Abstract
Background
Hypergammaglobulinemia is frequently observed in patients with chronic liver disease (CLD) of different causes. On the other hand, elevated levels of serum immunoglobulin G (IgG) are the best diagnostic marker for autoimmune hepatitis (AIH). Thus, the ability to distinguish AIH patients from patients with other liver disease, especially patients with advanced liver cirrhosis, is important since most AIH patients will a have favorable treatment response if diagnosed properly.
Objective
We conducted this study to evaluate the significance of elevated IgG levels in patients with non-autoimmune CLD and to compare these IgG levels with those in patients with AIH upon diagnosis.
Setting and study population
The serum IgG levels in 27 patients with AIH determined at the time of diagnosis were compared to the serum IgG levels in 27 patients with other CLDs of variable severity at the King Abdul Aziz University Hospital in Jeddah, Saudi Arabia. Severity of the disease was evaluated in all patients.
Results
We found that the patients in the CLD group with decompensated cirrhosis had significantly higher serum IgG levels compared to the compensated CLD patients (p <0.02). In addition, the AIH patients had significantly higher serum IgG levels than the non-autoimmune hepatitis CLD patients and the decompensated cirrhosis patients in the CLD group (p <0.001 and p <0.044, respectively). Most patients with elevated serum IgG of the AIH group (67%) and the CLD group (75%) had significant hypergammaglobulinemia, not just isolated elevated IgG levels.
Conclusion
Elevated serum IgG levels with hypergammaglobulinemia are commonly found in patients with advanced CLD. The differentiation of such cases from AIH is important in order to avoid misdiagnosis and confusion with AIH.
Keywords: decompensated cirrhosis, hypergammaglobulinemia, chronic hepatitis C, compensated cirrhosis
Chronic liver diseases (CLD), especially decompensated cirrhosis, are recognized by abnormal immunological responses, including autoantibodies and hypergammaglobulinemia (1). Hypergammaglobulinemia is thought to be a marker for histologically advanced forms of fibrosis (2) and may play a role in the progression of liver disease (3). It has been suggested that hypergammaglobulinemia in CLD patients is due to the diminished removal of immunoglobulins by the diseased liver (4). On the other hand, elevated levels of immunoglobulins G and M (IgG and IgM) are important diagnostic markers for autoimmune hepatitis (AIH) and primary biliary cirrhosis (PBC), respectively (5, 6). The diagnosis of AIH is based on the criteria that were established and modified by the international AIH group, which include predominant elevation in the levels of serum aminotransferases, negative markers for viral hepatitis, the exclusion of genetic liver diseases, the absence of toxic or alcohol liver injury, the presence of autoantibodies for AIH, elevated levels of serum IgG, and histological features of AIH (7). A serum IgG level of 1.5-fold greater than the normal level, and more recently 1.1-fold greater than the normal level, have been accepted as diagnostic criteria for AIH (6, 8). Although serum IgG is not the only diagnostic marker for AIH, a level of 1.44-fold greater than normal was found to be the best diagnostic predictor of AIH (8). High serum IgG levels in patients with advanced cirrhosis (where liver biopsy may not be helpful or may be difficult because of coagulopathy), absence of viral markers and negative screening for genetic disorders represent diagnostic difficulties that may lead to confusion with AIH, especially in patients with autoantibodies-negative AIH (about 20% of patients with AIH) (9). Correct diagnosis of AIH is important because even patients with advanced AIH, if properly diagnosed, will have a favorable treatment response (10). The aim of this study was to evaluate the significance of elevated serum IgG levels in patients with non-AIH CLD and to compare these levels to the IgG levels found in patients with AIH at the time of diagnosis.
Subjects and methods
A cohort comparative study was performed to compare the IgG levels in patients with AIH at the time of diagnosis and the IgG levels in patients with other liver disease.
Study population
Patients followed at the hepatology clinic in King Abdul Aziz University Hospital and who were either diagnosed with AIH based on the international scoring system (the AIH group) or were diagnosed with CLD due to other causes (the CLD group) were included in this study.
Procedure
The data were collected from May to December 2008. We reviewed the charts of 34 patients with AIH who were diagnosed between 1995 and 2008 (AIH group). The patients were eligible for this study if the diagnosis of AIH was definite, if the levels of serum IgG at the time of diagnosis were available in the records and if the records were complete regarding clinical, immunological, and biochemical data. Patients with incomplete data and those who did not have their serum IgG levels recorded at the time of diagnosis were excluded. We obtained the data regarding the clinical presentations at the time of diagnosis (whether compensated or decompensated) and liver biochemical parameters, which included serum levels of alanine aminotransferase (ALT), aspartate amino transferase, alkaline phosphatase, gamma-glutamyl transferase, total protein, albumin, and the total and direct bilirubin. We also obtained the complete blood count (CBC) and the prothrombin time. We also reviewed the serum autoimmune profiles, which included antinuclear antibody (ANA) that were weakly positive (1/40) and strongly positive (1/1,280), smooth muscle antibody (SMA), liver kidney microsomal-1 antibodies (LKM-1), and antimitochondrial antibodies (AMA). Moreover, we looked at the immunological viral markers, the IgG levels that were determined at the time of diagnosis by nephelometry, and the results of the liver biopsies, if available.
Twenty-seven patients with other liver diseases (compensated or decompensated) who agreed to provide blood samples for testing serum IgG levels were also included (CLD group). We assessed these patients clinically, performed liver biochemical tests, and measured serum IgG levels like we did for the AIH patient group. The cause of liver disease in the CLD group was defined by reviewing the biochemical, serological and immunological data, and the liver biopsy results. For all patients in the AIH and CLD groups, we used the clinical and biochemical markers (ascites, hepatic encephalopathy, serum albumin, total bilirubin, and prothrombin time) to calculate the Child–Pugh score. All of the patients were checked for the presence of autoimmune diseases other than AIH.
Statistical analysis
We used the statistical package for the social sciences (SPSS 15) to determine the mean, standard deviation, and frequencies. We used the independent t-test to compare the parametric variables, where a p-value < 0.05 was considered statistically significant. In addition, we used the Receiver Operating Characteristic (ROC) curve to compare the serum IgG levels between patients in the AIH and CLD groups.
Results
Between 1995 and 2008, 34 patients had been diagnosed at the hospital with AIH type 1 based on the AIH diagnostic criteria and the response to therapy (the AIH group). Of these, 27 patients were included in this study after exclusion of seven patients because data on serum IgG levels at the time of diagnosis were missing. Twenty-seven patients with other liver diseases were randomly selected from the hepatology department's in- and out-patient sections. The mean age of patients in the AIH group was 33 years (range 12–65 years) while the mean age for the CLD group with other liver disease was 45.2 years (range 16–75 years). Most of the patients were females in both the AIH group (22; 81%) and the CLD group (16; 59.3%). Notably, 48% of the patients in the AIH group and 52% of patients in the CLD group had decompensated cirrhosis. In addition, 26 patients (96.2%) of the AIH group and 16 patients (59.2%) of the CLD group had elevated levels of serum IgG.
The mean value of serum IgG in the AIH group was 30.6 g/L±13.248 standard deviation (range 14.3–66 g/L), which is 1.9-fold greater than the upper limit of the normal range. The mean IgG level of the patients in the CLD group was 19.2 g/L±7.838 standard deviation (range 6.28–39.366 g/L), which is 1.19-fold greater than the upper limit of the normal range. The difference between the two groups was statistically significant (p <0.001). Similarly, decompensated cirrhosis patients in the AIH group had significantly higher levels of serum IgG than the decompensated cirrhosis patients of the CLD group (p = 0.044).
Ten of the 14 (78.3%) patients in the CLD group with decompensated cirrhosis had elevated levels of serum IgG, while only five of 13 (34.4%) patients from the compensated CLD patients had elevated levels of serum IgG. In the CLD group, the decompensated cirrhosis patients had a significantly higher (p <0.02) level of IgG (25.3 g/L) than the compensated CLD patients (16.92 g/L). By contrast, in the AIH group the serum IgG levels in those with compensated cirrhosis (32.59 g/L±16.1494) was higher (p = 0.036) than in those with decompensated cirrhosis (28.59 g/L±9.149).
In addition, 67% of the patients in the AIH group had hypergammaglobulinemia rather than isolated high IgG levels while 12 of 16 patients (75%) with elevated levels of IgG in the CLD group had hypergammaglobulinemia.
Furthermore, eight patients in the AIH group had acute hepatitis at presentation that was reflected by serum ALT levels and an AST concentration of more than 500–1,000 IU/L, but all of the patients in the CLD group had CLD.
The autoimmune profiles of the AIH group showed strongly positive ANA in eight patients (29.6%) and moderately positive ANA in 11 patients (40.74%), while the rest of the AIH patients were weakly positive for ANA. SMA was strongly positive in seven patients (25.9%), moderately positive in 17 patients (62.9%), and negative in the rest of the AIH patients. Furthermore, one patient in the AIH group was positive for LKM-1 and all of them were negative for AMA. For the CLD group, 17 patients were tested for ANA and 10 of them (58.8%) were weakly positive (1:40–1:160), two were moderately positive (one of them had Grave's disease), and the rest were negative. Nine patients from the CLD group were tested for SMA and only one of them demonstrated a weakly positive result.
Liver biopsy results were obtained for 15 patients from the AIH group, and all of them were consistent with a diagnosis of AIH. The remaining patients of the AIH group did not have a liver biopsy performed either because of an advanced stage of the disease that was coupled with severe coagulopathy or because they refused the liver biopsy procedure.
Five patients of the AIH group had systemic lupus erythematosus (SLE), one patient of the CLD group had Grave's disease, and one had PBC. The most common cause of liver disease in the CLD group was chronic hepatitis C (Table 1).
Table 1.
The causes of liver disease in CLD group
| Frequency | Percentage (%) | |
|---|---|---|
| Hemochromatosis | 2 | 7.4 |
| Chronic hepatitis C | 12 | 44.4 |
| Chronic hepatitis B | 5 | 18.5 |
| Primary intrahepatic familial cholestasis | 1 | 3.7 |
| Non-alcoholic steatohepatitis | 2 | 7.4 |
| Congenital liver fibrosis | 1 | 3.7 |
| Primary biliary cirrhosis | 1 | 3.7 |
| Bilharzial liver disease | 3 | 11.1 |
| Total | 27 | 100.0 |
Discussion
We show that patients with CLD other than AIH also tend to have elevated serum IgG levels with or without hypergammaglobulinemia, and that patients with decompensated cirrhosis (51.8% in our study) are more likely to have elevated serum IgG levels as compared to patients with compensated CLD. This may indicate that elevated serum IgG levels are related to the severity of liver disease rather than to its cause. These findings are similar to the data reported for patients with chronic hepatitis C (11, 12). Similarly, the most common cause for CLD in our study was chronic hepatitis C. Immune activation with positive autoantibodies of variable levels, including ANA, SMA, LKM-1, and AMA, is another feature of non-AIH CLD (13, 14). The combination of both hypergammaglobulinemia and positive autoantibodies may confuse the diagnosis of non-AIH CLD with that of AIH, especially in patients with advanced liver cirrhosis.
Most of the patients with elevated levels of IgG, in both groups but particularly in the CLD group (75%), had hypergammaglobulinemia rather than elevated levels of serum IgG. Watt and colleagues related similar findings to the extent of fibrosis and a possible role of immunoglobulins in the progression of liver disease (3).
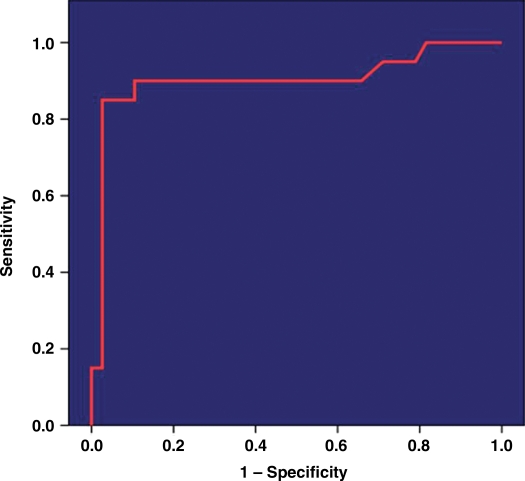
Overall, patients with AIH had serum mean IgG levels that were significantly higher than in patients with other liver diseases. Using the mean serum IgG level for the AIH group (30.6 g/L), we obtained a sensitivity of 90–98% and a specificity of about 96% for the diagnosis of AIH patients (Fig. 1). In our cohort, 81.4% of the patients with AIH had serum IgG levels above the mean level of the CLD group, but on the other hand, three patients (11%) of the CLD group had serum IgG levels equal to or higher than the mean of the AIH group. The importance of such findings in CLD patients with negative viral markers, mildly to moderately elevated levels of autoantibodies (13, 14) and advanced disease where liver biopsy may not be helpful, is to avoid the potential confusion in diagnosing these patients with AIH. These aforementioned three patients were administered trial doses of Prednisolone, but none of them responded to treatment. On the other hand, 10 patients from the AIH group with advanced cirrhosis had favorable responses to the treatment with Prednisolone and Azathioprine.
Fig. 1.
ROC curve for serum IgG level in autoimmune hepatitis compared to other chronic liver disease. Area under the curve equals 0.902.
One patient in the CLD group had chronic hepatitis C and he was treated with a combination of Pegylated interferon and Ribavirin and had a rapid virologic response (RVR), his post treatment serum IgG level was normal (15.2 g/L). Maruyama and colleagues showed that the serum IgG levels in chronic Hepatitis C patients who responded to treatment were reduced compared to non-responders (2). On the other hand, the response to treatment in patients with AIH will be predicted by the reduction of the serum ALT, AST, and IgG levels (10).
The limitation of our study is the small sample size. Similar studies with a larger number of patients may help in defining the cut-off level of IgG that can help in differentiating patients with AIH from patients with other advanced liver diseases. This would be of value because using the most recently published diagnostic criteria, an AIH IgG level of 1.1-fold greater than the normal value is given two points out of six for the diagnosis of AIH (8).
Conclusion
Hypergammaglobulinemia with significantly elevated levels of IgG is a common finding in patients with advanced liver cirrhosis of different etiologies. This may result in the misdiagnosis of AIH in some patients. Studies on larger number of patients may help to define a cut-off level of IgG in order to differentiate between advanced cirrhosis due to AIH and other causes of liver disease associated with high IgG.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.Wegener M, Neuhausen P, Börsch G, Ricken D. Significance of serum immunoglobulins for the diagnosis of alcohol-induced liver diseases. Dtsch Med Wochenschr. 1986;111:1716–20. doi: 10.1055/s-2008-1068698. [DOI] [PubMed] [Google Scholar]
- 2.Maruyama S, Hirayama C, Horie Y, Yorozu K, Maeda K, Inoue M, et al. Serum immunoglobulins in patients with chronic hepatitis C: a surrogate marker of disease severity and treatment outcome. Hepatogastroenterology. 2007;54:493–8. [PubMed] [Google Scholar]
- 3.Watt K, Uhanova J, Gong Y, Kaita K, Doucette K, Pettigrew N, et al. Serum immunoglobulins predict the extent of hepatic fibrosis in patients with chronic hepatitis C virus infection. J Viral Hepat. 2004;11:251–6. doi: 10.1111/j.1365-2893.2004.00507.x. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka S, Okamoto Y, Yamazaki M, Mitani N, Nakqjima Y, Fukui H. Significance of hyperglobulinemia in severe chronic liver diseases – with special reference to the correlation between serum globulin/IgG level and ICG clearance. Hepatogastroenterology. 2007;54:2301–5. [PubMed] [Google Scholar]
- 5.Czaja AJ. Diagnosis and therapy of autoimmune liver disease. Med Clin North Am. 1996;80:973–94. doi: 10.1016/s0025-7125(05)70476-4. [DOI] [PubMed] [Google Scholar]
- 6.Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929–38. doi: 10.1016/s0168-8278(99)80297-9. [DOI] [PubMed] [Google Scholar]
- 7.Bogdanos D, Invernizzi P, Mackay I, Vergani D. Autoimmune liver serology current diagnostic and clinical challenge. World J Gastroenterol. 2008;14:3374–87. doi: 10.3748/wjg.14.3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;48:169–76. doi: 10.1002/hep.22322. [DOI] [PubMed] [Google Scholar]
- 9.Johnson PJ, McFarlane IG. Meeting report: International Autoimmune Hepatitis Group. Hepatology. 1993;18:998–1005. doi: 10.1002/hep.1840180435. [DOI] [PubMed] [Google Scholar]
- 10.Czajal A, Freese D. Diagnosis and treatment of autoimmune hepatitis. Hepatology. 2002;36:479–97. doi: 10.1053/jhep.2002.34944. [DOI] [PubMed] [Google Scholar]
- 11.Gonzàlez-Quintela A, Alende MR, Gamallo R, Gonzàlez-Gil P, López-Ben S, Tomé S, et al. Serum immunoglobulins (IgG, IgA, IgM) in chronic hepatitis C. A comparison with non-cirrhotic alcoholic liver disease. Hepatogastroenterology. 2003;50:2121–6. [PubMed] [Google Scholar]
- 12.El-Kady IM. Assessment of humoral immune response in patients with chronic hepatitis C virus infection. Egypt J Immunol. 2004;11:141–7. [PubMed] [Google Scholar]
- 13.Bayraktar Y, Bayraktar M, Gurakar A, Hassanein TI, Van Thiel DH. A comparison of the prevalence of autoantibodies in individuals with chronic hepatitis C and those with autoimmune hepatitis: the role of interferon in the development of autoimmune diseases. Hepatogastroenterology. 1997;44:417–25. [PubMed] [Google Scholar]
- 14.Ghonaim M, Al-Ghamdi A, El-Bana H, Bakr A, Ghoneim E, El-Edel R, et al. Autoantibodies in chronic liver disease. Egypt J Immunol. 2005;12:101–11. [PubMed] [Google Scholar]