Abstract
Study objective
Previous studies suggest improved patient outcomes for providers who perform high volumes of complex medical procedures. Out-of-hospital tracheal intubation is a difficult procedure. We seek to determine the association between rescuer procedural experience and patient survival after out-of-hospital tracheal intubation.
Methods
We analyzed probabilistically linked Pennsylvania statewide emergency medicine services, hospital discharge, and death data of patients receiving out-of-hospital tracheal intubation. We defined tracheal intubation experience as cumulative tracheal intubation during 2000 to 2005; low=1 to 10 tracheal intubations, medium=11 to 25 tracheal intubations, high=26 to 50 tracheal intubations, and very high=greater than 50 tracheal intubations. We identified survival on hospital discharge of patients intubated during 2003 to 2005. Using generalized estimating equations, we evaluated the association between patient survival and out-of-hospital rescuer cumulative tracheal intubation experience, adjusted for clinical covariates.
Results
During 2003 to 2005, 4,846 rescuers performed tracheal intubation. These individuals performed tracheal intubation on 33,117 patients during 2003 to 2005 and 62,586 patients during 2000 to 2005. Among 21,753 cardiac arrests, adjusted odds of survival was higher for patients intubated by rescuers with very high tracheal intubation experience; adjusted odds ratio (OR) versus low tracheal intubation experience: very high 1.48 (95% confidence interval [CI] 1.15 to 1.89), high 1.13 (95% CI 0.98 to 1.31), and medium 1.02 (95% CI 0.91 to 1.15). Among 8,162 medical nonarrests, adjusted odds of survival were higher for patients intubated by rescuers with high and very high tracheal intubation experience; adjusted OR versus low tracheal intubation experience: very high 1.55 (95% CI 1.08 to 2.22), high 1.29 (95% CI 1.04 to 1.59), and medium 1.16 (95% CI 0.97 to 1.38). Among 3,202 trauma nonarrests, survival was not associated with rescuer tracheal intubation experience; adjusted OR versus low tracheal intubation experience: very high 1.84 (95% CI 0.89 to 3.81), high 1.25 (95% CI 0.85 to 1.85), and medium 0.92 (95% CI 0.67 to 1.26).
Conclusion
Rescuer procedural experience is associated with improved patient survival after out-of-hospital tracheal intubation of cardiac arrest and medical nonarrest patients. Rescuer procedural experience is not associated with patient survival after out-of-hospital tracheal intubation of trauma nonarrest patients.
INTRODUCTION
Background
In the United States, emergency medical services (EMS) rescuers (paramedics, nurses, and physicians) perform out-of-hospital tracheal intubation on patients with critical illness such as cardiopulmonary arrest, respiratory failure, and major trauma.1–4 Tracheal intubation is difficult and requires multiple actions, including respiratory status assessment, airway device selection and preparation, laryngoscopy and intubation, ventilation between intubation efforts, endotracheal tube placement confirmation, securing the endotracheal tube in place, and rescue alternate airway placement.5 Reports of tracheal intubation adverse events (for example, endotracheal tube misplacement or dislodgement, multiple tracheal intubation laryngoscopy attempts, and inadvertent hyperventilation) highlight the complexity of the procedure in the uncontrolled out-of-hospital setting.6–11
Importance
Previous studies suggest improved outcomes and fewer adverse events for hospitals or providers who perform high volumes of complex medical procedures.12–17 For example, mortality is lower among patients undergoing coronary bypass surgery or cardiac catheterization in high-volume hospitals.14 Low-surgical-volume hospitals have higher rates of postoperative wound infections.12 Survival is higher for injured patients treated at specialty trauma centers.15–17 Although there are plausible connections between rescuer procedural experience and patient survival after out-of-hospital tracheal intubation, to our knowledge no previous efforts have evaluated this relationship.
Goals of This Investigation
The objective of this study was to identify the association between rescuer procedural experience and patient survival after out-of-hospital tracheal intubation. We hypothesized that increased tracheal intubation experience would be associated with improved patient survival.
MATERIALS AND METHODS
Study Design
The institutional review boards of the University of Pittsburgh, University of Utah, and University of Alabama at Birmingham approved the study.
In this retrospective analysis, we linked statewide EMS, hospital discharge, and death data from the Commonwealth of Pennsylvania to determine the relationship between rescuer procedural experience and patient survival after out-of-hospital tracheal intubation.
Study Setting
We studied patients treated by out-of-hospital EMS rescuers in Pennsylvania. Pennsylvania EMS care is diverse and encompasses a range of care configurations and practice settings. Independent private and municipal agencies provide both local and regional EMS care. Pennsylvania EMS practice settings include dense urban population centers (for example, Philadelphia and Pittsburgh), as well as extensive suburban and remote rural areas. Eleven independent air medical services provide care across the commonwealth.
Pennsylvania EMS rescuers work in both volunteer and career capacities and include first responders, emergency medical technicians, paramedics, out-of-hospital registered nurses, and EMS physicians. Advanced life support vehicles may have one or two advanced life support rescuers. Only EMS paramedics, nurses, and physicians are allowed to perform out-of-hospital tracheal intubation. Composing more than 90% of Pennsylvania advanced life support rescuers, paramedics perform more than 94% of out-of-hospital tracheal intubation. Although all air medical rescuers may use neuromuscular-blockade-assisted (rapid sequence) tracheal intubation, select ground EMS units are allowed to use tracheal intubation facilitated by sedatives only.
We used 3 sources of data: Pennsylvania Emergency Medical Services Patient Care Report data, Pennsylvania Health Care Cost Containment Council hospital discharge data, and the Pennsylvania Death Registry.
The Pennsylvania Emergency Medical Services Patient Care Report is a database of all Pennsylvania EMS patient care incidents. In Pennsylvania, all EMS agencies must use electronic medical record systems that transmit patient care data to a central database. EMS services without computer access must submit patient care reports by using computer scan forms. Following the National Highway Traffic Safety Administration standards for EMS data collection and reporting, the Pennsylvania Emergency Medical Services Patient Care Report contains data about patient characteristics, nature and severity of illness, injury patterns, administered drugs, procedures and interventions, and information about the EMS service and out-of-hospital rescuers delivering care.18 We used Pennsylvania Emergency Medical Services Patient Care Report data for the 6-year period January 1, 2000, to December 31, 2005.
The Pennsylvania Health Care Cost Containment Council contains demographic, diagnostic, and clinical information on all hospital discharges in the commonwealth.19 Hospitals use standard software to report basic demographic (patient age, sex), clinical (the date, time, and location of hospital admission, the discharge status and hospital length of stay) and diagnostic information (primary and up to nine secondary International Classification of Diseases, Ninth Revision [ICD-9] discharge diagnoses). The Pennsylvania Health Care Cost Containment Council includes only patients surviving to hospital admission; the data set does not include patients dying in the emergency department (ED) before hospital admission. We used data for the 3-year period January 1, 2003, through December 31, 2005.
The Pennsylvania Death Registry contains demographic and clinical information on all deaths in the commonwealth.20 We used death data for the 3-year period January 1, 2003, through December 31, 2005.
Selection of Participants
We studied patients receiving successful out-of-hospital tracheal intubation by advanced life support rescuers, including EMS paramedics, nurses, and physicians. Rescuers self-reported tracheal intubation success in the Pennsylvania Emergency Medical Services Patient Care Report; there are no statewide protocols for independent confirmation by a second rescuer or physician. The Pennsylvania Emergency Medical Services Patient Care Report does not include information on unsuccessful tracheal intubations or post–tracheal intubation tube placement events.
We determined the outcomes of patients receiving tracheal intubation during 2003 to 2005. To determine the cumulative experience of rescuers performing these tracheal intubations, we used the longer overlapping period 2000 to 2005.
We linked the 3 data sets to connect out-of-hospital tracheal intubation and patient outcomes. Because the data sets did not have unique patient identifiers (for example, name, social security number, date of birth, and medical record number), we connected patient records with probabilistic linkage. Probabilistic linkage compares the values from several data fields (for example, date, time, age, sex, and geographic region) to estimate the probability that pairs of records match. 21–22 Many medical research studies have used probabilistic linkage.25–31
A more comprehensive description of the record linkage process is given in Appendix E1, Table E1 (available online at http://www.annemergmed.com). To optimize record linkage, we narrowed the Pennsylvania Emergency Medical Services Patient Care Report to tracheal intubation cases. We limited the Pennsylvania Health Care Cost Containment Council to patients (1) admitted through the ED and (2) admitted to an ICU or discharged with a diagnosis of mechanical ventilation (ICD-9p 96.7 to 96.72), cardiopulmonary arrest (ICD-9 427.4 to 427.5), or respiratory arrest (ICD-9 799.1).
We probabilistically linked the 3 data sets by using combinations of the following variables: date and time of encounter, patient age, patient sex, patient race, receiving hospital facility, EMS agency location, and patient geographic location (minor civil division). Because an EMS patient might appear in both the Pennsylvania Health Care Cost Containment Council and Pennsylvania Death Registry data sets, we used a “triple match” algorithm to resolve these overlapping linkages.32
A customary practice in probabilistic linkage is to retain only record pairs with predicted match weights over an a priori fixed threshold (eg, match probability >0.90).33 However, this approach often results in low match rates and may inadvertently exclude true matches just below the defined threshold. To avoid this outcome, we used a multiple imputation procedure, creating a series of linked data sets based on the probability distribution of match weights.32 Using this technique, we created 5 probability-linked data sets. We conducted separate analyses on each probability-linked data set and combined the estimates using Rubin’s method.34,35
We linked patient records for the period January 1, 2003, to December 31, 2005. We performed record linkage with Linksolv, version 6 (Strategic Matching Inc., Morrisonville, NY).
Outcome Measures
Patient survival to hospital discharge was the primary outcome, determined from Pennsylvania Death Registry and Pennsylvania Health Care Cost Containment Council records. If the patient appeared in the Pennsylvania Health Care Cost Containment Council data set, we used the reported discharge status (alive/dead). If a patient did not appear in the Pennsylvania Health Care Cost Containment Council data set but had a death record on the date of encounter, we classified the patient as dead. If the patient appeared in both the Pennsylvania Health Care Cost Containment Council and Pennsylvania Death Registry, we used the outcome reported in Pennsylvania Health Care Cost Containment Council. We identified outcomes of patients intubated during 2003 to 2005 only.
Because of their differing prognoses and airway management approaches, we separately analyzed the cardiac arrest, medical nonarrest, and trauma (major injury) nonarrest subsets. We defined cardiac arrests as patients receiving cardiopulmonary resuscitation (CPR) chest compressions, receiving automated external defibrillator use, or who exhibited an ECG rhythm of ventricular fibrillation, ventricular tachycardia, pulseless electrical activity, or asystole. We classified all other patients as nonarrests.
The Pennsylvania Emergency Medical Services Patient Care Report did not contain standard measures of trauma acuity such as the Abbreviated Injury Score.36 We therefore defined trauma (major injury) nonarrests as patient incidents involving assault, shooting, stabbing, fall, or fire, or bicycle, motorcycle, pedestrian, recreational, or other vehicular crash. We also included cases with major injury situational modifiers such as flail chest, burns greater than 10%, face or airway burns, vehicular extrication greater than 20 minutes, fall greater than 20 feet, extremity paralysis, vehicular speed greater than 40 miles per hour, vehicular speed change greater than 20 miles per hour, vehicular deformity greater than 20 inches, passenger compartment intrusion greater than 12 inches, vehicular rollover, passenger ejection, death in same vehicle, pedestrian/ vehicle crash greater than 5 miles per hour, pedestrian thrown/ run over, and motorcycle crash greater than 20 miles/hour. The Pennsylvania Emergency Medical Services Patient Care Report a priori defined these categories. We defined all other nonarrest patients as medical nonarrests.
For cardiac arrests, we used the covariates patient age, patient sex, major injury/trauma bystander-witnessed cardiac arrest, bystander CPR, EMS automated external defibrillator use, EMS response time (dispatch to arrival on scene), rescuer cumulative patient contacts, EMS agency population setting, and year of encounter. We included trauma/major injury as a covariate in the cardiac arrest model to account for traumatic cardiac arrest cases in the data set. We adjusted for bystander-witnessed arrest, bystander CPR, EMS automated external defibrillator use, and EMS response time because of their identified relationships with out-of-hospital cardiac arrest outcome.37
For the medical and trauma nonarrests, we used the covariates patient age, patient sex, pulse, systolic blood pressure, Glasgow Coma Scale score, rescuer cumulative patient contacts, EMS agency population setting, and year of encounter. Because of the absence of trauma severity covariates, we did not incorporate Injury Severity Scores in the trauma nonarrest model. The Pennsylvania Emergency Medical Services Patient Care Report did not have information on the use of rapid-sequence or sedation-facilitated intubation or the administration of neuromuscular-blocking or sedative agents. Therefore, we did not adjust for the use of rapid sequence or sedation-facilitated intubation.
Acquired clinical experience outside of tracheal intubation procedures may affect patient outcomes. Therefore, for each tracheal intubation we also determined the paramedic’s cumulative number of patient contacts between January 1, 2000, and the date of the tracheal intubation.
We classified EMS agency population setting as urban, nonurban, or air medical. Although the Pennsylvania Emergency Medical Services Patient Care Report contains the minor civil division of a patient encounter, the distribution of urban and rural settings may vary within these regions. Also, the Pennsylvania Emergency Medical Services Patient Care Report does not use standard federal urban/rural coding systems.38 Because our intention was to broadly characterize EMS provider practice setting (not the precise geographic location of the patient), we classified urban EMS agencies as services located in the greater Allentown, Erie, Harrisburg, Lancaster, Philadelphia, Pittsburgh, Reading, Wilkes-Barre, and York areas. We used zip codes of the EMS agencies to confirm their locations. We classified other EMS agencies as nonurban services. Because air medical helicopters may cross geographic boundaries and have distinctly different practice settings, we classified these agencies in a separate air medical category.
We divided patient age into the intervals less than or equal to 6, 7 to 17, and greater than 17 years old. We divided pulse into the intervals less than or equal to 40, 40 to 80, and greater than 80 beats/min and systolic blood pressure into the intervals less than or equal to 60, 61 to 100, 101 to 140, and greater than 140 mm Hg. We divided Glasgow Coma Scale score into the intervals 3 to 8, 9 to 12, and 13 to 15. We divided rescuer cumulative patient contacts to the intervals less than 1,000, 1,001 to 2,000, 2,001 to 4,000, and greater than 4,000. We divided EMS response time to the intervals 0 to 3, 4 to 6, 7 to 10, and greater than 10 minutes. We selected these ordinal categories because they optimized multivariable model fit.
Although the outcomes analysis encompassed January 1, 2003, to December 31, 2005, we sought to account for each rescuer’s accumulated proficiency before this period. Therefore, for each tracheal intubation we defined cumulative tracheal intubation experience as the accumulated number of tracheal intubations since January 1, 2000. Accurate procedural data before January 1, 2000, were not available. Because the Pennsylvania Emergency Medical Services Patient Care Report does not record unsuccessful tracheal intubations, these figures included only successful tracheal intubations.
Primary Data Analysis
To evaluate the association between patient survival and rescuer tracheal intubation experience, we fit multivariable models with generalized estimating equations.39 The general form of the models was
We defined patient survival as the primary dependent outcome. We defined rescuer cumulative tracheal intubation experience as the key independent variable. If the data set attributed a tracheal intubation to more than one rescuer, we used the experience level of the rescuer with the higher cumulative tracheal intubation experience. If the 2 rescuers had the same cumulative tracheal intubation experience, we selected the individual with the higher number of cumulative patient contacts.
We separately analyzed cardiac arrest, medical nonarrest, and trauma nonarrest patients. For the cardiac arrest patients, we adjusted for patient age, patient sex, major injury/trauma bystander-witnessed cardiac arrest, bystander CPR, EMS automated external defibrillator use, EMS response time (dispatch to arrival on scene), rescuer cumulative patient contacts, EMS agency population setting, and year of encounter. For the nonarrest patients, we adjusted for patient age, patient sex, pulse, systolic blood pressure, Glasgow Coma Scale score, rescuer cumulative patient contacts, EMS agency population setting, and year of encounter.
Because each rescuer may have performed several tracheal intubations, we used generalized estimating equations to account for clustering, applying independent covariance structure. We repeated the multivariable analysis on each of the 5 probability-linked sets, combining the results using Rubin’s method. We implemented Rubin’s method through the SAS procedure MIANALYZE.34,35 We analyzed the data with Stata 10.0 (StataCorp, College Station, TX) and SAS v.9.2 (SAS Institute, Inc., Cary, NC).
Sensitivity Analyses
In the primary analysis, if the data set attributed multiple rescuers to a tracheal intubation, we used the tracheal intubation experience of the most experienced rescuer. We repeated the analysis with the tracheal intubation experience of the least experienced rescuer in these scenarios. We repeated the analysis separately for each EMS agency population setting (urban, nonurban, air medical).
RESULTS
During the 3-year outcome analysis period 2003 to 2005, 4,846 rescuers performed tracheal intubation. These individuals performed tracheal intubation on 33,117 patients during 2003 to 2005 and 62,586 patients during 2000 to 2005. Median 6-year (2000 to 2005) tracheal intubation experience was 10 tracheal intubations per rescuer (interquartile range 4–19).
The 33,117 tracheal intubation patients included 21,753 cardiac arrest, 8,162 medical nonarrest, and 3,202 trauma nonarrest tracheal intubations (Tables 1–3). Across the 5 probability-linked data sets, we matched an average of 26,266 of 33,117 tracheal intubations to patient outcomes (mean linkage rate 77.7%). The distributions of patient characteristics were similar between the whole data set and the linked subset. Among patients linked to outcomes, overall survival was 16.1% (95% confidence interval [CI] 15.6% to 16.6%) for cardiac arrest, 62.7% (95% CI 61.4% to 63.9%) for medical nonarrest, and 69.7% (95% CI 67.8% to 71.7%) for trauma nonarrest tracheal intubation.
Table 1.
Characteristics of cardiac arrest tracheal intubation patients for outcomes analysis period 2003 to 2005.*
| Cardiac Arrests (n=21,753) |
Cardiac Arrest, Linked Cases Only (n=19,135) |
|||
|---|---|---|---|---|
| Characteristic | No. | (%) | No. | (%) |
| Patient age, y | ||||
| ≤6 | 478 | (2.2) | 319 | (1.7) |
| 7–17 | 283 | (1.3) | 228 | (1.2) |
| ≥18 | 20,869 | (95.9) | 18,511 | (96.7) |
| Unknown | 123 | (0.6) | 77 | (0.4) |
| Sex | ||||
| Male | 13,466 | (61.9) | 11,902 | (62.2) |
| Female | 8,075 | (37.1) | 7,095 | (37.1) |
| Unknown | 212 | (1.0) | 138 | (0.7) |
| Major injury/trauma | ||||
| No | 20,245 | (93.1) | 17,890 | (93.5) |
| Yes | 1,508 | (6.9) | 1,245 | (6.5) |
| Bystander-witnessed arrest | ||||
| No | 4,816 | (22.1) | 4,331 | (22.6) |
| Yes | 8,489 | (39.0) | 7,496 | (39.2) |
| Unknown | 8,444 | (38.8) | 7,308 | (38.2) |
| Bystander CPR | ||||
| No | 7,494 | (30.6) | 6,704 | (35.0) |
| Yes | 6,660 | (34.5) | 5,890 | (30.8) |
| Unknown | 7,595 | (34.9) | 6,541 | (34.2) |
| EMS automated external defibrillator use | ||||
| No | 19,701 | (90.6) | 17,334 | (90.6) |
| Yes | 2,052 | (9.4) | 1,801 | (9.4) |
| Initial ECG rhythm | ||||
| Nonshockable rhythm | 13,792 | (63.4) | 12,269 | (64.1) |
| Shockable rhythm | 3,184 | (14.6) | 2,793 | (14.6) |
| Unknown | 4,773 | (22.0) | 4,073 | (21.3) |
| Response time, min | ||||
| 0–3 | 4,208 | (19.3) | 3,690 | (19.3) |
| 4–6 | 7,351 | (33.8) | 6,515 | (34.0) |
| 7–10 | 5,796 | (26.7) | 5,140 | (26.9) |
| >10 | 4,394 | (20.2) | 3,788 | (19.8) |
| Unknown | 4 | (0) | 2 | (0) |
| Rescuer cumulative patient contacts (2000–2005) | ||||
| <1,000 | 5,248 | (24.1) | 4,568 | (23.9) |
| 1,001–2,000 | 7,081 | (32.6) | 6,279 | (32.8) |
| 2,001–4,000 | 6,068 | (27.9) | 5,343 | (27.9) |
| >4,000 | 3,356 | (15.4) | 2,945 | (15.4) |
| EMS agency population setting | ||||
| Nonurban | 11,560 | (53.1) | 10,126 | (52.9) |
| Urban† | 9,985 | (45.9) | 8,872 | (46.4) |
| Air medical | 166 | (0.8) | 102 | (0.5) |
| Unknown | 42 | (0.2) | 35 | (0.2) |
| Year | ||||
| 2003 | 7,853 | (36.1) | 6,840 | (35.7) |
| 2004 | 7,181 | (33.0) | 6,350 | (33.2) |
| 2005 | 6,719 | (30.9) | 5,945 | (31.1) |
|
Cumulative tracheal intubation experience (2000–2005) of rescuer performing tracheal intubation, No. |
||||
| 1–10 | 7,509 | (34.5) | 6,594 | (34.5) |
| 11–25 | 9,208 | (42.3) | 8,073 | (42.2) |
| 26–50 | 4,412 | (20.3) | 3,927 | (20.5) |
| >50 | 624 | (2.9) | 541 | (2.8) |
| Patient outcome (survival; linked cases only) | ||||
| Alive | N/A | N/A | 3,080 | (16.1) |
| Dead | N/A | N/A | 16,055 | (83.9) |
Column for linked cases reflects patients linked to hospital or death records in any of the 5 imputed data sets.
EMS agency located in Allentown, Erie, Harrisburg, Lancaster, Philadelphia, Pittsburgh, Reading, Wilkes-Barre, or York areas.
Table 3.
Characteristics of trauma (major injury) nonarrest tracheal intubation patients for outcomes analysis period 2003 to 2005.*
| Trauma Nonarrest (n=3,202) |
Trauma Nonarrest, Linked Cases Only (n=2,104) |
|||
|---|---|---|---|---|
| Characteristic | No. | (%) | No. | (%) |
| Patient age, y | ||||
| ≤6 | 218 | (6.8) | 93 | (4.4) |
| 7–17 | 319 | (10.0) | 212 | (10.1) |
| ≥18 | 2,553 | (79.7) | 1,747 | (83.0) |
| Unknown | 112 | (3.5) | 52 | (2.5) |
| Sex | ||||
| Male | 2,214 | (69.1) | 1,476 | (70.2) |
| Female | 867 | (27.1) | 573 | (27.2) |
| Unknown | 121 | (3.8) | 55 | (2.6) |
| Pulse, beats/min | ||||
| ≤40 | 370 | (11.5) | 240 | (11.4) |
| 40–80 | 686 | (21.4) | 447 | (21.2) |
| >80 | 1,952 | (61.0) | 1,293 | (61.5) |
| Unknown | 194 | (6.1) | 124 | (5.9) |
| Systolic blood pressure, mm Hg | ||||
| ≤60 | 621 | (19.4) | 406 | (19.3) |
| 61–100 | 463 | (14.4) | 303 | (14.4) |
| 101–140 | 1,063 | (33.2) | 695 | (33.0) |
| >140 | 780 | (24.4) | 526 | (25.0) |
| Unknown | 275 | (8.6) | 174 | (8.3) |
| Glasgow Coma Scale score | ||||
| 3–8 | 2,152 | (67.2) | 1,420 | (67.5) |
| 9–12 | 398 | (12.4) | 272 | (12.9) |
| 13–15 | 518 | (16.2) | 324 | (15.4) |
| Unknown | 134 | (4.2) | 88 | (4.2) |
| Rescuer cumulative patient contacts (2000–2005), No. | ||||
| <1,000 | 1,790 | (55.9) | 1,157 | (55.0) |
| 1,001–2,000 | 715 | (22.3) | 461 | (21.9) |
| 2,001–4,000 | 414 | (12.9) | 256 | (12.2) |
| >4000 | 283 | (8.8) | 230 | (10.9) |
| EMS agency population setting | ||||
| Nonurban | 888 | (27.7) | 464 | (22.1) |
| Urban† | 625 | (19.5) | 492 | (23.4) |
| Air medical | 1,674 | (52.3) | 1,143 | (54.3) |
| Unknown | 15 | (0.5) | 5 | (0.2) |
| Year | ||||
| 2003 | 1,050 | (32.8) | 667 | (31.7) |
| 2004 | 1,108 | (34.6) | 734 | (34.9) |
| 2005 | 1,044 | (32.6) | 703 | (33.4) |
|
Cumulative tracheal intubation experience (2000–2005) of rescuer performing tracheal intubation, No. |
||||
| 1–10 | 918 | (28.7) | 579 | (27.5) |
| 11–25 | 1,429 | (44.6) | 964 | (45.8) |
| 26–50 | 748 | (23.4) | 482 | (22.9) |
| >50 | 107 | (3.3) | 79 | (3.8) |
| Patient outcome (survival; linked cases only) | ||||
| Alive | N/A | N/A | 1,467 | (69.7) |
| Dead | N/A | N/A | 637 | (30.3) |
Column for linked cases reflects patients linked to hospital or death records in any of the 5 imputed data sets.
EMS agency located in Allentown, Erie, Harrisburg, Lancaster, Philadelphia, Pittsburgh, Reading, Wilkes-Barre, or York areas.
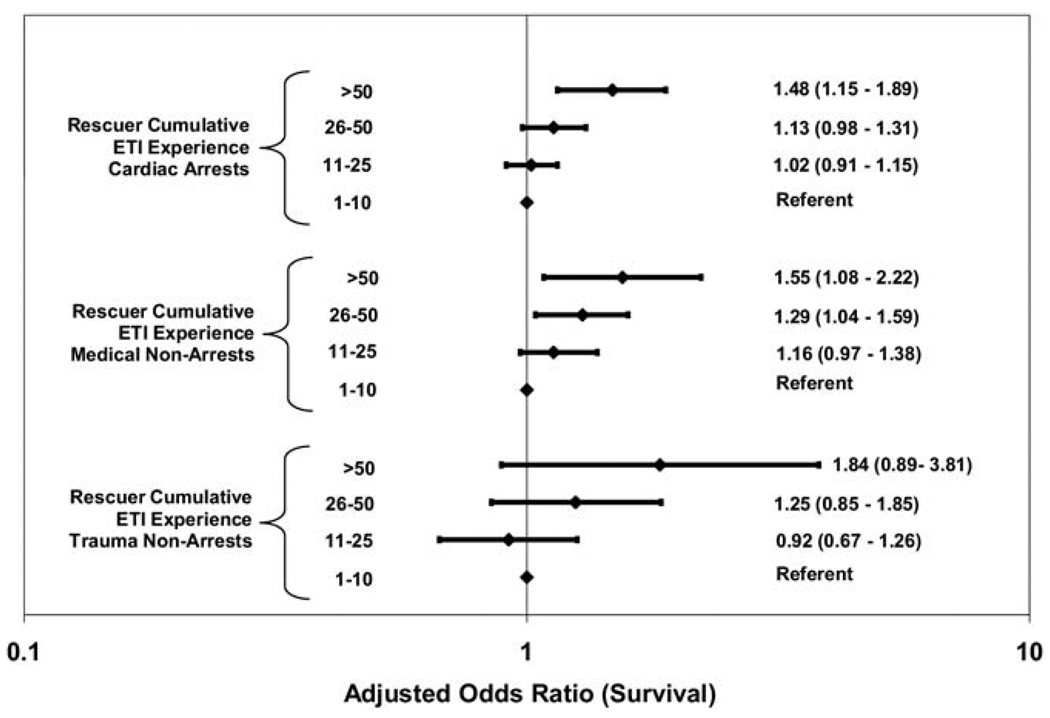
Among the 21,753 cardiac arrests, the adjusted odds of survival was highest for patients intubated by rescuers with very high tracheal intubation experience; adjusted odds ratio (OR) versus low tracheal intubation experience: very high 1.48 (95% confidence interval [CI] 1.15 to 1.89), high 1.13 (95% CI 0.98 to 1.31), and medium 1.02 (95% CI 0.91 to 1.15). (Figure; Table E2, available online at http://www.annemergmed.com). Among 8,162 medical nonarrests, adjusted odds of survival were higher for patients intubated by rescuers with very high or high tracheal intubation experience; adjusted OR versus low tracheal intubation experience: very high 1.55 (95% CI 1.08 to 2.22), high 1.29 (95% CI 1.04 to 1.59), and medium 1.16 (95% CI 0.97 to 1.38). (Figure; Table E3, available online at http://www.annemergmed.com).
Figure.
Adjusted associations between patient survival and rescuer cumulative tracheal intubation experience. Data include tracheal intubation patients January 1, 2003, to December 31, 2005. Cardiac arrests, medical nonarrests, and trauma nonarrests were analyzed separately. Tracheal intubation experience was defined as rescuer’s cumulative number of tracheal intubations since January 1, 2000. Cardiac arrest estimates were adjusted for patient age, patient sex, major injury/trauma bystander-witnessed cardiac arrest, bystander CPR, EMS automated external defibrillator use, EMS response time (dispatch to arrival on scene), rescuer cumulative patient contacts, EMS agency population setting, and year of encounter. Medical and trauma nonarrests were adjusted for patient age, patient sex, pulse, systolic blood pressure, Glasgow Coma Scale score, rescuer cumulative patient contacts, EMS agency population setting, and year of encounter.ETI, endotracheal intubation. (Full models presented in Tables E2 and E3, available online at http://www.annemergmed.com.)
Among 3,202 trauma nonarrests, survival was not associated with rescuer tracheal intubation experience; adjusted OR versus low tracheal intubation experience: very high 1.84 (95% CI 0.89 to 3.81), high 1.25 (95% CI 0.85 to 1.85), and medium 0.92 (95% CI 0.67 to 1.26). (Figure; Table E3, available online at http://www.annemergmed.com). However, treatment by an air medical EMS agency was associated with improved outcome (adjusted odds ratio [OR] 1.95; 95% CI 1.28 to 2.96).
In the main analysis, a tracheal intubation was attributed to more than one rescuer in 1,584 instances (2 rescuers for 1,532 patients, 3 rescuers for 52 patients, and 4 rescuers for 1 patient). In these cases, we used the cumulative tracheal intubation count of the most experienced rescuer. In the sensitivity analysis, we repeated the analysis with the cumulative tracheal intubation count of the least experienced rescuer and found the associations between adjusted mortality and tracheal intubation experienced largely unchanged. However, in the cardiac arrest subset, both very high (>50 cumulative tracheal intubations) and high (26 to 50 cumulative tracheal intubations) tracheal intubation experience were now associated with survival (Table E4, available online at http://www.annemergmed.com).
To account for potential EMS care delivery differences between population settings, we repeated the analysis separately for patients treated by urban, nonurban, and air medical EMS agencies, observing some key differences (Table E5, available online at http://www.annemergmed.com). Among urban medical nonarrests, patient survival was no longer associated with rescuer tracheal intubation experience. However, in the nonurban trauma subset, patient survival was now associated with increased rescuer tracheal intubation experience; adjusted OR versus low tracheal intubation experience, medium 1.30 (95% CI 0.71 to 2.39), high 2.32 (95% CI 1.03 to 5.26), and very high 5.91 (95% CI 1.38 to 25.3). The cardiac arrest and medical nonarrest models for air medical agencies did not converge because of the relatively small numbers of observations (air medical cardiac arrest 166; medical nonarrest 847). There were no other major differences.
LIMITATIONS
Limitations of this study include the use of administrative data without unique identifiers, which precluded exact deterministic linkages to outcomes. We attempt to dampen this by examining a large, longitudinal, geographically and clinically diverse tracheal intubation population. Our use of probabilistic linkage represented the best option for connecting these data sets. Although probabilistic linkage often excludes cases because of nonlinkage, our use of multiple imputation algorithms improved the linkage rate.
Although we used multivariate regression to account for variations in severity of illness, we could not adjust for unmeasured or unknown factors. For example, because of the absence of injury severity measures in the study data sets, we could not fully adjust for severity of injury in the major trauma subset. We also could not adjust for rapid sequence intubation, which is used by select air and ground EMS units nationally. We used the best approaches, given the limitations of the available data sets. The consistency of results using multiple modeling approaches supports the robustness of our inferences.
We observed that in nonarrest medical cases, paramedics with very high experience tended to intubate patients with higher systolic blood pressure and Glasgow Coma Scale scores; this selection bias could explain part of the increased survival in this subset (Tables E6 and E7, available online at http://www.annemergmed.com). Conversely, in the trauma subset, paramedics with very high experience tended to intubate hypotensive patients with low Glasgow Coma Scale scores, potentially obscuring survival benefi ts (Tables E8 and E9, available online at http://www.annemergmed.com).
Our observed rate of cardiac arrest survival exceeds that of other studies. However, most studies of out-of-hospital cardiac arrest involve non-EMS-witnessed events. Therefore, our effort may reflect a more heterogeneous population.
Our analysis contains successful tracheal intubation only. Up to 15% of out-of-hospital tracheal intubation efforts may fail.41,42 It is unclear how including failed tracheal intubation would have altered the underlying inferences. Our analysis modeled patient survival. Other metrics of tracheal intubation quality may have plausible links to procedural experience; for example, tracheal intubation success rates or the frequency of tracheal intubation adverse events or errors such as endotracheal tube misplacement, inadvertent hyperventilation, or prolonged tracheal intubation efforts.6–7,9,43 In the current study, we could not evaluate these alternate endpoints.
In instances in which multiple rescuers received credit for the tracheal intubation, we were unable to separate the effects between individuals. However, the results were generally unchanged whether we assigned the case to the most or the least experienced rescuer. We also could not account for tracheal intubation experience acquired outside of the clinical setting; for example, mannequin or operating-room-based training.
Our study did not account for other concurrent interventions. For example, we could not determine CPR chest compression continuity or ventilatory rate.9–11,44 Our study also could not account for variations in individual rescuer characteristics or hospital course. Other potential factors include parallel experience with other procedures such as chest compressions, bag-valve-mask ventilation, and intraosseous access.
DISCUSSION
Previous studies suggest improved outcomes and fewer adverse events for hospitals or providers who perform high volumes of complex medical procedures.12–16 Out-of-hospital tracheal intubation is a widely practiced and complex intervention requiring the coordination of multiple actions. Our study suggests associations between increased rescuer procedural experience and improved patient survival after out-of-hospital tracheal intubation of cardiac arrests and medical nonarrests. However, we did not observe similar associations with tracheal intubation of trauma nonarrest patients.
There are plausible connections between practitioner tracheal intubation experience and patient outcomes. Experienced rescuers may be more adept at executing and coordinating the complex psychomotor elements of tracheal intubation such as recognition of respiratory failure, selection of airway interventions, preparation and testing of equipment, patient positioning, laryngoscopy and intubation, endotracheal tube placement verification, and securing the tube in place.5 Experienced rescuers may be better poised to prevent tracheal intubation adverse events such as endotracheal tube misplacement or dislodgement.6–7,41 Rescuers with increased experience may also be more skilled at preventing tracheal intubation interactions with other key actions; for example, preventing inadvertent hyperventilation or CPR chest compression interruptions.9–11,44
We did not observe an association between patient survival and rescuer tracheal intubation experience in trauma nonarrests. This finding was unexpected because clinicians often perceive trauma tracheal intubation as difficult compared with medical tracheal intubation. The most likely explanation was the absence of injury severity scales (for example, the Abbreviated Injury Score or Injury Severity Score), precluding further risk adjustment.36,45 As discussed previously, paramedics with very high experience tended to intubate hypotensive trauma patients with low Glasgow Coma Scale scores; these patients may have been less likely to survive (Tables E8 and E9, available online at http://www.annemergmed.com).
Another possibility was the absence of information about rapid sequence intubation use.46 The odds of survival for air medical trauma patients were almost twice that of other patients. Because only air medical rescuers may use neuromuscular-blocking agents in Pennsylvania, our adjustment for EMS agency population setting (urban, nonurban, air medical) may have partially accounted for rapid sequence intubation use. The improved survival may have also reflected the specialized airway management and critical care training of air medical personnel.47,48 In the sensitivity analysis, however, we observed statistically significant volume-outcome associations in the nonurban ground EMS subset, suggesting potential underlying connections with tracheal intubation experience.
Although our observations might point to tracheal intubation training expansion or limiting tracheal intubation to the most highly experienced rescuers, the potential actions or policy shifts are not clear. For example, our study suggests that rescuers should perform at least 4 to 12 annual tracheal intubations. Although selected EMS agencies require this level of tracheal intubation experience, most rescuers perform far fewer procedures; for example, most Pennsylvania rescuers perform only 1 tracheal intubation annually.47,49,50 Although many paramedics acquire and maintain tracheal intubation skills in the operating room under the guidance of anesthesiologists, the opportunities for operating-room-based tracheal intubation training nationally are limited and declining.51 The effectiveness of substituting clinical tracheal intubation or critical care experience with simulated training remains unproven.52,53 Although many EMS systems optimize rescuer experience through dual-tiered response (ie, multiple basic-level ambulances supported by a single advanced-level paramedic unit), a large portion of EMS systems in the United States currently uses single-tiered response.54
Another potential approach is to require rescuers with less experienced to use simpler alternate airway devices such as the Combitube (Kendall, Inc., Mansfield, MA) and King LT airway (King Systems, Noblesville, IN). However, the effectiveness of this approach remains unverified. Because EMS rescuers view tracheal intubation as an essential skill, widespread adoption of alternate airways would require major shifts in EMS operations and culture.55
In volume-outcome studies, it is often difficult to disentangle whether increased volume is the cause or result of improved outcomes; that is, do patients tend to choose practitioners with better outcomes, creating high volumes for these providers? This factor does not apply to out-of-hospital tracheal intubation because critically ill individuals receive care from the ambulance and rescuers appearing on scene; there is no opportunity to “choose” providers.
Rescuer procedural experience is associated with improved patient survival after out-of-hospital tracheal intubation of cardiac arrests and medical nonarrests. Rescuer procedural experience is not associated with patient survival after out-of-hospital tracheal intubation of trauma nonarrests.
Supplementary Material
Table 2.
Characteristics of medical nonarrest tracheal intubation patients for outcomes analysis period 2003 to 2005.*
| Medical Nonarrest (n=8,162) |
Medical Nonarrest, Linked Cases Only (n=5,641) |
|||
|---|---|---|---|---|
| Characteristic | No. | (%) | No. | (%) |
| Patient age, y | ||||
| ≤6 | 175 | (2.1) | 47 | (0.8) |
| 7–17 | 171 | (2.1) | 69 | (1.2) |
| ≥18 | 7,757 | (95.0) | 5,504 | (97.6) |
| Unknown | 59 | (0.7) | 21 | (0.4) |
| Sex | ||||
| Male | 3,990 | (48.9) | 2,712 | (48.1) |
| Female | 4,050 | (49.6) | 2,871 | (50.9) |
| Unknown | 122 | (1.5) | 58 | (1.0) |
| Pulse, beats/min | ||||
| ≤40 | 742 | (9.1) | 508 | (9.0) |
| 40–80 | 1,724 | (21.1) | 1,175 | (20.8) |
| >80 | 5,454 | (66.8) | 3,830 | (67.9 |
| Unknown | 242 | (3.0) | 128 | (2.3) |
| Systolic blood pressure, mm Hg | ||||
| ≤60 | 1,338 | (16.4) | 952 | (16.9) |
| 61–100 | 1,301 | (15.9) | 947 | (16.8) |
| 101–140 | 2,881 | (28.0) | 1,459 | (25.8) |
| >140 | 2,765 | (33.9) | 1,980 | (35.1) |
| Unknown | 477 | (5.8) | 303 | (5.4) |
| Glasgow Coma Scale score | ||||
| 3–8 | 4,968 | (60.9) | 3,480 | (61.7) |
| 9–12 | 887 | (10.9) | 621 | (11.0) |
| 13–15 | 1,994 | (24.4) | 1,352 | (24.0) |
| Unknown | 313 | (3.8) | 188 | (3.3) |
| Rescuer cumulative patient contacts (2000–2005), No. | ||||
| <1,000 | 2,456 | (30.1) | 1,479 | (26.2) |
| 1,001–2,000 | 2,329 | (28.5) | 1,615 | (28.6) |
| 2,001–4,000 | 2,242 | (27.5) | 1,671 | (29.6) |
| >4,000 | 1,135 | (13.9) | 876 | (15.5) |
| EMS agency population setting | ||||
| Nonurban | 4,070 | (49.8) | 2,747 | (48.7) |
| Urban† | 3,237 | (39.7) | 2,562 | (45.4) |
| Air medical | 847 | (10.4) | 327 | (5.8) |
| Unknown | 8 | (0.1) | 5 | (0.1) |
| Year | ||||
| 2003 | 2,842 | (24.8) | 1,947 | (34.5) |
| 2004 | 2,778 | (34.0) | 1,913 | (33.9) |
| 2005 | 2,542 | (31.1) | 1,781 | (31.6) |
|
Cumulative tracheal intubation experience (2000–2005) of rescuer performing tracheal intubation, No. |
||||
| 1–10 | 2,482 | (30.4) | 1,634 | (29.0) |
| 11–25 | 3,342 | (41.0) | 2,327 | (41.2) |
| 26–50 | 1,953 | (23.9) | 1,398 | (24.8 |
| >50 | 385 | (4.7) | 282 | (5.0) |
| Patient outcome (survival; linked cases only) | ||||
| Alive | N/A | N/A | 3,534 | (62.7) |
| Dead | N/A | N/A | 2,107 | (37.3) |
Column for linked cases reflects patients linked to hospital or death records in any of the 5 imputed data sets.
EMS agency located in Allentown, Erie, Harrisburg, Lancaster, Philadelphia, Pittsburgh, Reading, Wilkes-Barre, or York areas.
Acknowledgments
Funding and support: This study was supported by National Heart, Lung, and Blood Institute grant R21-HL084528. Dr. Wang received support from Clinical Scientist Development Award K08-HS013628 from the Agency for Health Care Research and Quality, Rockville, MD. The funders had no direct role in the design or execution of the study or the composition of the resulting article.
Footnotes
Author contributions: HEW conceived the study. HEW, JRL, and DMY designed the study. HEW obtained the data. LJC performed data set linkage. HEW, GKB, and LJC performed the analysis. HEW drafted the article, and all authors contributed substantially to its revision. HEW had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. HEW takes responsibility for the paper as a whole.
By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article that might create any potential conflict of interest. See the Manuscript Submission Agreement in this issue for examples of specific conflicts covered by this statement.
Presented at the National Association of EMS Physicians annual meeting, January 2009, Jacksonville, FL.
REFERENCES
- 1.Jacobs LM, Berrizbeitia LD, Bennett B, et al. Endotracheal intubation in the prehospital phase of emergency medical care. JAMA. 1983;250:2175–2177. [PubMed] [Google Scholar]
- 2.Stewart RD, Paris PM, Winter PM, et al. Field endotracheal intubation by paramedical personnel. Success rates and complications. Chest. 1984;85:341–345. doi: 10.1378/chest.85.3.341. [DOI] [PubMed] [Google Scholar]
- 3.De Leo BC. Endotracheal intubation by rescue squad personnel. Heart Lung. 1977;6:851–854. [PubMed] [Google Scholar]
- 4.Guss DA, Posluszny M. Paramedic orotracheal intubation: a feasibility study. Am J Emerg Med. 1984;2:399–401. doi: 10.1016/0735-6757(84)90041-x. [DOI] [PubMed] [Google Scholar]
- 5.Wang HE, Kupas DF, Greenwood MJ, et al. An algorithmic approach to prehospital airway management. Prehosp Emerg Care. 2005;9:145–155. doi: 10.1080/10903120590924618. [DOI] [PubMed] [Google Scholar]
- 6.Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32–37. doi: 10.1067/mem.2001.112098. [DOI] [PubMed] [Google Scholar]
- 7.Wang HE, Lave JR, Sirio CA, et al. Paramedic intubation errors: isolated events or symptoms of larger problems? Health Aff (Millwood) 2006;25:501–509. doi: 10.1377/hlthaff.25.2.501. [DOI] [PubMed] [Google Scholar]
- 8.Wang HE, Yealy DM. How many attempts are required to accomplish out-of-hospital endotracheal intubation? Acad Emerg Med. 2006;13:372–377. doi: 10.1197/j.aem.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Davis DP, Dunford JV, Poste JC, et al. The impact of hypoxia and hyperventilation on outcome after paramedic rapid sequence intubation of severely head-injured patients. J Trauma. 2004;57:1–8. doi: 10.1097/01.ta.0000135503.71684.c8. discussion 8–10. [DOI] [PubMed] [Google Scholar]
- 10.Aufderheide TP, Lurie KG. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32(9 suppl):S345–S351. doi: 10.1097/01.ccm.0000134335.46859.09. [DOI] [PubMed] [Google Scholar]
- 11.Aufderheide TP, Sigurdsson G, Pirrallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960–1965. doi: 10.1161/01.CIR.0000126594.79136.61. [DOI] [PubMed] [Google Scholar]
- 12.Luft HS. Hospital Volume, Physician Volume, and Patient Outcomes: Assessing the Evidence. Ann Arbor, MI: Health Administration Press; 1990. [Google Scholar]
- 13.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? a systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 14.Kelly JV, Hellinger FJ. Heart disease and hospital deaths: an empirical study. Health Serv Res. 1987;22:369–395. [PMC free article] [PubMed] [Google Scholar]
- 15.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 16.Nathens AB, Jurkovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285:1164–1171. doi: 10.1001/jama.285.9.1164. [DOI] [PubMed] [Google Scholar]
- 17.Smith RF, Frateschi L, Sloan EP, et al. The impact of volume on outcome in seriously injured trauma patients: two years’ experience of the Chicago Trauma System. J Trauma. 1990;30:1066–1075. doi: 10.1097/00005373-199009000-00002. discussion 1075–1076. [DOI] [PubMed] [Google Scholar]
- 18.Spaite D, Benoit R, Brown D, et al. Uniform prehospital data elements and definitions: a report from the Uniform Prehospital Emergency Medical Services Data Conference. Ann Emerg Med. 1995;25:525–531. doi: 10.1016/s0196-0644(95)70271-7. [DOI] [PubMed] [Google Scholar]
- 19. [Accessed March 20, 2008];Pennsylvania Health Care Cost Containment Council. Available at: http://www.phc4.org. [Google Scholar]
- 20. [Accessed January 8, 2010];Pennsylvania Department of Health, Bureau of Health Statistics and Research, Death registration. Available at: http://www.portal.state.pa.us/portal/server.pt/community/death_registration/14278. [Google Scholar]
- 21.Fellegi I, Sunter A. A theory for record linkage. J Am Stat Assoc. 1969;64:1183–1210. [Google Scholar]
- 22.Jaro MA. Probabilistic linkage of large public health data files. Stat Med. 1995;14:491–498. doi: 10.1002/sim.4780140510. [DOI] [PubMed] [Google Scholar]
- 23.Newcombe H, Kennedy J. Record linkage. Commun Assoc Computing Machinery. 1962;5:563–566. [Google Scholar]
- 24.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 25.Cercarelli LR, Rosman DL, Ryan GA. Comparison of accident and emergency with police road injury data. J Trauma. 1996;40:805–809. doi: 10.1097/00005373-199605000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Overpeck MD, Hoffman HJ, Prager K. The lowest birth-weight infants and the US infant mortality rate: NCHS 1983 linked birth/ infant death data. Am J Public Health. 1992;82:441–444. doi: 10.2105/ajph.82.3.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henderson J, Goldacre MJ, Graveney MJ, et al. Use of medical record linkage to study readmission rates. BMJ. 1989;299:709–713. doi: 10.1136/bmj.299.6701.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldacre MJ, Simmons H, Henderson J, et al. Trends in episode based and person based rates of admission to hospital in the Oxford record linkage study area. Br Med J (Clin Res Ed) 1988;296:583–585. doi: 10.1136/bmj.296.6621.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Henderson J, Goldacre MJ, Griffith M. Hospital care for the elderly in the final year of life: a population based study. BMJ. 1990;301:17–19. doi: 10.1136/bmj.301.6742.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Newman TB, Brown AN. Use of commercial record linkage software and vital statistics to identify patient deaths. J Am Med Inform Assoc. 1997;4:233–237. doi: 10.1136/jamia.1997.0040233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cook LJ, Knight S, Olson LM, et al. Motor vehicle crash characteristics and medical outcomes among older drivers in Utah, 1992–1995. Ann Emerg Med. 2000;35:585–591. [PubMed] [Google Scholar]
- 32.McGlincy MH. ASA Proceedings of the Joint Statistical Meetings. Alexandria, VA: American Statistical Association; 2004. A bayesian record linkage methodology for multiple imputation of missing links; pp. 4001–4008. [Google Scholar]
- 33.Cook LJ, Olson LM, Dean JM. Probabilistic record linkage: relationships between file sizes, identifiers and match weights. Methods Inf Med. 2001;40:196–203. [PubMed] [Google Scholar]
- 34.Rubin DB, Schenker N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10:585–598. doi: 10.1002/sim.4780100410. [DOI] [PubMed] [Google Scholar]
- 35.Little RJA, Rubin DB. Statistical Analysis With Missing Data. 2nd ed. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- 36.Sakles JC, Laurin EG, Rantapaa AA, et al. Airway management in the emergency department: a one-year study of 610 tracheal intubations. Ann Emerg Med. 1998;31:325–332. doi: 10.1016/s0196-0644(98)70342-7. [DOI] [PubMed] [Google Scholar]
- 37.Stiell IG, Wells GA, DeMaio VJ, et al. Modifiable factors associated with improved cardiac arrest survival in a multicenter basic life support/defibrillation system: OPALS Study Phase I results. Ontario Prehospital Advanced Life Support. Ann Emerg Med. 1999;33:44–50. doi: 10.1016/s0196-0644(99)70415-4. [DOI] [PubMed] [Google Scholar]
- 38.Ricketts TC. Rural Health in the United States. New York, NY: Oxford University Press; 1999. [Google Scholar]
- 39.Hardin JW, Hilbe J. Generalized Estimating Equations. Boca Raton, FL: Chapman & Hall/CRC; 2002. [Google Scholar]
- 40.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang HE, Kupas DF, Paris PM, et al. Preliminary experience with a prospective, multi-centered evaluation of out-of-hospital endotracheal intubation. Resuscitation. 2003;58:49–58. doi: 10.1016/s0300-9572(03)00058-3. [DOI] [PubMed] [Google Scholar]
- 42.Wang HE, O’Connor RE, Schnyder ME, et al. Patient status and time to intubation in the assessment of prehospital intubation performance. Prehosp Emerg Care. 2001;5:10–18. doi: 10.1080/10903120190940254. [DOI] [PubMed] [Google Scholar]
- 43.Garza AG, Gratton MC, Coontz D, et al. Effect of paramedic experience on orotracheal intubation success rates. J Emerg Med. 2003;25:251–256. doi: 10.1016/s0736-4679(03)00198-7. [DOI] [PubMed] [Google Scholar]
- 44.Wang HE, Simeone SJ, Weaver MD, et al. Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Ann Emerg Med. 2009;54:645–652. doi: 10.1016/j.annemergmed.2009.05.024. e641. [DOI] [PubMed] [Google Scholar]
- 45.Baker SP, Neill BO, Haddon W, et al. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 46.Davis DP, Hoyt DB, Ochs M, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444–453. doi: 10.1097/01.TA.0000053396.02126.CD. [DOI] [PubMed] [Google Scholar]
- 47.Wayne MA, Friedland E. Prehospital use of succinylcholine: a 20-year review. Prehosp Emerg Care. 1999;3:107–109. doi: 10.1080/10903129908958916. [DOI] [PubMed] [Google Scholar]
- 48.Wang HE, Davis DP, O’Connor RE, et al. Drug-assisted intubation in the prehospital setting (resource document to NAEMSP position statement) Prehosp Emerg Care. 2006;10:261–271. doi: 10.1080/10903120500541506. [DOI] [PubMed] [Google Scholar]
- 49.Wang HE, Yealy DM. Out-of-hospital endotracheal intubation: where are we? Ann Emerg Med. 2006;47:532–541. doi: 10.1016/j.annemergmed.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 50.Wang HE, Kupas DF, Hostler D, et al. Procedural experience with out-of-hospital endotracheal intubation. Crit Care Med. 2005;33:1718–1721. doi: 10.1097/01.ccm.0000171208.07895.2a. [DOI] [PubMed] [Google Scholar]
- 51.Johnston BD, Seitz SR, Wang HE. Limited opportunities for paramedic student endotracheal intubation training in the operating room. Acad Emerg Med. 2006;13:1051–1055. doi: 10.1197/j.aem.2006.06.031. [DOI] [PubMed] [Google Scholar]
- 52.Hall RE, Plant JR, Bands CJ, et al. Human patient simulation is effective for teaching paramedic students endotracheal intubation. Acad Emerg Med. 2005;12:850–855. doi: 10.1197/j.aem.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 53.Wang HE, Yealy DM. Human patients or simulators for teaching endotracheal intubation: whom are we fooling? Acad Emerg Med. 2006;13:232. doi: 10.1197/j.aem.2005.10.002. author reply 232–233. [DOI] [PubMed] [Google Scholar]
- 54.Persse DE, Key CB, Bradley RN, et al. Cardiac arrest survival as a function of ambulance deployment strategy in a large urban emergency medical services system. Resuscitation. 2003;59:97–104. doi: 10.1016/s0300-9572(03)00178-3. [DOI] [PubMed] [Google Scholar]
- 55.Thomas JB, Abo BN, Wang HE. Paramedic perceptions of challenges in out-of-hospital endotracheal intubation. Prehosp Emerg Care. 2007;11:219–223. doi: 10.1080/10903120701205802. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.