Abstract
Context
This case series reports the changes in the respiratory health of eight asthmatic subjects and the relationship to air quality associated with the October, 2007 firestorm in San Diego County of California.
Case Presentation
Participants were eight subjects with asthma enrolled in Asthma Clinical Research Network (ACRN) (NIH# U10-HL074218) studies at the University of California San Diego, School of Medicine, (UCSD), who had study data collected immediately prior, during and one month after the five-day firestorm in San Diego County. Air quality deteriorated to an extreme average of 71.5 ug/m3small particulate matter less than 2.5 microns (PM2.5) during the firestorm. Respiratory health data included morning and evening peak expiratory flow rates [PEFR], morning and evening Forced Expiratory Volume in one second [FEV1], rescue medication usage, and sputum eosinophils. Morning and evening PEFR and FEV1 rates remained stable. The two subjects tested during the fires had elevated eosinophil counts and rescue medication usage was increased in five of the eight subjects.
Discussion
Pulmonary function test values were stable during the wildfires for all eight subjects but there was a statistical significant increase in rescue medication usage during the wildfires which correlated with PM 2.5 values. The two subjects tested during the fires showed increases in sputum eosinophil counts consistent with increased airways inflammation.
Relevance
These findings suggests that poor air quality associated with wildfires resulted in an increase airways inflammation in these asthmatic subjects, but pulmonary function tests remained stable, possibly due to increased rescue medication usage. This is especially pertinent as there is an increase in incidence of wildfires this decade.
Keywords: asthma, fire, pollution, particles, eosinophil
Introduction
Over a five day period in October, 2007, five major wildfires burned 369,000 acres in San Diego County and half a million residents were evacuated. With fire, small particle matters < 2.5 microns (PM2.5) are released into the air. These smaller particles cause serious respiratory health problems as they are inhaled deep into the lung.1 Asthma is a prevalent chronic obstructive lung disease2 and it is well documented that increased PM2.5 values are particularly associated with respiratory symptoms in hypersensitive individuals including asthmatics. During the 2003 fires, 28,000 acres were burned with 300,150 tons of particle matter and other pollutants released into the environment.1 The PM2.5 concentrations were found to directly correlate with a significant increase in emergency department visits for asthma and other respiratory illnesses.3
This case series of eight subjects enrolled in the NIH sponsored ACRN clinical trials during the October, 2007 wildfires in San Diego County evaluated the relationship between a sudden increase of environmental PM2.5 and asthmatic airways function by comparing environmental PM2.5 values, with subjects’ pulmonary function, use of rescue medication and sputum eosinophil values measured during the wildfires.
Material and Methods
Study Subjects
A convenience sample of eight subjects with asthma and enrolled in Asthma Clinical Research Network (ACRN) (NIH# U10-HL074218) studies at the University of California San Diego, School of Medicine, (UCSD) were included as they had study data collected one week prior, during and two weeks after the five-day firestorm in San Diego County. Informed consent was obtained according to UCSD Institutional Review Board (IRB) requirements. All subjects were assessed as asthmatics and met the inclusive criteria of their respective ACRN protocols.
Study Design
The case series examined the association between the air quality during wildfires, determined by PM2.5 values, and the respiratory health of asthmatics determined by pulmonary function tests of peak expiratory flow rates [PEFR] and forced expired volume in one second [FEV1], rescue medicine use of an inhaled short-acting bronchodilator (albuterol) and sputum eosinophil counts. Eight subjects had complete datasets and two subjects had sputum eosinophil counts collected during the period of the fires. Data reported is for the four days prior to the fire, October 14-18, 2007, during the fires, October 22 – 26, 2007 and two weeks afterwards from November 13 – 17, 2007.
Methods
Air Quality
PM2.5, temperature and humidity values were collected at the Downtown San Diego station. All subjects resided within twenty-five miles. The PM2.5 values for before, during, and after the wildfires were retrospectively collected through the County of San Diego - Air Pollution Control District’s website at http://www.sdapcd.org/air/air_quality.html.4
Pulmonary Function Tests --PEFR and FEV1 Values: All eight subjects were provided with a take-home Jaeger Asthma Monitor AM1 and used it adequately before, during, and after the wildfires. Subjects demonstrated proficiency with the device and were instructed to use the monitor two times each day: once in the morning and once at night. The subjects were instructed to record the values in a diary. Only subjects that were compliant (>75% usage) were included in the study.
Rescue Medication Usage
Sputum Eosinophil Values
Values were collected for two subjects using the standard ACRN protocol [ACRN Macrolides in Asthma Study, 2006]
Analysis
Wilcoxon signed-rank test analyses, a non-parametric alternative to the paired t-test, were computed using a commercially available software package (SYSTAT Software, Inc, Ver 12, Chicago, IL). Variables were considered significantly different when the p-value was 0.05 or less.
Results
Subjects
The average age was 36 ± 10 years with a reported history of asthma for an average of 24 ± 12 years. Distance of their residence from the downtown air quality station was an average of 10 ± 6 miles.
Air Quality
Mean environmental PM2.5 values ranged from a baseline of 11.0ug/m3 pre-fires, 71.5ug/m3 during the firestorm and down to 18.1ug/m3 two weeks after the firestorm. There was a statistical significant increase in PM2.5 values during the wildfires compared to before the wildfires both during the day and at night (Table 1, p<0.005). Temperature was significantly elevated during the fires (p < 0.007) with a significantly reduced percent humidity (p < 0.008, Table 1).
Table 1.
Mean and standard deviations of pulmonary function test values, medication use, and air particle mass by time period
| Measure | Baseline | Fires | Post | Difference Baseline-Firesa |
Difference Baseline- Posta |
|---|---|---|---|---|---|
| FEV1 (AM) | 2.23 ± 0.42 | 2.19 ± 0.46 | 2.24 ± 0.36 | 0.35 | 0.44 |
| FEV1 (PM) | 2.17 ± 0.31 | 2.22 ± 0.43 | 2.17 ± 3.54 | 0.86 | 0.93 |
| Peak Flow (AM) | 411 ± 91 | 404 ± 91 | 400 ± 88 | 0.40 | 0.16 |
| Peak Flow (PM) | 384 ± 91 | 406 ± 88 | 405 ± 97 | 0.50 | 0.9 |
| Rescue Medication | 3 subjects | 5 subjects | 5 subjects | b | b |
| Average # rescue medication doses of users |
0.9 ± 1.3 | 2.6 ± 2.0 | 1.6 ± 1.3 | 0.03 | 0.14 |
| PM2.5 (AM) | 11.0 ± 5.3 | 71.8 ± 24.5 | 18.5 ± 12.8 | 0.005 | 0.005 |
| PM2.5 (PM) | 7.8 1.0 | 59 ± 11.2 | 18.5 ± 1.7 | 0.005 | 0.005 |
| Average Temperature degress Fahrenheit |
63.4 ± 0.9 | 76.6 ± 5.2 | 63.8 ± 4.9c | 0.007 | 0.707 |
| Average % humidity | 76.6 ± 5.2 | 29.2 ± 7.9 | 55.8 ± 14.3c | 0.008 | 0.03 |
significance value presented.
Data is nominal therefore analysis not performed.
p value = 0.01 between time period of fires and post fires
FEV1 = Forced expiratory volume in one second
PM2.5 = particle matter < 2.5 microns in diameter
Morning Pulmonary Function Tests
There were no significant changes in morning pulmonary function measures during the wildfires compared to pre or post fire periods. Morning PEFR values (Table 1, p = 0.40) and FEV1 (p < 0.35) remained consistent. There was no correlation between morning PM2.5 values and morning PEFR values or FEV1 values.
Night Pulmonary Function Tests
There were no significant changes in night pulmonary function tests as measured by PEFR or FEV1 (Table 1).
Rescue Medication Usage
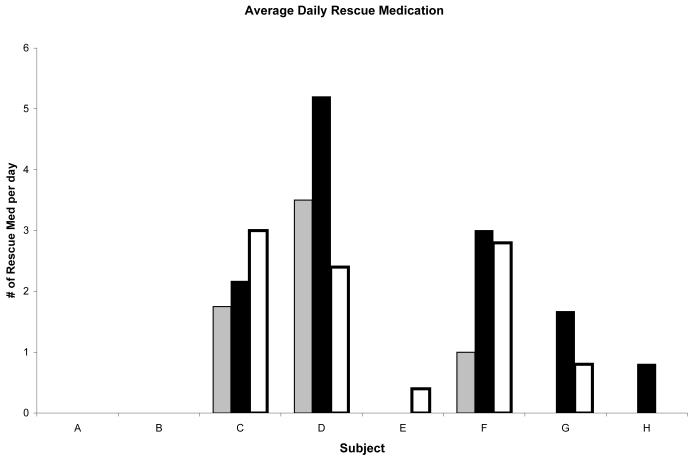
Two subjects reported no rescue medication use during the study period. There was an increase in number of doses from baseline (Average # doses: 0.94 ± 1.3 doses per day) to both during the fires (2.6 ± 2.0 doses per day; p = 0.03), and remained elevated post fires (1.6 ± 1.3 doses per day), figure 1.
Figure 1. Average number of doses per day of short-acting albuterol (asthma rescue medication) by the individual subjects (labeled A-H on x axis).
X-axis is individual subject. Light white bars = pre-fire, dark bars = during the fire and grey bars = post fires.
Sputum eosinophils
For the two subjects monitored, there was a significant increase in sputum eosinophil values (Table 2).
Table 2.
Sputum Eosinophil Values (Cell Count Percentage) and Differences for Subjects Before and During the Wildfires
| Subject | Pre-Fire | During Fires | Percent Difference |
|---|---|---|---|
| A | 0.20 | 7.80 | increase of 3800% |
| B | 2.40 | 3.00 | increase of 25% |
Discussion
The collection of data for the ACRN studies during the time of the wildfires in San Diego County provided a unique opportunity for evaluating the effect of these catastrophic fires on lung function and markers of inflammation in civilian asthmatics. Since all asthmatic subjects completed these tests and diaries while they were exposed to naturally occurring wildfires, the data they generated provides insights into how environmental changes associated with wildfires impact respiratory physiology changes on a real time basis.
Our observations suggest that the increases in wildfire associated PM2.5 values caused by the October, 2007 San Diego wildfires may have led to an increase in airways inflammation in asthmatics. Serial PEFR and FEV1 measures in real time remained stable, perhaps masked by significant increases in rescue medication usage.
There are various methods for determining how the poor air quality produced by wildfires affects the respiratory health of asthmatics. Previous studies have used real-time pulmonary function tests, specifically FEV1 values and PEFR values. However, to our knowledge, no study has yet used sputum eosinophil counts. This case series had access to both real-time pulmonary function tests and sputum is eosinophil counts. Sputum eosinophil counts during the wildfires offer the possibility of directly monitor airways inflammation.5 The wildfires were associated with marked increases sputum eosinophil values of the two subjects available for study (Table 2). This is a very limited sample is consistent with an inflammatory response. It is impossible to say whether this was a direct response to the fire or part of the subjects’ underlying inflammatory process. It is interesting that increased sputum eosinophilia has been reported in occupational asthma, another asthma syndrome usually precipitated by airway irritants or chemicals as opposed to specific allergens.6 Our findings suggest that sputum eosinophil may be an important area for future study in trying to understand the airway’s response to wildfires in asthmatics. Possibly that real time PEFR and FEV1 measures did not decrease during the wildfires because of significant increase in rescue medication usage. If we were to observe only PFT measures, increases in inflammation may have been overlooked.
While previous studies have shown that increased PM2.5 values are associated with negative respiratory health, a report of measurements of PEFR during a Sydney Australia bushfire in 1994 indicated that a large increase in environmental PM values had little or no effect on asthmatics’ PEFR values in real time.7 Use of rescue medication was not reported in that study.
It is important to consider the limitations of our observations. First, we had the small sample size of two subjects for sputum eosinophil measures. The repeated measures design allowed for comparison within subjects, with baseline measurements serving as the control period. Thus, the data from our study is anecdotal. In future studies, it would be important to assess the sputum eosinophil count during real-time wildfires in a larger sample size to draw meaningful conclusions. However, we present this study as empirical data because we were fortunate to have taken measures of the respiratory health of asthmatics during an unprepared for, natural disaster. Second, it is possible that the increased sputum eosinophil values were caused by factors other than fire-induced-asthma, including parasite infections and allergies. In the future, IgE values could be observed to better assess the asthmatic and/or allergic response. Third, observations of quality and quantity of fire exposure would enlighten the data presented; for example, how much time each subject was outdoors versus indoors and what kind of air filters were used if used at all. However, this data was not warranted in the parent ACRN protocol and thus was not included. Fourth, our data only represents asthmatics that did not evacuate from San Diego. It is possible that those who fled San Diego may have suffered from a larger degree of inflammation and may have used their inhalers to a larger extent than depicted by our data because of their proximity to the concentrated smoke.
Conclusion
The overall data in this case series suggests that the wildfires may have resulted in subjects’ airways inflammation and suggests that the symptoms and degree of pulmonary function abnormality are easily controlled with albuterol usage. We recommend that further studies be conducted to understand the pulmonary pathology in asthmatics caused by wildfires, the role of sputum eosinophil counts in future environmental asthma studies, and the most appropriate treatment options available for asthmatics exposed to wildfires. It seems evident that asthmatics that live in areas highly susceptible to wildfires should have immediate access to rescue medication to attempt reversing the effects of the poor atmospheric conditions; our case series warrants further investigation.
ACKNOWLEDGEMENTS
Funded in part by NHLBI Asthma Clinical Research Center, #U10-HL074218
Work was performed at University of California, San Diego
Dr. Ramsdell received support from the Asthma Clinical Research Network, (NIH# U10-HL074218), where the convenience sample was drawn.
ABBREVIATIONS
- ACRN
Asthma Clinical Research Network
- FEV1
Forced expiratory volume in one second
- PM2.5
small particle matters < 2.5 microns
- PEFR
peak expiratory flow rates
- UCSD
University of California San Diego
Footnotes
Declaration of interest
The authors report no conflict of interest.
DISCLAIMER: The authors report no conflicting interest
References
- 1.Clinton N, Scott K, Gong P. Southern California Fires – GIS Estimation of Fuels and Air Quality Impacts. Atmospheric Environment. 2006;40:3686–3695. [Google Scholar]
- 2.National Heart, Lung, and Blood Institute. National Institutes of Health International consensus report on diagnosis and treatment of asthma. Eur. Respir. J. 1992 March;5(5):601–641. Bethesda, Maryland 20892. Publication no. 92-3091. [PubMed] [Google Scholar]
- 3.Viswanathan S, Eria L, Diunugala N, Johnson J, McClean C. An Analysis of Effects of San Diego Wildfire on Ambient Air Quality. J Air Waste Management Association. 2006;56(1):56–67. doi: 10.1080/10473289.2006.10464439. [DOI] [PubMed] [Google Scholar]
- 4.Pollutant Data Archive. Air Pollution Control District; County of San Diego: Retrieved November, 2007. http://www.sdapcd.org/air/air_quality.html. [Google Scholar]
- 5.Carroll N, Cooke C, James A. The distribution of eosinophils and lymphocytes in the large and small airways of asthmatics. Eur. Respir. J. 1997;10:292–300. doi: 10.1183/09031936.97.10020292. [DOI] [PubMed] [Google Scholar]
- 6.Vandenplas O, D’Alpaos V, Heymans J, Jamart J, Thimpont J, Huaux F, Lison D, Renauld JC. Sputum eosinophilia: an early marker of bronchial response to occupational agents. Allergy. 2009 May;64(5):754–61. doi: 10.1111/j.1398-9995.2008.01896.x. Epub 2009 Feb 12. [DOI] [PubMed] [Google Scholar]
- 7.Jalaludin B, Smith M, O’Toole B, Leeder S. Acute effects of bushfires on peak expiratory flow rates in children with wheeze: a time series analysis. Australian and New Zealand Journal of Public Health. 2000;24(2):174–177. doi: 10.1111/j.1467-842x.2000.tb00138.x. [DOI] [PubMed] [Google Scholar]