Abstract
Recently, the World Health Organization emphasized the potential benefit of intermittent preventive treatment in infants (IPTi) to control malaria and officially recommended implementation of IPTi with sulfadoxine-pyrimethamine (SP) in areas with moderate and high transmission, where SP resistance is not high. As reported rebound effects make further observation mandatory, we performed a survey of participants of a former IPTi trial. Malariometric parameters were similar in the SP and the placebo group. In contrast, anti–Plasmodium falciparum lysate immunoglobulin G antibody levels, a proxy measure for preceding malaria episodes, remained lower in the SP arm. The most likely explanation is a lower overall exposure to parasitic antigens after IPTi.
Intermittent preventive treatment in infants (IPTi) is regarded as a promising malaria control tool, and the World Health Organization (WHO) has recommended implementation of IPTi with sulfadoxine-pyrimethamine (SP) in areas with moderate to high malaria transmission, where parasitic resistance to SP is not high [1]. The strategy behind IPTi is to administer full courses of antimalarials alongside routine vaccinations of the Expanded Program on Immunization of the WHO, regardless of whether an infant is parasitemic [2]. A pooled analysis of 6 trials using SP for IPTi in 4 African countries demonstrated a protective efficacy of 30.3% against uncomplicated malaria, 21.3% against anemia, and 22.9% against all-cause hospital admission during the first year of life [3]. In another trial from northern Tanzania comparing various drugs for IPTi, SP failed to provide protective efficacy due to preexisting drug resistance [4].
So far, however, long-term effects of IPTi such as possible extended efficacy or rebound phenomena are largely unknown. During the first SP-IPTi trial in Tanzania, an extended protective antimalarial effect beyond the duration of the pharmacological effects was described [5]. A detailed analysis of data from 2 studies from Ghana and Gabon suggested that SP-IPTi works mainly through a therapeutic and prophylactic effect over 30–60 d after drug application and that sustained effects beyond posttreatment prophylaxis might be very low [6]. In at least 3 of the SP-IPTi trials, distinct rebound effects of anemia, high-density parasitemia, or hospital admissions were reported [7–9]. Nevertheless, results from an extended follow-up study in Gabon do not appear to support the concept of rebound effects after SP-IPTi [10].
To assess the long-term effects of SP-IPTi, a cross-sectional follow-up survey of former study participants was performed 4 years after initial recruitment [7]. Anti–Plasmodium falciparum lysate immunoglobulin G antibody (PfLIgG) levels were used as a proxy measure for the frequency of preceding malaria episodes, as has been shown to be expedient in this setting [11].
METHODS
The follow-up survey took place in the same 9 villages (Afigya Sekyere district, Ashanti region, Ghana) where the placebo-controlled, double-blind, randomized SP-IPTi trial was performed (registered at www.ClinicalTrials.gov; NCT00206739). Recruitment in the present study was between September and November 2007, which was 3 years after the unblinding in the IPTi trial. In the study area, there is intense perennial malaria transmission. Documentation of medical histories, physical examinations, blood sampling, and laboratory testing were performed following the same standard operating procedures as described previously [7, 11]. Axillary temperature of ≥38.0°C or fever during the preceding 48 h reported by caretakers without being asked, accompanied by asexual P. falciparum parasitemia of >500 parasites/μL, was defined as malaria. Both attendance at outpatient clinics and admission to hospital in the time between the original trial and the current survey were assessed by interviewing caretakers and checking medical records.
Children with uncomplicated malaria were treated with artesunate (4 mg/kg/d) plus amodiaquine (10 mg/kg/d) for 3 d according to national guidelines. PfLIgG levels were measured by enzyme-linked immunosorbent assay and expressed in relative units (RUs) as described previously [11]. Methods of PfLIgG assessment were identical in the IPTi trial and in the present study but were performed independently at different time points.
Analyses were performed using Stata/IC software (version 10.0; StataCorp). Variables were compared between study arms by a contingency test (χ2) for proportions and a nonparametric test (Wilcoxon rank-sum) for continuous variables. The Spearman rank correlation test was used to correlate PfLIgG levels at age 24 months with malaria incidence rates during the first 2 years of life (original trial) and with PfLIgG levels measured at the time of the current survey. The risk of being parasite positive at the time of the survey in dependence on rates of parasitemia during the original trial was calculated using a bivariate logistic regression model, testing SP treatment as a possible confounding covariate. P values <.05 were considered significant.
The aim and principles of the study were explained to the caretakers of participants, and informed consent was signed or thumbprinted by participants’ caregivers in accordance with the Declaration of Helsinki. The study was approved by the Committee on Human Research Publication and Ethics of the School of Medical Science of the Kwame Nkrumah University of Science and Technology, Kumasi, Ghana.
RESULTS
More than 4 years after initial recruitment, 730 (82.3%) of the 887 children who had completed the original IPTi trial could be included. Baseline characteristics were similar in both study arms (Table 1). In total, 45 (6.2%) children had uncomplicated malaria and 246 (33.7%) had P. falciparum parasitemia, without significant differences between the treatment arms.
Table 1.
Characteristics and Outcomes of Study Participants at Follow-up
| Placebo (n = 350) | SP (n = 380) | Pa | |
| Characteristics | |||
| Sex Male Female |
183 (52.3) 167 (47.7) |
192 (50.5) 188 (49.5) |
.64 |
| Age, months, mean ± SD | 53.1 ± 3.7 | 52.8 ± 3.8 | .37 |
| β-Globin genotypeb HbAA HbAS HbSS HbAC HbCC HbSC Missing data |
258 (73.7) 39 (11.1) 1 (.3) 34 (9.7) 1 (.3) 4 (1.1) 13 (3.7) |
275 (72.4) 44 (11.6) 1 (.3) 45 (11.8) 1 (.3) 4 (1.1) 10 (2.6) |
.96 |
| Absent at follow up Moved Withdrawn Lost to follow-up Died |
51 (57.3) 16 (18.0) 20 (22.5) 2 (2.3) |
38 (55.9) 14 (20.6) 13 (19.0) 3 (4.3) |
.82 |
| Outcomes | |||
| Uncomplicated malariac Yes No Missing data |
18 (5.1) 319 (91.1) 13 (3.7) |
27 (7.1) 337 (88.7) 16 (4.2) |
.50 |
| Parasitemia Positive Negative Missing data |
120 (34.3) 217 (62.0) 13 (3.7) |
126 (33.2) 238 (62.6) 16 (4.2) |
.91 |
| Total PfLIgG level, RUs, median (IQR) Missing data |
22.2 (9.3-38.5) 12 (3.4) |
19.1 (6.8-34.5) 9 (2.4) |
<.05 |
| Hb level, g/dL, mean ± SD | 10.3 ± 1.6 | 10.3 ± 1.5 | .77 |
| Anemia Moderate anemia (<7.5 g/dL) Severe anemia (<5.0 g/dL) |
10 (2.9) 0 |
11 (2.9) 2 (.5) |
.98 .39 |
| Outpatient visitsd Yes, many times Yes, sometimes Yes, once in a while No Missing data |
119 (34.0) 141 (40.3) 71 (20.3) 18 (5.1) 1 (.3) |
120 (31.6) 159 (41.8) 83 (21.8) 18 (4.7) 0 |
.77 |
| Hospital admissionsd No Yes, once Yes, more than once Yes, frequency unknown |
277 (79.1) 47 (13.4) 23 (6.6) 3 (.9) |
305 (80.3) 38 (10.0) 34 (9.0) 3 (.8) |
.36 |
NOTE. Data are no. (%) of participants, unless otherwise indicated. Hb, hemoglobin; IQR, interquartile range; PfLIgG, anti-Plasmodium falciparum lysate IgG antibody; RUs, relative units; SD, standard deviation; SP, sulfadoxine-pyrimethamine.
Determined using Wilcoxon rank-sum test or χ2 test. P values <.05 were considered significant.
β-Globin genotype was determined by polymerase chain reaction.
An episode of malaria was defined as fever (axillary temperature of ≥38.0°C or fever during the preceding 48 h reported by caretakers without being asked accompanied by asexual P. falciparum parasite load of >500/μL.
Frequencies since last follow-up of core study. Information obtained by interviewing participants’ mothers and caretakers and reviewing medical records.
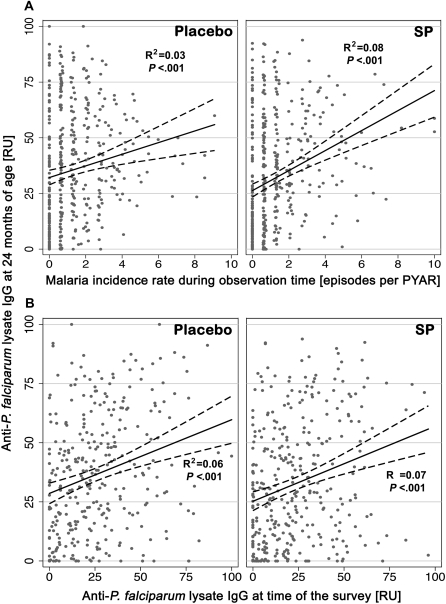
At the age of 2 years, PfLIgG levels were significantly higher in children of the placebo group than in those of the SP group (median, 32.3 RUs [interquartile range, 13.7–55.8] vs 28.4 RUs [8.9–51.8], respectively; P = .03). Interestingly, at the time of the current survey, PfLIgG levels were—with borderline significance—still higher in the placebo group (Table 1). The validity of PfLIgG levels as a proxy measure for the number of malaria episodes during the nonobservation period could be demonstrated by the positive correlation between PfLIgG levels and the malaria incidence rates during the 21-month observation period, showing a similar pattern in each of the study arms (Figure 1A). Accordingly, the individual PfLIgG level at the age of 24 months and that at the time of the current survey showed a slight but significant positive correlation, despite the long time interval between the 2 measurements (Figure 1B). It is noteworthy that the risk of parasite positivity at the time of the survey increased markedly with each measured episode of parasitemia during the first 2 years of life. This effect was approximately linear with an odds ratio of 1.28 (95% confidence interval, 1.20–1.36; P < .001) for each additional episode of parasitemia, independent of SP treatment.
Figure 1.
Correlation of anti–Plasmodium falciparum lysate IgG antibody (PfLIgG) levels and malaria incidence rate. A, Correlation of PfLIgG levels at the age of 24 months with the documented malaria incidence rates during the 21-month observation period. There is a similar pattern in children formerly treated with placebo or sulfadoxine-pyrimethamine (SP). B, Correlation between individual PfLIgG levels at age 24 months and PfLIgG levels at the time of the survey, plotted by treatment. Despite the long time interval between the 2 measurements, there is a positive correlation with a similar pattern in both study arms. PfLIgG level was measured by enzyme-linked immunosorbent assay and expressed in relative units (RUs) as described previously [11]. PYAR, person-years at risk.
Prevalences of outpatient visits, hospital admissions, and anemia were not significantly different between the SP and placebo arms, possibly due to a low power in those variables with rare events. Since the end of the original trial, 5 deaths were reported in the study population, 2 in the placebo arm and 3 in the SP arm. Verbal autopsies were performed during visits to families of the deceased children. Four deaths occurred within 5 months after the last active follow-up and 1 in a child 4 years of age. Two deaths, 1 in each study arm, were assumed to be related to severe malaria; 1 death resembled an acute renal failure of unknown origin; and the remaining 2 deaths were thought to be caused by typhoid fever. No evidence for Stevens-Johnson syndrome, known to be a rare serious adverse event of SP, was recorded.
DISCUSSION
In the present survey, which was performed almost 3 years after the last dose of SP had been given to participants in a clinical trial of IPTi, there were no differences in the malariometric measures, morbidity, or mortality between the 2 study groups. This finding supports the assumption of the absence of a rebound effect, but cross-sectional surveys only depict information at a single point in time, which is clearly inferior to longitudinal studies. Therefore, PfLIgG level was used as a proxy measure for malaria episodes during the nonobservation period [11, 12]. At the end of the original IPTi trial, when participants were 24 months of age, PfLIgG levels were significantly higher in the placebo group than in the SP group, most likely due to the higher malaria incidence rate in the unprotected placebo arm. Unexpectedly, PfLIgG levels still tended to be higher in children of the placebo arm at the time of the current survey. Assuming similar malaria exposure risks in the 2 arms due to environmental factors, there are 3 main interpretations for this observation: The lower PfLIgG level in the SP arm may indicate that (1) a rebound phenomenon with an inhibition of the development of immune responses during and/or after IPTi occurred, (2) malaria episodes were less frequent in the SP arm since the end of the clinical trial, or (3) PfLIgG titers have not yet equalized in both study arms, leading to a remaining imbalance of PfLIgG levels 2 years after the end of the clinical trial. Notably, a selection or reporting bias is unlikely, since all data were derived from a randomized trial and the laboratory personnel measuring PfLIgG levels were blinded to treatment arms.
First, the possibility that SP treatment could have exhibited immunosuppressive effects is conceivable, but unlikely, and such an effect on P. falciparum lysate responses has not been reported so far. Moreover, a review of studies assessing the immune responses after vaccination in combination with SP therapy reported no evidence of relevant differences [13]. Interestingly, antibody responses to single erythrocytic-stage P. falciparum antigens in infants in Mozambique did not significantly differ between children receiving IPTi with SP and those receiving placebo at any time point measured, with the exception of IgG and IgG1 responses to apical membrane antigen 1 and/or merozoite surface protein 1, which were even higher in the SP-treated group [14].
Second, during the observation period there was no further protective efficacy after elimination of SP from the children’s blood, as shown previously [7]. Consequently, long-lasting protective effects beyond posttreatment prophylaxis are not expected, although a sustained protection has been described elsewhere [5]. This is in line with findings from a study in northern Tanzania that tested different antimalarials for IPTi and showed that the benefits of IPTi are directly dependent on the pharmacodynamics of the drugs involved [15]. However, it cannot be excluded that small long-term effects on the risk of parasitemia exist, which could not have been observed clinically. Third, it has been demonstrated before that PfLIgG levels in the second year of life are dependent on the frequency of preceding infections in both study arms [11]. In that study, PfLIgG levels were generally lower in children protected by SP. Furthermore, PfLIgG levels were dependent on malaria incidences in children’s home villages and this correlation was more pronounced in children in the SP arm than in those from the placebo arm, indicating a higher reduction of overall parasitic exposure in more intense transmission settings [16].
One interesting observation, that each parasitemia episode during the first 2 years of life increases the risk of parasite positivity at time of the survey, was independent of former SP treatment. This corresponds to the positive correlation of individual PfLIgG level, which indicates that children with high levels of antibodies in the past also tend to have higher antibody levels years later. Apart from indirectly supporting the hypothesis that immune responses were not selectively inhibited by SP, these results show that individual susceptibilities to P. falciparum are sustainable over years. This is in line with earlier observations that a small percentage of the population suffers the majority of infections [17]. Identifying this high-risk group is essential to successfully targeting future malaria control interventions. Meanwhile, by presumptively treating all infants, IPTi is not very selective, but it is cheap, safe, and effective.
In summary, it seems appropriate to use PfLIgG level as a proxy measure for the number of malaria episodes during the nonobservation period. Accordingly, the most likely explanation for lower PfLIgG levels in children of the SP arm seems to be a lower overall exposure to parasitic antigens in comparison to children who received placebo. Taken together, these findings argue against long-term negative rebound effects after SP-IPTi in areas of high malaria transmission.
Funding
No external funding source, including the IPTi Consortium, had any influence on design and conduct of the study; preparation, review, and approval of the manuscript; or analysis and interpretation of the data.
Acknowledgments
We thank all participants and their parents and/or guardians for participating in the study.
References
- 1.WHO. Report of the Technical Consultation on Intermittent Preventive Treatment in Infants (IPTi), Technical Expert Group on Preventive Chemotherapy. Geneva: April 23–24, 2009. http://malaria.who.int/docs/IPTi/TEGConsultIPTiApr2009Report.pdf. Accessed 10 February 2009. [Google Scholar]
- 2.Grobusch MP, Egan A, Gosling RD, Newman RD. Intermittent preventive therapy for malaria: progress and future directions. Curr Opin Infect Dis. 2007;20:613–20. doi: 10.1097/QCO.0b013e3282f1ae3b. [DOI] [PubMed] [Google Scholar]
- 3.Aponte JJ, Schellenberg D, Egan A, et al. Efficacy and safety of intermittent preventive treatment with sulfadoxine-pyrimethamine for malaria in African infants: a pooled analysis of six randomised, placebo-controlled trials. Lancet. 2009;374:1533–42. doi: 10.1016/S0140-6736(09)61258-7. [DOI] [PubMed] [Google Scholar]
- 4.Gosling RD, Gesase S, Mosha JF, et al. Protective and efficacy safety of three antimalarial regimens for intermittent preventive treatment for malaria in infants: a randomised, double-blind, placebo-controlled trial. Lancet. 2009;374:1521–32. doi: 10.1016/S0140-6736(09)60997-1. [DOI] [PubMed] [Google Scholar]
- 5.Schellenberg D, Menendez C, Aponte JJ, et al. Intermittent preventive antimalarial treatment for Tanzanian infants: follow-up to age 2 years of a randomised, placebo-controlled trial. Lancet. 2005;365:1481–83. doi: 10.1016/S0140-6736(05)66418-5. [DOI] [PubMed] [Google Scholar]
- 6.May J, Adjei S, Busch W, et al. Therapeutic and prophylactic effect of intermittent preventive anti-malarial treatment in infants (IPTi) from Ghana and Gabon. Malar J. 2008;7:198. doi: 10.1186/1475-2875-7-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kobbe R, Kreuzberg C, Adjei S, et al. A randomized controlled trial of extended intermittent preventive antimalarial treatment in infants. Clin Infect Dis. 2007;45:16–25. doi: 10.1086/518575. [DOI] [PubMed] [Google Scholar]
- 8.Chandramohan D, Owusu-Agyei S, Carneiro I, et al. Cluster randomised trial of intermittent preventive treatment for malaria in infants in area of high, seasonal transmission in Ghana. BMJ. 2005;331:727–33. doi: 10.1136/bmj.331.7519.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mockenhaupt FP, Reither K, Zanger P, et al. Intermittent preventive treatment in infants as a means of malaria control: a randomized, double-blind, placebo-controlled trial in northern Ghana. Antimicrob Agents Chemother. 2007;51:3273–81. doi: 10.1128/AAC.00513-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grobusch MP, Gabor JJ, Aponte JJ, et al. No rebound of morbidity following intermittent preventive sulfadoxine-pyrimethamine treatment of malaria in infants in Gabon. J Infect Dis. 2009;200:1658–61. doi: 10.1086/647990. [DOI] [PubMed] [Google Scholar]
- 11.Schreiber N, Kobbe R, Adjei S, Adjei O, Klinkert MQ, May J. Immune responses after single-dose sulphadoxine-pyrimethamine indicate underestimation of protective efficacy of intermittent preventive treatment in infants. Trop Med Int Health. 2007;12:1157–63. doi: 10.1111/j.1365-3156.2007.01902.x. [DOI] [PubMed] [Google Scholar]
- 12.Marsh K, Otoo L, Hayes RJ, Carson DC, Greenwood BM. Antibodies to blood stage antigens of Plasmodium falciparum in rural Gambians and their relation to protection against infection. Trans R Soc Trop Med Hyg. 1989;83:293–303. doi: 10.1016/0035-9203(89)90478-1. [DOI] [PubMed] [Google Scholar]
- 13.Rosen JB, Breman JG. Malaria intermittent preventive treatment in infants, chemoprophylaxis, and childhood vaccinations. Lancet. 2004;363:1386–88. doi: 10.1016/S0140-6736(04)16052-2. [DOI] [PubMed] [Google Scholar]
- 14.Quelhas D, Puyol L, Quintó L, et al. Impact of intermittent preventive treatment with sulfadoxine-pyrimethamine on antibody responses to erythrocytic-stage Plasmodium falciparum antigens in infants in Mozambique. Clin Vaccine Immunol. 2008;15:1282–91. doi: 10.1128/CVI.00044-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cairns M, Gosling R, Carneiro I, et al. Duration of protection against clinical malaria provided by three regimens of intermittent preventive treatment in Tanzanian infants. LoS One. 2010;5:e9467. doi: 10.1371/journal.pone.0009467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kobbe R, Adjei S, Kreuzberg C, et al. Malaria incidence and efficacy of intermittent preventive treatment in infants (IPTi) Malar J. 2007;6:163. doi: 10.1186/1475-2875-6-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith DL, Dushoff J, Snow RW, Hay SI. The entomological inoculation rate and Plasmodium falciparum infection in African children. Nature. 2005;438:492–5. doi: 10.1038/nature04024. [DOI] [PMC free article] [PubMed] [Google Scholar]