Abstract
Background. There is some consensus that malaria in pregnancy may negatively affect infant's mortality and malaria morbidity, but there is less evidence concerning the factors involved.
Methods. A total of 1030 Mozambican pregnant women were enrolled in a randomized, placebo-controlled trial of intermittent preventive treatment with sulfadoxine-pyrimethamine, and their infants were followed up throughout infancy. Overall mortality and malaria morbidity rates were recorded. The association of maternal and fetal risk factors with infant mortality and malaria morbidity was assessed.
Results. There were 58 infant deaths among 997 live-born infants. The risk of dying during infancy was increased among infants born to women with acute placental infection (odds ratio [OR], 5.08 [95% confidence interval (CI), 1.77–14.53)], parasitemia in cord blood (OR, 19.31 [95% CI, 4.44–84.02]), low birth weight (OR, 2.82 [95% CI, 1.27–6.28]) or prematurity (OR, 3.19 [95% CI, 1.14–8.95]). Infants born to women who had clinical malaria during pregnancy (OR, 1.96 [95% CI, 1.13–3.41]) or acute placental infection (OR, 4.63 [95% CI, 2.10–10.24]) had an increased risk of clinical malaria during infancy.
Conclusions. Malaria infection at the end of pregnancy and maternal clinical malaria negatively impact survival and malaria morbidity in infancy. Effective clinical management and prevention of malaria in pregnancy may improve infant's health and survival.
During the last 20 years, mortality rates in infants and children <5 years old have declined steadily worldwide [1]. However, there are still many areas in the world with unacceptably high rates of infant mortality, especially in Sub-Saharan Africa [2]. Many causes have been identified as responsible for infant deaths in developing settings, such as human immunodeficiency virus (HIV), respiratory infections, diarrhea, prematurity, malaria, and malnutrition [3–5]. However, the cause of most infant deaths remains unknown in many developing countries, because most children die at home, few deaths are attended by qualified personnel, and information on specific causes of death is often of poor quality [6, 7].
Malaria infection during pregnancy has been said to cause infant mortality indirectly through its contribution to low birth weight and premature delivery, and it has been estimated that it would be responsible for 75,000–200,000 infant deaths in the sub-Saharan region [8–14]. Some studies have examined this association. Two studies conducted in Sudan and Uganda, respectively, found that peripheral malaria infection during pregnancy was not associated with increased infant mortality [15, 16]. Similarly, another study in Kenya found that placental malaria was not associated with postneonatal mortality in both HIV-positive and HIV-negative mothers [17]. On the other hand, a study in Zaire found that maternal peripheral infection significantly increased the risk of perinatal death; however, placentas were not examined in this study, and the HIV infection status of women in the study was not available [18]. Two more studies in Malawi found that the risk of dying during the postneonatal period was higher for infants born to women with placental malaria infection [19, 20]. Thus, there is still inconclusive evidence in the literature as to the true impact of maternal malaria on infant survival and the factors involved in this association.
There is more consistency with regard to the effect of maternal malaria on the risk of malaria infection during infancy. In Cameroon the prevalence of malaria parasitemia between 4 and 6 months of age was higher among offspring born to women with malaria-infected placentas than in those born to women without placental infection [21].Two other studies carried out in Tanzania and Gabon showed that infants born to multigravid women with placental infection had higher risk of parasitemia or clinical malaria, respectively, than those born to multigravid women without placental infection [22, 23]. A more recent study, conducted in Kenya, found that infants exposed to malaria in utero, but without evidence of immune priming, had an increased risk of malaria infection and anemia during childhood [24].To contribute to the understanding of the effect of malaria in pregnancy on infant's health, which would help guide control policies in pregnancy, the association of maternal and fetal factors with the risk of mortality and clinical malaria during the first year of life was studied in southern Mozambique.
METHODS
Study Area and Population
The study was carried out in Manhiça, Maputo Province, a semirural area in Southern Mozambique. A Demographic Surveillance System is carried out by the Centro de Investigaçâo em Saúde de Manhiça (CISM) and covers Manhiça town and surrounding villages—the Manhiça study area—with a total population under surveillance of ∼80,000 inhabitants. Adjacent to the CISM is the Manhiça District Hospital (MDH), a 110-bed health facility. The characteristics of the study area have been described in detail elsewhere [25]. Malaria transmission of moderate intensity is perennial with some seasonality. The estimated entomological inoculation rate for 2002 was, on average, 38 infective bites per person per year. Anopheles funestus is the main vector [26, 27].
More than 90% of pregnant women attend the Antenatal Clinic (ANC) at least once during pregnancy and ∼80% of the deliveries in this area are institutional (A. Nhacolo, personal communication). In 2005 the infant mortality rate was of 77.4/1000 live births, and the mortality rate in children <5 years old was 148/1000 live births [28]. At the time of the study, malaria control in pregnancy relied on case management only [29]. Prevention of mother-to-child transmission of HIV relied on the administration of a single dose nevirapine to the mother and the newborn [30].
Study Design
The study was carried out as part of a randomized placebo-controlled trial of intermittent preventive treatment with sulfadoxine-pyrimethamine and long-lasting insecticide-treated bed nets for malaria prevention in pregnancy (trial registration number: NCT00209781) [31]. A total of 1030 women were enrolled into the trial at the ANC of the MDH from August 2003 to April 2005, after giving informed consent. There were 1004 live-born infants (501 in the sulfadoxine-pyrimethamine group, 503 in the placebo group); 7 were lost to follow-up owing to migration (3 in the placebo group, 3 in the sulfadoxine-pyrimethamine group) or refusal (1 in the sulfadoxine-pyrimethamine group), resulting in a total of 997 live-born infants that were followed up until 12 months of life and included in this analysis.
An ongoing clinical surveillance system established at the MDH covers all pediatric outpatient and inpatient visits up to 14 years of age. At each consultation, a standardized questionnaire, recording demographic and clinical data, is completed for each attending child. Blood films are prepared for malaria parasite examination, and the hematocrit is measured if there is a history of fever in the preceding 24 h or if the axillary temperature was ≥37.5°C. Clinical malaria episodes are treated according to national guidelines [32]. During the study, a clinical surveillance system was also established at the MDH maternity clinic for all pregnant and puerperal women attending with clinical complaints. Study personnel recorded demographic, obstetric, and clinical information. A capillary blood sample for parasitemia examination and anemia screening was collected if a woman reported clinical symptoms suggestive of malaria. All women were offered voluntary counselling and testing for HIV, and those testing positive and their children were given prophylaxis with nevirapine and referred for adequate clinical follow-up.
At delivery, blood samples were collected from the mother and the umbilical cord for hematological and parasitological determinations. Placental blood and tissue samples were also collected for malaria infection examination. A capillary blood sample was collected from the mother and the infant for parasitological and hematological determinations 8 weeks after delivery. Twelve months after birth a capillary blood sample from the infant was obtained for parasitological and hematological assessment. Deaths occurring during the follow-up period were recorded from hospital records and through the demographic surveillance visits.
Laboratory Methods
Thick and thin blood smears were Giemsa stained and read with a light microscope to quantify parasitemia according to standard, quality-controlled procedures [27, 33]. To identify maternal and infant anemia, hematocrits were read in a Hawksley hematocrit reader (Hawksley & Sons) after centrifuge in a microhematocrit centrifuge. Maternal HIV status was assessed using the Determine HIV-1/2 Rapid Test (Abbott Laboratories) and positive results were confirmed by the Uni-Gold Rapid Test (Trinity Biotech). Syphilis screening was performed with the rapid plasma reagin test, (Syphacard, Wellcome). Placental biopsies and impression smears from placental blood were processed and read according to standard procedures [34, 35].
Statistical Methods and Definitions
Differences in proportions were estimated with Fisher's exact test. Continuous values were evaluated with the nonparametric Wilcoxon test. Odds ratios (ORs) were calculated using logistic regression. Univariate and multivariate analysis were done to evaluate the association between a group of maternal and fetal factors and the risk of infant death and malaria morbidity. Factors included in the models are shown in Table 1 and Table 2. Variables for the multivariate analysis were selected using the backward-stepwise elimination procedure removing variables with a P value of >.05. Study women without a result available for the HIV test were classified as unknown data. Apart from this, the majority of unknown data (placental infection status, birth weight, gestational age) was due to deliveries occurring outside the study health facility, mostly at home. The survival analysis of death between birth and the first birthday, or censoring by withdrawal, whichever occurred first, was estimated using Cox regression models. Data analysis was performed using Stata 11 software (Stata).
Table 1.
Maternal Factors and Infant Mortality
| Infant Mortality |
||||||
| Yes |
No |
|||||
| (n = 58) |
(n = 939) |
|||||
| Maternal Factor | No. | (%) | No. | (%) | P valuea | |
| Gravidity | .422 | |||||
| Primigravid | 19 | (7.5) | 237 | (92.5) | ||
| 1–3 pregnancies | 22 | (5.5) | 373 | (94.5) | ||
| ≥4 or pregnancies | 17 | (5) | 329 | (95) | ||
| HIV test | .009 | |||||
| Negative | 31 | (5) | 614 | (95) | ||
| Positive | 21 | (11) | 176 | (89) | ||
| Unknownb | 6 | (4) | 149 | (96) | ||
| Intervention group | .136 | |||||
| Placebo | 35 | (7) | 465 | (93) | ||
| Sulfadoxine-pyrimethamine | 23 | (5) | 474 | (95) | ||
| Rapid plasma reagin syphilis test | .034 | |||||
| Positive | 12 | (10) | 104 | (90) | ||
| Negative | 46 | (5) | 835 | (95) | ||
| Literacy | .446 | |||||
| Able to read and/or write | 20 | (5) | 390 | (95) | ||
| Unable to read or write | 38 | (6.5) | 546 | (93.5) | ||
| Unknown | 0 | (0) | 3 | (100) | ||
| Malaria episodes during pregnancy | .031 | |||||
| No | 48 | (5) | 860 | (95) | ||
| Yes | 10 | (11) | 79 | (89) | ||
NOTE.
Unadjusted P value (Fisher's exact test).
Refused voluntary counseling and testing.
Table 2.
Fetal Outcomes and Infant Mortality
| Fetal Outcome |
Infant Mortality |
|||||
| Yes |
No |
P valuea | ||||
| (n = 58) |
(n = 939) |
|||||
| No. | (%) | No. | (%) | |||
| Sex of newborn | .436 | |||||
| Male | 34 | (7) | 479 | (93) | ||
| Female | 24 | (5) | 456 | (95) | ||
| Unknown | 0 | (0) | 4 | (100) | ||
| Premature delivery | <.001 | |||||
| No | 37 | (4) | 870 | (96) | ||
| Yes | 10 | (25) | 30 | (75) | ||
| Unknown | 11 | (22) | 39 | (78) | ||
| Low birth weight | <.001 | |||||
| No | 37 | (4) | 835 | (96) | ||
| Yes | 19 | (16) | 97 | (84) | ||
| Unknown | 2 | (10.5) | 17 | (89.5) | ||
| Fetal anemia (hematocrit, <37%) | .378 | |||||
| No | 45 | (6) | 719 | (94) | ||
| Yes | 6 | (9) | 63 | (91) | ||
| Unknown | 7 | (4) | 157 | (96) | ||
| Cord blood parasitemia | .002 | |||||
| No | 46 | (6) | 779 | (94) | ||
| Yes | 4 | (44) | 5 | (56) | ||
| Unknown | 8 | (5) | 155 | (95) | ||
| Placental malariab | .008 | |||||
| Not infected | 20 | (5) | 404 | (95) | ||
| Past infection | 18 | (6) | 303 | (94) | ||
| Acute infection | 7 | (17) | 35 | (83) | ||
| Chronic infection | 9 | (11) | 73 | (89) | ||
| Unknown | 4 | (3) | 124 | (97) | ||
NOTE.
Unadjusted P value (Fisher's exact test).
Past infection was defined as the presence of malaria pigment but not parasites; acute infection, as the presence of malaria parasites and minimal pigment; and chronic infection, as the presence of malaria parasites and pigment.
Maternal clinical malaria was defined as P. falciparum asexual parasitemia of any density in a peripheral blood slide plus any signs and/or symptoms suggestive of malaria disease, such as referred history of fever in the last 24 h, fever (axillary temperature, ≥37.5°C), pallor, arthromyalgias, headache, or history of convulsions. The definition of clinical malaria in infants used in the passive morbidity surveillance was presence of fever (axillary temperature, ≥37.5°C) or a history of fever in the preceding 24 h plus a P. falciparum asexual parasitemia of any density on a blood slide. The duration of a malaria episode was estimated as 28 days to avoid counting the same episode twice. Subjects were not considered at risk during the 28 days after an episode and did not contribute to either the denominator or the numerator during this period. Fetal anemia was defined as a hematocrit level in cord blood <37%. According to a previous definition based on histological examination, placental infection was classified as past (presence of malaria pigment only), acute (presence of parasites and minimal pigment), or chronic (presence of malaria parasites and pigment). Active infection includes both acute and chronic infection [36].
RESULTS
There were 1004 live-born infants born to the 1030 enrolled pregnant women, of whom 997 infants (99%) were included in the analysis. There were 58 infant deaths, 25 in the neonatal period (<28 days after birth). Of the 25 infants who died within the neonatal period, 20 (80%) died within the first week of life (early neonatal mortality).
Univariate Analysis of Maternal and Fetal Factors and Association with Infant Mortality
Table 1 and Table 2 show the crude analysis of maternal and fetal factors respectively and their association with infant mortality. Maternal HIV status (21/197 [11%] vs 31/645 [5%]; P = .009), a positive rapid plasma reagin test (12/116 [10%] vs 46/881 [5%]; P = .034)], and clinical malaria episodes during pregnancy (10/89 [11%] vs 48/908 [5%]; P = .031) were all significantly associated with an increased risk of dying during infancy. Premature delivery (10/40 [25%] vs 37/907 [4%]; P < .001), low birth weight (19/116 [16%] vs 37/872 [4%]; P < .001), cord blood parasitemia (4/9 [44%] vs 46/825 [6%]; P = .002), and acute placental malaria infection (7/42 [17%]; P = .008) were also associated with an increased risk of infant mortality.
Multivariate Analysis of Maternal and Fetal Factors and Association with Infant Mortality
The adjusted analysis of the association between maternal and fetal outcomes with infant mortality is shown in Table 3. Among infants born to HIV-positive mothers, the risk of death was more than twice as high as that in infants born to HIV-negative mothers (OR, 2.59 [95% confidence interval (CI), 1.35–4.98]; P = .005). Infant mortality was strongly associated with both low birth weight and prematurity (OR for low birth weight, 2.82 [95% CI, 1.27–6.28]; P = .012; OR for prematurity, 3.19 [95% CI, 1.14–8.95]; P < .001).
Table 3.
Risk Factors for Infant Mortality: Adjusted Multivariate Model (n = 967)a
| Risk Factor | OR | (95% CI) | P value | |
| HIV test | .005 | |||
| Negative | 1 | |||
| Positive | 2.59 | (1.35–4.98) | ||
| Unknownb | 0.64 | (0.23–1.82) | ||
| Any malaria episodes during pregnancy | .087 | |||
| No | 1 | |||
| Yes | 2.14 | (0.90–5.10) | ||
| Premature delivery | <.001 | |||
| No | 1 | |||
| Yes | 3.19 | (1.14–8.95) | ||
| Unknown | 29.82 | (9.97–89.21) | ||
| Low birth weight (<2500 g) | .012 | |||
| No | 1 | |||
| Yes | 2.82 | (1.27–6.28) | ||
| Unknown | 19.94 | |||
| Fetal anemia (hematocrit, <37%) | .077 | |||
| No | 1 | |||
| Yes | 1.07 | (0.39–2.90) | ||
| Unknown | 0.04 | (0.00–0.69) | ||
| Cord blood parasitemia | <.001 | |||
| Not infected | 1 | |||
| Infected | 19.31 | (4.44–84.02) | ||
| Unknown | 6.57 | (.63–68.64) | ||
| Placental malariac | .012 | |||
| Not infected | 1 | |||
| Past infection | 1.12 | (.53–2.33) | ||
| Acute infection | 5.08 | (1.77–14.53) | ||
| Chronic | 1.55 | (.59–4.04) | ||
| Unknown | 0.25 | (.04–1.83) | ||
| Intervention group | .189 | |||
| Placebo | 1 | |||
| Sulfadoxine-pyrimethamine | 0.44 | (.13–1.49) | ||
NOTE.
Factors included in the models are those shown in Table 1 and Table 2. CI, confidence interval; HIV, human immunodeficiency virus; OR, odds ratio.
Refused voluntary counseling and testing.
Past infection was defined as the presence of malaria pigment but not parasites; acute infection, as the presence of malaria parasites and minimal pigment; and chronic infection, as the presence of malaria parasites and pigment.
The risk of dying during infancy was also independently associated with malaria infection of the placenta (P = .012). This increased risk was mainly accounted for by women with acute placental malaria (OR, 5.08 [95% CI, 1.77–14.53]). Cord blood parasitemia was also significantly associated with an increased risk of infant mortality (OR, 19.31 [95% CI, 4.44–84.02]; P < .001]. There were more infant deaths among women who had an episode of clinical malaria during pregnancy, although this difference was of borderline statistical significance (OR, 2.14 [95% CI, 0.90–5.10]; P = .087].
Interestingly, when just the postneonatal period was considered, the risk of death was also higher among infants born to women who had acute placental infection (OR, 5.79 [95% CI, 1.81–18.51]; P < .019), parasites in the cord blood (OR, 21.30 [95% CI, 3.56–127.36]; P < .003), or clinical malaria during gestation (OR, 2.84 [95% CI, 1.03–7.86]; P < .045).
Multivariate Analysis of the Risk of Clinical Malaria in the First Year of Life
Table 4 shows the adjusted analysis of the association between maternal and fetal factors and infant malaria morbidity. Infants born to women who had clinical malaria episodes during pregnancy had nearly twice as high a risk of having clinical malaria during the first year of life as did infants born to women who did not have malaria during pregnancy (OR, 1.96 [95% CI, 1.13–3.41]; P = .016]. The risk of clinical malaria was also increased in infants born to women with placental malaria infection. This increased risk was accounted mainly for women with acute placental infection (OR, 4.63 [95% CI, 2.10–10.24]), followed by chronic infection (OR, 3.95 [95% CI, 2.07–7.55]) and past infection (OR, 3.06 [95% CI, 1.94–4.82]; P < .001). Children born to women with HIV infection had a lower risk of clinical malaria episodes during infancy (OR, 0.50 [95% CI, 0.30–0.85]; P = .017]
Table 4.
Risk Factors for Clinical Malaria Episodes in Infants (n = 997)a
| Univariate Model |
Multivariate Model |
||||||
| Risk Factor | OR | (95% CI) | P value | OR | (95% CI) | P value | |
| Maternal HIV test | .030 | .017 | |||||
| Negative | 1 | 1 | |||||
| Positive | 0.56 | (0.34–0.93) | .50 | (0.30–0.85) | |||
| Unknownb | 0.61 | (0.35–1.10) | 0.62 | (0.35–1.10) | |||
| Any malaria episodes during pregnancy | .001 | .016 | |||||
| No | 1 | 1 | |||||
| Yes | 2.40 | (1.45–3.98) | 1.96 | (1.13–3.41) | |||
| Maternal mid–upper arm circumference | .028 | .008 | |||||
| >22 cm | 1 | 1 | |||||
| ≤22 cm | 1.21 | (0.34–4.30) | 1.40 | (0.37–5.31) | |||
| Unknown | 0.50 | (0.29–0.83) | 0.43 | (0.25–0.74) | |||
| Placental malariac | <.001 | <.001 | |||||
| Not infected | 1 | 1 | |||||
| Past infection | 3.43 | (2.20–5.33) | 3.06 | (1.94–4.82) | |||
| Acute infection | 4.20 | (1.94–9.12) | 4.63 | (2.10–10.24) | |||
| Chronic infection | 3.82 | (2.06–7.08) | 3.95 | (2.07–7.55) | |||
| Unknown | 0.90 | (0.42–1.93) | 0.88 | (0.41–1.92) | |||
| Gravidity | .199 | … | |||||
| Primigravid | 1 | … | … | ||||
| 1–3 pregnancies | 0.71 | (0.46–1.09) | … | … | |||
| ≥4 pregnancies | 0.70 | (0.45–1.09) | … | … | |||
| Intervention group | .166 | … | |||||
| Placebo | 1 | … | … | ||||
| Sulfadoxine-pyrimethamine | 1.28 | (0.90–1.83) | … | … | |||
| Rapid plasma reagin syphilis test | .551 | … | |||||
| Positive | 1 | … | … | ||||
| Negative | 1.17 | (0.69–1.99) | … | … | |||
| Literacy | .608 | … | |||||
| Able to read and/or write | 1 | … | … | ||||
| Unable to read or write | 1.10 | (0.77–1.58) | … | … | |||
| Sex of newborn | .288 | … | |||||
| Male | 1 | … | … | ||||
| Female | 1.21 | (0.85–1.72) | … | … | |||
| Premature delivery | .380 | … | |||||
| No | 1 | … | … | ||||
| Yes | 0.81 | (0.31-2.10) | … | … | |||
| Unknown | 0.49 | (0.17–1.39) | … | … | |||
| Low birth weight | .581 | … | |||||
| No | 1 | … | … | ||||
| Yes | 1.16 | (0.68–1.96) | … | … | |||
| Fetal anemia (hematocrit, <37%) | .019 | … | |||||
| No | 1 | … | … | ||||
| Yes | 0.88 | (0.44–1.77) | … | … | |||
| Unknown | 0.41 | (0.22–0.76) | … | … | |||
| Cord blood parasitemia | .020 | … | |||||
| No | 1 | … | … | ||||
| Yes | 0.66 | (0.08–5.29) | … | … | |||
| Unknown | 0.42 | (0.23–0.77) | … | … | |||
NOTE.
Factors included in the models are those shown in Table 1 and Table 2. CI, confidence interval; HIV, human immunodeficiency virus; OR, odds ratio.
Refused voluntary counseling and testing.
Past infection was defined as the presence of malaria pigment but not parasites; acute infection, the presence of malaria parasites and minimal pigment; and chronic infection, the presence of malaria parasites and pigment.
Placental Malaria and Malaria Morbidity in the Infant
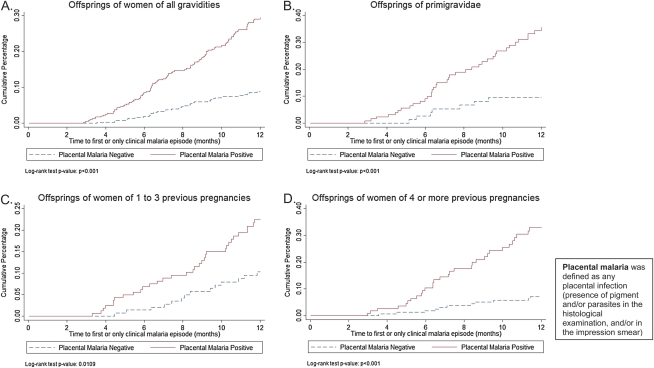
A total of 135 first clinical malaria episodes were recorded among the 997 infants followed up during the first year of life. Of these episodes, 102 (75.7%) malaria episodes occurred among infants born to women with any placental infection (presence of pigment and/or parasites at histological examination and/or in the impression smear), and 33 (24.3%) occurred among infants born to women without malaria infection in the placenta (P < .001). Among infants born to primigravid women, 38 (84.4%) of the 45 first malaria episodes recorded occurred in infants born to women with placental malaria, compared with 7 (15.6%) episodes recorded in infants whose mothers did not have placental infection (P < .001). Among infants born to women with 1–3 previous pregnancies, 33 (68.8%) of the 48 episodes recorded occurred in infants whose mothers had placental infection, compared with 15 (31.2%) malaria episodes among those whose mothers did not have placental infection (P = .018). Finally, among women with ≥4 previous pregnancies, 31 (73.8%) of 42 clinical malaria episodes occurred in infants born to women with placental infection, compared with 11 (26.2%) among infants whose mothers did not have placental malaria (P < .001). Figure 1 shows the Kaplan-Meier curves of the time to first or only clinical malaria episodes in infants by parity and placental infection. The incidence rate of clinical malaria episodes among infants born to women with placental infection was 0.28 episodes per person-year at risk, compared with 0.09 among infants born to women without placental infection (P < .001). This difference was similar in all parity groups (P = .001 in primigravid women, P = .012 in women with 1–3 previous pregnancies, and P < .001 in women with ≥4 previous pregnancies).
Figure 1.
Time to first or only clinical malaria episode in infants born to women with placental malaria compared with those born to women without placental malaria, by parity. Infants born to women of all parities (A), primigravid women (B), women with 1–3 previous pregnancies (C), and women with ≥4 previous pregnancies (D). P values adjusted by season: <.001 (primigravid women), .014 (1–3 previous pregnancies), <.001 (≥4 pregnancies), and <.001 (all gravidities). P values adjusted by previous malaria episodes during pregnancy: .002 (primigravid women), <.026 (1–3 previous pregnancies), <.001 (≥4 pregnancies), and <.001 (all gravidities).
DISCUSSION
This study builds on previous evidence showing a negative impact of malaria infection during pregnancy on the risk to malaria in the infant [21, 23, 37]. It also confirms the inconclusive evidence on the negative effect of maternal infection on infants’ survival [18–20].
The detailed placental examination done in this study revealed that placental infections occurring at the end of pregnancy are those most likely to have an impact on infants' survival. This is supported by the independent, significant association of both acute placental infection (parasites with or without minimal pigment deposition) and cord blood parasitemia with an increase in the infant's risk of death. The inflammatory changes associated with malaria infection in the placenta may compromise the transfer of metabolic and nutrient factors, as well as fetal oxygen supply, all of which may negatively affect the developing fetus [39–42]. In addition, it has been reported that placental malaria is associated with a reduction in the placental transfer of antibodies [43, 44]. This may affect the immune status of the newborn and thus make the infant more vulnerable to infectious diseases [45, 46]. The latter could explain why the effect of acute placental malaria seems to extend beyond the neonatal period.
Little is known of the actual impact of congenital malaria, defined as the presence of cord blood parasitemia, on the infant's health in endemic areas other than an increased frequency of anemia a few months after birth [47]. Cord blood parasitemia is usually of low density, but it may be more frequent than previously thought, as is shown when molecular techniques are used for parasite detection [48]. Malaria parasites may cross the placenta either during pregnancy or at the time of delivery. Vertical transmission of malaria is likely to have important implications for fetal and newborn development. Direct infection of the fetus may be associated with preterm delivery and fetal growth restriction or could increase the likelihood of stillbirth. Fetal exposure to blood-stage malaria antigens may also have profound long-term effects during infancy by priming the immune responses of the fetus, inducing immune tolerance, or both [24, 48]. Depending on the effect on the fetal immune system, exposure to the parasite antigens in utero may cause a reduced (priming) or increased (immune tolerance) susceptibility to malaria in the infant [49].
An alternative explanation for the increased risk of infant mortality associated with the presence of parasites at the end of pregnancy may be the occurrence of confounding factors that are independently associated with both the risk of malaria and death. These may be poor socioeconomic, nutritional or other health-related factors. In this study no difference was observed in socioeconomic or nutritional factors between women with and those without malaria infection during pregnancy or at delivery (data not shown).
The presence of parasites in the placenta was also associated with an increased incidence of malaria episodes during infancy. Again, this association might be explained by a similar level of exposure to the infection in both mother and infant, or it may indicate an increased immune susceptibility to malaria in the infant due to in utero antigenic exposure [24].
Malaria morbidity during pregnancy has not been reported in other studies in which peripheral and/or placental infection was studied in relation to outcomes in infants. Importantly, clinical malaria episodes during pregnancy were associated with both a trend to increased infant mortality and a significant increased incidence of malaria episodes during infancy. These effects were independent of the presence of placental malaria, suggesting that pathophysiological mechanisms other than those associated with placental infection may be responsible for the negative impact of maternal malaria on infant health. This also indicates that in addition to implementating malaria-preventive strategies, it is also important to improve the detection and adequate treatment of malaria episodes during pregnancy.
In this cohort of infants, clinical malaria episodes were more frequent, and the incidence of first or only episodes higher among infants born to mothers with placental malaria. This increased incidence of malaria episodes in infants born to women with placental malaria was similar across all parity groups (Figure 1). These results do not support findings from a Tanzanian cohort of infants in which this association varied with parity, being significant only among multigravid women [37]. In that study the authors speculate that differences in inflammatory reactions in the placenta between primigravid and multigravid women were responsible for the increased risk of malaria in infants born to multigravid women with placental infection. Our results are consistent with those of 2 other studies that found no parity difference in the risk of malaria among infants born to women with placental infection [23, 24]. This discrepancy indicates that the role of parity in the relationship between placental infection and malaria morbidity risk in infants is not completely resolved, and more careful research still needs to be done to understand the pathogenic mechanisms of maternal malaria and its impact on infants' health.
Other factors such as low birth weight, prematurity and maternal HIV infection, have all been reported elsewhere to be associated with infant mortality [8, 12, 50]. Interestingly, maternal HIV infection was associated with a reduced risk of clinical malaria in infants. This might be explained by the occurrence of deaths in these infants before the age when the risk of clinical malaria begins to increase at ∼6 months [32].
Even though pregnant women in this study received all or part of the currently recommended malaria-preventive measures, the occurrence of poor pregnancy outcomes associated with the infection was not completely abolished. It is important to keep in mind that neither of these measures are 100% effective in preventing malarial infection. More effective antimalarial drugs for intermittent preventive treatment in pregnancy with prolonged prophylactic effect, as well as increased compliance with the use of insecticide-treated bed nets could further reduce the harmful effects of maternal malaria on infants.
In summary, the results of this study confirm that malaria during pregnancy, particularly in the last stage, may be determinant for infant health. These findings emphasize the importance of developing and implementing effective malaria control strategies throughout gestation in women of all gravidities and also suggest that their beneficial effects in infants may extend to the first year of life.
Funding
This work was supported by the Banco de Bilbao, Vizcaya, Argentaria Foundation (grant number BBVA 02-0). The Centro de Investigaçao em Saude de Manhiça receives major core funding from the Spanish Agency for International Cooperation.
Acknowledgments
We are grateful to the women who participated in the study. We also thank the staff of the Manhiça Health Center, especially those at the maternity clinic, and the staff at the Manhiça Health Research Center (CISM). Special thanks to Sonia Amos for her dedication throughout the study.
References
- 1.United Nations. The Millennium Development Goals report. 2010 [Google Scholar]
- 2.Statistical Annex. United Nations. The Millennium Development Goals report. 2009 MDG Indicators Database. [Google Scholar]
- 3.Hamer DH, Mwanakasale V, Macleod WB, et al. Two-dose versus monthly intermittent preventive treatment of malaria with sulfadoxine-pyrimethamine in HIV-seropositive pregnant Zambian women. J Infect Dis. 2007;196:1585–94. doi: 10.1086/522142. [DOI] [PubMed] [Google Scholar]
- 4.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361:2226–34. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 5.Bryce J, Boschi-Pinto C, Shibuya K, Black RE. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 6.Sacarlal J, Nhacolo AQ, Sigauque B, et al. A 10 year study of the cause of death in children under 15 years in Manhica, Mozambique. BMC Public Health. 2009;9:67. doi: 10.1186/1471-2458-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdullah S, Adazu K, Masanja H, et al. Patterns of age-specific mortality in children in endemic areas of sub-Saharan Africa. Am J Trop Med Hyg. 2007;77:99–105. [PubMed] [Google Scholar]
- 8.Greenwood BM, Greenwood AM, Snow RW, Byass P, Bennett S, Hatib-N'Jie AB. The effects of malaria chemoprophylaxis given by traditional birth attendants on the course and outcome of pregnancy. Trans R Soc Trop Med Hyg. 1989;83:589–94. doi: 10.1016/0035-9203(89)90362-3. [DOI] [PubMed] [Google Scholar]
- 9.Brabin B. An assessment of low birthweight risk in primiparae as an indicator of malaria control in pregnancy. Int J Epidemiol. 1991;20:276–83. doi: 10.1093/ije/20.1.276. [DOI] [PubMed] [Google Scholar]
- 10.Menendez C, Ordi J, Ismail MR, et al. The impact of placental malaria on gestational age and birth weight. J Infect Dis. 2000;181:1740–5. doi: 10.1086/315449. [DOI] [PubMed] [Google Scholar]
- 11.Romagosa C, Ordi J, Saute F, et al. Seasonal variations in maternal mortality in Maputo, Mozambique: the role of malaria. Trop Med Int Health. 2007;12:62–7. doi: 10.1111/j.1365-3156.2006.01755.x. [DOI] [PubMed] [Google Scholar]
- 12.Steketee RW, Nahlen BL, Parise ME, Menendez C. The burden of malaria in pregnancy in malaria-endemic areas. Am J Trop Med Hyg. 2001;64:28–35. doi: 10.4269/ajtmh.2001.64.28. [DOI] [PubMed] [Google Scholar]
- 13.Greenwood AM, Armstrong JR, Byass P, Snow RW, Greenwood BM. Malaria chemoprophylaxis, birth weight and child survival. Trans R Soc Trop Med Hyg. 1992;86:483–5. doi: 10.1016/0035-9203(92)90078-q. [DOI] [PubMed] [Google Scholar]
- 14.Luxemburger C, McGready R, Kham A, et al. Effects of malaria during pregnancy on infant mortality in an area of low malaria transmission. Am J Epidemiol. 2001;154:459–65. doi: 10.1093/aje/154.5.459. [DOI] [PubMed] [Google Scholar]
- 15.Haghdoost AA, Alexander N, Smith T. Maternal malaria during pregnancy and infant mortality rate: critical literature review and a new analytical approach. J Vector Borne Dis. 2007;44:98–104. [PubMed] [Google Scholar]
- 16.Brahmbhatt H, Sullivan D, Kigozi G, et al. Association of HIV and malaria with mother-to-child transmission, birth outcomes, and child mortality. J Acquir Immune Defic Syndr. 2008;47:472–6. doi: 10.1097/QAI.0b013e318162afe0. [DOI] [PubMed] [Google Scholar]
- 17.van Eijk AM, Ayisi JG, Ter Kuile FO, et al. HIV, malaria, and infant anemia as risk factors for postneonatal infant mortality among HIV-seropositive women in Kisumu, Kenya. J Infect Dis. 2007;196:30–7. doi: 10.1086/518441. [DOI] [PubMed] [Google Scholar]
- 18.Nyirjesy P, Kavasya T, Axelrod P, Fischer PR. Malaria during pregnancy: neonatal morbidity and mortality and the efficacy of chloroquine chemoprophylaxis. Clin Infect Dis. 1993;16:127–32. doi: 10.1093/clinids/16.1.127. [DOI] [PubMed] [Google Scholar]
- 19.Bloland PB, Wirima JJ, Steketee RW, Chilima B, Hightower A, Breman JG. Maternal HIV infection and infant mortality in Malawi: evidence for increased mortality due to placental malaria infection. AIDS. 1995;9:721–6. doi: 10.1097/00002030-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Verhoeff FH, Le Cessie S, Kalanda BF, Kazembe PN, Broadhead RL, Brabin BJ. Post-neonatal infant mortality in Malawi: the importance of maternal health. Ann Trop Paediatr. 2004;24:161–9. doi: 10.1179/027249304225013448. [DOI] [PubMed] [Google Scholar]
- 21.Le Hesran JY, Cot M, Personne P, et al. Maternal placental infection with Plasmodium falciparum and malaria morbidity during the first 2 years of life. Am J Epidemiol. 1997;146:826–31. doi: 10.1093/oxfordjournals.aje.a009200. [DOI] [PubMed] [Google Scholar]
- 22.Mutabingwa TK. Artemisinin-based combination therapies (ACTs): best hope for malaria treatment but inaccessible to the needy! Acta Trop. 2005;95:305–15. doi: 10.1016/j.actatropica.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 23.Schwarz NG, Adegnika AA, Breitling LP, et al. Placental malaria increases malaria risk in the first 30 months of life. Clin Infect Dis. 2008;47:1017–25. doi: 10.1086/591968. [DOI] [PubMed] [Google Scholar]
- 24.Malhotra I, Dent A, Mungai P, et al. Can prenatal malaria exposure produce an immune tolerant phenotype? A prospective birth cohort study in Kenya. PLoS Med. 2009;6:e1000116. doi: 10.1371/journal.pmed.1000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alonso PLSF, Aponte JJ, Gómez-Olivé FX, et al. Population and health in developing countries. Vol 1. Population, health, and survival at INDEPTH sites. 1st ed. Ottawa, Ontario: International Development Research Centre; 2002. Mozambique. In INDEPTH; pp. 189–95. [Google Scholar]
- 26.Aranda C, Aponte JJ, Saute F, et al. Entomological characteristics of malaria transmission in Manhica, a rural area in southern Mozambique. J Med Entomol. 2005;42:180–6. doi: 10.1093/jmedent/42.2.180. [DOI] [PubMed] [Google Scholar]
- 27.Alonso PL, Sacarlal J, Aponte JJ, et al. Efficacy of the RTS, S/AS02A vaccine against Plasmodium falciparum infection and disease in young African children: randomised controlled trial. Lancet. 2004;364:1411–20. doi: 10.1016/S0140-6736(04)17223-1. [DOI] [PubMed] [Google Scholar]
- 28.Nhacolo AQ, Nhalungo DA, Sacoor CN, Aponte JJ, Thompson R, Alonso P. Levels and trends of demographic indices in southern rural Mozambique: evidence from demographic surveillance in Manhica district. BMC Public Health. 2006;6:291. doi: 10.1186/1471-2458-6-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Documento estrategico para o controlo e combate da Malaria em Moçambique, 2006- 2009. Programa Nacional de Controlo de Malaria. Ministerio da Saúde de Moçambique Maputo, 2006 [Google Scholar]
- 30.Programa Nacional de Controlo de ITS/HIV/SIDA. Plano estratégico nacional de combate às ITS/HIV/SIDA do Ministério da Saúde 2004-2008. Maputo, Mozambique: Ministério da Saúde; 2004. [Google Scholar]
- 31.Menendez C, Bardaji A, Sigauque B, et al. A randomized placebo-controlled trial of intermittent preventive treatment in pregnant women in the context of insecticide treated nets delivered through the antenatal clinic. PLoS ONE. 2008;3:e1934. doi: 10.1371/journal.pone.0001934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guinovart C, Bassat Q, Sigauque B, et al. Malaria in rural Mozambique. I. Children attending the outpatient clinic. Malar J. 2008;7:36. doi: 10.1186/1475-2875-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alonso PL, Smith T, Schellenberg JR, et al. Randomised trial of efficacy of SPf66 vaccine against Plasmodium falciparum malaria in children in southern Tanzania. Lancet. 1994;344:1175–81. doi: 10.1016/s0140-6736(94)90505-3. [DOI] [PubMed] [Google Scholar]
- 34.Ordi J, Ismail MR, Ventura PJ, et al. Massive chronic intervillositis of the placenta associated with malaria infection. Am J Surg Pathol. 1998;22:1006–11. doi: 10.1097/00000478-199808000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Rogerson SJ, Mkundika P, Kanjala MK. Diagnosis of Plasmodium falciparum malaria at delivery: comparison of blood film preparation methods and of blood films with histology. J Clin Microbiol. 2003;41:1370–4. doi: 10.1128/JCM.41.4.1370-1374.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ismail MR, Ordi J, Menendez C, et al. Placental pathology in malaria: a histological, immunohistochemical, and quantitative study. Hum Pathol. 2000;31:85–93. doi: 10.1016/s0046-8177(00)80203-8. [DOI] [PubMed] [Google Scholar]
- 37.Mutabingwa TK, Bolla MC, Li JL, et al. Maternal malaria and gravidity interact to modify infant susceptibility to malaria. PLoS Med. 2005;2:e407. doi: 10.1371/journal.pmed.0020407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Menendez C, Bardaji A, Sigauque B, et al. Malaria prevention with IPTp during pregnancy reduces neonatal mortality. PLoS ONE. 5:e9438. doi: 10.1371/journal.pone.0009438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Duffy PE, Fried M, editors. Malaria in pregnancy: deadly parasite, susceptible host. New York, Taylor & Francis: 2001. pp. 70–126. [Google Scholar]
- 40.Brabin BJ, Romagosa C, Abdelgalil S, et al. The sick placenta-the role of malaria. Placenta. 2004;25:359–78. doi: 10.1016/j.placenta.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 41.Brabin BJ, Fletcher KA, Brown N. Do disturbances within the folate pathway contribute to low birth weight in malaria? Trends Parasitol. 2003;19:39–43. doi: 10.1016/s1471-4922(02)00004-1. [DOI] [PubMed] [Google Scholar]
- 42.de Moraes-Pinto MI, Verhoeff F, Chimsuku L, et al. Placental antibody transfer: influence of maternal HIV infection and placental malaria. Arch Dis Child Fetal Neonatal Ed. 1998;79:F202–5. doi: 10.1136/fn.79.3.f202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brair ME, Brabin BJ, Milligan P, Maxwell S, Hart CA. Reduced transfer of tetanus antibodies with placental malaria. Lancet. 1994;343:208–9. doi: 10.1016/s0140-6736(94)90991-1. [DOI] [PubMed] [Google Scholar]
- 44.O'Dempsey TJ, McArdle TF, Lloyd-Evans N, et al. Pneumococcal disease among children in a rural area of west Africa. Pediatr Infect Dis J. 1996;15:431–7. doi: 10.1097/00006454-199605000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Riley EM, Wagner GE, Akanmori BD, Koram KA. Do maternally acquired antibodies protect infants from malaria infection? Parasite Immunol. 2001;23:51–9. doi: 10.1046/j.1365-3024.2001.00364.x. [DOI] [PubMed] [Google Scholar]
- 46.Brabin B. Fetal anaemia in malarious areas: its causes and significance. Ann Trop Paediatr. 1992;12:303–10. doi: 10.1080/02724936.1992.11747589. [DOI] [PubMed] [Google Scholar]
- 47.Ndyomugyenyi R, Magnussen P. Chloroquine prophylaxis, iron/folic-acid supplementation or case management of malaria attacks in primigravidae in western Uganda: effects on congenital malaria and infant haemoglobin concentrations. Ann Trop Med Parasitol. 2000;94:759–68. doi: 10.1080/00034980020015189. discussion 769–70. [DOI] [PubMed] [Google Scholar]
- 48.Menendez C, Mayor A. Congenital malaria: the least known consequence of malaria in pregnancy. Semin Fetal Neonatal Med. 2007;12:207–13. doi: 10.1016/j.siny.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 49.Rasheed FN. Maternal infections influence infection susceptibility in childhood. Med Hypotheses. 1994;42:76–80. doi: 10.1016/0306-9877(94)90079-5. [DOI] [PubMed] [Google Scholar]
- 50.Naniche D, Lahuerta M, Bardaji A, et al. Mother-to-child transmission of HIV-1: association with malaria prevention, anaemia and placental malaria. HIV Med. 2008;9:757–64. doi: 10.1111/j.1468-1293.2008.00626.x. [DOI] [PubMed] [Google Scholar]