Abstract
Background:
Routine turning of critically ill patients is a standard of care. In recent years, specialized beds that provide automated turning have been introduced. These beds have been reported to improve lung function, reduce hospital-acquired pneumonia, and facilitate secretion removal. This trial was designed to measure the physiological effects of routine turning and respiratory therapy in comparison with continuous lateral rotation (CLR).
Methods:
The study was a prospective, quasi-experimental, random assignment, trial with patients serving as their own controls. Paralyzed, sedated patients with acute respiratory distress syndrome were eligible for study. Patients were randomized to receive four turning and secretion management regimens in random sequence for 6 h each over a period of 24 h: (1) routine turning every 2 h from the left to right lateral position; (2) routine turning every 2 h from the left to right lateral position including a 15-min period of manual percussion and postural drainage (P&PD); (3) CLR with a specialized bed that turned patients from left to right lateral position, pausing at each position for 2 min; and (4) CLR with a specialized bed that turned patients from left to right lateral position pausing at each position for 2 min, and a 15-min period of percussion provided by the pneumatic cushions of the bed every 2 h.
Results:
Nineteen patients were entered into the study. There were no statistically significant differences in the measured cardiorespiratory variables. There was a tendency for the ratio of partial pressure of arterial oxygen to fractional inspired oxygen concentration (PaO2/FIO2) to increase (174 ± 31 versus 188 ± 36; P = 0.068) and for the ratio of deadspace to tidal volume (Vd/Vt) to decrease (0.62 ± 0.18 versus 0.59 ± 0.18; P = 0.19) during periods of CLR, but these differences did not achieve statistical significance. There were statistically significant increases in sputum volume during the periods of CLR. The addition of P&PD did not increase sputum volume for the group as a whole. However, in the four patients producing more than 40 ml of sputum per day, P&PD increased sputum volume significantly. The number of patient turns increased from one every 2 h to one every 10 min during CLR.
Conclusion:
The acute effects of CLR are undoubtedly different in other patient populations (spinal cord injury and unilateral lung injury). The link between acute physiological changes and improved outcomes associated with CLR remain to be determined.
Keywords: continuous lateral rotation, hypoxemia, mechanical ventilation, paralysis, positioning, secretion removal, sedation
Introduction
The complications of bed rest have been known for nearly a century [1]. Routine care of mechanically ventilated patients typically involves a regimen of body position changes to aid in the prevention of skin breakdown, to enhance secretion clearance, and to improve ventilation/ perfusion relationships [2,3]. In the recent past, specialized beds have been introduced that automatically turn patients on a much more frequent basis independently of caregiver availability. Several clinical trials have suggested that this type of rotational or 'kinetic' therapy might reduce the incidence of hospital-acquired pneumonia and reduce the duration of stay in an intensive care unit (ICU) [4,5,6,7,8,9]. Each of these studies can be criticized for design errors, and these specialized beds are not in routine use at present. Interestingly, little work has been performed to evaluate the physiological effects of rotational therapy. In fact, a recent paper was the first to evaluate gas exchange during short periods of rotation in comparison with the supine position [10].
We designed a study to evaluate the acute physiological effects of rotational therapy in a group of critically ill, paralyzed, mechanically ventilated patients with acute respiratory distress syndrome (ARDS) over a 24-h period.
Materials and methods
The study was approved by the Institutional Review Board of the University of Cincinnati, and informed consent was obtained from the next of kin. Inclusion criteria included (1) patients with ARDS as defined by the North American-European Consensus document [11], (2) a requirement for sedation and paralysis for medical management, and (3) the presence of a pulmonary artery catheter. Patients were excluded from the study if they were hemodynamically unstable, defined as having a systolic blood pressure of less than 90 mmHg despite vasopressor support, or undergoing supraventricular arrhythmias. Patients with head injuries requiring intracranial pressure monitoring, with unstable spinal injuries, and with rib fractures were also excluded. Additionally, any patient judged to be at risk from routine turning as determined by the attending surgeon was also excluded.
Patients
All patients had previously been diagnosed with ARDS, were chemically paralyzed, and were sedated. Paralysis was monitored with routine train-of-four monitoring. ARDS was defined in accordance with the consensus definition of having a ratio of partial pressure of arterial oxygen to fractional inspired oxygen concentration (PaO2/FIO2) of less than 200, bilateral infiltrates on the anterior-posterior chest radiograph, normal cardiac filling pressures (wedge pressure less than 18 mmHg), and a causative factor. Chest radiographs were interpreted by the attending radiologist. Table 1 lists characteristics of the patients in the study. All patients were ventilated with pressure-control ventilation. Positive end-expiratory pressure (PEEP) was set to maintain oxygen saturation at more than 93% and the tidal volume was set between 8 and 10 ml/kg. Tidal volume was reduced to maintain peak airway pressures of less than 40 cmH2O. Respiratory rate was adjusted to maintain a pH of more than 7.30. Inspiratory to expiratory time ratio was less than 1:1. Inspiratory time was set to increase mean airway pressure, to allow a period of zero flow during inspiration, and to avoid intrinsic PEEP.
Table 1.
Characteristics of patients enrolled in the study
| Patient | Gender | Age | Diagnosis | Static Cl | Qs/Qt (%) | PEEP | FIO2 | DOV (h) |
| 1 | F | 33 | Multiple trauma, multiple long bone fractures - indirect ARDS | 34 | 28 | 10 | 0.50 | 18 |
| 2 | M | 26 | Liver laceration, ruptured spleen - indirect ARDS | 26 | 31 | 12 | 0.55 | 10 |
| 3 | M | 62 | Ruptured bladder, sepsis - indirect ARDS | 38 | 21 | 10 | 0.60 | 15 |
| 4 | M | 44 | Pancreatitis, sepsis | 31 | 37 | 15 | 0.50 | 20 |
| 5 | M | 59 | Aspiration pneumonia - direct ARDS | 37 | 24 | 10 | 0.60 | 9 |
| 6 | F | 67 | Intra-abdominal sepsis, perforated bowel - indirect ARDS | 25 | 33 | 15 | 0.65 | 13 |
| 7 | M | 41 | Gun shot wound to abdomen - indirect ARDS | 29 | 21 | 18 | 0.60 | 10 |
| 8 | M | 19 | Multiple trauma - indirect ARDS | 28 | 19 | 10 | 0.45 | 9 |
| 9 | F | 72 | Perforated gastric ulcer, sepsis - indirect ARDS | 35 | 24 | 12 | 0.50 | 18 |
| 10 | M | 66 | Perforated colon, sepsis - indirect ARDS | 33 | 35 | 15 | 0.60 | 16 |
| 11 | F | 57 | Aspiration pneumonia - direct ARDS | 33 | 21 | 10 | 0.60 | 14 |
| 12 | M | 63 | Aspiration pneumonia - direct ARDS | 38 | 23 | 10 | 0.55 | 6 |
| 13 | F | 30 | Multiple stab wounds - indirect ARDS | 29 | 27 | 14 | 0.5 | 15 |
| 14 | M | 70 | Liver resection - indirect ARDS | 25 | 30 | 16 | 0.5 | 5 |
| 15 | M | 38 | Mesenteric artery occlusion, ischemic bowel - indirect ARDS | 24 | 29 | 18 | 0.6 | 19 |
| 16 | M | 48 | Pancreatitis - indirect ARDS | 29 | 23 | 15 | 0.70 | 12 |
| 17 | F | 28 | Crushed pelvis - indirect ARDS | 27 | 20 | 12 | 0.50 | 20 |
| 18 | M | 60 | Perforated gastric ulcer, aspiration pneumonia - direct ARDS | 38 | 22 | 10 | 0.60 | 13 |
| 19 | F | 55 | Esophagectomy, pneumonia - indirect ARDS | 36 | 29 | 10 | 0.70 | 17 |
| N = 19 | 12 M, | 49 ± 17 | 31.3 ± | 26.1 ± | 12.7 ± | 0.57 ± | 13.6 ± | |
| 7 F | 4.8 | 5.3 | 2.9 | 0.07 | 4.5 |
DOV, duration of ventilation; Qs/Qt, venous admixture; FIO2, fractional inspired oxygen concentration.
Study design
Patients were randomized to receive four turning and secretion management regimens in random sequence for 6 h each over a period of 24 h. Sequence was determined by a random-number table, varying the assignment of management regimens equally. These regimens included (1) routine turning by the ICU staff every 2 h from the left lateral to the right lateral position; (2) routine turning by the ICU staff every 2 h from the left lateral to the right lateral position including a 15-min period of manual percussion and postural drainage (P&PD) by the respiratory therapists; (3) continuous lateral rotation (CLR) with a specialized bed (Effica; Hill-Rom, Batesville, Indiana, USA) that turned patients from left to right lateral position, pausing at each position for 2 min; and 4) CLR with a specialized bed (Effica) that turned patients from left to right lateral position, pausing at each position for 2 min, and a 15-min period of percussion provided by the pneumatic cushions of the bed every 2 h. P&PD was done 60-90 min into the 2-h turn regimen.
Measurements
Routine cardiorespiratory monitoring was accomplished in accordance with ICU protocol. Continuous monitoring of the electrocardiogram with lead II, systolic, diastolic, and mean arterial blood pressures from indwelling radial catheters, and pulse oximetry were accomplished. Systolic, diastolic, and mean pulmonary artery pressures and central venous pressure were also monitored continuously. These variables were recorded hourly from cardiovascular monitors (Sirecust; Siemens, Danvers, Massachusetts, USA).
All pressure monitoring systems were calibrated in accordance with the manufacturer's specifications and the zero reference was verified before data collection. Every 3 h, measurements of pulmonary capillary wedge pressure (PCWP) were made and cardiac output was determined from thermodilution curves with iced saline in triplicate. At the 3-h time point, arterial and pulmonary artery blood was drawn for measurements of blood gases, pH, and oxygen saturation. Samples were drawn, iced, and analyzed within 5 min by using standard blood gas (Corning, Medfield, Massachusetts, USA) and co-oximeters (OSM-3; Radiometer, Westlake, Ohio, USA). This time point was chosen to allow a 1-h period of rest after suctioning and P&PD. All measurements were made with the patient in the supine position to prevent positional effects on the results. All patients were ventilated with a Puritan-Bennett 7200ae (Puritan-Bennett, Carlsbad, California, USA). Airway pressures and tidal volume were recorded directly from the ventilator's digital display. All patients were ventilated by using pressure control ventilation. Pressure was limited to less than 40 cmH2O and tidal volume targets were 8 ml/kg. Intrinsic PEEP was measured with an expiratory pause of 2.0 s and displayed by the ventilator's intrinsic PEEP maneuver. Static pulmonary compliance was measured during the delivery of a volume-controlled, constant-flow breath by recording inspiratory plateau pressure after a 1.0-s pause, total PEEP and exhaled tidal volume. Static compliance was calculated as static compliance (ml/cmH2O)=tidal volume/plateau pressure - total PEEP.
Continuous measurements of oxygen consumption (VO2), CO2 production (VCO2), respiratory quotient (RQ), and resting energy expenditure (REE) were accomplished with an open-circuit indirect calorimeter with the use of the dilutional principle (DeltaTrac' Sensormedics, Yorba Linda, California, USA) [12,13]. VO2, VCO2, RQ, and REE were averaged on a minute-to-minute basis and saved to a personal computer for later analysis. Mixed expired CO2 concentration (PeCO2) was also measured and used along with the partial pressure of arterial CO2 (PaCO2) to determine the ratio of deadspace to tidal volume (Vd/Vt). Vd/Vt was calculated with the Bohr equation, Vd/Vt= PaCO2 - PeCO2/PaCO2.
Routine care
Patients continued to receive routine care including bathing, mouth care, suctioning, and measurement of hourly vital signs. Every effort was made to maintain continuous rotation during the study period. No patient had received continuous rotation before the start of the study. Additionally, routine procedures were accomplished more than 2 h before blood gas data were obtained. Suctioning was accomplished as needed in the judgement of the nursing and respiratory therapy staff. Indications for suctioning included rhonchi on auscultation, audible secretion noises, patient coughing, and the presence of a sawtooth pattern in the expiratory waveform in the absence of ventilator circuit condensate. A suctioning procedure was also accomplished following P&PD. Suctioning was done with a sterile, open-circuit technique with a single-use disposable suction catheter. Patients were pre-oxygenated before suctioning and manually ventilated with a self-inflating bag in between suction catheter passes. Normal saline was instilled at the discretion of the surgical ICU staff in an attempt to thin secretions. The volume of secretions aspirated were collected in a sputum trap and recorded. Suctioning was performed after each P&PD period or at the time that P&PD would have been accomplished.
All data were collected prospectively by the researchers (RDB and RSC), who were present throughout the 24-h study period. Changes in ventilator settings were limited to temporary increases in inspired oxygen concentrations to alleviate hypoxemia (pulse oximetry saturation less than 90%).
Statistical analysis
All data were collected and analyzed with commercially available data management and statistical software. All data are shown as means ± SD. Data were analyzed with analysis of variance for repeated measures and Tukey's test for post hoc analysis.
Results
All patients completed the 24-h trial period. There were no statistically significant differences in the measured cardiorespiratory variables (Table 2). There was a tendency for PaO2/FIO2 to increase (174 ± 31 versus 188 ± 36; P = 0.068) and Vd/Vt to decrease (0.62 ± 0.18 versus 0.59 ± 0.18; P = 0.19) during periods of CLR, but these differences did not achieve statistical significance. There were no changes in PaCO2 during the study (Fig. 1). Airway pressures were unchanged during the study period and cardiac output was unaffected. VO2 and VCO2 tended to be higher during the periods of P&PD than without, although this difference was similarly not statistically significant. Results for the cardiorespiratory measurements are shown in Table 2.
Table 2.
Mean values for cardiorespiratory variables during the four 6-h periods studied
| Manual turning + | Continuous rotation + | |||
| Cardiorespiratory variable | Manual turning | P&PD | Continuous rotation | P&PD |
| Mean VO2 (ml/min) | 299 ± 88 | 323 ± 114 | 288 ± 79 | 302 ± 97 |
| Mean VCO2 (ml/min) | 269 ± 71 | 294 ± 69 | 260 ± 73 | 272 ± 77 |
| Mean PIP (cmH2O) | 38 ± 9 | 40 ± 9 | 36 ± 10 | 38 ± 8 |
| Mean Pplat (cmH2O) | 34 ± 7 | 37 ± 6 | 33 ± 6 | 34 ± 6 |
| Mean Vt (ml) | 733 ± 104 | 710 ± 119 | 751 ± 96 | 745 ± 113 |
| Vd/Vt (%) | 0.62 ± 0.18 | 0.63 ± 0.23 | 0.59 ± 0.18 | 0.64 ± 0.19 |
| Cardiac output (litres/min) | 7.4 ± 2.3 | 7.8 ± 2.7 | 7.1 ± 2.2 | 7.4 ± 2.7 |
| Turns per 6 h | 2.5 ± 0.4 | 3.0 ± 0.2 | 41 ± 8* | 43 ± 20* |
Values are means ± SD of data recorded every hour for the study period, except Vd/Vt, which was every 3 h. PIP, peak inspiratory pressure; P&PD, percussion and postural drainage; Pplat, inspiratory plateau pressure; VO2, oxygen consumption; VCO2, CO2 production.
Figure 1.
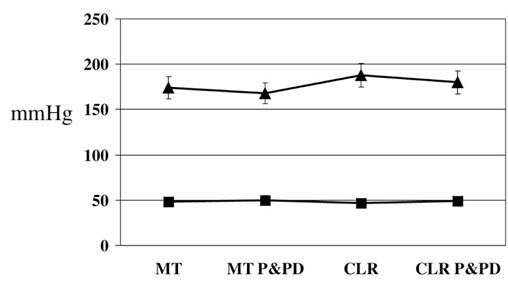
Changes in PaO2 and PaCO2 during the four study periods.
There were statistically significant increases in sputum volume during the periods of CLR (Table 3). The addition of P&PD did not increase sputum volume for the group as a whole. However, in the four patients producing more than 40 ml of sputum per day, P&PD increased sputum volume significantly (Table 3). The number of patient turns increased from one every 2 h to one every 10 min during CLR.
Table 3.
Effects of P&PD on sputum production, effects of percussion and postural drainage (P&PD) on oxygen consumption (VO2), and number of patient turns during the four 6-h study periods
| Manual turning + | Continuous rotation + | |||
| Variable | Manual turning | P&PD | Continuous rotation | P&PD |
| Sputum volume (ml) | 13 ± 7 | 15 ± 5 | 23 ± 9* | 25 ± 9* |
| Sputum volume, high production (ml) | 18 ± 8 | 27 ± 13† | 26 ± 14 | 30 ± 11‡ |
| Change in VO2 during P&PD (%) | NA | [+] 22 ± 8† | NA | [+] 7 ± 4 |
| Turns per 6 h | 2.5 ± 0.4 | 3.0 ± 0.2 | 41 ± 8 | 43 ± 10 |
Sputum volume is the total volume for each 6-h period; high production refers to patients with a sputum production of more than 40 ml/day. NA, not applicable. Change in VO2 is the percentage change from previous period without P&PD. *, P < 0.05 versus manual turning periods. †, P < 0.001 versus manual turning periods. ‡, P < 0.05 versus times without P&PD.
During P&PD, all patients showed a rise in VO2 and VCO2 associated with the procedure. In each case, the increase in VO2 and VCO2 during manual P&PD was greater than that during P&PD provided by the bed. In one case, P&PD with the bed was associated with multi-focal premature ventricular contractions and 'whip' artefact on the pulmonary artery pressure tracing. The intensity of the percussion was reduced and this problem was eliminated.
Discussion
Turning regimens are an essential part of the routine management of mechanically ventilated patients. Position changes are thought to reduce atelectasis, enhance fluid mobilization, prevent skin breakdown, improve oxygenation, and decrease the incidence of hospital-acquired pneumonia [4,5,6,7,8,9]. This study was designed to study the acute effects of CLR in comparison with manual turning, in paralyzed patients with ARDS. Our study was designed to identify the underlying physiological changes that might be related to the positive outcomes attributed to position changes. The major findings of the study are as follows: (1) blood gases are unaffected by a short period (6 h) of CLR, (2) secretion clearance is enhanced by CLR, and (3) P&PD results in an increase in sputum volume only in patients with excessive secretions. These findings are specific to this population of critically ill, paralyzed, surgical patients with ARDS. Extrapolation of these findings to other patient populations should be made with caution.
Few studies have attempted to elucidate the underlying physiological changes that might be responsible for positive outcomes seen with the use of CLR. Bein et al [10] recently compared the effects of a 20 min period of rotation to 20 min in the supine position in 10 ARDS patients. They found an increase in PaO2/FIO2 from 174 ± 82 to 217 ± 137 and decrease in intrapulmonary shunt from 23 ± 14% to 19.1 ± 15%. Using the multiple inert-gas elimination technique they attributed this improvement in gas exchange to a decrease in the amount of low ventilation/perfusion (V/Q) lung units and increase in normal V/Q units. In this study, measurements for the rotation periods were made with the patient in an extreme lateral position. This differs from our design. Bein et al also found that patients with more severe lung disease (Murrary Lung injury score more than 2.5) did not respond to rotational therapy, whereas those with less severe disease (less than 2.5) had significant changes in PaO2/FIO2. This can be explained by the changes in ARDS with time, as the lung evolves from a wet, heavy, atelectatic lung to a brittle fibrotic lung [12]. Early in ARDS, postural changes including CLR and prone positioning can be effective in altering the distribution of ventilation and blood flow [13,14,15]. In late ARDS, pathophysiological changes seem to render postural changes largely ineffective.
Nelson and Anderson [16] have shown previously that steep lateral positioning can result in either an improvement or a worsening of oxygenation. In their study of ten patients with apparent bilateral lung disease, steep positioning resulted in a decrease in PaO2 in four patients and an increase in PaO2 in six patients. These measurements were made in the extreme lateral position. They found that continuous rotation returned blood gas values to those in the supine position. These authors also suggested that extreme changes in lateral posture were associated with adverse effects on hemodynamics in comparison with continuous rotation. Bein et al [17] have also reported adverse hemodynamic effects in patients placed in the extreme lateral position. They suggested that the left lateral position resulted in a hyperdynamic state and that the right lateral position decreased right ventricular preload, resulting in hypotension. The measurement of plasma atrial natriuretic peptide indicated that these changes were due to the gravitational effects on the distensibility of the right heart. However, patients in this study were not solely patients with ARDS. We did not ascertain any significant hemodynamic effects during continuous rotation or manual turning. In many cases, pain associated with manual turning resulted in transient tachycardia and hypertension. Our findings did not reveal the magnitude of changes in gas exchange seen by others. However, PaO2/FIO2 increased in every patient after a period of rotation (188 ± 47 versus 174 ± 48, range 8-29) in our study. However, this difference was not statistically significant.
Position changes in unilateral lung disease have long been shown to be of value [18]. Placing the 'good lung' lower results in improved ventilation perfusion matching and an increase in oxygenation due to the gravitational effects on blood flow. More recently, the use of prone positioning has been shown to improve oxygenation in ARDS by improving distribution of ventilation through changes in regional pleural pressure gradients [14,15,19,20]. These two positioning techniques alter ventilation perfusion relationships through very different mechanisms. Prone positioning uses the shape and size of the dorsal lung compared with the ventral lung to improve the distribution of ventilation in bilateral lung disease. Extreme lateral positioning attempts to alter perfusion through the effects of gravity.
The process of routine turning is steeped in tradition, follows common-sense guidelines, and has some historical prescedent [21,22]. Lambert and colleagues determined that the immobilized postoperative patient was prone to atelectasis in the dependent lung. Chulay et al [22] found that turning the patient at 2-h intervals during the first 24 h after coronary artery bypass surgery decreased the incidence of fever and shortened ICU stay compared with patients remaining in the supine position. Routine turning also follows the normal pattern of sleep, where the average person changes posture every 12 min [23]. On the basis of this evidence, routine body position changes to prevent pulmonary complications have become a standard of care. Additionally, turning is important for decreasing skin breakdown and contributing to the mobilization of fluid.
We did find that the use of CLR significantly increased the number of times that the patients were turned each hour. During scheduled turning every 2 h by the staff, turns occurred only every 3 h. This finding is related in part to the study design, but is also related to the availability of staff. Turning patients can be difficult owing to the severity of illness, patient size, patient weight, and the presence of traction, indwelling lines, and ancillary equipment surrounding the bed. During the 2-h manual turning portion of the study, turning was accomplished less frequently owing to the workload of ICU staff. During continuous rotation, patients were turned from left to right six times per hour. Clearly, when used appropriately, a rotational bed facilitates patient turning and reduces nursing workload spent performing this task.
We also demonstrated improved secretion clearance in patients during CLR that were unrelated to P&PD. Compared with manual turning, continuous rotation seems to facilitate secretion clearance in paralyzed patients. This finding might be specific to paralyzed patients who are unable to cough. Changes in body position are an important part of postural drainage and this is most likely to be the mechanism through which secretion clearance is enhanced. Acutely, improved secretion clearance might be responsible for the reported decrease in pneumonia during prolonged use of CLR [5,6,7,8]. Interestingly, the addition of percussion to the postural drainage occurring during CLR failed to increase secretion clearance in our patient population. However, previous work has questioned the use of P&PD in patients without increased secretion production [24,25,26]. Four of our patients demonstrated high volumes of secretions (40 ml/day); in each of the four, P&PD increased secretion clearance. This finding is not wholly unexpected. Our results suggest that routine P&PD is unnecessary. However, patients with excessive secretions seem to benefit from a combination of continuous rotation and P&PD. Whether this increase in secretion clearance alters outcomes cannot be determined from our 24-h study.
The metabolic cost of P&PD had been previously described [27]. Horiuchi et al [28] have measured a 40% increase in VO2 during P&PD in postoperative surgical patients. This effect has been attributed to both a stress-like and an exercise-like response of the patient to P&PD. In this most recent investigation, these authors found that VO2 was increased both by manual turning into the lateral decubitus position and by the administration of percussion. When vecuronium was given before the procedure, these changes in VO2 were abated. The authors suggested that both patient muscle activity and increased sympathetic output contribute to the increase in VO2 seen during P&PD. Interestingly, our patients tolerated turning and percussion by the bed better than manual turning and percussion. The change in VO2 during P&PD provided by the bed was much lower than that seen during manual techniques. This might be related to the abrupt changes that occur with manual turning, and pain associated with manual hand clapping on the chest wall.
The study design and 24-h trial period impose significant limitations on the results. Because we attempted to determine physiological changes, a short study period was required. It might be that several days of CLR is required before the identification of beneficial effects. Our design cannot answer this question. All measurements were made by the same two investigators in an attempt to limit measurement errors. However, during a 24-h period, changes in lung mechanics as a consequence of disease progression/resolution might have occurred. We attempted to limit these confounding variables by randomizing the sequence of regimens. Variations in blood gases over time in a given patient have been reported and demonstrate significant variation based on timing [29]. We attempted to standardize the collection of data to coincident events, to prevent variability.
This investigation found that, whereas PaO2 improved slightly during periods of rotation, no significant increases in gas exchange were identified between manual turning every 2 h and CLR. There were no adverse hemodynamic effects of either turning procedure. Continuous rotation did increase secretion clearance compared with manual turning, but the addition of percussion did not further improve secretion removal. In patients with large secretion volumes, P&PD did increase secretion clearance. P&PD was better tolerated when delivered by the bed in comparison with manual turning, as judged by the change in VO2. The acute effects of CLR are undoubtedly different in other patient populations. The link between acute physiological changes and improved outcomes associated with CLR remain to be determined.
References
- Ray JF, III, Yost L, Moallem S, Sanoudos GM, Villamena P, Paredes RM, Clauss RH. Immobility, hypoxemia, and pulmonary arteriovenous shunting. Arch Surg. 1974;109:537–541. doi: 10.1001/archsurg.1974.01360040055014. [DOI] [PubMed] [Google Scholar]
- Hess D, Agarwal NN, Myers CL. Positioning, lung function, and kinetic bed therapy. Respir Care. 1992;37:181–197. [Google Scholar]
- Clauss RH, Scalabrini BY, Ray JF, Reed GE. Effects of changing body position upon improved ventilation perfusion relationships. Circulation. 1968;37:214–217. doi: 10.1161/01.cir.37.4s2.ii-214. [DOI] [PubMed] [Google Scholar]
- Raoof S, Chowdrey N, Raoof S, Feuerman M, King A, Sriraman R, Khan FA. Effect of combined kinetic therapy and percussion therapy on the resolution of atelectasis in critically ill patients. Chest. 1999;115:1658–1666. doi: 10.1378/chest.115.6.1658. [DOI] [PubMed] [Google Scholar]
- Fink M, Helsmoortel CM, Stein KL, Lee PC, Cohn SM. The efficacy of an oscillating bed in the prevention of lower respiratory tract infection in critically ill victims of blunt trauma. Chest. 1990;97:132–137. doi: 10.1378/chest.97.1.132. [DOI] [PubMed] [Google Scholar]
- Summer WR, Curry P, Haponik EF, Nelson S, Elston R. Continuous mechanical turning of ICU patients shortens length of stay in some diagnostic-related groups. J Crit Care. 1989;4:45–53. [Google Scholar]
- Gentilello L, Thompson DA, Tonnesen AS, Hernandez D, Kapadia AS, Allen SJ, Houtchens BA, Miner ME. Effect of rotating bed on the incidence of pulmonary complications in critically ill patients. Crit Care Med. 1988;16:783–786. doi: 10.1097/00003246-198808000-00010. [DOI] [PubMed] [Google Scholar]
- Clemmer TP, Green S, Ziegler B, Wallace CJ, Menlove R, Orme JF, Jr, Thomas F, Tocino I, Crapo RO. Effectiveness of kinetic treatment table for preventing and treating pulmonary complications in severely head injured patients. Crit Care Med. 1990;18:614–617. doi: 10.1097/00003246-199006000-00007. [DOI] [PubMed] [Google Scholar]
- Takiguchi SA, Myers SA, Yu M, Levy MM, McNamara JJ. Clinical and financial outcomes of lateral low air-loss therapy in patients in the intensive care unit. Heart Lung. 1995;24:315–320. doi: 10.1016/s0147-9563(05)80076-7. [DOI] [PubMed] [Google Scholar]
- Bein T, Reber A, Metz C, Jauch KW, Hedenstierna G. Acute effects of continuous rotational therapy on ventialtion-perfusion inequality in lung injury. Intens Care Med. 1998;24:132–137. doi: 10.1007/s001340050534. [DOI] [PubMed] [Google Scholar]
- Bernard GR, Artigas A, Bingham KL. Definitions, mechanisms, relevant outcomes and clinical trial coordination. Am J Resp Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- Gattinoni L, Bombino M, Pelosi P, Lissoni A, Presenti A, Fumagalli R, Tagliabue M. Lung structure and function in different stages of severe adult respiratory distress syndrome. J Am Med Ass. 1994;271:1772–1779. [PubMed] [Google Scholar]
- Lamm WJE, Graham MM, Albert RK. Mechanism by which prone position improves oxygenation in acute lung injury. Am J Resp Crit Care Med. 1994;10:184–193. doi: 10.1164/ajrccm.150.1.8025748. [DOI] [PubMed] [Google Scholar]
- Langer M, Mascheroni D, Marcolin R, Gattinoni L. The prone position in ARDS patients. Chest. 1988;94:103–107. doi: 10.1378/chest.94.1.103. [DOI] [PubMed] [Google Scholar]
- Pappert D, Rossaint R, Slama K, Gruning T, Falke KJ. Influence of positioning on ventialtion perfusion relationships in severe adult respiratory distress syndrome. Chest. 1994;106:1511–1516. doi: 10.1378/chest.106.5.1511. [DOI] [PubMed] [Google Scholar]
- Nelson LD, Anderson HB. Physiologic effects of steep positioning in the surgical intensive care unit. Arch Surg. 1989;124:352–355. doi: 10.1001/archsurg.1989.01410030102017. [DOI] [PubMed] [Google Scholar]
- Bein T, Metz C, Keyl C, Pfeifer M, Taeger K. Effects of extreme lateral posture on hemodynamics and plasma atrial natriuretic peptide levels in critically ill patients. Intens Care Med. 1996;22:651–655. doi: 10.1007/BF01709741. [DOI] [PubMed] [Google Scholar]
- Ibanez J, Raurich R, Abizanda R, Claramonte P, Ibanez P, Bergada J. The effect of lateral positions on gas exchange in patients with unilateral lung disease during mechanical ventilation. Intens Care Med. 1981;7:231–234. doi: 10.1007/BF01702625. [DOI] [PubMed] [Google Scholar]
- Sinclair SE, Albert RK. Altering ventilation-perfusion relationships in ventilated patients with acute lung injury. Intens Care Med. 1997;23:942–950. doi: 10.1007/s001340050436. [DOI] [PubMed] [Google Scholar]
- Chattey G, Sab JM, Dubois JM, Sirodot M, Gaussorgues P, Robert D. Prone position in mechanically ventilated patients with severe acute respiratory failure. Am J Resp Crit Care Med. 1997;155:473–478. doi: 10.1164/ajrccm.155.2.9032181. [DOI] [PubMed] [Google Scholar]
- Lambert RL, Wilauer G, Dasch FW. The postoperative status of the dependent lung. J Thorac Surg. 1955;30:713–718. [PubMed] [Google Scholar]
- Chulay M, Brown J, Summer W. Effect of postoperative immobilization after coronary artery bypass surgery. Crit Care Med. 1982;10:176–179. doi: 10.1097/00003246-198203000-00007. [DOI] [PubMed] [Google Scholar]
- Aserinsky E, Kleitman N. Regular periods of eye motility and concomitant phenomenon during sleep. Science. 1953;118:273–279. doi: 10.1126/science.118.3062.273. [DOI] [PubMed] [Google Scholar]
- Johnson D, Kelm C, Thomson D, Burbridge B, Mayers I. The effect of physical therapy on respiratory complications following cardiac valve surgery. Chest. 1996;109:638–644. doi: 10.1378/chest.109.3.638. [DOI] [PubMed] [Google Scholar]
- Kirilloff LH, Owens GR, Rogers RM, Mazzocco MC. Does chest physical therapy work? Chest. 1985;88:436–444. doi: 10.1378/chest.88.3.436. [DOI] [PubMed] [Google Scholar]
- Connors AE, Hammon WE, Martin RJ, Rogers RM. Chest physical therapy: the immediate effect on oxygenation in acutely ill patients. Chest. 1980;78:559–584. doi: 10.1378/chest.78.4.559. [DOI] [PubMed] [Google Scholar]
- Weissman C, Kemper MS, Elwyn DH, Askanazi J, Hyman AI, Kinney JM. The effect of routine ventilator interactions on metabolic rate. Chest. 1984;86:815–818. doi: 10.1378/chest.86.6.815. [DOI] [PubMed] [Google Scholar]
- Horiuchi K, Jordan D, Cohen D, Kemper MC, Weissman C. Insights into the increased oxygen demand during chest physiotherapy. Crit Care Med. 1997;25:1347–1351. doi: 10.1097/00003246-199708000-00022. [DOI] [PubMed] [Google Scholar]
- Thorson SH, Marini JJ, Pierson DJ, Hudson LD. Variability of arterial blood gas values in stable patients in the ICU. Chest. 1983;84:14–18. doi: 10.1378/chest.84.1.14. [DOI] [PubMed] [Google Scholar]


