Abstract
Background. The 2009 influenza A(H1N1) pandemic called attention to the limited influenza treatment options available, especially in individuals at high risk of severe disease. Neuraminidase inhibitor–resistant seasonal H1N1 viruses have demonstrated the ability to transmit well despite early data indicating that resistance reduces viral fitness. 2009 H1N1 pandemic viruses have sporadically appeared containing resistance to neuraminidase inhibitors and the adamantanes, but the ability of these viruses to replicate, transmit, and cause disease in mammalian hosts has not been fully characterized.
Methods. Two pretreatment wild-type viruses and 2 posttreatment multidrug-resistant viruses containing the neuraminidase H275Y mutation collected from immunocompromised patients infected with pandemic influenza H1N1 were tested for viral fitness, pathogenicity, and transmissibility in ferrets.
Results. The pretreatment wild-type viruses and posttreatment resistant viruses containing the H275Y mutation all demonstrated significant pathogenicity and equivalent viral fitness and transmissibility.
Conclusions. The admantane-resistant 2009 pandemic influenza A(H1N1) virus can develop the H275Y change in the neuraminidase gene conferring resistance to both oseltamivir and peramivir without any loss in fitness, transmissibility, or pathogenicity. This suggests that the dissemination of widespread multidrug resistance similar to neuraminidase inhibitor resistance in seasonal H1N1 is a significant threat.
Influenza A viruses are significant human pathogens, both in their sporadic pandemic and endemic (seasonal) forms. Antiviral therapies are commonly used to treat both severe illness in high-risk patients and self-limited influenza infection. Widespread emergence of antiviral resistance among seasonal influenza A viruses began during the 2004–2005 influenza season, when a significant increase in the prevalence of adamantane resistance among H3N2 influenza viruses was observed [1, 2]. In most cases, a single amino acid substitution in the M2 protein (S31N) was responsible for this resistance, having no effect on viral fitness [3, 4]. During the subsequent season in 2005–2006, H3N2 adamantane resistance surpassed 90%, rendering this class of drugs ineffective as a viable treatment for seasonal H3N2 influenza infections [3].
By the time H3N2 adamantane resistance became prominent, a shift in practice was already occurring for a number of reasons, and despite seasonal H1N1 strains remaining adamantane susceptible, use of these drugs decreased and the neuraminidase inhibitors (NAIs), particularly oseltamivir, became the primary influenza antiviral of choice. Widespread resistance to oseltamivir was deemed unlikely because NAIs closely resemble the sialic acids that are the natural substrates for the neuraminidase's active site [5], and that any mutation leading to resistance was expected to lead to reduced fitness of the virus [6, 7].
When NAI resistance mutations were first identified through both in vitro selection under drug pressure and during oseltamivir treatment of experimentally infected individuals [8–10], the neuraminidase (NA) changes at position 275, 292, and 119 identified in H3N2 and H1N1 viruses led to a significant reduction in the ability of the viruses to replicate and transmit in animal models [7, 9, 11, 12]. This correlated well with the low incidence of NAI resistance of 0.32% in the adult population observed during 2005–2006, when most circulating seasonal viruses retained susceptibility to oseltamivir [6].
During 2007–2009, the unexpected emergence of a dominant clade of oseltamivir-resistant seasonal H1N1 virus demonstrated that NAI resistance could occur in the context of an otherwise fit and transmissible virus. By the end of the 2008–2009 influenza season, ∼98% of seasonal H1N1 isolates worldwide exhibited resistance to oseltamivir [13]. Recent studies have identified permissive changes in the NA of seasonal H1N1 that might account for the widespread circulation of oseltamivir-resistant strains [14].
Over the past 4 years, a smaller number of NAI-resistant H3N2 viruses have been identified, some containing the H274Y change (equivalent mutation in N2 subtype NA) or other newly identified NA amino acid changes. In animal models, these resistant H3N2 viruses demonstrated equivalent fitness and transmissibility to wild-type viruses, suggesting that widespread seasonal H3N2 NAI resistance is also a threat [15–17].
Recently, the 2009 pandemic H1N1 influenza virus emerged in Mexico and the southwestern United States [18, 19] and rapidly spread worldwide, causing increased morbidity and mortality among children and young adults throughout most of 2009 and early 2010. Similar to seasonal H3N2 viruses, the 2009 pandemic viruses are resistant to the adamantanes [20], making NAIs the drug class of choice. The concern for increased levels of severe disease and need for a parenteral therapy for patients unable to achieve adequate NAI levels orally or via inhalation prompted the US Food and Drug Administration (FDA) to release a new parenteral NAI, peramivir, on an emergency use authorization for treatment of severe pandemic H1N1 infections.
After only a few months into the pandemic, reports of sporadic NAI resistance emerged, leading to the possibility of a virus with limited susceptibility to available antivirals transmitting in the community [21–23]. Recently, we isolated 2 adamantine-resistant pandemic H1N1 viruses from 2 different immunocompromised patients and found that, after a period of 9–14 days of NAI treatment, the viruses from these patients independently acquired the NA H275Y mutation [23]. We further demonstrated that the H275Y change in these pandemic H1N1 viruses conferred resistance not only to oseltamivir, but also to peramivir, suggesting that for those at risk of severe disease with NAI resistant infections, intravenous peramivir may not be an adequate treatment option.
In this report, we characterized the multidrug-resistant pandemic influenza A(H1N1) viruses isolated from the 2 individuals described previously [23], to determine how great a potential exists for widespread multidrug antiviral resistance and transmissibility. We examined their viral genomes for other significant amino acid substitutions and then evaluated the virulence, fitness, and transmissibility in a mammalian host with use of a ferret transmission model.
METHODS
Viruses
Viral isolates were collected from patients in an institutional review board–approved protocol (clinicaltrials.gov identifier: NCT00533182). and the patients from which these viruses were isolated have been previously described [23]. The initial isolates from each patient are A/Bethesda/NIH107-D0/2009, referred to here as virus A, and A/Bethesda/NIH106-D0/2009, referred to here as virus B, corresponding to patient A and B in the previous report. We selected the NAI-resistant isolate from each patient [23] A/Bethesda/NIH107-D31/2009 and A/Bethesda/NIH106-D14/2009, referred to here as virus Ar and virus Br, respectively. All 4 viruses were passed twice in MDCK cells.
Ferrets
Thirty-two influenza A virus–seronegative, 4-month-old, male ferrets were housed in pairs in separate cages with individual airflow. The ferrets were divided into 8 groups of 4 ferrets each. Four groups were inoculated intranasally with 105 plaque-forming units (pfu) of virus, 1 group each with each original virus (virus A and virus B), and 1 group each with the H275Y-containing mutants (virus Ar and virus Br). After 48 h, the other 4 groups were placed in contact with the inoculated ferrets by placing 2 naive ferrets in each cage with 2 inoculated ferrets. Daily weights, temperatures, nasal washes, and clinical scores were performed, as previously described [17].
Two ferrets from each of the inoculated groups were euthanized on day 4 after inoculation and on day 6 after inoculation (day 4 after exposure), 2 from each of the transmission groups were euthanized. On day 14 after inoculation (day 12 after exposure), all remaining animals were euthanized. Whole lungs, trachea, tracheobronchial lymph nodes, rostral nasal turbinates, and spleen were harvested. All animal experiments were performed following National Institutes of Health Institutional Animal Care and Use Committee–approved protocols and guidelines.
Quantification of Virus
Quantification of viral shedding in nasal washes was determined using 1-step real-time reverse-transcription polymerase chain reaction (RT-PCR) for the influenza A virus matrix 1 gene, as previously described [24]. Amplification and sequencing of the NA gene was performed on each viral isolate recovered to determine if the NA gene sequence remained stable after infection and transmission.
Lung tissues were weighed and homogenized in sterile cold Leibovitz's medium (Gibco l-15, Invitrogen) containing 1X penicillin, streptomycin, and amphotericin B (Gibco Anti–Anti, Invitrogen). Standard plaque assays were performed [25]. Titers are expressed as pfu per gram of tissue.
Sequence Analysis
RT-PCR and sequencing was performed on the primary viral isolates, as previously described [26]. Full-length sequences of each gene segment of the 4 viruses used to inoculate the ferrets were generated and deposited into GenBank (accession numbers HQ263267-HQ263294, GU571152–GU571156). The hemagglutinin (HA) and NA genes were amplified and sequenced from virus isolated from the ferret nasal washes. These sequences were compared with the sequences generated from the viral isolates used for inoculation.
Histopathological Analysis
Standard hematoxylin-and-eosin stains were performed for all tissues, and Brown and Hopps tissue Gram stain was applied to select sections. Immunohistochemistry was performed on all sections from ferrets euthanized on day 4, as previously described [27].
RESULTS
Full Viral Genome Analysis
All 4 viruses used for inoculation were sequenced, and amino acid sequences of the deduced open reading frames were aligned. The wild-type viruses, A and B, differed in 4 of the gene segments by 8 amino acids (Table 1). Virus A and NAI resistant virus Ar differed only by 2 nonsynonymous changes, coding for an H275Y mutation in NA and an L95I mutation in NS1. Viruses B and Br differed by 3 nonsynonymous changes, coding for A15T and F432L mutations in HA, and the H275Y mutation in NA (Table 1). HA and NA gene sequences of viruses isolated from the ferret nasal washes contained sequences identical to those of the inoculating viruses.
Table 1.
Amino acids differing between virus A and B and changes observed between wild-type and resistant viruses.
| Changes between the 2 wild-type viruses | |||
| Gene | Position | Virus A | Virus B |
| PB1 | 537 | S | N |
| 563 | K | R | |
| PA | 14 | V | I |
| 716 | K | Q | |
| HA | 114 | N | D |
| NP | 194 | V | I |
| 270 | V | I | |
| 444 | V | I | |
| Changes between the wild-type and resistant viruses | |||
| Virus A to Ar | NS | L95I | |
| NA | H275Y | ||
| Virus B to Br | HA | A15T, F432L | |
| NA | H275Y | ||
NOTE. Eight amino acid differences were observed between the 2 wild-type viruses, demonstrating that the viruses isolated from the 2 patients were not identical at baseline. The only shared mutation selected for under drug pressure between the resistant viral isolates was the NA H275Y mutation.
Clinical Disease and Transmission
All ferrets inoculated with virus showed signs of clinical disease and weight loss 2 days after inoculation. Viruses A and Ar caused similar mean weight loss of 5%–10% (Figure 1A) and a mean clinical score of 1, with duration of clinical symptoms of 6–7 days (Figure 2A). Viruses B and Br caused a similar mean weight loss of 6% on day 2 and 6%–7% by the end of the study, but B demonstrated increased weight loss of 13% during the study (Figure 1B). Virus B and Br also showed no statistically significant difference in clinical score in the inoculated animals, with a mean score near 2 and duration of clinical symptoms of 7–10 days (Figure 2B).
Figure 1.
Mean percentage weight loss from baseline after inoculation (Inoc) and contact transmission (Contact) of viruses in ferrets. All ferrets demonstrated significant weight loss from baseline after inoculation or contact transmission. Error bars represent standard error of the mean.
Figure 2.
Mean clinical score of ferrets in each group after inoculation (Inoc) and contact transmission (Contact). All ferrets demonstrated clinical illness, but those infected by contact transmission had higher clinical scores during the duration of illness, but similar duration of illness to those in the inoculation group. No statistically significant difference was seen between wild-type and resistant viruses. Error bars represent standard error of the mean.
All ferrets in each of the 4 contact transmission groups demonstrated clinical illness. The wild-type and resistant virus, viruses A and Ar, demonstrated similar mean peak weight loss of 10%–11% (Figure 1A). Clinical symptoms began 2 days after contact with infected animals, and duration of symptoms in both groups was >10 days. The clinical scores in both groups were similar until day 9, shortly after 1 ferret in the resistant virus group was found dead on day 6. Although the ferrets in the wild-type group exhibited a higher mean peak clinical score during days 9–14, no deaths occurred in this group (Figure 2A).
Virus B and Br demonstrated nearly equivalent clinical scores, slightly higher than those seen with virus A and Ar, and similar in duration of disease (Figure 2B). Weight loss in both groups was also equivalent until day 9, after which virus B demonstrated increased weight loss including an animal found dead on day 12 (Figure 1B).
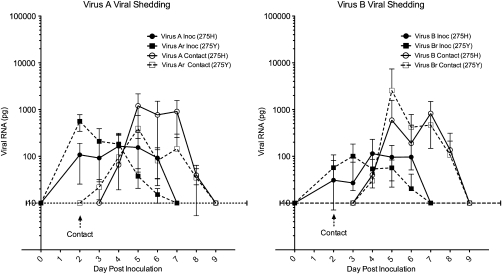
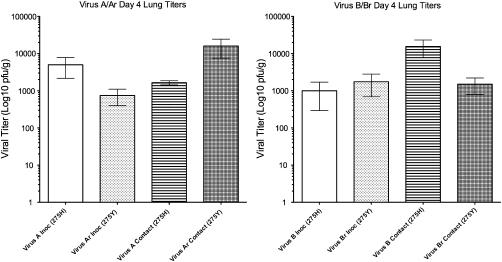
Viral Shedding and Lung Titers
No difference was observed between the wild-type and resistant viruses in initiation or duration of shedding in the inoculated groups. All ferrets inoculated with either the wild-type or resistant viruses demonstrated active viral shedding by day 2, and viral RNA was detectable for ∼5 days (Figure 3). Similar amounts of viral RNA were detected in the nasal washes of both the wild-type and resistant virus groups. Likewise, day 4 viral titers of lung tissue were equivalent in all 4 virus groups, reaching mean peak titers of 102–103pfu/g of tissue (Figure 4). No virus was isolated from the lungs harvested on day 14.
Figure 3.
Mean quantity of viral RNA detected by quantitative polymerase chian reaction in the nasal washes of ferrets after inoculation (Inoc) and contact transmission (Contact). All ferrets in all groups shed virus, and significant amounts of viral RNA was detectable. Shedding was similar between resistant and wild-type viruses. Quanitity of viral RNA reported in picograms (pg) [24]. Dotted line represents lower limit of detection of 10pg. Error bars represent standard error of the mean.
Figure 4.
Mean viral titer isolated from the lungs of ferrets infected by inoculation (Inoc) and contact transmission (Contact). All animals euthanized on day 4 after exposure had significant growth of influenza A from the lungs. No growth of influenza A was detected from those lungs harvested on day 14. On day 4, no statistically significant difference was observed between inoculated A and Ar (P = .165) or B and Br (P = .492). Similarly, contact acquired A and Ar (P = .193) and B and Br (P = .127) also demonstrated no significant difference in lung titer. Titers expressed as plaque forming units per gram of tissue (pfu/g). Error bars represent standard error of the mean.
In the animals infected by transmission, both wild-type and resistant virus groups for all viruses demonstrated detectable viral RNA in nasal washes 48 h after contact for a duration of 6 days. Similar amounts of viral RNA, 102–103pg, were detected in each virus group with the highest amount of viral RNA detected from those animals exposed to virus Br (Figure 3). As with their inoculated peers, day 4 viral titers of lung tissue were equivalent in all 4 virus groups, reaching titers of 102–103pfu/g of tissue. No virus was isolated from the lungs harvested on day 14.
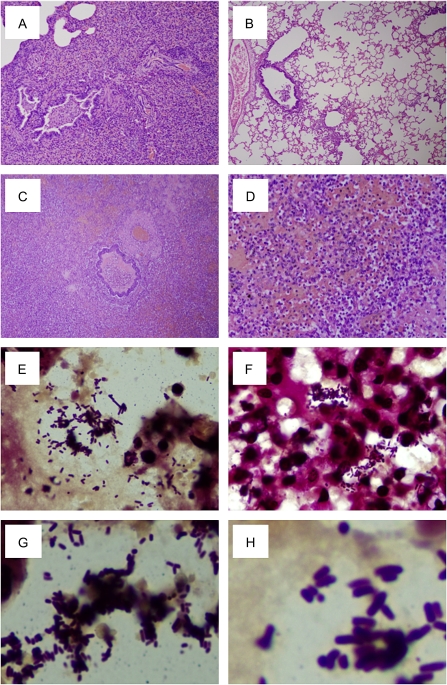
Pathology
There were no discernible differences in gross pathology attributable to specific viruses or route of viral inoculation. Gross examination of the lungs varied in each ferret from no obvious gross pathology to occasionally severe, multifocal, bronchocentric, firm tan foci often accompanied by diffuse mild to moderate congestion. Tracheobronchial lymph nodes were enlarged and firm but normal in appearance on cut section. Examination of the upper respiratory tract revealed no gross findings except variable amounts of mucus within the nasal cavity or proximal trachea. Grossly all other organs were within normal limits except for the animal that was found dead on day 12. This animal was found to have a hemothorax, and its lungs were dark red with tan foci and partially atelectatic.
Histopathological analysis of ferrets euthanized on day 4 and 14 demonstrated no significant differences between ferret groups attributable to a specific virus or route of inoculation. On day 4, some ferrets showed a mild neutrophilic and lymphocytic sinusitis with some submucosal gland involvement [Figure 5 A], and all ferrets had a mild to moderate, multifocal, neutrophilic, and lymphohistiocytic laryngitis and sialadenitis, with similar inflammation in the overlying epithelium [Figure 5 C]. A distal tracheitis was observed, and in some animals, similar changes extended throughout the entire trachea, with occasional foci of ulceration in the tracheal epithelium [Figure 5 E, G].
Figure 5.
Histopathology and immunohistochemistry of 2009 pandemic H1N1 influenza A virus–infected ferret respiratory tissue. Representative photomicrographs of hematoxylin-and-eosin-stained tissue sections and immunohistochemically-stained sections to detect influenza viral antigen from ferrets infected with wild-type or NAI resistant viruses at 4 days after inoculation or exposure by contact transmission. No statistically significant differences in the range of histopathology were observed between the ferrets inoculated with the 4 different viruses or between them and the contact ferrets in each group. Viral antigen is stained brown on a hematoxylin-stained background. A and B, Nasal cavity showing mild acute inflammation of the squamous epithelium and underlying submucosal glands, both of which show influenza viral antigen (virus B contact ferret; original magnification 100×). C and D, Acute laryngitis with an acute, necrotizing inflammation of the respiratory epithelium, and acute sialadenitis of the submucosal glands. Influenza viral antigen is prominent in the acinar cells of the submucosal glands (virus B inoculated ferret; original magnification 200×). E–I, Acute tracheitis and sialadentis of the proximal trachea. Acute necrotizing inflammation of the respiratory epithelium and acute sialadenitis of the submucosal glands was seen multifocally in the proximal trachea. Abundant viral antigen is seen in submucosal glands (virus Br contact ferret) (E, F), the respiratory epithelium (H), and in residual basal cells and submucosal glands in an area of epithelial necrosis (virus Ar contact ferret) (G, I) (original magnification 100× [E, F, G, I] and 400× [H]). J–R, Acute viral pneumonia with multifocal bronchiolitis and associated alveolitis. Acute often necrotizing bronchiolitis (J, K), with luminal necrotic debris (K) showed abundant viral antigen in the respiratory epithelium (virus B inoculated ferret; L) or (virus B contact ferret; M). Multifocal to coalescing acute alveolitis was seen involving alveolar ducts (N, O) and alveoli (P–R). A mixed inflammatory cell infiltrate was observed with neutrophils, macrophages, and lymphocytes (P). Influenza viral antigen was observed in the epithelial cells lining the alveolar duct (O) and in type I (Q) and type II alveolar epithelial cells and alveolar macrophages (virus B contact ferret) (R) (original magnification 40× [J], 100× [K, L], 200× [N, O], 400× [P], and 1000× [M, Q, R]).
Immunohistochemistry of the rostral nasal cavity, larynx, and trachea of animals euthanized on day 4 revealed influenza viral antigen labeling in the acinar cells of the submucosal glands and in pseudostratified respiratory epithelium, most frequently in goblet cells, but also in the squamous epithelium of the nasal cavity [Figure 5 B, D, F, H–I]. There was also significant labeling of esophageal submucosal glands, although no inflammation of these glands was observed.
An acute bronchointerstitial pneumonia was present in peripheral and medial sections of the right lung lobes of all ferrets euthanized at day 4. This was characterized by diffuse, occasionally severe, lymphohistiocytic necrotizing bronchiolitis accompanied by multifocal, coalescing lymphohistiocytic and neutrophilic alveolitis with multifocal type II pneumocyte hyperplasia [Figure 5 J–K, N, P]. Similar inflammation was also seen in bronchi. Lymphoplasmacytic aggregates were common both perivascularly and peribronchially and were seen scattered subpleural and in the pulmonary parenchyma. Influenza viral antigen distribution in the lungs was in both the epithelium and submucosal glands of the bronchi and bronchioles and was present in alveolar duct epithelium, type I and type II alveolar epithelial cells, and alveolar macrophages [Figure 5 L–M, O, Q–R]. The degree and distribution of labeling correlated closely with the degree of inflammation. Histopathology of the enlarged tracheobronchial lymph nodes revealed a pattern consistent with reactive lymph nodes.
In the animals euthanized on day 14, the typical histopathologic pattern seen was an upper respiratory tract in normal limits and a resolving bronchointerstitial pneumonia characterized by mild, multifocal, lymphohistiocytic bronchiolitis with occasional extension of this inflammation in adjacent alveolar ducts and alveoli [Figure 6 A]. In addition, scattered foci of interstitial fibrosis were located adjacent to bronchi and bronchioles, intrapulmonary parenchymal lymphoplasmacytic aggregates, and mild to moderate congestion and edema. One ferret euthanized at day 14 had a focus of bronchiolitis obliterans with organizing pneumonia characterized by replacement of alveolar architecture by fibrosis [Figure 6 B], as previously described in ferrets infected with a classical swine influenza virus [27].
Figure 6.
Histopathology and immunohistochemistry of 2009 pandemic influenza A(H1N1) virus–infected ferret respiratory tissue. Representative photomicrographs of hematoxylin-and-eosin-stained tissue sections and Brown and Hopps tissue Gram-stained sections to detect bacteria from ferrets infected with wild-type or NAI resistant viruses at 14 days after inoculation or 12 days after exposure of the contact animals. A and B, Chronic changes observed in recovering animals included occasional examples of bronchiolitis obliterans with organizing pneumonia (A) and residual chronic active bronchiolitis and focal, mild alveolitis (B) (virus B inoculated ferret); original magnification 40×). One ferret found dead 12 days after exposure by contact transmission with virus B demonstrated pathology consistent with an acute bacterial pneumonia with destruction of the pulmonary architecture and a massive inflammatory infiltrate consisting predominantly of neutrophils (C, D) (original magnification 40× [A], 200× [B]). (E–H) Tissue Gram stain revealed abundant Gram-positive short rods, morphologically consistent with Listeria monocytogenes(original magnification 1000×).
The animal that died on day 6 had no notable histopathologic changes other than those seen in the animals that survived, and no specific cause of death was determined. Histopathologic analysis of the animal that died with a hemothorax on day 12 revealed coalescing hemorrhage and edema and acute, suppurative bronchopneumonia that obliterated the underlying pulmonary architecture [Figure 6 C–D]. These changes overlaid the viral pneumonia pattern already described in the day 4 ferrets. Bronchopneumonia were present in myriads of gram-positive short bacilli, morphologically consistent with Listeria monocytogenes [Figure 6 E–H].
DISCUSSION
This study illustrates that naturally occurring NAI-resistant pandemic H1N1 influenza mutants retain replicative fitness, transmissibility, and virulence in the ferret model. These multidrug-resistant viruses isolated after just 9–14 days of NAI therapy from immunocompromised patients are resistant to the adamantanes, oseltamivir, and peramivir and maintain their ability to cause significant disease in a relevant animal model.
An analysis of the full genome of these viruses demonstrates that amino acid changes can be selected for rapidly in multiple genes of the virus during a single infection, occurring rapidly in the 2 cases described [23]. Viruses A and B differed at 8 amino acid positions in their genome when first isolated, but most were previously reported polymorphisms seen in 2009 pandemic H1N1 influenza viruses. After a short period of NAI treatment of the host, both viruses isolated, virus Ar and Br, contained the NA H275Y change as the dominant genotype.
It is unclear whether the small number of other changes that were seen in each virus after selection under drug pressure play any role in the maintenance of virulence and transmissibility. The H275Y change was the only common change observed under drug pressure. The H275Y change was maintained during the infection and transmission experiment, with no other amino acid changes or reversion occurring, demonstrating that the H275Y was stable even without drug pressure. This strongly suggests that these pandemic H1N1 viruses were able to accommodate the single H275Y change conferring multi-NAI resistance without requiring any other NA changes to maintain virulence and transmissibility, unlike recent oseltamivir-resistant seasonal H1N1 influenza viruses [14].
The clinical disease caused by both resistant viruses containing the H275Y was similar to that induced by the initial wild-type isolates. In the case of viruses A and Ar, slightly more severe disease was noted in the resistant virus-infected groups characterized by higher weight loss and 1 spontaneous death, but clinical score and duration of symptoms were very similar and, in some cases, were slightly lower than those in the wild-type groups. The opposite was noted with virus B and Br, with more weight loss and 1 death occurring in the wild-type infected groups, but duration of symptoms and clinical scores generally higher in the resistant virus–infected groups. These data demonstrate that no single measure can easily describe the extent of clinical disease, suggesting that a summation of data including weight loss, duration of illness, clinical score, and pathological changes more accurately reflects the overall disease in these animals. With this in mind, it is clear that despite the small differences described, the overall clinical disease caused by each of the resistant and wild-type viruses in this study is similar.
We noted nearly identical duration of shedding between wild-type and resistant virus groups and no significant difference in amounts of viral RNA detected at each time point. The quantity of virus isolated from the lungs on day 4 was also similar between groups, demonstrating that the resistant viruses maintain their ability to replicate in both the upper and the lower respiratory tract. A difference was seen between those ferrets inoculated intranasally and those who contracted influenza by transmission. In the latter groups, a higher level of viral RNA was detected in nasal washes, and both deaths occurred in these groups of animals. However, no difference was seen in the overall mean lung titers and duration of illness.
All viruses tested in this study caused similar quality and quantity of pathology, and a significant amount of pathology was observed both in the upper and lower respiratory tract. Influenza viral antigen was detected throughout the respiratory tract, and disease was documented from the nasal cavity to the alveoli, again demonstrating the ability of both the wild-type and the resistant viruses to cause significant upper and lower respiratory tract disease.
The finding of bacteria in the lungs of the animal infected by contact transmission with virus Br that died on day 12 is interesting. This animal exhibited pathology consistent with a secondary bacterial pneumonia and hemothorax superimposed on the viral pathology pattern seen in the other ferrets. Studies of autopsies of victims of the 1918 influenza pandemic demonstrated that >95% of individuals who died did so with a secondary bacterial pneumonia [28]. Autopsy reports from the current H1N1 pandemic also confirm the significant role that secondary bacterial pneumonias play in deaths due to pandemic influenza A [29]. The majority of these secondary bacterial infections both today and during past pandemics are with bacterial species that commonly colonize the human upper respiratory tract, such as Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus. The gram-positive bacteria that caused pneumonia in this ferret are consistent morphologically with Listeria monocytogenes, a known colonizer of ferrets that has been shown to cause secondary pulmonary disease when ferrets are infected with canine distemper virus [30]. This observation and the death of this ferret serve to reinforce the importance that a secondary bacterial pathogen can play in a significant underlying viral infection, in this case leading to mortality.
If we consider the duration of infection and shedding in the immunocompromised human hosts together with the clear transmission and pathogenesis of these viruses in the ferret model, the data demonstrate that pandemic H1N1 viruses can accommodate the NA H275Y mutation without attenuation or loss of transmissibility. This suggests that the selection for resistance to oseltamivir and peramivir can occur quickly and efficiently, and may be able to spread effectively in the population. The significant upper and lower respiratory tract pathology observed demonstrates that the rapid selection for multidrug resistance has no effect on the ability of the virus to replicate and cause disease and that, in the presence of a secondary bacterial pathogen, can lead to a fatal outcome.
These findings reinforce the significance of drug-resistant influenza A viruses and the need for new and alternative treatment strategies for influenza. Multidrug-resistant seasonal and pandemic viruses pose new problems that must be further investigated, including the mechanisms of resistance development, influenza treatment practices that lead to resistance, and the populations of patients, especially immunocompromised patients, in whom such resistant viruses may readily develop. Only through careful evaluation will we be able to develop better treatment and preventative strategies for both seasonal and pandemic influenza A, especially for those at high risk of severe disease or complicated infections.
Funding
This work was supported by the intramural funds of the National Institutes of Health and the National Institute of Allergy and Infectious Diseases.
Acknowledgments
We thank the Comparative Medicine Branch (National Institutes of Health, National Institute of Allergy and Infectious Diseases) for assistance with animal studies, and the Histopathology Laboratory at the College of Veterinary Medicine, North Carolina State University, for assistance with the immunohistochemical analysis.
References
- 1.Bright RA, Medina MJ, Xu X, et al. Incidence of adamantane resistance among influenza A (H3N2) viruses isolated worldwide from 1994 to 2005: a cause for concern. Lancet. 2005;366:1175–81. doi: 10.1016/S0140-6736(05)67338-2. [DOI] [PubMed] [Google Scholar]
- 2.Rahman M, Bright RA, Kieke BA, et al. Adamantane-resistant influenza infection during the 2004-05 season. Emerg Infect Dis. 2008;14:173–6. doi: 10.3201/eid1401.070460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bright RA, Shay DK, Shu B, Cox NJ, Klimov AI. Adamantane resistance among influenza A viruses isolated early during the 2005-2006 influenza season in the United States. JAMA. 2006;295:891–4. doi: 10.1001/jama.295.8.joc60020. [DOI] [PubMed] [Google Scholar]
- 4.Deyde VM, Xu X, Bright RA, et al. Surveillance of resistance to adamantanes among influenza A(H3N2) and A(H1N1) viruses isolated worldwide. J Infect Dis. 2007;196:249–57. doi: 10.1086/518936. [DOI] [PubMed] [Google Scholar]
- 5.Kim CU, Lew W, Williams MA, et al. Influenza neuraminidase inhibitors possessing a novel hydrophobic interaction in the enzyme active site: design, synthesis, and structural analysis of carbocyclic sialic acid analogues with potent anti-influenza activity. J Am Chem Soc. 1997;119:681–90. doi: 10.1021/ja963036t. [DOI] [PubMed] [Google Scholar]
- 6.Aoki FY, Boivin G, Roberts N. Influenza virus susceptibility and resistance to oseltamivir. Antivir Ther. 2007;12:603–16. [PubMed] [Google Scholar]
- 7.Ives JA, Carr JA, Mendel DB, et al. The H274Y mutation in the influenza A/H1N1 neuraminidase active site following oseltamivir phosphate treatment leave virus severely compromised both in vitro and in vivo. Antiviral Res. 2002;55:307–17. doi: 10.1016/s0166-3542(02)00053-0. [DOI] [PubMed] [Google Scholar]
- 8.Gubareva LV, Kaiser L, Matrosovich MN, Soo-Hoo Y, Hayden FG. Selection of influenza virus mutants in experimentally infected volunteers treated with oseltamivir. J Infect Dis. 2001;183:523–31. doi: 10.1086/318537. [DOI] [PubMed] [Google Scholar]
- 9.Tai CY, Escarpe PA, Sidwell RW, et al. Characterization of human influenza virus variants selected in vitro in the presence of the neuraminidase inhibitor GS 4071. Antimicrob Agents Chemother. 1998;42:3234–41. doi: 10.1128/aac.42.12.3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang ZM, Tai CY, Mendel DB. Characterisation of an influenza A virus variant selected in vitro in the presence of the neuraminidase inhibitor, GS4071. Antiviral Res. 2000;46 (Abstract 80) [Google Scholar]
- 11.Carr J, Ives J, Kelly L, et al. Influenza virus carrying neuraminidase with reduced sensitivity to oseltamivir carboxylate has altered properties in vitro and is compromised for infectivity and replicative ability in vivo. Antiviral Res. 2002;54:79–88. doi: 10.1016/s0166-3542(01)00215-7. [DOI] [PubMed] [Google Scholar]
- 12.Herlocher ML, Carr J, Ives J, et al. Influenza virus carrying an R292K mutation in the neuraminidase gene is not transmitted in ferrets. Antiviral Res. 2002;54:99–111. doi: 10.1016/s0166-3542(01)00214-5. [DOI] [PubMed] [Google Scholar]
- 13.Dharan NJ, Gubareva LV, Meyer JJ, et al. Infections with oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA. 2009;301:1034–41. doi: 10.1001/jama.2009.294. [DOI] [PubMed] [Google Scholar]
- 14.Bloom JD, Gong LI, Baltimore D. Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science. 2010;328:1272–5. doi: 10.1126/science.1187816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abed Y, Baz M, Boivin G. A novel neuraminidase deletion mutation conferring resistance to oseltamivir in clinical influenza A/H3N2 virus. J Infect Dis. 2009;199:180–3. doi: 10.1086/595736. [DOI] [PubMed] [Google Scholar]
- 16.Baz M, Abed Y, McDonald J, Boivin G. Characterization of multidrug-resistant influenza A/H3N2 viruses shed during 1 year by an immunocompromised child. Clin Infect Dis. 2006;43:1555–61. doi: 10.1086/508777. [DOI] [PubMed] [Google Scholar]
- 17.Memoli MJ, Hrabal RJ, Hassantoufighi A, et al. Rapid selection of a transmissible multidrug-resistant influenza A/H3N2 virus in an immunocompromised host. J Infect Dis. 2010;201:1397–403. doi: 10.1086/651610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dawood FS, Jain S, Finelli L, et al. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–15. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 19.Garten RJ, Davis CT, Russell CA, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Update: influenza activity–United States, August 30-October 31, 2009. MMWR Morb Mortal Wkly Rep. 2009;58:1236–41. [PubMed] [Google Scholar]
- 21.Update: drug susceptibility of swine-origin influenza A (H1N1) viruses, April 2009. MMWR Morb Mortal Wkly Rep. 2009;58:433–5. [PubMed] [Google Scholar]
- 22.Baz M, Abed Y, Papenburg J, Bouhy X, Hamelin ME, Boivin G. Emergence of oseltamivir-resistant pandemic H1N1 virus during prophylaxis. N Engl J Med. 2009;361:2296–7. doi: 10.1056/NEJMc0910060. [DOI] [PubMed] [Google Scholar]
- 23.Memoli MJ, Hrabal RJ, Hassantoufighi A, Eichelberger MC, Taubenberger JK. Rapid selection of oseltamivir- and peramivir-resistant pandemic H1N1 virus during therapy in 2 immunocompromised hosts. Clin Infect Dis. 2010;50:1252–5. doi: 10.1086/651605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krafft AE, Russell KL, Hawksworth AW, et al. Evaluation of PCR testing of ethanol-fixed nasal swab specimens as an augmented surveillance strategy for influenza virus and adenovirus identification. J Clin Microbiol. 2005;43:1768–75. doi: 10.1128/JCM.43.4.1768-1775.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szretter KJ, BAa KJ. Influenza: Propagation, Quantification, and Storage. Hoboken, NJ: John Wiley and Sons, 2007 (R C, ed. Current protocols in immunology) [DOI] [PubMed] [Google Scholar]
- 26.Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. Universal primer set for the full-length amplification of all influenza A viruses. Arch Virol. 2001;146:2275–89. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]
- 27.Memoli MJ, Tumpey TM, Jagger BW, et al. An early ‘classical’ swine H1N1 influenza virus shows similar pathogenicity to the 1918 pandemic virus in ferrets and mice. Virology. 2009;393:338–45. doi: 10.1016/j.virol.2009.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008;198:962–70. doi: 10.1086/591708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gill JR, Sheng ZM, Ely SF, et al. Pulmonary pathologic findings of fatal 2009 pandemic influenza A/H1N1 viral infections. Arch Pathol Lab Med. 2010;134:235–43. doi: 10.5858/134.2.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morris JA, Norman MC. The isolation of Listeria monocytogenes from ferrets. J Bacteriol. 1950;59:313–4. doi: 10.1128/jb.59.2.313-314.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]