Abstract
Introduction
Penetrating hand injuries are common and improper assessment can result in missed foreign bodies. These bodies can result in a wide range of complications.
Aim
The aim of our study was to study the profile of patients reporting with missed foreign bodies in the hand.
Materials and methods
All the cases treated in the Department of Surgery, Sheri Kashmir Institute of Medical Sciences (medical college), Kashmir, for missed foreign bodies in hands from June 2003 to May 2009 were studied retrospectively.
Results
A total of 61 cases with missed foreign bodies of different nature were treated over the period of six years. Wooden splinters were the most common foreign bodies missed. Preoperative localization was accomplished with plain radiographs and ultrasonograms. Most of the cases were treated on outpatient basis.
Conclusions
Foreign bodies should be suspected and ruled out in all cases of penetrating injuries of hands. Missed foreign bodies need to be removed after proper localization by imaging.
Keywords: foreign body, radio-opaque, splinter, exploration, complication
Accidental penetration of foreign bodies in the hand is common particularly in labor class and most of the times these foreign bodies are removed without any sequelae. However, if missed initially, these foreign bodies may get retained in the tissues to remain dormant or else result in wide range of complications. Missing the foreign bodies is not uncommon (1, 2) and this entity is deemed as one of the major causes of medical litigations (3–5). In recent years, multiple clinical and experimental studies have been conducted in the Indian subcontinent (6, 7) and elsewhere highlighting the importance and management of this entity (8–10). Our hospital is located in the vicinity of a major fruit and vegetable market of Kashmir valley and gets a wide range of hand injuries including foreign body penetration, but no prior study has been conducted addressing the issue of missed foreign bodies. This prompted us to study the profile of patients who report with missed foreign bodies in the hand.
Materials and methods
A retrospective study was conducted of all the patients who were treated in the Department of Surgery, Sheri Kashmir Institute of Medical Sciences (medical college), Bemina, Srinagar, Kashmir, India, from June 2003 to May 2009 for missed foreign bodies in the hand. Data regarding all cases managed for missed foreign bodies in hands were retrieved from the databank and minor procedures registry of the hospital, and processed and analyzed with respect to patient demographics and management. For our study, we defined the missed foreign body as the one which had been overlooked at the time of injury, and all such cases which reported with various complications resulting from the foreign bodies were studied irrespective of the time-interval between injury and complication.
Results
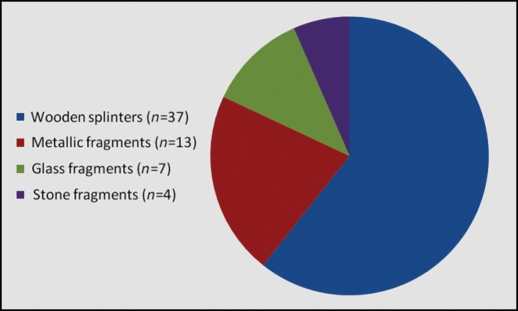
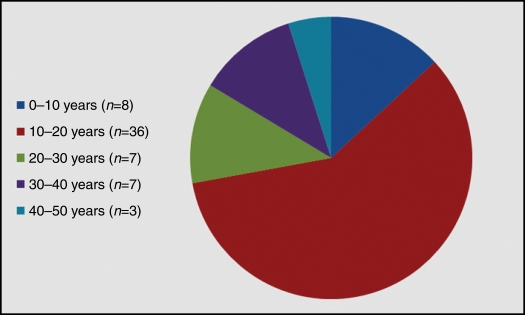
Over a period of six years from June 2003 to May 2009, 61 cases with missed foreign bodies in hands were managed (52 males and 9 females). Foreign bodies of different types were retrieved in patients of all age groups and belonging to all walks of life as shown in Figs. 1, 2 and Tables 1, 2. The clinical presentation and the time elapsed since possible penetration of foreign bodies is depicted in Table 3. As shown in Fig. 1, wooden splinters (n=37; 60.66%) were the most common foreign bodies retrieved followed by metallic fragments (n=13; 21.31%), glass fragments (n=7; 11.47%), and stone fragments (n=4; 6.56%). The metallic fragments included components of explosive devices like land mines and grenades (n=4), needles (n=3), iron/copper wire fragments (n=3), and aluminum wire fragment (n=1).
Fig. 1.
Nature of retained foreign bodies.
Fig. 2.
Age distribution (in years).
Table 1.
Occupational status of the patients
| Occupation of patients | Number (n) and percentage |
|---|---|
| Laborers | 36 (59.02%) |
| Students | 9 (14.75%) |
| Housewives | 5 (8.20%) |
| Office employees | 4 (6.56%) |
| Artisans/Sculptors | 7 (11.47%) |
Table 2.
Presenting features of missed foreign bodies
| Presenting feature of missed foreign bodies | Number (n) and percentage |
|---|---|
| Non-healing/Discharging wound | 33 (54.1%) |
| Chronic pain | 21 (34.4%) |
| Visible lump/Foreign body sensation | 5 (8.2%) |
| Spontaneous hematoma | 1 (1.6%) |
| Median nerve deficit (paresthesias) | 1 (1.6%) |
Table 3.
Time elapsed since possible penetration of foreign body
| Time since injury and possible penetration of foreign bodies | Number (n) and percentage |
|---|---|
| Up to two weeks | 6 (9.84%) |
| Two weeks to two months | 9 (14.75%) |
| Two to six months | 2 (3.28%) |
| Six months to two years | 6 (9.84%) |
| Above two years | 1 (1.64%) |
| Unknown | 37 (60.65%) |
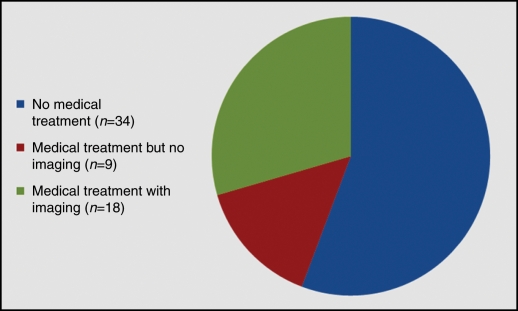
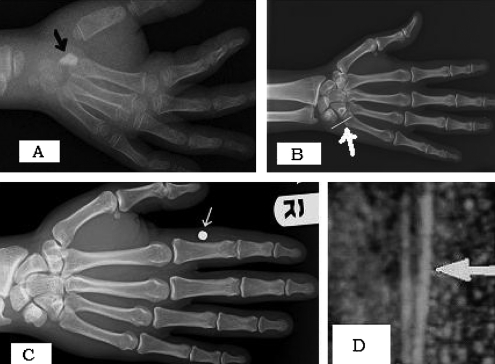
As is shown in Fig. 3, among the 61 cases treated by us, 34 (55.74%) patients had not taken any medical treatment before reporting to our department. In the rest of the 27 cases, basic wound care had been provided after imaging with plain radiograms in 18 (29.51%) cases and in 9 (17.75%) cases, only wound care had been provided without any imaging. Among these 18 cases that had been imaged with only radiograms, five cases had been missed in our facility and 13 patients had been managed in other health centers. Preoperative evaluation with ultrasonography and exploration led to recovery of wooden splinters in 17 cases and aluminum wire fragment in one case (see Fig. 4).
Fig. 3.
Management of injuries resulting in missed foreign bodies.
Fig. 4.
(A) Plain radiograph showing a retained glass piece (arrow). (B) Plain radiograph showing a retained sewing needle. (C) Plain radiograph showing a radio-opaque pellet along proximal phalanx of index finger (arrow). (D) Ultrasonogram revealing echogenic wooden splinters (arrow).
Besides clinical assessment, plain radiographs and ultrasound (high resolution and high frequency) were the tools utilized in the diagnosis and localization of the missed foreign bodies as shown in Table 4.
Table 4.
Diagnostic modalities used for localizing missed foreign bodies
| Nature of foreign bodies | Number (n) | Diagnosis by plain radiographs | Diagnosis by ultra sonograms |
|---|---|---|---|
| Wooden splinters | 37 | 2 (3.3%) | 35 (96.7%) |
| Glass pieces | 7 | 6 (85.7%) | 1 (14.3%) |
| Metallic fragments | 13 | 12 (92.30%) | 1 (7.70%) |
| Stone fragment | 4 | 4 (100%) | – |
Management of all the missed foreign bodies comprised of localization by imaging and removal. In 47 cases, removal of the foreign body was accomplished under local anesthesia on outpatient basis. In the rest of the 14 cases, exploration and removal of foreign bodies was undertaken under general/regional anesthesia. The indications for resorting to general anesthesia included young age (n=8), failed exploration or incomplete removal under local anesthesia (n=4). There were no postoperative complications in 27 patients who remained under follow-up up to three months. Eighteen patients were lost to follow-up after surgical intervention. Sixteen patients were discharged from services within a month as their wounds had healed normally and they had no symptoms/signs to warrant further follow-up.
Discussion
Penetrating injuries to hands are the most common cause of hospital emergency room visits (11) and an important health hazard associated with many occupations. The obvious foreign bodies might be removed by the patients themselves or the primary health providers. However, it is reported that 15–38% of the foreign bodies get overlooked at the time of initial examination (1, 2), and wound management depending upon the clinical acumen of the health care provider and the availability and use of imaging facilities. These overlooked foreign bodies form a major cause of medical litigations (3–5).
The missed foreign body may remain asymptomatic for prolonged periods or else lead to a wide range of complications including pain, abscess, chronic discharging wound, necrotizing fasciitis (12), bone and joint destructive lesions (13), granulomas (14) with impairment of tendon mobility or triggering of digits (15), migration (16), delayed tendon ruptures (16, 17), neurodeficits (15, 18), pyogenic granulomas (19), and vascular events (20, 21). In our series as is evident from Table 1, impairment of wound healing and chronic pain were the major presenting features. One of the cases reported with paresthesias in median nerve territory and had a small retained glass piece in the area of carpus impinging on the median nerve. The patient had a complete recovery after removal of glass piece. The vascular complications secondary to retained foreign bodies include major arterial erosion, spontaneous hematoma, thromboemboli, digital ischemia, and skin necrosis. One of the cases of retained shrapnel reported with spontaneous hematoma and on exploration, erosion in a small branch of superficial palmar arch was documented. We neither encountered any spontaneous ruptures of tendons nor did we retrieve any foreign body of plastic origin which is commonly reported in the literature.
Depending upon the occupational status, a wide range of retained foreign bodies has been reported in the literature. In our experience, wooden splinters formed the most common foreign bodies retained (n=37, 60.65%), followed by needles/metal pieces, glass pieces, stone fragments, and glass pieces. The increased incidence of wooden splinters can be explained by location of our hospital in the proximity of the biggest fruit market in Kashmir where wooden boxes are ferried. We also managed four cases of retained metallic fragments of explosives (pellets/shrapnel) in whom these foreign bodies had been ignored at the time of injury as they had reported to hospitals along with many other seriously injured victims of armed violence and had got less attention due to diversion of attention toward serious patients (scenario at the time of mass casualties like land mine blast).
Diagnosis of missed foreign bodies depends on imaging and clinical assessment. In penetrating injuries, the possibility of retained foreign bodies should always be entertained. It is the failure of the primary care physician to advise appropriate imaging due to lack of suspicion or the non-radio opaque nature of the foreign bodies, which lead to retention of foreign bodies and subsequent complications and litigations. We also managed 18 such cases in which non-radio opaque foreign bodies had got initially missed due to non-utilization of ultrasonography on part of physicians. Recently, various studies have been published which have strongly proven the sensitivity and cost effectiveness of ultrasonography in detection of foreign bodies in hands (6, 7, 11). It is against this background that many workers have suggested that ultrasound facilities and basic training be provided to emergency physicians so that foreign bodies can be ruled out in all cases of penetrating hand injuries (22). This suggestion is supported by the successful application of focused assessment with sonography for trauma (FAST) by emergency physicians (23).
In literature, depending upon the nature of foreign body and the available facilities, various modalities of imaging are recommended for diagnosis and localization, which include plain radiographs, ultrasonograms, CT scans, MRI, fistulograms, and xerographs (6, 7, 22, 24, 25). Radiopaque material is usually easy to detect but it is the radiolucent bodies like wooden splinters which are difficult to detect and are usually missed (4). High frequency–high resolution ultrasonography and MRI are useful in detection of these non-radio opaque foreign bodies (26–30). In our setting, free-of-cost MRI and CT-scan facilities are not available and all of the missed foreign bodies were detected by plain images or ultrasound as shown in Table 4. The only metallic body which was missed on plain image was picked up by ultrasound and on exploration turned out to be a piece of aluminum wire. CT and MRI if available can, however, provide additional information regarding the location and relationship of retained foreign body with adjacent tendons, neurovascular bundles, and muscle groups and thereby guide in selection of surgical approach and extent of exploration (29, 30).
The missed foreign bodies may produce immediate symptoms like wound infections or may remain dormant for even decades (2). In our series, 37 patients (61.6%) were not aware of the traumatic event leading to entry of the foreign bodies as they belonged to poor labor class who frequently get injured and hence tend to ignore the injuries to avoid disturbance in their routine life. One of our patients who belonged to non-labor class reported after two years of getting injured with retained glass piece.
Once diagnosed, proper surgical exploration and removal of the missed foreign body is the treatment. But the key to success is accurate localization of the foreign body (6, 10, 31, 32) using available imaging facilities. In most of the cases, the exploration can be done on outpatient basis under local anesthesia, but improper localization can end up in long and taxing explorations with no recovery of foreign bodies and extensive damage to soft tissues (25). In our experience, 47 cases (77%) were managed as outpatients and only 14 cases (23%) required exploration under general anesthesia. Among these 14 cases, four patients were such in whom exploration under local anesthesia had failed and intraoperative use of ultrasonogram was resorted to for successful recovery of foreign bodies. Intraoperative use of ultrasonography has in fact been recommended in literature also as an aid in real-time localization of foreign bodies (31). This accurate localization enables surgeons to make smaller and cosmetically appealing incisions and remove foreign bodies with a minimum amount of dissection and operation time (33).
Conclusion
A total of 61 cases of missed foreign bodies were managed over a period of six years in our hospital. Foreign bodies need to be suspected and ruled out in every case of penetrating injury to hands by use of appropriate imaging modality. In missed foreign bodies, management comprises of accurate localization by proper imaging, followed by surgical exploration and removal.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.Steele MT, Tran LV, Watson WA, Muelleman RL. Retained glass foreign bodies in wounds: predictive value of wound characteristics, patient perception, and wound exploration. Am J Emerg Med. 1998;16:627–30. doi: 10.1016/s0735-6757(98)90161-9. [DOI] [PubMed] [Google Scholar]
- 2.Anderson MA, Newmeyer WL, Kilgore ES., Jr Diagnosis and treatment of retained foreign bodies in the hand. Am J Surg. 1982;144:63–7. doi: 10.1016/0002-9610(82)90603-1. [DOI] [PubMed] [Google Scholar]
- 3.Dunn JD. Risk management in emergency medicine. Emerg Med Clin North America. 1987;5:51–69. [PubMed] [Google Scholar]
- 4.Vukmir RB. Medical malpractice: managing the risk. Med Law. 2004;23:495–513. [PubMed] [Google Scholar]
- 5.Vermeiren De A, Maeseneer M. Medico legal aspects of penetrating hand and foot trauma: ultrasound of soft tissue foreign bodies. JBR-BTR. 2004;87:205–6. [PubMed] [Google Scholar]
- 6.Shrestha D, Sharma UK, Mohammad R, Dhoju D. The role of ultrasonography in detection and localization of radiolucent foreign body in soft tissues of extremities. J Nepal Med Assoc. 2009;49:5–9. [PubMed] [Google Scholar]
- 7.Saboo SS, Saboo SH, Soni SS, Adhane V. High-resolution sonography is effective in detection of soft tissue foreign bodies: experience from a rural Indian center. J Ultrasound Med. 2009;28:1245–9. doi: 10.7863/jum.2009.28.9.1245. [DOI] [PubMed] [Google Scholar]
- 8.Ober CP, Jones JC, Larson MM, Lanz OI, Werre SR. Comparison of ultrasound, computed tomography, and magnetic resonance imaging in detection of acute wooden foreign bodies in the canine manus. Vet Radiol Ultrasound. 2008;49:411–8. doi: 10.1111/j.1740-8261.2008.00399.x. [DOI] [PubMed] [Google Scholar]
- 9.Peterson JJ, Bancroft LW, Kransdorf MJ. Wooden foreign bodies: imaging appearance. Am J Roentgenol. 2002;178:557–62. doi: 10.2214/ajr.178.3.1780557. [DOI] [PubMed] [Google Scholar]
- 10.Veselko M, Trobec R. Intraoperative localization of retained metallic fragments in missile wounds. J Trauma. 2000;49:1052–8. doi: 10.1097/00005373-200012000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Boyse TD, Fessell DP, Jacobson JA. US of soft-tissue foreign bodies and associated complications with surgical correlation. Radio Graph. 2001;21:1251–6. doi: 10.1148/radiographics.21.5.g01se271251. [DOI] [PubMed] [Google Scholar]
- 12.Yanay O, Vaughan DJ, Diab M, Brownstein D, Brogan TV. Retained wooden foreign body in a child's thigh complicated by severe necrotizing fasciitis: a case report and discussion of imaging modalities for early diagnosis. Pediatr Emerg Care. 2001;17:354–5. doi: 10.1097/00006565-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Fakoor M. Prolonged retention of an intra medullary wooden foreign body. Pak J Med Sci. 2006;22:78–9. [Google Scholar]
- 14.Freund EI, Weigl K. Foreign body granuloma. A cause of trigger thumb. J Hand Surg [Br] 1984;9:210. [PubMed] [Google Scholar]
- 15.Choudhari KA, Muthu T, Tan MH. Progressive ulnar neuropathy caused by delayed migration of a foreign body. Br J Neurosurg. 2001;15:263–5. doi: 10.1080/026886901750353728. [DOI] [PubMed] [Google Scholar]
- 16.Yang SS, Bear BJ, Wieland AJ. Rupture of the flexor pollicis longus tendon after 30 years due to migration of a retained foreign body. J Hand Surg [Br] 1995;20:803–5. doi: 10.1016/s0266-7681(95)80052-2. [DOI] [PubMed] [Google Scholar]
- 17.Jablon M, Rabin SI. Late flexor pollicis longus tendon rupture due to retained glass fragments. J Hand Surg Am. 1988;13:713–6. doi: 10.1016/s0363-5023(88)80131-x. [DOI] [PubMed] [Google Scholar]
- 18.Rainer C, Schoeller T, Wechselberger G, Bauer T, Heribert H. Median nerve injury caused by missed foreign body. Scand J Plast Reconstr Surg. 2000;34:401–3. doi: 10.1080/028443100750059228. [DOI] [PubMed] [Google Scholar]
- 19.Azzopardi EA, Xuereb CB, Iyer S. Pyogenic granuloma as a surrogate indicator of deep seated foreign bodies: a case report. Cases J. 2009;2:7354. doi: 10.4076/1757-1626-2-7354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James W, Robert A, Suzanne M. Vascular complications of a foreign body in the hand of an asymptomatic patient. Ann Plast Surg. 1995;34:92–4. doi: 10.1097/00000637-199501000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Meurer WJ. Radial artery pseudo aneurysm caused by occult retained glass from a hand laceration. Pediatr Emerg Care. 2009;25:255–7. doi: 10.1097/PEC.0b013e31819e3744. [DOI] [PubMed] [Google Scholar]
- 22.Blankstein A, Cohen I, Heiman Z, Salai M, Michael Heim M, Chechick A. Localization, detection and guided removal of soft tissue foreign body in the hands using sonography. Arch Orthop Trauma Surg. 2000;120:514–7. doi: 10.1007/s004020000173. [DOI] [PubMed] [Google Scholar]
- 23.Scalea TM, Rodriguez A, Chiu WC, Brenneman FD, Fallon WF, Kato K, et al. Focused assessment with sonography for trauma (FAST): results from an international consensus conference. J Trauma. 1999;46:466–72. doi: 10.1097/00005373-199903000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Ginsburg MJ, Ellis GL, Flom LL. Detection of soft-tissue foreign bodies by plain radiography, xerography, computed tomography and ultrasonography. Ann Emerg Med. 1990;19:701–3. doi: 10.1016/s0196-0644(05)82483-7. [DOI] [PubMed] [Google Scholar]
- 25.Courter BJ. Radiographic screening for glass foreign bodies – what does a “negative” foreign body series really mean? Ann Emerg Med. 1990;19:997–1000. doi: 10.1016/s0196-0644(05)82562-4. [DOI] [PubMed] [Google Scholar]
- 26.Schlager D, Saunders AB, Wiggins D, Boren W. Ultrasound for detection of foreign bodies. Ann Emerg Med. 1991;20:189–91. doi: 10.1016/s0196-0644(05)81220-x. [DOI] [PubMed] [Google Scholar]
- 27.McGeorge DD, McGeorge S. Diagnostic medical ultrasound in the management of hand injuries. J Hand Surg. 1990;2:256–61. doi: 10.1016/0266-7681_90_90133-o. [DOI] [PubMed] [Google Scholar]
- 28.Gilbert FJ, Campbell RS, Bayliss AP. The role of ultrasound in the detection of non-radiopaque foreign bodies. Clin Radiol. 1990;41:109–12. doi: 10.1016/s0009-9260(05)80140-0. [DOI] [PubMed] [Google Scholar]
- 29.Mizel MS, Steinmetz ND, Trepman E. Detection of wooden foreign bodies in muscle tissue: experimental comparison of computed tomography, magnetic resonance imaging, and ultrasonography. Foot Ankle Int. 1994;15:437–43. doi: 10.1177/107110079401500807. [DOI] [PubMed] [Google Scholar]
- 30.Bodne D, Quinn S, Cochran SF. Imaging foreign glass and wooden bodies of the extremities with CT and MR. J Comput Assist Tomogr. 1988;12:608–11. doi: 10.1097/00004728-198807000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Shiels WE, Babcock DS, Wilson JL, Burch RA. Localization and guided removal of soft-tissue foreign bodies with sonography. Am J Roentgenol. 1990;155:1277–81. doi: 10.2214/ajr.155.6.2122680. [DOI] [PubMed] [Google Scholar]
- 32.Coombs CJ, Mutimer KL, Slattery PG, Wise AG. Hide and seek: preoperative ultrasonic localization of non radio-opaque foreign bodies. ANZ J Surg. 1990;60:989–91. doi: 10.1111/j.1445-2197.1990.tb07519.x. [DOI] [PubMed] [Google Scholar]
- 33.Gooding GAW, Hardiman T, Sumers M, Stess R, Graf P, Grunfeld C. Sonography of the hand and foot in foreign body detection. J Ultrasound Med. 1987;6:441–7. doi: 10.7863/jum.1987.6.8.441. [DOI] [PubMed] [Google Scholar]