Abstract
Background:
Accessibility to tertiary intensive care resources differs among hospitals within a rural region. Determining whether accessibility is associated with outcome is important for understanding the role of regionalization when providing critical care to a rural population.
Methods:
In a prospective design, we identified and recorded the mortality ratio, percentage of unanticipated deaths, length of stay in the intensive care unit (ICU), and survival time of 147 patients transferred directly from other hospitals and 178 transferred from the wards within a rural tertiary-care hospital.
Results:
The two groups did not differ significantly in the characteristics measured. Differences in access to tertiary critical care in this rural region did not affect survival or length of stay after admission to this tertiary ICU. The odds ratio (1.14; 95% confidence interval 0.72-1.83) for mortality associated with transfer from a rural community hospital was not statistically significant.
Conclusions:
Patients at community hospitals in this area who develop need for tertiary critical care are just as likely to survive as patients who develop ICU needs on the wards of this rural tertiary-care hospital, despite different accessibility to tertiary intensive-care services.
Keywords: decision-making, interhospital transport, rural health services, survival analysis
Introduction
Some hospitalized medical and surgical patients develop the need for critical-care resources that are available only at tertiary hospitals. Differences in accessibility to tertiary intensive care exist among hospitals within a rural region. For example, some patients are admitted from rural community hospitals that do not provide the same access to critical-care resources as is available to patients in the wards of tertiary hospitals. Therefore, the location of care (rural community hospital versus tertiary care center) before admission to a tertiary intensive care unit (ICU) may affect outcome.
Determining whether accessibility is associated with outcome is important for understanding the role of regionalization when providing critical care to a rural population. Currently there is little direct evidence to support regionalization of adult medical and surgical critical-care services [1]. If accessibility proves to be a determinant of outcome, then development of a regional critical-care program might be beneficial. If, however, accessibility does not affect the outcome of tertiary critical care, then efforts to create a regional critical-care service may be unnecessary or even detrimental. Using the location of care (rural community hospital versus tertiary care center) before admission to a tertiary ICU to describe differences in accessibility, we examined the relationship of accessibility to mortality and length of stay.
Patients and methods
Study population
This prospective cohort study was approved by our institutional review board. The study was completed in a rural region of the United States that is primarily served by one tertiary-care referral center. Based on the Dartmouth Atlas of Health Care, the Lebanon, NH, hospital-service area (HSA) served a Medicare population of 53,000 in 1996, which was in the second quartile (25th to 50th percentile) of Medicare population distribution for all United States HSAs [2]. The average distance from the referring hospitals to the tertiary-care facility was 64.5 miles. Seventeen of the 29 outside hospitals were more than 50 miles away, and the farthest one was 129 miles away. Eight of the 29 hospitals had fewer than 50 inpatient beds, and 21 of the 29 had fewer than 100 beds. A power analysis was completed to determine sample size. A sample size of 304 patients was needed to detect a 20% difference in mortality rate, with α 0.05 and β 0.20. From consecutive ICU admissions at the tertiary facility during a 15-month period from October 1996 to December 1997, 325 patients were transferred 1) from the wards or ICUs of community hospitals or 2) from the wards of the tertiary-care hospital. Patients admitted from the emergency room, operating room, recovery room, or another ICU within the tertiary-care hospital were excluded.
Patient, process, and outcome measures
Data regarding age, sex, diagnosis upon admission to ICU, primary-diagnosis-related grouping, primary service, pre-ICU source, Acute Physiology and Chronic Health Evaluation (APACHE) II score, and Therapeutic Intervention Scoring System (TISS) scores were collected for each patient upon admission to the ICU [3,4]. In-hospital mortality, intensive care, and length of hospital stay were recorded for each patient. Unanticipated death was defined as any death of a patient whose predicted risk of hospital death was less than 25% using APACHE II. Standardized mortality ratios were calculated using the predicted risk of hospital death from the APACHE II scoring system.
Matching analysis
A matching analysis was also performed using these data to evaluate the potential impact of differences in the distribution of admission diagnoses on the primary results. Patients transferred from an outside hospital were matched to patients transferred from the wards of the tertiary-care hospital based on the primary-admission diagnosis that prompted admission to the ICU, sex, and a difference in age less than 5 years. Severity of illness was not used as a matching criterion.
Statistical analysis
Statistical analysis was performed using STATA software [5]. A P value less than 0.05 was considered statistically significant for all analyses. Mortality rates, percentage medical admissions, sex, the percentage of admissions according to the day of the week, and the distribution of admission diagnoses were compared using the chi-square test. APACHE II and TISS scores and age were compared using analysis of variance, and these results are presented as mean ± standard deviation. All comparisons of length of stay were made using the log rank test and are presented as medians because of non-normal distribution. Survival time was determined from the time of ICU admission. Kaplan-Meier survival curves for each group were compared using the log rank test. For the matching analysis, McNemar's chi-square test was used.
Results
Study population
There were 803 admissions to the ICU during the 15-month study period. Of these, 147 (18%) were of patients transferred directly from other hospitals and 178 (22%) were of patients transferred from wards within the hospital. Patients who were transferred from other hospitals arrived from one of 29 community hospitals. Only four of these hospitals sent more than 10 patients during the study period, and 12 of these hospitals referred fewer than two.
Distribution of ICU admissions by day of the week
The frequency of admission for each day of the week was compared according to source of admission. For internal transfers, the percentage of admission by day of week ranged from 11 to 20, with Saturdays the busiest. For outside transfers, the range was 12-16% per day of the week, with Wednesdays and Fridays the busiest. There was no significant difference in these distributions by day of the week.
Characteristics of patients
Patient characteristics are summarized in Table 1. Outside transfers had a lower mean age (53.4 ± 17.4 versus 59.3 ± 17.3 years, P < 0.05) than internal transfers. The distributions of primary-admission diagnoses at ICU admission were significantly different for the two groups. For outside transfers, the most frequent admission diagnoses were gastrointestinal bleeding (n = 24) and multiple trauma (n = 23); for internal transfers, they were respiratory infection (n = 29) and sepsis (n = 23). The numbers of medical admissions were not significantly different. The mean APACHE II score upon ICU admission for outside transfers was 16.6 ± 7.9, and for internal transfers was 17.5 ± 6.5 (P = 0.24).
Table 1.
Characteristics of patients admitted to ICU of Tertiary Hospital
| From outside | From within | ||
| tertiary hospital | tertiary hospital | P | |
| Sample size (n) | 147 | 178 | |
| Mean age (y) | 53.4 (± 17.4) | 59.5 (± 17.3) | 0.005 |
| Sex (% female) | 43 | 45 | 0.70 |
| Mean APACHE II score, | 16.6 (± 7.9) | 17.5 (± 6.5) | 0.24 |
| ICU day 1 | |||
| Mean TISS score, | 25.0 (± 6.1) | 25.3 (± 7.1) | 0.76 |
| ICU day 1 | |||
| Medical patients | 62 % | 60 % | 0.74 |
Outcomes
In-hospital mortality was not significantly different between outside and internal transfers: 33% versus 30%, respectively (P = 0.58) (Table 2). The odds ratio for transferring from another hospital was 1.14 (95% confidence interval 0.72-1.83). There was no significant difference in the frequency of unanticipated deaths, 7.5% versus 9.5%, respectively (P = 0.51). In addition, standardized mortality ratios for both groups were within 95% confidence intervals, demonstrating no significant difference between observed mortality and predicted mortality based on APACHE II. The median length of stay (LOS) from time of admission to the ICU to either hospital discharge or death was not significantly different between outside and internal transfers (9 versus 11 days, respectively, P = 0.08). Median LOS in the ICU (3 versus 4 days, respectively, P = 0.74) was also comparable. Survival time analysis was completed using LOS from time of admission to the ICU to either discharge or in-hospital death. Seventy-five per cent of hospital discharges or deaths occurred within 19 days from admission to the ICU date. Survival time (Fig. 1) after adjustment for severity of illness was not significantly different for the interhospital transfer group as compared with internal ICU transfers (log rank test, P = 0.24).
Table 2.
Outcomes of patients studied
| From outside | From within | ||
| tertiary hospital | tertiary hospital | P | |
| Crude mortality rate | 33% | 30% | 0.58 |
| Median intensive care | 3 | 4 | 0.74 |
| LOS (days) | |||
| Median survival time (days) | 24 | 34 | 0.24 * |
| Unanticipated deaths | 7.5% | 9.5% | 0.51 |
| Mortality ratio | 1.27 | 1.07 | |
| (95% CI) | (0.92-1.67) | (0.79-1.39) |
*Log rank test.
Figure 1.
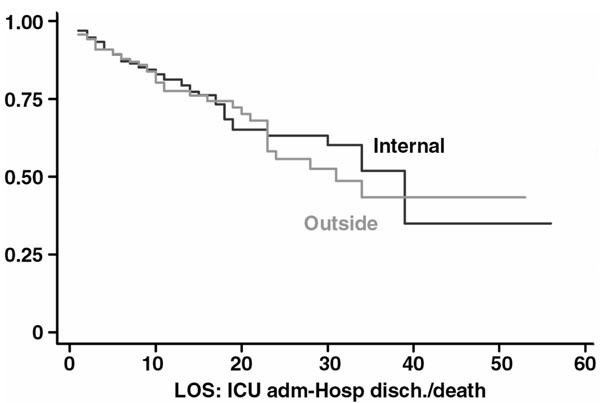
Kaplan-Meier plot of in-hospital survival time adjusted for APACHE score on ICU day 1.
Adjustment for case mix: matching analysis
From among the study population of 325 patients, 138 could be matched according to the three criteria (diagnosis at primary admission to the ICU, sex, and age within 5 years), giving 69 pairs who were transferred to the ICU from within and from outside the tertiary-care hospital. For this matching analysis, the mean APACHE II score upon admission to the ICU was 16.5 for outside transfers and 17.7 for internal transfers (P = 0.33). The outside transfers were no more or less likely to survive than internal transfers (McNemar's test, P = 0.83). Survival time was not significantly different for the two groups (log rank test, P = 0.58).
Discussion
We observed that differences in access to tertiary critical-care resources in this rural region did not affect survival or length of stay after admission to this tertiary ICU. The odds ratio (1.14; 95% confidence interval: 0.72-1.83) for mortality associated with transfer from a rural community hospital was not statistically significant. This observation suggests that medical and surgical patients within this rural health-service area who develop the need for tertiary intensive care are not hindered by receiving prior care at a community hospital. Patients at community hospitals in this area who develop a need for tertiary critical care are just as likely to survive, despite different accessibilities to tertiary intensive-care services.
While there is evidence that regionalization of trauma, burn, and neonatal care leads to improved outcomes, there is not clear evidence that regionalization provides a benefit for more common disorders requiring intensive care, such as chronic obstructive pulmonary exacerbation requiring ventilation, inflammatory syndromes, or renal failure [1,6,7,8]. Although we did not observe a significant difference between the outcomes of the two groups, this study was powered to detect a 20% difference in mortality rate. Evaluation of at least 1900 patients would be necessary to determine the significance of the odds ratio (1.14) found in this study. Using a similar methodology to examine 4857 admissions to a tertiary surgical ICU, Rosenberg et al [9] observed an odds ratio for hospital mortality of 1.9 for patients who transferred from another hospital.
The results of the current study do not support the need for further development of regional critical-care services in this hospital-service area. However, there were regional programs that existed during the study period and continue to operate now. This tertiary-care hospital is a level I trauma center and its trauma service maintains a quality assurance and educational network to these referring hospitals. The importance of rapid, early transport has been emphasized in these ongoing educational efforts [10,11,12]. In addition, a critical-care fellow or staff person is available 24 hours a day at the tertiary hospital for referring physicians to contact regarding triage issues. Finally, a helicopter transport service staffed by flight paramedics is available for transfers to the tertiary-care facility, weather permitting.
These data also illustrate how infrequently inpatients develop the need for tertiary intensive care at any of the referring hospitals. Physicians at these hospitals are faced with the formidable triage challenge of identifying the few patients who need tertiary critical-care services. Based on our observations, we conclude that these physicians are just as capable of selecting appropriate patients for transfer to this tertiary ICU as physicians within the tertiary-care hospital. However, we did not study the outcome of patients who were not selected during triage for transfer to the tertiary ICU at either the rural community hospitals or the tertiary hospital. Important geographic variations in the delivery of health care have been documented, which consistently reveal a lack of conformity of practice patterns among physicians in the same hospital-service area [13].
In order to identify a group of patients comparable with those being transferred from outside community hospitals, we selected patients who were transferred from the wards of this tertiary-care hospital. While these two groups did not differ significantly in mean age or severity of illness, they did differ in distribution of diagnoses at admission. Therefore, we sought to examine whether selection bias could explain our observation, by completing a matching analysis. We matched patients by primary diagnosis at admission, by age, and by sex, in order to identify two groups with the same distribution of diagnoses at admission. We did not use severity of illness as a matching criterion, because APACHE II scores for this parameter did not differ significantly among the groups in the cohort of 803 patients, and the use of an additional criterion would have unnecessarily limited the matching process. We observed the same finding as before in this matching analysis: that the two groups did not differ in their in-hospital mortality or survival. This suggests that differences in the distribution of admission diagnoses are not likely to explain the reported findings. We also controlled for lead-time bias in this analysis. 'Lead time' is defined as the interval between identifying a need for critical care using screening and identifying a need for critical care based on clinical deterioration. In order to eliminate lead-time bias, we defined the beginning of the stay for this analysis as admission to the tertiary ICU.
Although the two groups had similar survival times, we did not examine other outcomes such as cost, functional status, family satisfaction, or long-term survival. There may be significant differences in these outcomes with different locations of pre-ICU care. Quantification of these outcomes is important for a thorough understanding of the impact of transfer decisions and location of care on outcomes for critical care.
The major reason for moving a critically ill patient is to provide more care. Because the period of transfer may impose risks on the patient, transfer should not be considered unless some resulting benefit is expected. The decision to transfer the patient to another hospital is the responsibility of the attending physician at the referring hospital, and it is their responsibility to obtain the informed consent of the patient, or of their legally authorized representative if the patient is not capable of making decisions. Guidelines for the transfer of patients have been published [14].
For this analysis, information about the process of care before and during transfer to the ICU was not collected. Further study is necessary to define more precisely how pre-ICU processes of care, triage, and transport are associated with survival after ICU care. For example, the processes of triage among the 30 hospitals that transferred patients to this ICU probably differ, and will therefore influence the patient population at the tertiary-care ICU. Patients who remained in the ICUs of the community hospitals were not included in the analysis, and their survival ratio may have been different. Inclusion of such patients in future studies will improve our understanding of how to optimize the delivery of intensive care in a rural area.
Conclusion
Differences in access to tertiary critical care in the rural region studied did not significantly affect survival or length of stay after admission to the tertiary ICU in the region. Interfacility transfer is important to regional critical-care systems, and this study does not show any negative impact on survival as a result of current interfacility transfer practice in this hospital-service region.
References
- Crippen D. Regionalization, prioritization, and sailing ships in the year 2010. New Horizons. 1999;7:218–228. [Google Scholar]
- The Dartmouth Atlas of Health Care Chicago: American Hospital Publishing, 1999.
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- Keene AR, Cullen DJ. Therapuetic Intervention Scoring System: update 1983. Crit Care Med. 1983;11:1–3. doi: 10.1097/00003246-198301000-00001. [DOI] [PubMed] [Google Scholar]
- Stata Statistical Software: Release 60 College Station, TX: Stata Corporation; 1997.
- Cales RH. Trauma mortality in Orange County: the effect of implementation of a regional trauma system. Ann Emerg Med. 1984;13:1–10. doi: 10.1016/s0196-0644(84)80375-3. [DOI] [PubMed] [Google Scholar]
- Gortmaker S, Sobol A, Clark C, Walker DK, Geronimus A. The survival of very low birth weight infants by level of hospital of birth: a population study of perinatal systems in four states. Am J Obstet Gynecol. 1985;152:517–525. doi: 10.1016/0002-9378(85)90618-0. [DOI] [PubMed] [Google Scholar]
- Thompson DR, Clemmer TP, Applefield JJ, Crippen DW, Jastremski MS, Lucas CE, Pollack MM, Wedel SK. Regionalization of critical care medicine: Task Force report of the American College of Critical Care Medicine. Crit Care Med. 1994;22:1306–1313. doi: 10.1097/00003246-199408000-00015. [DOI] [PubMed] [Google Scholar]
- Rosenberg AL, Hofer TP, Hayward RA, Strachan C, Watts CM, Bartlett RH. Admission source predicts surgical ICU outcomes: implications for tertiary referral centers [abstract]. Anesthesiology. 2000;3A:B7. [Google Scholar]
- Schwartz RJ, Jacobs LM, Yaezel D. Impact of pre-trauma center care on length of stay and hospital charges. J Trauma. 1989;29:1611–1615. doi: 10.1097/00005373-198912000-00002. [DOI] [PubMed] [Google Scholar]
- Valenzuela TD, Criss EA, Copass MK, Luna GK, Rice CL. Critical care air transportation of the severely injured: does the long transport adversely affect survival? Ann Emerg Med. 1990;19:169–172. doi: 10.1016/s0196-0644(05)81803-7. [DOI] [PubMed] [Google Scholar]
- Norwood S, Fernandez L, England J. The early effects of implementing American College of Surgeons Level II criteria on transfer and survival rates at a rurally based community hospital. J Trauma. 1995;39:240–245. doi: 10.1097/00005373-199508000-00009. [DOI] [PubMed] [Google Scholar]
- Wennberg JE. Understanding geographic variations in health care delivery. N Engl J. 1999;340:52–53. doi: 10.1056/NEJM199901073400111. [DOI] [PubMed] [Google Scholar]
- Anonymous: Guidelines for the transfer of critically ill patients. Crit Care Med. 1993;21:931–937. [PubMed] [Google Scholar]


