Abstract
Over the past decade Point-of-Care Ultrasound (POC US) is increasingly performed in adult emergency medicine for a variety of indications. Pediatric emergency medicine has been much slower to embrace POC US. The authors report a case of a 15-year-old boy that presented to the pediatric emergency department with abdominal pain. A diagnosis of appendicitis was made using real-time POC US by a pediatric emergency medicine attending. Knowledge of the sonographic characteristics of appendicitis can help the physician in the prompt diagnosis of this condition, thereby reducing morbidity and mortality that may result from a delay in diagnosis.
Over the past decades ultrasound (US) has been utilized by many different medical specialties and is no longer limited to radiology. In 1999, the American Academy of Emergency Medicine published its position statement defining POC US as a sonographic imaging procedure by an emergency physician on a patient in the emergency department in an effort to detect acute medical problems.1 POC US has grown dramatically over the last years in adult emergency departments and increasingly emergency physicians have dedicated ultrasound machines available for POC evaluation. In 2001, the American College of Emergency Physicians (ACEP) issued a policy statement on the use of emergency ultrasound, endorsing its use in emergency departments nationwide.2 Emergency medicine physicians have been on the forefront of clinical use and research of new ultrasound techniques, particularly in adult patients. A POC US is not a complete US but a focused, limited, goal directed exam with the purpose of answering a specific clinical question. The attraction of immediate POC US in the evaluation of specific emergent complaints makes it an ideal tool in the emergency department. The ability to perform these focused studies may allow for faster and safer management of patients.
Most emergency medicine residencies in the United States currently train their residents in POC US as part of the curriculum and it is an accepted tool for the rapid assessment of the emergency patient.3 Both the American College of Emergency Physicians and the Society for Academic Emergency Medicine continue to support these advancements. In a revised statement from October 2008 the ACEP suggested guidelines for specific training pathways, quality improvement, documentation and credentialing guidelines, but at this time there is no set national standard for training and competency assessment is left to the individual program directors.4 Pediatric emergency medicine physicians have been much slower to embrace POC US ultrasound, but they have the luxury of adapting some of the proven uses to the pediatric population, for example the FAST exam (Focused Assessment with Sonography in Trauma).5 Although only a few pediatric emergency medicine fellowships have integrated POC US training into their curriculum and offer a 2- to 4-week ultrasound rotation during the fellowship,6 94% of pediatric emergency medicine fellowship directors expressed a desire for pediatric-specific POC US training.7 Currently, numerous courses and “mini-fellowships” exist and are generally designed for emergency physicians who graduated without ultrasound training. However, none of these are pediatric specific.
To the authors' knowledge, there are no previous reported cases of acute appendicitis diagnosed by a pediatric emergency medicine attending using POC US. One of the authors (BMH), who obtained experience in pediatric US through a foreign pediatric residency program that incorporates ultrasound into their curriculum, reports her case here.
Case Report
A 15-year-old boy was brought to the pediatric emergency department by his father with the chief complaint of abdominal pain for one day. The patient described the pain as intermittent and located initially in the periumbilical area, but stated the pain had become constant and more severe in the right lower abdomen over the last several hours. He reported several non-bilious and non-bloody emeses. He denied any fever, chills, dysuria, cough, or runny nose. His fluid intake and urine output were decreased. Past medical history revealed no hospitalizations or surgery. His immunizations were up to date and he had no known drug allergies. Vital signs on initial examination included a blood pressure of 128/69 mmHg, heart rate of 76 beats/min, respiratory rate of 24/min, temperature of 101° F and an oxygen saturation of 100% in room air. His weight was 48 kg.
He was alert but in obvious pain. His heart and lung exam was normal. He had strong peripheral pulses and good perfusion. The abdomen was non-distended with decreased bowel sounds in all quadrants. He had significant right lower quadrant abdominal tenderness with guarding and rebound. The remainder of the physical examination was unremarkable.
ER Course
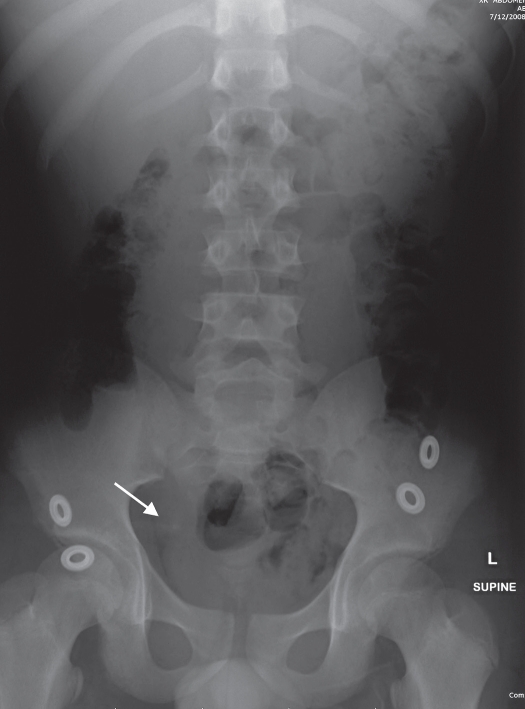
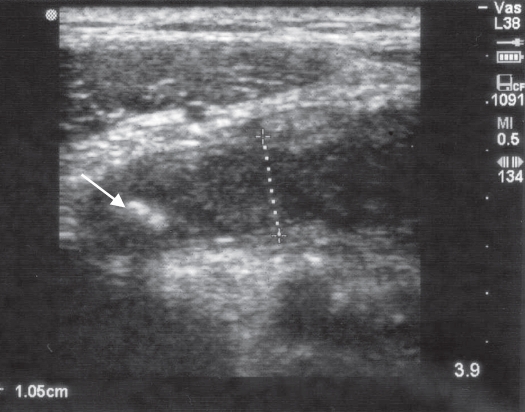
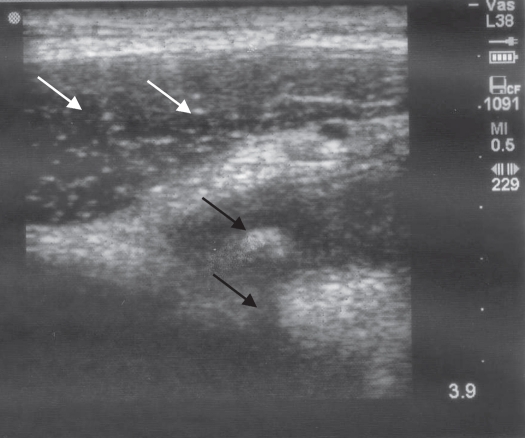
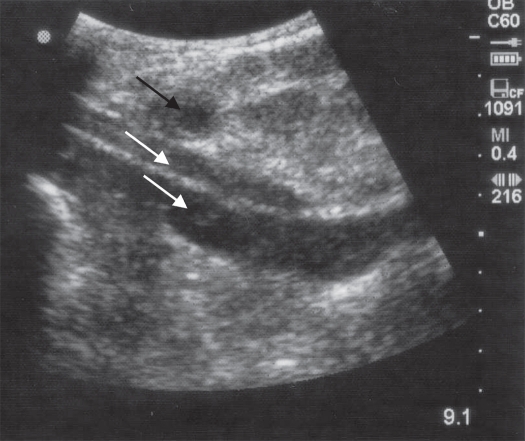
Intravenous fluids with normal saline were started and the patient was given 4 mg of morphine IV for pain control. Laboratory results revealed a white blood cell count of 13,800 per microliter with 71% neutrophils, 13% bands and 16% lymphocytes. CRP was 2.2mg/dl. His electrolytes and renal function were within normal limits. Urinalysis was normal. An abdominal x-ray (Figure 1) revealed a normal intestinal gas pattern and a 2mm calcification in the right side of the pelvis. A radiology US was ordered because of suspicion for appendicitis. However, the US technician was not in-house and needed to be called in. In the meantime, the pediatric emergency medicine attending performed a POC US. A TITAN Handcarried Ultrasound (SonoSite, Inc. Bothell, WA) with a 10-5 MHz 38-mm broadband linear array transducer was utilized. POC US with graded compression technique was performed in the region of maximal pain while the patient was in the supine position. The study revealed a swollen, noncompressible, blind ending tubular structure measuring 1.05 cm in diameter with no peristaltic activity inside the lumen (Figure 2). It also showed an appendicolith with acoustic shadowing. Anterior to the appendix the rectus abdominis muscle could be visualized on transverse view with its speckled appearance (Figure 3). A picture taken with a 3.5MZ curved array probe showed the proximity to the iliac artery and vein (Figure 4). A surgical consultation was obtained and the patient was seen and evaluated by a pediatric surgeon. The POC US pictures were reviewed and assured the surgeon of the diagnosis. The patient was taken to the operating room just before the US technician arrived. A laparoscopic appendectomy was performed and the diagnosis of acute, suppurative, non-perforated appendicitis was confirmed by visual inspection and pathologic analysis. The patient had an uneventful postoperative course and was discharged home the next day.
Figure 1.
Calcification in the Right Lower Quadrant (white arrow)
Figure 2.
A noncompressible tubular structure measuring 1.05cm in diameter with an appendicolith in the lumen (white arrow)
Figure 3.
Appendicolith with acoustic shadowing (black arrows). Rectus abdominis muscle (white arrows) anterior to the appendix
Figure 4.
Appendix in cross-sectional view (black arrow) anterior to the iliac vessels (white arrows)
Discussion
Appendicitis is a common, yet serious, cause of acute abdominal pain in adolescents and young adults often presenting to an emergency department. In most cases acute appendicitis is caused by a luminal obstruction, which leads to distension, increased intraluminal pressure, and mucosal compromise with subsequent mural invasion by intraluminal bacteria.8
With increasing pressure and venous obstruction, gangrene and perforation can result which may lead to peritonitis and death. Early surgical intervention in patients with acute appendicitis is imperative to avoid appendiceal perforation, which is associated with increased morbidity and mortality. Duration of symptoms is the factor most closely associated with advanced disease.9
With the invention of helical computed tomography (CT) in the mid 90's, CT has emerged as the leading imaging modality for adult patients with suspected appendicitis in the United States. There is a growing body of literature that shows this imaging modality to be the most accurate way to diagnose or exclude appendicitis. Kim et al reported that helical CT's in patients with a high degree of clinical suspicion for acute appendicitis reduces the number of false positives and has the potential to reduce negative appendectomies.10 However, Brenner and Hall remind of the significant cancer risk from CT examinations due to exposure to ionizing radiation, especially for children.11
Ultrasound has been used for the diagnosis of acute appendicitis as early as 1981.12 Technologic improvements in ultrasound equipment have made systems more portable, easier to use at the bedside and of higher image quality, enhancing the accuracy of diagnosis. It is a risk free, low-cost, noninvasive, fast and painless procedure that does not use ionizing radiation and can be done at the bedside.
The diagnosis of appendicitis is made by graded compression technique that was first described by Puylaert in 1986. A linear high-frequency transducer is placed on the right lower quadrant and pressure is applied gradually while imaging, displacing the overlying gas-filled loops of bowel.13
POC US in the diagnosis of appendicitis is increasingly used in other specialties including gynecology and surgery.14–16
Sonographic findings consistent with acute appendicitis include visualization of a blind-ending, non-compressible, tubular structure, 6 mm or greater in diameter, that lacks peristalsis. Secondary signs include hyperemia with color-flow Doppler, periappendiceal fluid, and visualization of a shadowing appendicolith.17,18
The success of ultrasound depends largely on the skill and experience of the sonographer. In the hands of emergency physicians, sensitivity ranges between 39% to 96%, whereas the radiology literature reports sensitivities of 75% to 90%.19–23 A meta-analysis of 9,356 children and 4,341 adults demonstrated sensitivities of 88% and 83% and specificities of 94% and 93%, respectively in diagnosing appendicitis by radiology department ultrasound.24 Many studies have demonstrated that emergency medicine physicians can be trained in POC US to answer a specific question.25–30
In a prospective study, 40 consecutive patients with equivocal physical findings of acute appendicitis were examined with graded compression sonography by emergency medicine residents after a 1-hour lecture and 20 observations. The primary sonographic criterion for diagnosing acute appendicitis was an incompressible appendix with an outer diameter of 6 mm or larger with periappendicular inflamed fat with or without an appendicolith. The sonographic findings were correlated with surgical and pathologic findings. The sensitivity of emergency medicine residents diagnosing acute appendicitis by POC US was 83%, and specificity was 100%. The positive predictive value was 100% and negative predictive value was 69%.31
An important limitation of US is that the sensitivity and specificity for perforated appendicitis are lower than those seen for non-perforated appendicitis.32–34
The presence of an appendicolith on US in a patient with acute right lower quadrant abdominal pain is indicative of appendicitis. A retrospective study in 388 patients younger than 18 years found that the presence of an appendicolith was associated with earlier and higher rates of appendiceal perforation in pediatric patients with acute appendicitis.35
Management of children with clinically suspected appendicitis involves a risk management decision whether to operate or not. Therefore any examination that improves diagnostic accuracy is helpful.
CT scan and US have assumed critical roles in the diagnosis of patients suspected to have appendicitis.
In the clinical setting the choice between US and CT largely depends on institutional preference and on available expertise. US does not involve ionizing radiation, in contrast to CT, and should therefore be the initial imaging study in children if available. If US is positive, an appendectomy should be performed and if it is equivocal, normal, or doubt remains, the child should undergo CT scanning.36–39
Traditionally the radiology department makes the diagnosis of appendicitis with ultrasound. In some pediatric hospitals, radiology department US may not be available.40 The goal is to diagnose and treat appendicitis as early as possible, since a delay in diagnosis may result in perforation with increased morbidity and mortality. POC US may be valuable if access to radiological facilities is delayed and the pediatric emergency physician has had adequate training in POC US. Surgeons have good understanding of clinical ultrasound and can incorporate the POC US images in the final decision-making.
Conclusion
For pediatric emergency medicine physicians rapid diagnosis and treatment of life-threatening conditions is of utmost importance. Appendicitis is in the differential diagnosis of children presenting with right lower abdominal pain. The initial imaging modality in children should be graded compression exam by US done by the most experienced sonographer, usually the radiologist. However, if a delay for this study is anticipated, POC US by a physician trained in POC US can be crucial in reducing time to diagnosis and definitive treatment and therefore reducing morbidity and prolonged hospital stay.
References
- 1.American Academy of Emergency Medicine, author. Position statement on performance of emergency screening ultrasound examinations. [10/5/2009]. Available at: http://www.aaem.org/positionstatements/ultra.php.
- 2.American College of Emergency Physicians, author. Use of ultrasound imaging by emergency physicians. Ann Emerg Med. 2001;38:469–470. doi: 10.1067/mem.2001.118487. [DOI] [PubMed] [Google Scholar]
- 3.Counselman FL, Sanders A, Slovis CM, et al. The status of bedside ultrasonography training in emergency medicine residency programs. Acad Emerg Med. 2003;10:37–42. doi: 10.1111/j.1553-2712.2003.tb01974.x. [DOI] [PubMed] [Google Scholar]
- 4.Emergency ultrasound guidelines. Ann Emerg Med. 2009;53:550–570. doi: 10.1016/j.annemergmed.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 5.Levy JA, Noble VE. Bedside ultrasound in pediatric emergency medicine. Pediatrics. 2008;121:e1404–e1412. doi: 10.1542/peds.2007-1816. [DOI] [PubMed] [Google Scholar]
- 6.Ramirez-Schrempp D, Dorfman DH, Tien I, et al. Bedside ultrasound in pediatric emergency medicine fellowship programs in the United States: little formal training. Pediatr Emerg Care. 2008;24:664–667. doi: 10.1097/PEC.0b013e3181884955. [DOI] [PubMed] [Google Scholar]
- 7.Chen L, Santucci KA. Probing the availability of emergency ultrasound in pediatrics. Pediatr Emerg Care. 2006;22:688. [Google Scholar]
- 8.Crawford JM. The Gastrointestinal Tract. In: Contran R, Kumar V, Collins T, editors. Robbins pathologic basis of disease. 6th edition. Philadelphia: Saunders; 1999. pp. 775–843. [Google Scholar]
- 9.Velanovich V, Satava R. Balancing the normal appendectomy rate with the perforated appendicitis rate: implications for quality assurance. Am Surg. 1992;58:264–269. [PubMed] [Google Scholar]
- 10.Kim K, Rhee JE, Lee CC, et al. Impact of helical computed tomography in clinically evident appendicitis. Emerg Med J. 2008;25:477–481. doi: 10.1136/emj.2006.044552. [DOI] [PubMed] [Google Scholar]
- 11.Brenner DJ, Hall EJ. Computed tomography - an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 12.Deutsch A, Leopold GR. Ultrasonic demonstration of the inflamed appendix: case report. Radiology. 1981;140:163–164. doi: 10.1148/radiology.140.1.6941334. [DOI] [PubMed] [Google Scholar]
- 13.Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology. 1986;158:355–360. doi: 10.1148/radiology.158.2.2934762. [DOI] [PubMed] [Google Scholar]
- 14.Benson CB, Bluth EI. Ultrasound in Obstetrics and Gynecology, a Practical Approach to Clinical Problems. 2nd Edition. Thieme publishing group; 2008. Acute pelvic pain; pp. 11–21. [Google Scholar]
- 15.Deziel DJ. Ultrasonography and the surgeon. Surg Endosc. 1996;10:615–616. doi: 10.1007/BF00188511. [DOI] [PubMed] [Google Scholar]
- 16.Lindelius A, Torngren S, Pettersson H, et al. Role of surgeon-performed ultrasound on further management of patients with acute abdominal pain: a randomised controlled clinical trial. Emerg Med J. 2009;26:561–566. doi: 10.1136/emj.2008.062067. [DOI] [PubMed] [Google Scholar]
- 17.Rettenbacher T, Hollerweger A, Macheiner P, et al. Outer diameter of the vermiform appendix as a sign of acute appendicitis: evaluation at US. Radiology. 2001;218:757–762. doi: 10.1148/radiology.218.3.r01fe20757. [DOI] [PubMed] [Google Scholar]
- 18.Brown MA. Imaging acute appendicitis. Semin Ultrasound CT MR. 2008;29:293–307. doi: 10.1053/j.sult.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 19.Chen SC, Wang HP, Hsu HY, et al. Accuracy of ED sonography in the diagnosis of acute appendicitis. Am J Emerg Med. 2000;18:449–452. doi: 10.1053/ajem.2000.7343. [DOI] [PubMed] [Google Scholar]
- 20.Sivit CJ, Applegate KE, Stallion A, et al. Imaging evaluation of suspected appendicitis in a pediatric population: effectiveness of sonography versus CT. AJR Am J Roentgenol. 2000;175:977–980. doi: 10.2214/ajr.175.4.1750977. [DOI] [PubMed] [Google Scholar]
- 21.Poortman P, Lohle PNM, Schoemaker C, et al. Comparison of CT and sonography in the diagnosis of acute appendicitis: a blinded prospective study. AJR Am J Roentgenol. 2003;181:1355–1359. doi: 10.2214/ajr.181.5.1811355. [DOI] [PubMed] [Google Scholar]
- 22.Dilley A, Wesson D, Munden M, et al. The impact of ultrasound examinations on the management of children with suspected appendicitis: a 3-year analysis. J Pediatr Surg. 2001;36:303–308. doi: 10.1053/jpsu.2001.20702. [DOI] [PubMed] [Google Scholar]
- 23.Fox JC, Hunt MJ, Zlidenny AM, et al. A Retrospective Analysis of Emergency Department Ultrasound for Acute Appendicitis. West J Emerg Med. 2007;8:41–45. [PMC free article] [PubMed] [Google Scholar]
- 24.Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis. Radiology. 2006;241:83–94. doi: 10.1148/radiol.2411050913. [DOI] [PubMed] [Google Scholar]
- 25.Bowra J, McLaughlin R. Emergency Ultrasound Made Easy. London, UK: Churchill Livingstone; 2006. [Google Scholar]
- 26.Pershad J, Myers S, Plouman C, et al. Bedside limited echocardiography by the emergency physician is accurate during evaluation of the critically ill patient. Pediatrics. 2004;114:e667–e671. doi: 10.1542/peds.2004-0881. [DOI] [PubMed] [Google Scholar]
- 27.Jang TB, Aubin C, Sineff S, et al. The learning curve for EP-performed focused abdominal sonography for trauma (FAST) exams in the detection of intraperitoneal free fluid. Acad Emerg Med. 2003;10:428. [Google Scholar]
- 28.Kuhn M, Bonnin RL, Davey MJ, et al. Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate, and advantageous. Ann Emerg Med. 2000;36:219–223. doi: 10.1067/mem.2000.108616. [DOI] [PubMed] [Google Scholar]
- 29.Durston W, Carl ML, Guerra W. Patient satisfaction and diagnostic accuracy with ultrasound by emergency physicians. Am J Emerg Med. 1999;17:642–646. doi: 10.1016/s0735-6757(99)90150-x. [DOI] [PubMed] [Google Scholar]
- 30.Squire BT, Fox JC, Anderson C. ABSCESS: applied bedside sonography for convenient evaluation of superficial soft tissue infections. Acad Emerg Med. 2005;12:601–606. doi: 10.1197/j.aem.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 31.Min YG, Lee CC, Bae YS, et al. Accuracy of sonography performed by emergency medicine residents for the diagnosis of acute appendicitis. Ann Emerg Med. 2004;44:S60. [Google Scholar]
- 32.Borushok KF, Jeffrey RB, Jr, Laing FC, et al. Sonographic diagnosis of perforation in patients with acute appendicitis. AJR Am J Roentgenol. 1990;154:275–278. doi: 10.2214/ajr.154.2.2105013. [DOI] [PubMed] [Google Scholar]
- 33.Puylaert JB, Rutgers PH, Lalisang RI, et al. A prospective study of ultrasonography in the diagnosis of appendicitis. N Engl J Med. 1987;317:666–669. doi: 10.1056/NEJM198709103171103. [DOI] [PubMed] [Google Scholar]
- 34.Quillin SP, Siegel MJ, Coffin CM, et al. Acute appendicitis in children: value of sonography in detecting perforation. AJR Am J Roentgenol. 1992;159:1265–1268. doi: 10.2214/ajr.159.6.1442398. [DOI] [PubMed] [Google Scholar]
- 35.Alaedeen DI, Cook M, Chwals WJ. Appendiceal fecalith is associated with early perforation in pediatric patients. J Pediatr Surg. 2008;43:889–892. doi: 10.1016/j.jpedsurg.2007.12.034. [DOI] [PubMed] [Google Scholar]
- 36.Jeffrey RB, Jr, Laing FC, Townsend RR. Acute appendicitis: sonographic criteria based on 250 cases. Radiology. 1988;167:327–329. doi: 10.1148/radiology.167.2.3282253. [DOI] [PubMed] [Google Scholar]
- 37.Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000;215:337–348. doi: 10.1148/radiology.215.2.r00ma24337. [DOI] [PubMed] [Google Scholar]
- 38.Garcia Pena BM, Mandl KD, Kraus SJ, et al. Ultrasonography and limited computed tomography in the diagnosis and management of appendicitis in children. JAMA. 1999;282:1041–1046. doi: 10.1001/jama.282.11.1041. [DOI] [PubMed] [Google Scholar]
- 39.Baldisserotto M, Marchiori E. Accuracy of noncompressive sonography of children with appendicitis according to the potential positions of the appendix. AJR Am J Roentgenol. 2000;175:1387–1392. doi: 10.2214/ajr.175.5.1751387. [DOI] [PubMed] [Google Scholar]
- 40.Moore CL, Molina AA, Lin H. Ultrasonography in community emergency departments in the United States: access to ultrasonography performed by consultants and status of emergency physician-performed ultrasonography. Ann Emerg Med. 2006;47:147–153. doi: 10.1016/j.annemergmed.2005.08.023. [DOI] [PubMed] [Google Scholar]