholar]
- 7.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 8.Varadarajan P, Joshi N, Appel D, Duvvuri L, Pai RG. Effect of Beta-blocker therapy on survival in patients with severe mitral regurgitation and normal left ventricular ejection fraction. Am J Cardiol. 2008;102:611–615. doi: 10.1016/j.amjcard.2008.04.029. [DOI] [PubMed] [Google Scholar]
- 9.Stewart RA, Raffel OC, Kerr AJ, Gabriel R, Zeng I, Young AA, Cowan BR. Pilot Study to Assess the Influence of ß-Blockade on Mitral Regurgitant Volume and Left Ventricular Work in Degenerative Mitral Valve Disease. Circulation. 2008;118:1041–1046. doi: 10.1161/CIRCULATIONAHA.108.770438. [DOI] [PubMed] [Google Scholar]
- 10.Nemoto S, Hamawaki M, De Freitas G, Carabello BA. Differential effects of the angiotensin-converting enzyme inhibitor lisinopril versus the beta-adrenergic receptor blocker atenolol on hemodynamics and left ventricular contractile function in experimental mitral regurgitation. J Am Coll Cardiol. 2002;40:149–154. doi: 10.1016/s0735-1097(02)01926-5. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen TC, Itoh A, Carlhall CJ, Bothe W, Timek TA, Ennis DB, Oakes RA, Liang D, Daughters GT, Ingels NB, Jr., Miller DC. The effect of pure mitral regurgitation on mitral annular geometry and three-dimensional saddle shape. J Thorac Cardiovasc Surg. 2008;136:557–565. doi: 10.1016/j.jtcvs.2007.12.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young AA, Orr R, Smaill BH, Dell'Italia LJ. Three-dimensional changes in left and right ventricular geometry in chronic mitral regurgitation. Am J Physiol. 1996;271(6 Pt 2):H2689–2700. doi: 10.1152/ajpheart.1996.271.6.H2689. [DOI] [PubMed] [Google Scholar]
- 13.Mahmood F, Subramaniam B, Gorman JH, 3rd, Levine RM, Gorman RC, Maslow A, Panzica PJ, Hagberg RM, Karthik S, Khabbaz KR. Three-dimensional echocardiographic assessment of changes in mitral valve geometry after valve repair. Ann Thorac Surg. 2009;88:1838–1844. doi: 10.1016/j.athoracsur.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tibayan FA, Rodriguez F, Langer F, Zasio MK, Bailey L, Liang D, Daughters GT, Ingels NB, Jr., Miller DC. Annular remodeling in chronic ischemic mitral regurgitation: ring selection implications. Ann Thorac Surg. 2003;76:1549–1554. doi: 10.1016/s0003-4975(03)00880-4. discussion 1554–1545. [DOI] [PubMed] [Google Scholar]
- 15.Gorman JH, 3rd, Jackson BM, Enomoto Y, Gorman RC. The effect of regional ischemia on mitral valve annular saddle shape. Ann Thorac Surg. 2004;77:544–548. doi: 10.1016/S0003-4975(03)01354-7. [DOI] [PubMed] [Google Scholar]
- 16.Grewal J, Suri R, Mankad S, Tanaka A, Mahoney DW, Schaff HV, Miller FA, Enriquez-Sarano M. Mitral annular dynamics in myxomatous valve disease: new insights with real-time 3-dimensional echocardiography. Circulation. 2010;121:1423–1431. doi: 10.1161/CIRCULATIONAHA.109.901181. [DOI] [PubMed] [Google Scholar]
- 17.Daimon M, Saracino G, Gillinov AM, Koyama Y, Fukuda S, Kwan J, Song JM, Kongsaerepong V, Agler DA, Thomas JD, Shiota T. Local dysfunction and asymmetrical deformation of mitral annular geometry in ischemic mitral regurgitation: a novel computerized 3D echocardiographic analysis. Echocardiography. 2008;25:414–423. doi: 10.1111/j.1540-8175.2007.00600.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.