Abstract
The current biomedical and psychosocial frameworks that form the conceptual basis of medicine today are insufficient to address the needs of the medically complex and environmentally challenged populations of patients often cared for by physical medicine and rehabilitation specialists. The expanded biopsycho-ecological model of health, illness, injury, and disability operating through mechanisms of Health Environmental Integration (HEI) encourages a more complete understanding of illness, injury, activity limitation, and participation restriction as arising at the interface between the person and the environment. HEI recognizes complex interacting multilevel functional hierarchies beginning at the cellular level and ending at the individual’s experience of the environment. Although the foci of illness and injury are within the body and mind, the physical and social environments contain elements that can cause or exacerbate disease and barriers that interact in ways that lead to injuries and disabilities. Furthermore, these environments hold the elements from which treating agents, facilitators, and social supports must be fashioned. The highly integrative biopsycho-ecological framework provides an expanded basis for understanding the objective causes and subjective meanings of disabilities. Disabilities are reduced through HEI by seeking to maximally integrate the body and mind (the self) with both the surrounding physical environment and other people in society. HEI offers mechanisms for interdisciplinary research, an expanded framework for education and empowerment, and a blueprint for optimizing day-to-day clinical care at both the individual patient and treatment population levels in the ever-changing scientific, political, and policy environments.
INTRODUCTION
As far back as 1747, James Linel carried out an experiment proving that citrus cures scurvy. Yet he rejected lack of fruits and vegetables as the causal mechanism, embracing instead his alternative theory of humidity as the primary cause [1]. Lack of available statistical methods in the 18th century and limited knowledge about establishing causality led, at that time, to what appears to be a clear misinterpretation of his own findings. Enlightened by scientific methods today, we can recognize this type II error. It was not until the emergence of Koch’s postulates, which were established in the late 19th century and commonly perceived as the origin of modern Western biomedicine and experimentation, that methods attributing the causality of illness were established [2].
Western medicine and public health measures during the 20th century were fueled by concepts of pathophysiology, with specific biochemical deviations informing initiatives in prevention, diagnosis, and treatment. The body is seen as a physical structure in which illnesses are explained by single rational predictable causes mediated by molecular mechanisms [3,4]. Rapid advances in medical technology driven by these biomedical concepts contributed to the reduction of highly fatal early-life diseases. In the 20th century, average life expectancy increased 25 years [5], leaving individuals with increased exposure to the cumulative effects of chronic illness. Recognizing that the presence of biochemical defects defines necessary but insufficient conditions for the expression of many diseases, George Engel, an internist and psychiatrist, proposed the biopsychosocial model as a new organizing principle for medicine [6]. In 1977, Engel wrote,
I contend that all medicine is in crises and further, that medicine’s crises derive from the same basic fault as psychiatry’s, namely, adherence to a model of disease no longer adequate for the scientific tasks and social responsibilities of either medicine or psychiatry. [6, p. 129]
The biopsychosocial paradigm accounts for interactions among biological, psychological, social, and cultural factors. Biopsychosocial principles informed clinical research in the 1980s and 1990s, as evidenced by increased federal funding and a huge body of published research on the relationships between stress, depression, immune competence, neuroendocrine function, cardiovascular and cancer risks, and disease incidence. This research led to important advances in understanding how stressful events modify personal vulnerability and the expression of illness [7] and how psychological well-being tends to protect against illness [8]. Now, more than 30 years after the introduction of Engel’s transformative ideas [9], medicine is yet again in a crisis for largely the same reason; namely, adherence to historical models of disease that are no longer adequate for the scientific tasks and social responsibilities of medicine.
EVOLUTION OF THE BIOPSYCHO-ECOLOGICAL MODEL
The biopsycho-ecological model, inspired by our research on human functioning, evolved over 2 decades. Early attempts to express the person-machine-environment interface associated with assistive technology (AT) led to the definition of 4 spheres of self-fulfillment. The mind and body spheres intrinsic to the person were seen as fundamental to impairment. The society and the physical world spheres extrinsic to the person were seen as interacting with impairments to cause disability. AT (eg, in the form of mechanical devices) operates at the interface between the intrinsic and extrinsic spheres. Effective AT enhances the person’s potential access to and interaction with society and the physical world [10]. Next, theories of Health Environmental Integration (HEI) were proposed to describe the ecological mechanisms through which the 4 spheres interact [11]. HEI adopts functional systems theory [12,13], recognizing that neither the person nor his or her health conditions can be fully understood without viewing the environment as part of a dynamic system of which all (ie, people, health conditions, and the environment) are integral parts. Health and illness occur within ecologies where small perturbations at any level can have large effects on overall person-level functioning and experienced quality of life.
The biopsycho-ecological model was tested empirically through cross-sectional analyses of more than 12,000 adults with basic physical limitations such as difficulties standing or reaching who were living in the community in the United States. After controlling for physical limitations and other characteristics, the odds of having activities of daily living (ADL) limitations were 3.7 times greater in persons who perceived that they had unmet needs for accessibility features in their homes than in those who did not perceive such needs [14,15]. The biopsycho-ecological model formed the foundation for functional independence staging and recovery preference exploration (RPE) [16]. Functional independence staging defines hierarchical thresholds of Functional Independence Measure (FIM) [17] functioning that stratify populations according to measured severity and types of disability [18,19], whereas RPE, a thought experiment, addresses the quality-of-life implications of disability [16].
The Oxford Dictionary of Public Health [20] defines theory as “a belief system based on observation and supposition, …., and experiments, including thought experiments.” All theories are subject to tests of validity and change. When theories change in ways that stimulate innovation, a field undergoes a paradigm shift. Verville and Thomas [21] recently suggested that the American Academy of Physical Medicine and Rehabilitation serve a leadership role in quality of care research addressing functioning. In addition, Kristi Kirschner, in her recent editorial on health care reform, suggested that rehabilitation medicine can lead in promulgating the biopsycho-ecological model of medicine [22]. In response, this article presents theories underlying the biopsycho-ecological model, illustrating its evolution and foundation for our research on human functioning during the past several decades [10,14,15,19,23]. Potential applications to clinical practice and research in physical medicine and rehabilitation (PM&R) are highlighted.
THE BIOPSYCHO-ECOLOGICAL MODEL
The biopsycho-ecological model is intended to be crosscutting and relevant to all health professions, synthesizing concepts from physiatry, medicine, psychiatry, geriatrics, and other medical fields, as well as physical therapy, occupational therapy, nursing, psychology, gerontology, neurobiology, rehabilitation sciences, phenomenology, dynamic systems, medical models of disability, social models of disability, empowerment, and advocacy [16,24–48]. Here, we focus primarily on applications in PM&R.
Although biopsycho-ecological principles can be illustrated by any number of disability frameworks [19], the International Classification of Functioning Disability and Health (ICF) terminology was selected because of its worldwide dissemination and extensive lists of environmental barriers and facilitators [49]. According to the ICF, functioning is “an umbrella term encompassing all body functions, activities and participation” and disability is an “umbrella term for impairments, activity limitation and participation restrictions” [49, p. 3]. These terms are defined in Table 1.
Table 1.
The hierarchies of functioning: the medical model, the social model, and the ICF taxonomy
| Levels* | Medical Model Terminology, Examples, and Concepts |
Social Model Terminology and Concepts |
ICF Terminology† |
|---|---|---|---|
| Level 1 (molecular or cellular) | Genetic predisposition, pathology, cellular injury, allostatic load, subclinical cellular dysregulation | NA | NA |
| Level 2 (body tissue) | Diagnosis of illness or injury (mental/physical, morbidity) | NA | “In the context of health” |
| Level 3 (organ or system) | Physical impairment, functional limitation, reduced reserve, cognitive impairment, organ or system-level dysregulation | Aspects of a person’s mind or body that do not function normally (including lack of motivation, initiative, engagement) | Body functions are the “physiological functions of body systems, including psychological functions” |
| Body structures are “anatomical parts of the body such as organs, limbs and their components” | |||
| Impairments are “problems in body function or structure such as significant deviation or loss” | |||
| Level 4 (whole organism or individual person) | Frailty at the organism level, disability, reduced resiliency or energy, inability to perform ADLs/IADLs at the organism level | Disability as a disadvantage | Activity is the “execution of a task or action by an individual” |
| Activity limitations are “difficulties an individual may have in executing activities” | |||
| Participation is “involvement in a life situation” | |||
| Participation restrictions are “problems an individual may experience in involvement in life situations” | |||
| Level 5 (environmental experience) | Pathogens and hazards in the environment | Barriers, loss, or limitation of opportunities resulting from direct or indirect discrimination | Social and physical environmental barriers and facilitators |
ADL = activities of daily living; IADL = instrumental activities of daily living; ICF = International Classification of Functioning Disability and Health; NA = not applicable.
Functional level 1 applies basic science in efforts to understand and improve medical and surgical management of levels 2 and 3. Levels 3 and 4 are the primary focus of physical medicine and rehabilitation, and level 5 needs development and exploration.
From World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva, Switzerland: World Health Organization; 2001 (pages 3 and 10).
The biopsycho-ecological model expands on the biomedical and the biopsychosocial models. First, it adds the physical environment as a fourth interacting element to the dynamic interactions of the body, mind, and sociocultural variables presented by the biopsychosocial model. Second, it postulates that hierarchies of the cellular, body tissue, organ or organ system, person, and environmental elements interact to drive physiological processes and determine personal life worlds reflecting the micro and macro levels of functioning, respectively. Third, it distinguishes between population and person levels of analyses. Fourth, it recognizes objective standardized measurement of activity limitation as distinct from its subjective qualitative meaning [50].
Physical Environment as a Fourth Interacting Element
The biopsycho-ecological model, as with earlier models [10,33,49,51], recognizes functioning as an interaction between impairment (arising from health conditions) and the environment. Examples of linkages between the environment and health abound [32,52–60]. Evidence linking the built environment and functioning also is growing [14,61,62]. Elderly persons with physical limitations who were living in communities and were rated as having high mobility barriers [61] were twice as likely to experience limitations in their daily activities. Studies of the social capital within neighborhoods identify linkages between the social and physical worlds within which people live. People who live in walkable, mixed-use neighborhoods where they can easily get to markets (in contrast to car-oriented suburbs) were more likely to know their neighbors, to trust others, and to be socially engaged [57]. Finally, lack of accessibility features in the home was associated with ADL limitations among persons with physical limitations [14].
Levels of Functioning (Theoretical Mechanism)
HEI expresses enablement and disablement as occurring through dynamic interactions between a person’s intrinsic status of body and mind and the barriers and facilitators in his or her surrounding physical world and society. There are 3 fundamental ecologies: external, internal, and global. External ecology is measurable person-environment interactions and functioning that defines an external life space. Internal ecology encompasses the subjective inner-life world, which is the personal meaning of that functioning conceptualized as internal life space. Global ecology is the functional interaction of humankind with the biosphere.
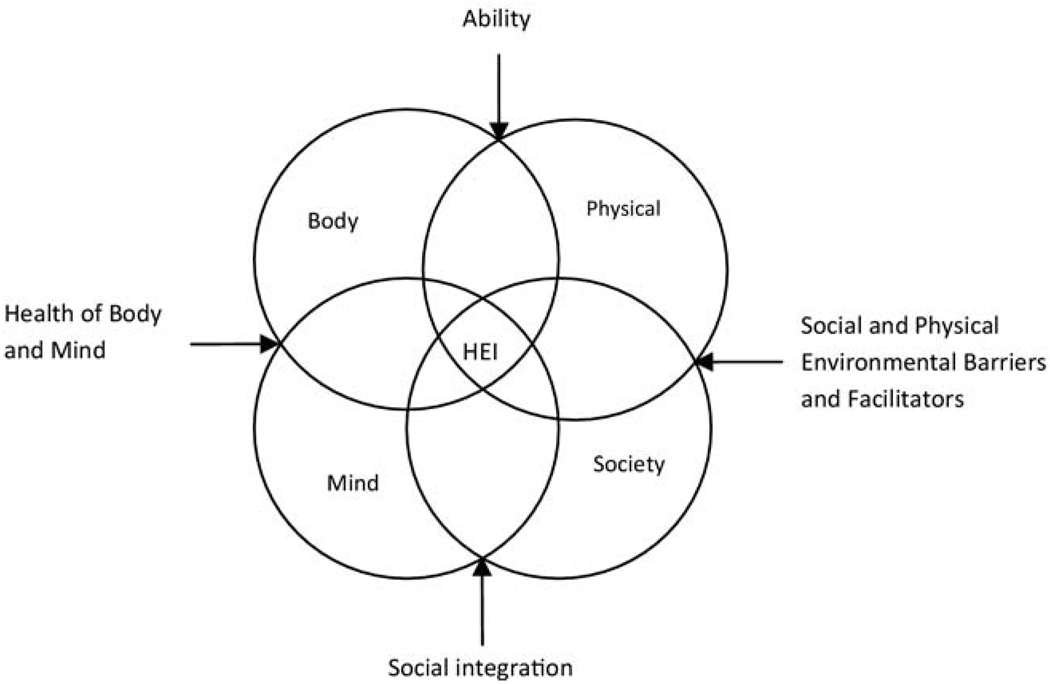
At the person level, “Health Environment Integration (HEI) determines how a person is able to function and integrate him or herself within particular physical and social environments [63].” Impairments interacting with physical and social barriers and facilitators delineate potential for functioning in external life space. Life space shrinks as access to the physical and social environment declines (ie, disability increases). Life space expands as the individual experiences greater access to the physical environment and more connections with others (ie, disability decreases). In contrast to the external ecology, internal ecology has no direct connections to the material. Subjective quality of life [64] and meaningfulness may represent the closest measurable concepts. External and internal life space in combination determines the theoretical HEI quantity, which includes both measurable and less-measurable aspects of human experience and participation as represented by the interacting area shared by all 4 spheres (Figure 1).
Figure 1.
The biopsycho-ecological model of health environmental integration. The overlap between the body and mind constitutes the biomedical model and the overlap of the body, mind, and society represents the biopsychosocial models. The intersection of all 4 spheres of the body, mind, society, and physical environment represents the biopsycho-ecological model. Activity and participation, which is constrained by interactions between the individual’s intrinsic health states and the external life world, occurs at the 4-way intersection. This area of reciprocal interactions encompasses objective activity limitation (type and severity as measurable constructs) and its subjective implications (meaning). Presumed determinants of ability and distinct causes of disability contribute to the ecology of human experience and define available life space as indicated by arrows. Modified, with permission, from reference [63].
HEI reduction or expansion occurs in response to the interactions among and within 5 hierarchical functional systems: molecules, cells, organs, whole persons, and environments environments (Figure 1). The systems selectively bring in elements from other levels [13] through processes of “homeostatic integration between the organism and the environment.” These actions define response mechanisms to illness across maximally objective dimensions essential to the advancement of biomedical sciences [65,66] and also those more abstract expressions and personal reactions to disease that currently lack absolute linkage to biology.
As observed by Descartes in the 17th century, the body is recognized as material and formed from measurable elements [67]. The mind is immaterial, referring to personal psychological reactions, feelings of stigma or empowerment, spirituality, and the shaping of self-concept through meanings. Although the mind and body are conceptually distinct, they are also functionally integrated, as in the biopsychosocial model. Psychological states influence the expression of somatic illness [68]. Somatic conditions affect psychological states. Also, the internal dynamics of cognitive and affective functioning operate as complex systems within the environment [69]. Consequently, measurable imbalances between activating and inhibiting neural groups occur in the body sphere (brain) that appear to explain affect [70]. Recent evidence suggests that even tasks such as decision making can be mapped to specific brain areas [71]. Yet the quality of daily lived experience—of being present in one’s mind, experiencing love, seeking recovery and restoration of emotional homeostasis after loss, and the ongoing processes of building a personally meaningful life— can never be fully explained. The mind, as opposed to the brain, represents the nonmeasurable immaterial experiences of being human that seem to remain beyond the reach of inferential logic or modern scientific inquiry.
Hierarchies within the human organism are built on principles of multiparametric interactions [13]. Molecules, cells, organs, and whole persons operate as complex nonlinear systems constantly exchanging matter with the environment at all levels. Health and illness reflect lower level interactions among these complex systems. Functional status at a higher level constantly evolves as the individual moves through and integrates with the environment. A positive state of HEI is realized when optimal health and productivity is achieved in harmony with nature, which both sustains the individual (or population) and the local environment (or biosphere).
Concepts of disability can be expressed broadly across medical-oriented and social disability– oriented models at various levels of the hierarchy. Medically and socially oriented concepts map into ICF terminology, which recognizes historic clashes between the orientations but also the importance of integrating them so as to achieve a more coherent view of health from biological and social perspectives (Table 1) [49]. Medical sciences, including PM&R, are informed by level 1. Practice tends to intervene mostly at the middle of the hierarchy (at levels 2, 3, and 4). A full understanding of disability and its optimal management requires level 5, bringing in built and natural environments, autonomy, empowerment, human rights, and broader issues of ecology. The 5 levels of functioning are as follows:
Level 1
Basic sciences begin at the largely genetically determined microscopic and mechanistic level of molecules. Biomarkers expressing various types of pathology are applied diagnostically, and mechanisms of pharmaceutical agents are determined. There are basic science questions fundamental to PM&R. The simple motion of kicking, for example, occurs through multiple complex dynamic control mechanisms between the brain and body that need to be activated in perfect sequence and timing across multiple joints [72]. Functional tasks depend on the coordination of many such simple motions.
Level 2
Level 2 consists of illness and injury (health conditions) resulting from pathology.
Level 3
Level 3 consists of organ-level dysfunction of the body resulting from health conditions. Organ impairments are the primary determinant of disability according to the biomedical model. Impairments cause symptoms including motor, sensory (eg, vision and hearing loss), pain, cognitive, or behavioral change, energy reductions, or other manifestations. Impairments can (but do not always), limit activity or restrict participation. Prosthetics in PM&R compensate for organ loss. For example, brain-operated neuroprostheses can aid paralyzed individuals through brain-robotic interfaces [73]. The mind, which is distinct from the brain (a part of the body), by its nature relates to the nonmeasurable and difficult-to-explain aspects of the human experience. The internal life world of the mind creates personal landscapes of thoughts and meanings. Not directly accessible to the outsider, the mind constantly reacts to perceived status of self relative to body states and environmental experiences.
Level 4
Activity and participation represent the level to which most occupational and physical therapy interventions are targeted. Activity limitations and participation restrictions represent common pathways caused by diverse types of sensory, cognitive, or motor impairments. Activities within traditional measures, for example, the FIM [17], can be grouped into domains whose accomplishment depends on distinct anatomic areas or organ systems [74]. Within such domains, person-level functioning tends to follow hierarchies driven by the underlying order through which people tend to lose and recover abilities [75]. In motor as well as in neurodegenerative disorders, loss of function tends to occur in the reverse order in which it is acquired during neonatal development [75], a phenomenon described by the term “retrogenesis” [76].
Observed functional hierarchies led to several approaches to staging activity limitation by applying profile thresholds [18,77] and Item Response Theory (IRT), respectively [78]. The lowest stages in any dimension begin with the acquisition of tasks that depend on basic motor, sensory, and cognitive integration. Within the ADL dimension, for example, eating is the most basic stage. Recovery of more complex culturally learned activities, such as bathing, does not occur until higher stages. Environmental influences increase with complexity of activities. The ability to bathe, more than the ability to eat, depends on balances between barriers and facilitators such as the presence or absence of grab bars or the size of the bathroom. Whether an architectural feature becomes a barrier depends on impairment.
Level 5
Environment reflects a person’s living space in society and the physical world. According to the social model of disability, the problems faced by individuals are not solely related to the person [79]. Disadvantages associated with disability are seen as largely socially imposed. The sociological sphere includes socioeconomic resources, significant others (eg, family, friends, peer groups, and cultural groups), health professionals and larger social institutions (such as the health care system), and society at large. Culture, social attitudes, and relationships help shape self-concept and the ways people participate and experience illness and disability. Abundant evidence also suggests the importance of psychosocial factors in the expression of illness [80–82]. Intersections among the 3 spheres—the body, mind, and society—represent the biopsychosocial model, which is widely accepted as the most heuristic approach to understanding illness and disability today [49].
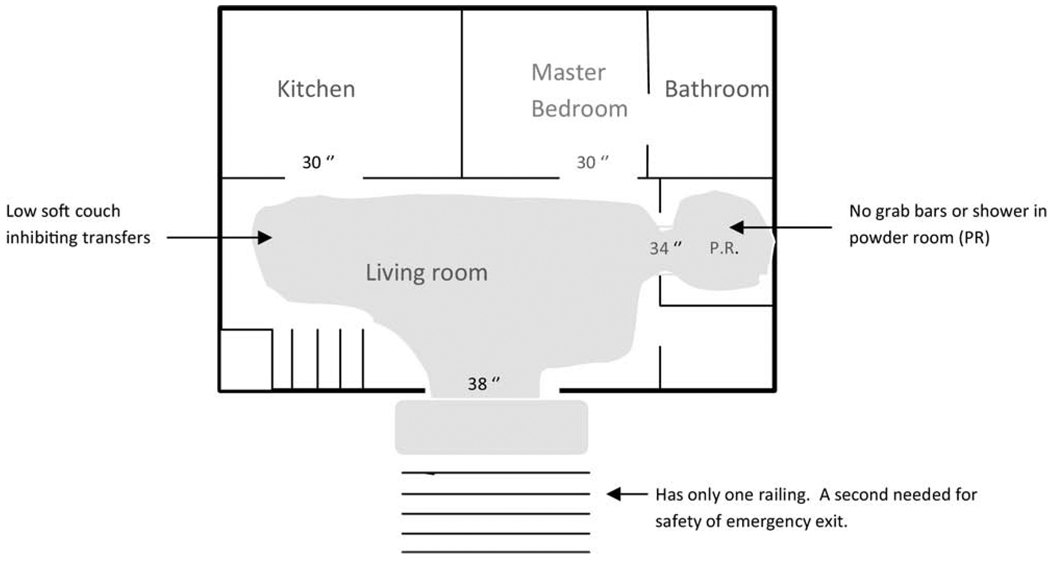
The fourth physical environment sphere completes the biopsycho-ecological model. There are partial hierarchies of matter, objects (natural and man-made), vistas, climatic conditions, the biosphere, and beyond. Interactions among biological, psychological, sociocultural, and environmental elements determine physical and mental functioning, and by delineating the particular conceptual spaces, a person is able to access and experience life over time. External life space expresses the external life world of HEI, a theoretical quantity akin to activity space [51]. Physical life space is measurable and recordable in diary format [83] or diagrammed for particular locations, such as a patient’s home (Figure 2). A life space diagram is an architectural sketch indicating barriers and facilitators. The space and the fixtures the person can use are shaded. Diagrams over time can show the effects of barrier removal, the addition of facilitators or assistive technology, or the progression of impairment. Social life space is the interaction and the integration of self within a personally meaningful and supportive social network. Social stressors, stigma, and cultural stereotypes restrict social life space. Physical and social life spaces define the ecology of personal experience.
Figure 2.
A physical life space sketch of the home of the patient in case 2 as might be drawn by an occupational therapist or other physical rehabilitation team member after obtaining simple measurements and descriptions from family members. The shaded area quantifies the space to which the patient currently has access. The diagram could be used to conceptualize the essential environmental modifications, adaptive equipment, or assistive technology that would be necessary to increase this patient’s physical life space within her home.
Population Versus Person Level Analyses
Evidence-based medicine focuses on standardization and the reduction of questions into cleanly testable problems. It gains its power by averaging covariates and outcomes across large populations. Many questions of importance to PM&R need to be addressed with population-level methods, such as randomized trials or observational studies. The future of PM&R depends on establishing evidence of clinical effectiveness through such methods. Theories of HEI offer theoretical mechanisms for addressing how person–environment interactions drive population recovery. In contrast, clinical practice requires appreciation of individuals. If persons are to live successfully in the community after hospitalization for a disabling illness, projections of their eventual functionality must occur within the contexts of their home architecture and available social supports. Providing meaningful consultation and developing an individualized plan of care for those who receive care in an inpatient rehabilitation facility will be particularly challenging for people who will be living alone [42].
Standardized Versus Subjective Measures of Activity Limitation
The full specification of activity limitation must include severity, the types of tasks that are limited, and meaning. IRT-based measures, stages, grades, and summed scales have all been proposed as alternative expressions of instruments that apply severity, such as the FIM [17,18,77,78]. Research is needed to optimize applications. Summed scales are easy to calculate and understand, but the activity limitations producing the score are obscured in the scoring [74]. IRT-based measures incorporate concepts of item difficulty and through item banking can expand the breadth of measurement by reducing floor and ceiling effects [84]. As with summed scores, the particular activity limitations producing the value are obscured, although an underlying hierarchy is inferred.
Severity is easily measured for single activities. Clearly, inability to walk is a more severe limitation than the need for minimal assistance to walk. With comparisons across activities, it is difficult to discuss severity. Who is to say whether the need for minimal assistance to walk represents a disability of equal severity to the need for minimal assistance to manage bladder functions? And when a person has different levels of disability across multiple activities (eg, requires maximal assistance to walk but only minimal assistance with dressing), how should we summarize the overall severity of disability?
Stages and grades address these problems by defining homogeneous groups of patients with similar types and severities of deficit within domains of related activities by explicitly defining achievement thresholds [77,78]. After a stage is reached, by definition, a person is functioning at or above a specified level for each component activity. Empirically derived stages within a domain reflect an ontology beginning with activities requiring the least and ending with activities requiring the most complex motor, sensory, and cognitive integration. Strong agreement between stages and IRT item difficulty calibrations independently supports concepts of an underlying biologically and sociologically based hierarchy of function [18,85].
People have varied profiles of disabilities, according to the performance levels that we can measure and the values and meanings that we are ill-equipped to measure. Disability can be analyzed by addressing the patient’s status across and between each HEI sphere and thinking about how that status might influence self-concept given the patient’s sociocultural and physical life space [14,86]. The sphere intersections show points of disability production (Figure 1). Overlap of the mind and body expresses impairment or health. Overlap of the physical world and society signifies environmental barriers and facilitators. Overlap of all 4 spheres indicates activity and participation. In theory, any activity limitation or participation restriction will have at least small contributions from each sphere. The resulting integration of body-mind-society-physical world contributes the substrate from which the personal landscape of thoughts and meanings emerge. Although it is not directly accessible to clinician “outsiders,” inductive reasoning in contrast to typical logic-based deductive reasoning is necessary to glimpse the internal life worlds of people with disabilities.
PM&R professionals are trained primarily in deductive rather than inductive reasoning. Yet if it is to be effective, successful rehabilitation, more than any other intervention, must be patient-centered, and empower the patient so as to uncover his or her internal ecology of meanings [47]. After catastrophic illnesses and injuries, patients forfeit life control to health care professionals. Rehabilitation involves patients taking back control and reorganizing their lives. A first step is to understand the idiosyncratic meaning of loss. The need to uncover ecological meanings led to development of the RPE [87], which is founded on principles of phenomenology [37].
RPE is an evolving, clinician-guided computer game intended to focus on the meaning of functional deficits. The player (ie, the patient, a family member, a clinician, or another person) is asked to imagine total dependency in many activities and then to imagine his or her patterns of recovery [23]. The procedure [87] deepens the player’s understanding of disability and the clinician’s understanding of the player’s internal life world. Studies with RPE indicate that patients undergoing inpatient rehabilitation tend to desire recovery pathways that are different from those desired by rehabilitation professionals [23,88–90]. Through enhanced insight and communication, results may help reduce conflicts around goal setting and discharge planning [91].
APPLYING BIOPSYCHO-ECOLOGICAL PRINCIPLES TO PM&R PRACTICE
Theory informs practice. HEI theories encourage clinicians to recognize interactions among the body (health and impairment), the mind (subjective reactions), society (available supports and stressors), and the physical environment (barriers and facilitators). HEI can improve clinical decision making and enhance meaningful communication by recognizing the rich contexts that define patients’ lives. Assessment and care organization occurs according to the 4 spheres and their intersections.
The following hypothetical cases derived from the authors’ clinical practices illustrate adverse outcomes related to HEI failure because of inadequate environmental assessment.
A 70-year-old man who previously played professional ice hockey and, as a result, had severely arthritic shoulders is referred to a physiatrist after being placed in a cast for a noncomplicated fracture of his left foot. Because he has a single uncomplicated fracture, he is not believed to be a candidate for inpatient rehabilitation. The surgeon discharges him to his 2-story home with instructions to use crutches and do no more than toe-touch weight bearing. The man has difficulty with the crutches because of his shoulders and falls while attempting to go upstairs to his bathroom.
A 39-year-old previously independent woman who is obese and has a previous history of depression becomes wheelchair dependent after a multiple sclerosis flair. During her hospitalization a resident physician checks off on a form in her medical record that there is a bedroom, bathroom, and kitchen on the first floor of her home with steps to enter the house. She is discharged to her husband’s care and is carried up the entry steps of her house by ambulance drivers. However, she is no longer able to enter her kitchen or bedroom because the doorways are too narrow to accommodate her large-size wheelchair, as illustrated by the physical life space sketch in Figure 2. She sleeps on her living room couch, is limited to the use of a powder room, and can no longer get prepared food from the refrigerator. Her husband now must maintain his outside employment as well as the home. Within several months the marriage is strained, the couple’s preteen children are having academic difficulties, and she is rehospitalized with profound recurrent depression, markedly increased spasticity, and incontinence.
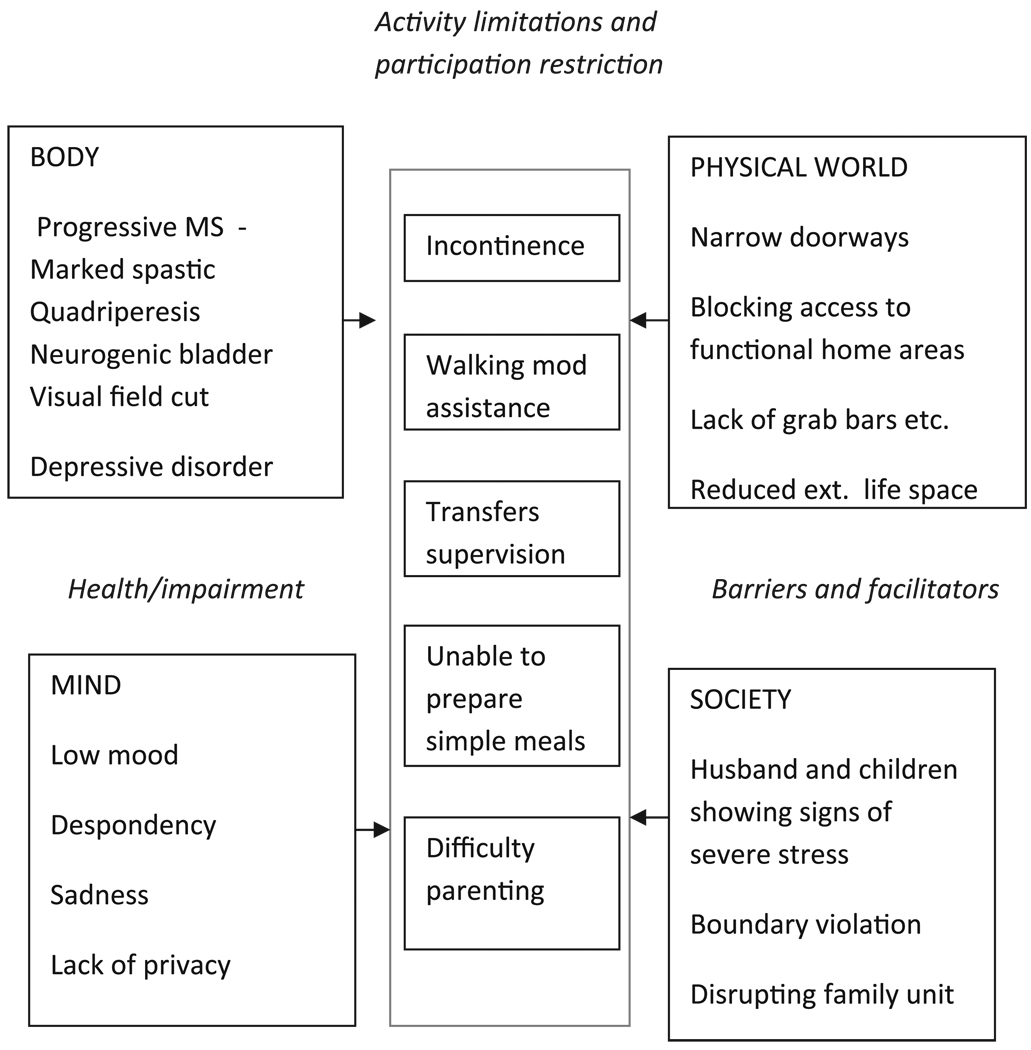
As patient and environmental complexity increase, an ecological approach becomes increasingly essential. Figure 3 shows a simplified sketch of HEI for the woman in case 2, visualizing interactions among the 4 spheres. For each activity, limitation, and participation restriction, the clinician analyzes impairment and environmental contributions. For example, neurologic impairment is causing urinary incontinence that is made worse by the increased time required for her to transfer safely onto a toilet without grab bars. The patient’s perceived lack of privacy is another potent example of confluence of effects across spheres. Her neurologic impairments interacting with specific architectural barriers are restricting her external life space, forcing her to sleep in the living room. Lost privacy, embarrassment, and boundary violation exacerbate her depression. Her depression has both somatic (body) and mental (mind) components. These components may affect her physical health, mental health, and desire to participate in life activities. Her circumstances disrupt the family’s normal use of the living room and, more importantly, the directions of their lives. The quality of her social support network declines, contributing to a downward spiral toward rehospitalization.
Figure 3.
Annotated HEI diagram for case 2. Key elements from the patient’s history, physical examination, and clinician observations are listed according to each sphere. The overlap of the 4 spheres depicts the etiological factors contributing to disability. When viewing the diagram, the clinician seeks to uncover and treat remediable physiologic and environmental elements according to each activity limitation and participation restriction.
In a resource-restricted environment, the questions change from what we can and cannot do for patients to what, given available physical and social resources, is the most efficient combination of interventions for enhancing HEI. Biomedical treatments (ie, optimizing pharmacologic management of her depression and spasticity) will be synergistic with ecological interventions (ie, enhancing the person-environment fit and providing supportive counseling to the patient and family).
Perceived increases in time and expense might be seen as barriers to PM&R’s adoption of the biopsycho-ecological model. The growing demand for more holistic approaches to medical practice that began in the 1990s was stimulated primarily by patients’ dissatisfaction with reductions in time spent with physicians [92]. This demand is ever present, as time pressures have become even greater during the past decade and can only be expected to accelerate. We cannot change time pressures, but we can alter the paradigms that guide practice in an effort to use available time more meaningfully. HEI theory calls for shift toward a more holistic multifactorial way of thinking about patients. It does not take more time to think more expansively [93]. A conceptually grounded synthesis of information from essential elements across the 4 HEI spheres ultimately may save time and resources and increase the patient’s quality of life. The physical qualities of the home environment were completely missed with catastrophic results in case 1. Although the physical environment was considered in case 2, interactions with the patient’s impairments were not addressed. Knowledge of home environmental features must be linked to specific aspects of the patient’s impairment to be meaningful. The question becomes, how do specific architectural features interact with particular impairments to limit activity and restrict participation? Similarly, how do patient’s social networks and internal mental responses influence motivation and experience? Finally, integrating all assessments, what person-level versus environment-level systems are best targeted for change? Yet it is important to acknowledge that physicians and other health professionals currently have limited control of the money and resources necessary to secure environmental modifications. Also, unfortunately, obtaining long-term, home-based supportive services for those without willing and capable family members can be extremely challenging.
According to the 2010 coverage policies of the Centers for Medicare and Medicaid Services for inpatient rehabilitation facility care, rehabilitation physicians must document concurrence with the findings and results of preadmission screening before patient admission [94]. The physician must synthesize and take responsibility for the individualized overall plan of care [95]. In doing so, it is essential to be able to estimate length of stay, medical prognosis, expected functional outcomes, and discharge destination. Such projections will be made more accurate through more careful consideration of the multiple dimensions of disability causation, including projective interactions of personal traits and impairments with the physical and social environments to which patients are to be discharged.
CONCLUSIONS
A risk in applying the biopsychosocial model is that concepts of straightforward causation and treatments established through the biomedical model can be blunted [4]. The biopsycho-ecological model, which is even more integrative, attempts to reduce this risk by distinguishing among distinct functional levels. Thus it fully embraces and honors advances continuing to be made through applications of biomedical principles. It recognizes the importance of pathogenesis, the adherence to standardized measures, and reductionistic scientific principles essential to establishing and maintaining evidence-based medical practice. It further incorporates advances from the biopsychosocial model with respect to the recognized impact of sociological factors. Finally, HEI honors the voice of individuals with disabilities and their advocates and the need to address environmental barriers, championed by the social model of disability and the ICF.
The biopsycho-ecological model of HEI recognizes illness and disabilities as arising from interactions between mental and physical characteristics and the physical and social environments. The intersections of these spheres provide a broad context beyond the medical condition for reflecting the multiple ways that disability is produced, measured, and perceived. It further distinguishes 5 levels of functioning, including cellular, body tissue, organ or system, person, and environmental experience. With this framework, the process of HEI at the most integrative levels determines both an individual’s objectively measurable activity limitations (external ecology) and the subjective meaning of that status (internal ecology). These ecologies delineate an individual’s life spaces within his or her internal and external life worlds.
Measured activity limitation along with the analysis of local environmental barriers and facilitators quantify external life space. RPE, in contrast, is applied to understand space within an individual’s internal life world, assaying the dimensions of meaning. Thus measured, activity limitation and RPE can be seen as parallel but distinct metrics that both operate to explain the same phenomenon (functioning) through objective and subjective lenses. Intended as tools of knowledge and empowerment staging, life space diagrams, HEI sketches, and the RPE procedure are examples of approaches that might prove useful in medical education, research, and clinical practice.
The clinical and research challenge for PM&R is to uncover the interventions at all levels of the hierarchy of functioning that can enhance the HEI of individual patients and populations. Future research will be necessary to explore internal and external ecology. Such research holds the promise of guiding PM&R toward incorporating the ideals of Empowerment Medicine [44, 47] (ie, the art and science of helping people regain the power of self-determination and independence).
Acknowledgments
This work was supported in part by grant R01-AG032420 from the NIH.
Footnotes
Disclosure: 8B, NIH
Contributor Information
Margaret Grace Stineman, Department of Physical Medicine and Rehabilitation, Center for Clinical Epidemiology and Biostatistics, 904 Blockley Hall, 423 Guardian Dr, Philadelphia, PA 19104-6021.
Joel E. Streim, Geriatric Psychiatry Section, University of Pennsylvania; VISN 4 Mental Illness Research Clinical & Education Center, Philadelphia Veterans Affairs Medical Center, Philadelphia, PA.
REFERENCES
- 1.De Vreese L. Causal (mis)understanding and the search for scientific explanations: A case study from the history of medicine. Stud Hist Philos Biol Biomed Sci. 2008;39:14–24. doi: 10.1016/j.shpsc.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 2.Gradmann C. A matter of methods: The historicity of Koch’s postulates 1840–2000[in German] Medizinhist J. 2008;43:121–148. [PubMed] [Google Scholar]
- 3.Hewa S, Hetherington RW. Specialists without spirit: Limitations of the mechanistic biomedical model. Theor Med. 1995;16:129–139. doi: 10.1007/BF00998540. [DOI] [PubMed] [Google Scholar]
- 4.Weiner BK. Difficult medical problems: On explanatory models and a pragmatic alternative. Med Hypotheses. 2007;68:474–479. doi: 10.1016/j.mehy.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. [Accessed December 31, 2009];A century of public health: From fluoridation to food safety: CDC celebrates Public Health Week. Available at http://www.cdc.gov/media/pressrel/a990401.htm.
- 6.Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 7.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 8.Ryff CD, Singer B. Psychological well-being: Meaning, measurement, and implications for psychotherapy research. Psychother Psychosom. 1996;65:14–23. doi: 10.1159/000289026. [DOI] [PubMed] [Google Scholar]
- 9.Fava GA, Sonino N. The biopsychosocial model thirty years later. Psychother Psychosom. 2008;77:1–2. doi: 10.1159/000110052. [DOI] [PubMed] [Google Scholar]
- 10.Stineman MG. The spheres of self fulfillment. In: Gray DB, Quatrano LA, Lieberman ML, editors. Designing and Using Assistive Technology: A Human Perspective. Baltimore, MD: Paul H. Brooks; 1998. pp. 51–74. [Google Scholar]
- 11.Stineman M, Strasser D. Team process and effectiveness: Patients, families and staff. Topic Stroke Rehabil. 1977;4:21–33. [Google Scholar]
- 12.Guarini G. The application of the theory of systems in internal medicine. State of the art and perspectives. Ann Ital Med Int. 1991;6:156–161. [PubMed] [Google Scholar]
- 13.Sudakov KV. The theory of functional systems: General postulates and principles of dynamic organization (dedicated to the Anokhin Centenary) Integr Physiol Behav Sci. 1997;32:392–414. doi: 10.1007/BF02688634. [DOI] [PubMed] [Google Scholar]
- 14.Stineman G, Ross R, Maislin G, Gray D. Population-based study of home accessibility features and the activities of daily living: Clinical and policy implications. Disabil Rehabil. 2007;29:1165–1175. doi: 10.1080/09638280600976145. [DOI] [PubMed] [Google Scholar]
- 15.Stineman MG. A model of health environmental integration. Top Stroke Rehabil. 2001;8:34–45. doi: 10.1310/0L5G-NQHY-GH4K-HV58. [DOI] [PubMed] [Google Scholar]
- 16.Stineman MG, Ross RN, Maislin G, Marchuk N, Hijirida S, Weiner MG. Recovery preference exploration: Analysis of patient feedback after imagined scenarios. Am J Phys Med Rehabil. 2007;86:272–281. doi: 10.1097/PHM.0b013e3180383acb. [DOI] [PubMed] [Google Scholar]
- 17.Granger CV, Hamilton BB, Keith RA, Zielezny M, Sherwin F. Advances in functional assessment for medical rehabilitation. Top Geriatr Rehabil. 1986;1:59–74. [Google Scholar]
- 18.Stineman MG, Ross RN, Fiedler R, Granger CV, Maislin G. Staging functional independence validity and applications. Arch Phys Med Rehabil. 2003;84:38–45. doi: 10.1053/apmr.2003.50060. [DOI] [PubMed] [Google Scholar]
- 19.Stineman MG. Defining the population, treatments, and outcomes of interest: Reconciling the rules of biology with meaningfulness. Am J Phys Med Rehabil. 2001;80:147–159. doi: 10.1097/00002060-200102000-00016. [DOI] [PubMed] [Google Scholar]
- 20. [Accessed May 2, 2010];A Dictionary of Public Health. “Theory.”. Available at http://www.oxfordreference.com/views/ENTRY.html?subview=Main&entry=t235.e4432.
- 21.Verville RE, Thomas PW. A new era in health care: Opportunities and challenges. PM R. 2009;1:511–515. doi: 10.1016/j.pmrj.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Kirschner KL, Breslin ML, Iezzoni LI, Sandel E. Attending to inclusion: People with disabilities and health-care reform. PM R. 2009;1:957–963. doi: 10.1016/j.pmrj.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Stineman M, Rist P, Kurichi J, Maislin G. Disability meanings according to patients & clinicians imagined recovery choice pathway. Qual Life Res. 2009;18:389–398. doi: 10.1007/s11136-009-9441-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Astin JA, Sierpina VS, Forys K, Clarridge B. Integration of the biopsychosocial model: Perspectives of medical students and residents. Acad Med. 2008;83:20–27. doi: 10.1097/ACM.0b013e31815c61b0. [DOI] [PubMed] [Google Scholar]
- 25.Avlund K, Lund R, Holstein BE, Due P. Social relations as determinant of onset of disability in aging. Arch Gerontol Geriatr. 2003;38:85–99. doi: 10.1016/j.archger.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Bakal D, Steiert M, Coll P, Schaefer J. An experiential mind-body approach to the management of medically unexplained symptoms. Med Hypotheses. 2006;67:1443–1447. doi: 10.1016/j.mehy.2006.05.028. [DOI] [PubMed] [Google Scholar]
- 27.Braun JV, Wykle MH, Cowling WR., III Failure to thrive in older persons: A concept derived. Gerontologist. 1988;28:809–812. doi: 10.1093/geront/28.6.809. [DOI] [PubMed] [Google Scholar]
- 28.Cohen DA, Inagami S, Finch B. The built environment and collective efficacy. Health Place. 2008;14:198–208. doi: 10.1016/j.healthplace.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Comfort A. Reality and Empathy: Physics, Mind, and Science in the 21st Century. Albany, NY: State University of New York Press Albany; 1984. [Google Scholar]
- 30.DeJong G. Independent living: from social movement to analytic paradigm. Arch Phys Med Rehabil. 1979;60:435–446. [PubMed] [Google Scholar]
- 31.Denman AM, Rager-Zisman B. Viruses and autoimmune diseases—adapting Koch’s postulates. Autoimmun Rev. 2004;3:355–361. doi: 10.1016/j.autrev.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 32.Ebers GC. Environmental factors and multiple sclerosis. Lancet Neurol. 2008;7:268–277. doi: 10.1016/S1474-4422(08)70042-5. [DOI] [PubMed] [Google Scholar]
- 33.Fougeyrollas PCR, Cloutier H, Bergeron J, Cote G. The Quebec classification: Disability creation process. Lac St-Charles, Quebec: NDCP/CSICIDH; 1998. [Google Scholar]
- 34.Freedman AM. The biopsychosocial paradigm and the future of psychiatry. Compr Psychiatry. 1995;36:397–406. doi: 10.1016/s0010-440x(95)90246-5. [DOI] [PubMed] [Google Scholar]
- 35.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 36.Fries JF. Successful aging—an emerging paradigm of gerontology. Clin Geriatr Med. 2002;18:371–382. doi: 10.1016/s0749-0690(02)00021-6. [DOI] [PubMed] [Google Scholar]
- 37.Giorgi A. The phenomenological movement and research in the human sciences. Nurs Sci Q. 2005;18:75–82. doi: 10.1177/0894318404272112. [DOI] [PubMed] [Google Scholar]
- 38.Gradmann C. Robert Koch and tuberculosis: The beginning of medical bacteriology[in German] Pneumologie. 2009;63:702–708. doi: 10.1055/s-0029-1214895. [DOI] [PubMed] [Google Scholar]
- 39.Hu P, Wagle N, Goldman N, Weinstein M, Seeman TE. The associations between socioeconomic status, allostatic load and measures of health in older Taiwanese persons: Taiwan social environment and biomarkers of aging study. J Biosoc Sci. 2007;39:545–556. doi: 10.1017/S0021932006001556. [DOI] [PubMed] [Google Scholar]
- 40.Jackson RJ. The impact of the built environment on health: An emerging field. Am J Public Health. 2003;93:1382–1384. doi: 10.2105/ajph.93.9.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jette AM, Norweg A, Haley SM. Achieving meaningful measurements of ICF concepts. Disabil Rehabil. 2008;30:963–969. doi: 10.1080/09638280701800426. [DOI] [PubMed] [Google Scholar]
- 42.Lichtenberg PA, MacNeill SE, Mast BT. Environmental press and adaptation to disability in hospitalized live-alone older adults. Gerontologist. 2000;40:549–556. doi: 10.1093/geront/40.5.549. [DOI] [PubMed] [Google Scholar]
- 43.Northridge ME, Sclar ED, Biswas P. Sorting out the connections between the built environment and health: A conceptual framework for navigating pathways and planning healthy cities. J Urban Health. 2003;80:556–568. doi: 10.1093/jurban/jtg064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nosek MA. Women with disabilities and the delivery of empowerment medicine. Arch Phys Med Rehabil. 1997;78 suppl 5:S1–S2. doi: 10.1016/s0003-9993(97)90214-8. [DOI] [PubMed] [Google Scholar]
- 45.Perdue WC, Gostin LO, Stone LA. Public health and the built environment: Historical, empirical, and theoretical foundations for an expanded role. J Law Med Ethics. 2003;31:557–566. doi: 10.1111/j.1748-720x.2003.tb00123.x. [DOI] [PubMed] [Google Scholar]
- 46.Saleebey D. Chapter 4: Human Behavior and Social Environments: A Biopsychosocial Approach. New York: Columbia University Press; 2001. [Google Scholar]
- 47.Stineman MG. Medical humanism and empowerment in medicine. Disabil Studies Q. 2000;20:11–16. [Google Scholar]
- 48.Whyte J, Hart T. It’s more than a black box; it’s a Russian doll: Defining rehabilitation treatments. Am J Phys Med Rehabil. 2003;82:639–652. doi: 10.1097/01.PHM.0000078200.61840.2D. [DOI] [PubMed] [Google Scholar]
- 49.World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 50.National Institutes of Health Office of Behavioral and Social Science Research. [Accessed October 18, 2004];Qualitative methods in health research: Opportunities and considerations in application and review, organized by the NIH Culture and Qualitative Research Interest Group. Available at http://obssr.od.nih.gov/Documents/Publications/Qualitative.PDF.
- 51.Kopec KA. Concepts of disability: The activity space model. Soc Sci Med. 1995;40:649–656. doi: 10.1016/0277-9536(94)00299-9. [DOI] [PubMed] [Google Scholar]
- 52.Frumkin H. Healthy places: Exploring the evidence. Am J Public Health. 2003;93:1451–1456. doi: 10.2105/ajph.93.9.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Galea S, Ahern J, Rudenstine S, Wallace Z, Vlahov D. Urban built environment and depression: A multilevel analysis. J Epidemiol Community Health. 2005;59:822–827. doi: 10.1136/jech.2005.033084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 55.Hood E. Dwelling disparities: How poor housing leads to poor health. Environ Health Perspect. 2005;113:A310–A317. doi: 10.1289/ehp.113-a310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kochtitzky CS, Frumkin H, Rodriguez R, et al. Urban planning and public health at CDC. MMWR Morb Mortal Wkly Rep. 2006;55 suppl 2:34–38. [PubMed] [Google Scholar]
- 57.Leyden KM. Social capital and the built environment: The importance of walkable neighborhoods. Am J Public Health. 2003;93:1546–1551. doi: 10.2105/ajph.93.9.1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rao M, Prasad S, Adshead F, Tissera H. The built environment and health [see comment] Lancet. 2008;371(9609):302. doi: 10.1016/S0140-6736(07)61260-4. [DOI] [PubMed] [Google Scholar]
- 59.Retting RA, Ferguson SA, McCartt AT. A review of evidence-based traffic engineering measures designed to reduce pedestrian-motor vehicle crashes. Am J Public Health. 2003;93:1456–1463. doi: 10.2105/ajph.93.9.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosenthal JK, Sclar ED, Kinney PL, Knowlton K, Crauderueff R, Brandt-Rauf PW. Links between the built environment, climate and population health: Interdisciplinary environmental change research in New York City. Ann Acad Med Singapore. 2007;36:834–846. [PubMed] [Google Scholar]
- 61.Keysor JJ, Jette AM, Lavalley MP, et al. Community environmental factors are associated with disability in older adults with functional limitations: The MOST Study. J Gerontol A Biol Sci Med Sci. 2009 doi: 10.1093/gerona/glp182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shumway-Cook A, Patla A, Stewart A, Ferrucci L, Ciol MA, Guralnik JM. Environmental components of mobility disability in community-living older persons. J Am Geriatr Soc. 2003;51:393–398. doi: 10.1046/j.1532-5415.2003.51114.x. [DOI] [PubMed] [Google Scholar]
- 63.Stineman MG, Qu W. Untangling function: Measuring the severity, type and meaning of disabilities. Eura Medicophys. 2007;43:543–549. [PubMed] [Google Scholar]
- 64.Joyce CR, Hickey A, McGee HM, O’Boyle CA. A theory-based method for the evaluation of individual quality of life: The SEIQoL. Qual Life Res. 2003;12:275–280. doi: 10.1023/a:1023273117040. [DOI] [PubMed] [Google Scholar]
- 65.Manchikanti L, Derby R, Wolfer L, Singh V, Datta S, Hirsch JA. Evidence-based medicine, systematic reviews, and guidelines in interventional pain management: Part 7: Systematic reviews and meta-analyses of diagnostic accuracy studies. Pain Physician. 2009;12:929–963. [PubMed] [Google Scholar]
- 66.Chung KC, Shauver MJ. Crafting practice guidelines in the world of evidence-based medicine. Plast Reconstr Surg. 2009;124:1349–1354. doi: 10.1097/PRS.0b013e3181b5a3db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Withers R. Descartes’ dreams. J Anal Psychol. 2008;53:691–709. doi: 10.1111/j.1468-5922.2008.00760.x. [DOI] [PubMed] [Google Scholar]
- 68.Porcelli P, Todarello O. Psychological factors affecting functional gastrointestinal disorders. Adv Psychosom Med. 2007;28:34–56. doi: 10.1159/000106796. [DOI] [PubMed] [Google Scholar]
- 69.Hayes AM, JL S. Dynamic systems theory as a paradigm for the study of change in psychotherapy: An application to cognitive therapy for depression. J Consult Clin Psychol. 1998;66:939–947. doi: 10.1037//0022-006x.66.6.939. [DOI] [PubMed] [Google Scholar]
- 70.Garcia-Toro M, Aguirre I. Biopsychosocial model in depression revisited. Med Hypotheses. 2007;68:683–691. doi: 10.1016/j.mehy.2006.02.049. [DOI] [PubMed] [Google Scholar]
- 71.Kable JW, Glimcher PW. The neurobiology of decision: consensus and controversy. Neuron. 2009;63:733–745. doi: 10.1016/j.neuron.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chow JY, Davids K, Button C, Rein R, Hristovski R, Koh M. Dynamics of multi-articular coordination in neurobiological systems. Nonlinear Dynamics Psychol Life Sci. 2009;13:27–55. [PubMed] [Google Scholar]
- 73.Kim HK, Park S, Srinivasan MA. Developments in brain-machine interfaces from the perspective of robotics. Hum Mov Sci. 2009;28:191–203. doi: 10.1016/j.humov.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 74.Stineman MG, Jette A, Fiedler R, Granger C. Impairment-specific dimensions within the Functional Independence Measure. Arch Phys Med Rehabil. 1997;78:636–643. doi: 10.1016/s0003-9993(97)90430-5. [DOI] [PubMed] [Google Scholar]
- 75.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 76.Reisberg B, Franssen EH, Hasan SM, et al. Retrogenesis: Clinical, physiologic, and pathologic mechanisms in brain aging, Alzheimer’s and other dementing processes. Eur Arch Psychiatry Clin Neurosci. 1999;249 suppl 3:28–36. doi: 10.1007/pl00014170. [DOI] [PubMed] [Google Scholar]
- 77.Stineman MG, Ross RN, Fiedler R, Granger CV, Maislin G. Functional independence staging: Conceptual foundation, face validity, and empirical derivation. Arch Phys Med Rehabil. 2003;84:29–37. doi: 10.1053/apmr.2003.50061. [DOI] [PubMed] [Google Scholar]
- 78.Tao W, Haley SM, Coster WJ, Ni P, Jette AM. An exploratory analysis of functional staging using an item response theory approach. Arch Phys Med Rehabil. 2008;89:1046–1053. doi: 10.1016/j.apmr.2007.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Goering S. Revisiting the relevance of the social model of disability. Am J Bioeth. 10:54–55. doi: 10.1080/15265160903460913. [DOI] [PubMed] [Google Scholar]
- 80.Hofkamp SE, Henrikson CA, Wegener ST. An interactive model of pain and myocardial ischemia. Psychosom Med. 2007;69:632–639. doi: 10.1097/PSY.0b013e318151a4bd. [DOI] [PubMed] [Google Scholar]
- 81.Raichle KA, Hanley M, Jensen MP, Cardenas DD. Cognitions, coping, and social environment predict adjustment to pain in spinal cord injury. J Pain. 2007;8:718–729. doi: 10.1016/j.jpain.2007.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wilz G, Barskova T. Predictors of psychological and somatic components of poststroke depression: A longitudinal study. Top Stroke Rehabil. 2007;14:25–40. doi: 10.1310/tsr1403-25. [DOI] [PubMed] [Google Scholar]
- 83.May D, Nayak US, Isaacs B. The life-space diary: a measure of mobility in old people at home. Int Rehabil Med. 1985;7:182–186. doi: 10.3109/03790798509165993. [DOI] [PubMed] [Google Scholar]
- 84.Jette AM, Haley SM, Ni P, Olarsch S, Moed R. Creating a computer adaptive test version of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2008;63:1246–1256. doi: 10.1093/gerona/63.11.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil. 1994;75:127–132. [PubMed] [Google Scholar]
- 86.Stineman MG. A model of health environmental integration. Top Stroke Rehabil. 2001;8:34–45. doi: 10.1310/0L5G-NQHY-GH4K-HV58. [DOI] [PubMed] [Google Scholar]
- 87.Stineman MG, Ross RN, Maislin G, Marchuk N, Hijirida S, Weiner M. Recovery preference exploration. Am J Phys Med Rehabil. 2007;86:272–281. doi: 10.1097/PHM.0b013e3180383acb. [DOI] [PubMed] [Google Scholar]
- 88.Kurz AE, Saint-Louis N, Burke JP, Stineman MG. Exploring the personal reality of disability and recovery: A tool for empowering the rehabilitation process. Qual Health Res. 2008;18:90–105. doi: 10.1177/1049732307309006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stineman MG, Maislin G, Nosek M, Fiedler R, Granger CV. Comparing consumer and clinician values for alternative functional states: Application of a new feature trade-off consensus building tool. Arch Phys Med Rehabil. 1998;79:1522–1529. doi: 10.1016/s0003-9993(98)90413-0. [DOI] [PubMed] [Google Scholar]
- 90.Rist PM, Freas DW, Maislin G, Stineman MG. Recovery from disablement: What functional abilities do rehabilitation professionals value the most? Arch Phys Med Rehabil. 2008;89:1600–1606. doi: 10.1016/j.apmr.2007.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mukherjee D, Brashler R, Savage TA, Kirschner KL. Moral distress in rehabilitation professionals: Results from a hospital ethics survey. PM R. 2009;1:450–458. doi: 10.1016/j.pmrj.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 92.Hughes MD. The holistic way: John Wesley’s practical piety as a resource for integrated healthcare. J Relig Health. 2008;47:237–252. doi: 10.1007/s10943-007-9146-x. [DOI] [PubMed] [Google Scholar]
- 93.Siebens H. The domain management model—a tool for teaching and management of older adults in emergency departments. Acad Emerg Med. 2005;12:162–168. doi: 10.1197/j.aem.2004.08.055. [DOI] [PubMed] [Google Scholar]
- 94.FY 2010 IRF PPS Final Rule. 74 Fed Reg. 2010;39762:39788–39788. [Google Scholar]
- 95.Department of Human Services. New coverage policies for inpatient rehabilitation services. Washington, DC: CMS Medicare Learning Network; 2009. Nov, [Google Scholar]