Abstract
Background
Hearing loss has been associated with tobacco smoking, but its relationship with secondhand smoke is not known. We sought to investigate the association between secondhand smoke exposure and hearing loss in a nationally representative sample of adults.
Methods
The National Health and Nutrition Examination Survey, a nationally representative cross-sectional dataset, was utilized to investigate the association between secondhand smoke exposure and hearing loss. Data collected from non-smoking participants aged 20-69 years were included in the analysis if they had completed audiometric testing, had a valid serum cotinine value, and provided complete smoking, medical co-morbidity and noise exposure histories (n=3,307). Hearing loss was assessed from averaged pure-tone thresholds over low- or mid-frequencies (500, 1,000, and 2,000 Hz) and high-frequencies (3,000, 4,000, 6,000, and 8,000 Hz), and was defined as mild or greater severity (pure-tone average in excess of 25 dB HL).
Results
SHS exposure was significantly associated with increased risk of hearing loss for low-/mid-frequencies (Adjusted Odds Ratio = 1.14; 95% CI = 1.02-1.28 for never smokers and 1.30; 1.10-1.54 for former smokers) and high-frequencies (1.40; 1.22-1.81 for former smokers), after controlling for potential confounders.
Conclusions
Findings from the present analysis indicate that SHS exposure is associated with hearing loss in non-smoking adults.
Keywords: Secondhand Smoke, Hearing Loss, Tobacco Policy, Audiology
What this study adds.
Although previous studies have shown an association between active smoking and increased risk of hearing loss, this is the first study to directly assess the relationship between hearing loss and passive smoking using national data and biomarkers for secondhand exposure among US adults. We report significantly increased adjusted odds for hearing loss among former smokers for both low-/mid- and high-frequency hearing loss and increased risk of low-frequency hearing loss among never smokers. The stronger findings among former smokers suggest that continued SHS exposure, even at low levels, may continue the progression of high-frequency hearing loss that began when they were active smokers.
INTRODUCTION
Hearing loss is a major public health concern affecting more than 16.1% (29 million) of adults in the United States.1 The consequences of untreated hearing loss include: reduced health-related quality of life in elderly populations2, increased risk of occupational3 and non-occupational injuries4, and reduced earning potential.5 Increased risk for hearing loss is associated with occupational and non-occupational noise exposure, age, male gender, and lower educational attainment.6-8 Numerous studies have shown primary tobacco smoke to be associated with a significant risk of hearing loss.7-12 For example, Cruickshanks et al.,7 using a population-based, cross-sectional study design, reported that current smokers were 1.69 times more likely to have a hearing loss relative to non-smokers after adjustment for other risk factors. Given the emerging evidence of a relationship between primary tobacco smoking and hearing loss it is reasonable to postulate that a similar association exists between secondhand smoke (SHS) exposure and hearing loss. However, the results of the few available studies of secondhand smoke (SHS) exposure, however, have been contradictory, associated with only a slightly increased or no increased risk of hearing loss.7 The aim of the present study was to investigate the relationship between SHS exposure in former or never smokers and sensorineural hearing loss from a large, representative study of US households.
METHODS
Description of Survey
The National Health and Nutrition Examination Survey (NHANES), a household survey combined with a medical examination, is conducted every year by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention.13 The survey is designed to be representative of the non-institutionalized civilian US population. We extracted data from the 1999-2004 NHANES, which included audiometric testing. During these years, the response rate to the household interview and medical examination ranged from 71-76% (73% [n=11,405] of the potential subject population aged 20-69 years [n=15,669]).14 One-half of these participants (n= 5,742) were randomly assigned for audiometric evaluation; 89.5% of this total (n=5,147) completed audiometric testing.
Measures
SHS exposure
Survey participants identified as having tried smoking were asked: “Do you smoke cigarettes now?” Those respondents who answered “yes” were classified as current smokers and were excluded from the analysis. Cotinine, the primary metabolite of nicotine, is widely used as a biomarker of exposure to tobacco for both active smoking and SHS.15 Cotinine levels above 3 ng/mL have been suggested to indicate a current smoker status for the majority of racial/ethnic groups.16 We therefore eliminated those with cotinine values above this threshold. Survey participants who had a serum cotinine level at or above the level of detection (0.050 ng/mL) were classified as SHS-exposed. For analysis purposes, the value for data below detectable limits was the limit divided by the square root of two.17
Audiometric Evaluation
Pure-tone air conduction hearing thresholds were obtained for each ear at frequencies of 500, 1,000, 2,000, 3,000, 4,000, 6,000, and 8,000 Hz using calibrated equipment and standard testing procedures. Using the methods employed by Bainbridge et al,18 test results were classified as the average worse-ear thresholds over low- or mid-frequencies (500, 1,000, and 2,000 Hz) and high-frequencies (3,000, 4,000, 6,000, and 8,000 Hz) and were defined as mild or greater severity (pure tone average in excess of 25 dB HL).19
Statistical Analysis
The dichotomous outcome for low-mid and high-frequency hearing loss was analyzed using multivariate logistic regression. The independent variable of interest was SHS exposure as measured by natural log-transformed cotinine level. All analyses were adjusted for age, gender, race/ethnicity, education level, diabetes status, exposure to firearms noise, and exposure to occupational noise to control for their possible confounding effects.18 SAS 9.2 survey procedures were used to perform the analyses, using the proper weights and adjusting for the complex sampling design effects.20 Estimated probabilities of low-mid and high-frequency hearing loss were computed as a function of log-transformed cotinine level from the logistic regression parameters, substituting means or proportions of the sample for covariate values to represent the average US adult population. These adjusted probabilities were used to plot the association between SHS exposure and hearing loss across the range of exposure values. We also conducted analyses stratified by age group (20-44, 45-64, and 65+) and by sex. Among the NHANES participants who completed the audiometric testing (n=5,147), we eliminated the data of those who: 1) had incomplete audiometric data (n=5); 2) did not have a cotinine measure (n=312); 3) were missing a covariate measure (n=7); and 4) were self-reported smokers and/or had a measured cotinine value > 3 ng/ml (n=1,516). As a result, the analytic sample included only former smokers (n=972) and never smokers (n=2,335). In addition, among former smokers, we assessed the relationship between number of years smoked, pack-years, and years since quitting and hearing loss.
RESULTS
Among former smokers the prevalence of low-/mid-frequency hearing loss and high frequency hearing loss was 14.0% and 46.6%, respectively. Among never smokers these prevalence estimates were 8.6% and 26.6%. The results of the multivariate analysis revealed a significant positive association between SHS exposure and low-/mid-frequency hearing loss for both former and never smokers (p=0.003 and p=0.027, respectively). A highly significant positive association was also observed between SHS exposure in former smokers and high-frequency hearing loss (p<0.001).
Covariates and Hearing Loss
Increased age, male gender, and diabetes were associated with significantly increased risk of high-frequency hearing loss for both never and former smokers (Table). Being older was associated with significantly increased risk of hearing loss for low-/mid-frequencies in both never and former smokers. Male gender and diabetes were associated with increased risk of low-/mid-frequency hearing loss in never smokers. Black former and never smokers were significantly less likely to have high-frequency hearing loss than whites, and college-educated never smokers were significantly less likely to have high-frequency hearing loss than those with high school education.
Table.
Multivariable odds ratios predicting high frequency and low/mid frequency hearing loss status in never and former smokers: National Health and Nutrition Examination Survey 1999-2004
| Never Smoker | Former Smoker | |||||
|---|---|---|---|---|---|---|
| n | Odds Ratio | 95% CI* | n | Odds Ratio | 95% CI* | |
|
High Frequency Hearing Loss | ||||||
| Age (years)1 | 2335 | 1.12 | 1.11–1.14 | 972 | 1.16 | 1.13–1.19 |
| Race | ||||||
| White | 1010 | 1.00 | 552 | 1.00 | ||
| Black | 456 | 0.56 | 0.39–0.79 | 129 | 0.20 | 0.09–0.45 |
| Other | 869 | 0.84 | 0.54–1.31 | 291 | 0.78 | 0.39–1.54 |
| Gender | ||||||
| Female | 1460 | 1.00 | 459 | 1.00 | ||
| Male | 875 | 3.95 | 2.81–5.55 | 513 | 5.41 | 3.19–9.19 |
| Education | ||||||
| Less than high school | 595 | 1.00 | 261 | 1.00 | ||
| High school or equivalent | 468 | 0.74 | 0.47–1.17 | 207 | 0.63 | 0.31–1.26 |
| Some college or greater | 1272 | 0.42 | 0.25–0.70 | 504 | 0.56 | 0.27–1.18 |
| Diabetic | ||||||
| No | 2165 | 1.00 | 875 | 1.00 | ||
| Yes | 170 | 2.26 | 1.34–3.80 | 97 | 2.21 | 1.17–4.16 |
| Exposed to Firearm Noise | ||||||
| No | 2236 | 1.00 | 895 | 1.00 | ||
| Yes | 99 | 1.64 | 0.97–2.78 | 77 | 1.72 | 0.77–3.83 |
| Exposed to Loud Occupational Noise | ||||||
| No | 1786 | 1.00 | 629 | 1.00 | ||
| Yes | 549 | 1.36 | 0.94–1.98 | 343 | 1.44 | 0.86–2.39 |
| Ln Cotinine Level (ng/mL)2 | 2335 | 1.08 | 0.97–1.20 | 972 | 1.40 | 1.23–1.61 |
|
Low/Mid Frequency Hearing Loss | ||||||
| Age (years)1 | 2335 | 1.08 | 1.01–1.10 | 972 | 1.13 | 1.10–1.16 |
| Race | ||||||
| White | 1010 | 552 | ||||
| Black | 456 | 0.58 | 0.34–1.00 | 129 | 0.63 | 0.31–1.29 |
| Other | 869 | 0.93 | 0.52–1.63 | 291 | 1.38 | 0.74–2.56 |
| Gender (Male Vs Female) | ||||||
| Female | 1460 | 459 | ||||
| Male | 875 | 1.33 | 0.82–2.16 | 513 | 0.93 | 0.61–1.42 |
| Education | ||||||
| Less than high school | 595 | 261 | ||||
| High school or equivalent | 468 | 0.70 | 0.39–1.24 | 207 | 1.07 | 0.59–1.96 |
| Some college or greater | 1272 | 0.63 | 0.33–1.18 | 504 | 0.71 | 0.46–1.11 |
| Diabetic (Yes vs No) | ||||||
| No | 2165 | 875 | ||||
| Yes | 170 | 2.19 | 1.23–3.88 | 97 | 1.00 | 0.44–2.27 |
| Exposed to Firearm Noise | ||||||
| No | 2236 | 895 | ||||
| Yes | 99 | 0.57 | 0.21–1.54 | 77 | 1.04 | 0.44–2.43 |
| Exposed to Loud Occupational Noise | ||||||
| No | 1786 | 629 | ||||
| Yes | 549 | 0.91 | 0.63–1.32 | 343 | 2.30 | 1.45–3.64 |
| Ln Cotinine Level (ng/mL)2 | 2335 | 1.14 | 1.02–1.29 | 972 | 1.30 | 1.10–1.54 |
CI=confidence interval
Odds ratio and confidence interval are for a 1 year increment
Odds ratio and confidence interval are for a 1 log unit increase
SHS and hearing loss
SHS exposure was significantly associated with increased risk of age-adjusted hearing loss for low-/mid-frequencies (Adjusted Odds Ratio (AOR) = 1.14; 95% CI = 1.02-1.28 for never smokers and 1.30; 1.10-1.54 for former smokers) and high-frequencies (AOR 1.40; (96% CI 1.22-1.81 for former smokers), after adjusting for all potential confounders. The Figure illustrates the probability of hearing impairment as a function of cotinine level for a former smoker and never smoker, after adjusting for age, race/ethnicity, gender, diabetes, loss due to firearm use, and loss due to occupational noise exposure. The graph showed very little increase in hearing loss risk as a function of SHS exposure levels despite a significant AOR for low-/mid-frequencies and a near significant effect for high-frequency hearing loss. However, for former smokers, a greater probability of hearing loss was associated with increased cotinine levels. There were no notable differences in the association between hearing loss and SHS in analyses stratified by age-group or sex. There was no statistically significant relationship between number of years smoked, pack-years, or years since quitting and hearing loss.
Figure 1.
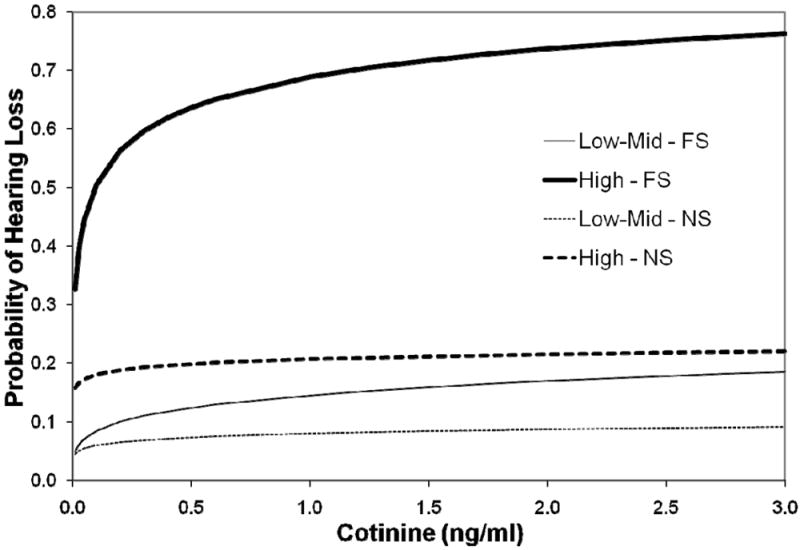
Probability of low-mid frequency and high frequency hearing impairment as a function of cotinine level for an average former smoker and never smoker adjusted for age, race/ethnicity, gender, diabetes, loss due to firearms use, and loss due to occupational noise.
DISCUSSION
In this population-based study, we found SHS to be associated with increased hearing loss among former smokers. The dramatic effects for former smokers raise the possibility that continued SHS exposure in this group, even at the relatively low levels as documented in the Figure, may continue a pathogenic process leading to the progression of high-frequency hearing loss possibly initiated when they were active smokers. This finding is even more intriguing given that even though current smoking has been shown to be associated with hearing loss in numerous studies,7-12 post-hoc analyses conducting using NHANES data revealed no increased risk of hearing loss among former smokers relative to never smokers (results not shown). These results are consistent with one previously published report.7 However, among reported never smokers, the association with SHS was not as strong. Additional epidemiologic research and animal studies will be needed in order to confirm our findings and to explore patho-physiologic mechanisms which could explain such an association. Regardless, 65% of the working US population is potentially exposed to SHS in the workplace,21 and over 29 million US adults suffer from hearing loss.1 Thus, our finding that SHS exposure is associated with the risk of hearing loss among former smokers and never smokers is of clear public health significance.
Possible Pathophysiologic Mechanisms
Several possible mechanisms may account for the relationship between smoking and hearing loss. Smoking has been reported to be both a direct ototoxic (nicotine effect) and as an inducer of ischemia in the cochlea through production of carboxyhemoglobin, vasospasm, increased blood viscosity, and its action in relation to blood vessel arteriosclerosis.22 However, these exposures may also interact with other ototoxic exposures such as noise and a variety of chemicals leading to synergistic adverse effects on the auditory system.23,24 Furthermore, one recent study reported smokers and former smokers with genetic variability in the cochlear antioxidant system (GSTM1 deletion) were at increased risk for noise-induced hearing loss than for never smokers, raising the possibility that select population sub-groups may be more vulnerable to the pathogenic effects of tobacco smoke exposure on the auditory system.23 Animal studies which systematically examine the otologic effects of SHS exposure are needed, yet there has not been any recent studies on this topic in recent years, with most research occurring decades earlier.25 Future investigators may consider studies which mimic ‘smoking’ conditions, followed by continued low-level exposures versus a control group of animals which live in smoke-free environments in order to further study potential pathophysiologic processes leading to hearing loss.
STRENGTHS AND LIMITATIONS
This is the only study to assess using nationally representative data the association between SHS and hearing loss, using a well-validated biomarker for secondhand exposure among US adults. In addition, the large sample size of the study allowed for high statistical power even after performing analyses in non-smokers stratified by former smoking history. Despite the strengths, there are limitations that should be noted which includes the cross-sectional design of the NHANES, which does not allow for causal inferences. In addition, there may be misclassification of SHS given that exposure estimates are based on serum cotinine levels which has a half life of 16-18 hours. A more accurate determination of SHS exposure would require repeat measurements of serum cotinine over a period of several days or the use of hair nicotine assays which reflect longer-term cumulative exposure. History of SHS exposure is not assessed in the NHANES; therefore, an estimate of cumulative or long term SHS is not possible. In an attempt to measure long term exposure to SHS, we conducted post-hoc analyses adding an indicator of the presence of household smoking, assuming that if an individual is exposed in the home, it is likely this exposure had occurred for a number of years. The prevalence of such exposure was less than 7% in both former and never smokers and this variable was not predictive of hearing loss when included in any of our multivariable models.
CONCLUSIONS
Although previous studies have reported the link between active smoking and increased risk of hearing loss,7-12 this study found significantly increased adjusted odds for hearing loss by former smokers for both low-/mid- and high-frequency hearing loss. Furthermore, never smokers exposed to SHS had increased risk of low-frequency hearing loss. As Figure 1 illustrates, the toxic threshold exposure level, in terms of serum cotinine levels, is extremely low. Although an active smoker is personally responsible for his/her own toxic exposures, involuntary exposures via SHS may also place never smokers and former smokers at increased risk for hearing loss. Furthermore, although several studies suggest a synergistic effect between active smoking and risk for noise –induced hearing loss,9, 11 further research is required to determine whether SHS exposure potentiates the effect of noise exposure and aging on hearing. If this finding is independently confirmed by other researchers then hearing loss can be added to the growing list of health consequences associated with exposure to SHS. 26,27 However, longitudinal studies are needed that assess, in a comprehensive fashion, all potential sources of SHS exposure (e.g., lifetime histories, including prenatal exposures) 28 as well as repeat assessment of cotinine and/or longer exposure biomarkers such as hair nicotine.29 Regardless, given the well documented toxic effects of SHS exposure, policy makers and employers should continue their work toward the development of policies to ban and/or prevent SHS exposure which can be applied in a variety of settings including the workplace, the community, and individual homes.30 Finally, the Audiologist’s role should be to advise patients that no level of active smoking or SHS exposure should be considered “safe”, and help to lower the burden of tobacco use by educating and advising their patients regarding the benefits of smoking cessation on hearing preservation.
Acknowledgments
This work was funded in part by grants from the Flight Attendant Medical Research Institute (FAMRI) and from the National Institute of Occupational Safety and Health (NIOSH) [R01 OH03915]. The authors would like to thank Dr. Lora Fleming, Mr. Alberto Caban-Martinez, Dr. John E. Lewis, Dr. William LeBlanc and Dr. Kathryn McCollister for providing assistance in interpretation of analytical data and critical revisions of the manuscript for important intellectual content.
Drs. Fabry, Arheart and Lee had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the analyses. The study concept and design was developed by Drs. Lee, Fabry and Arheart. The acquisition of the public-use data files was accomplished by Dr. LeBlanc and Dr. Arheart. Analysis and interpretation of data were conducted by Drs. Fabry, Arheart, Lee, Lewis, Serdar and Davila and by Mr. Caban-Martinez and Mr. Bandiera. Drafts of the manuscript were undertaken by Drs. Fabry, Lee, Arheart, Dietz, Davila and Serdar and by Mr. Bandiera. Critical revision of the manuscript for important intellectual content by Drs. Fabry, Lee, Arheart, Dietz and Serdar, Mr. Caban-Martinez, Dr. Davila, and Mr. Bandiera. Dr. Lee and Dr. Fleming obtained funding and provided study supervision and direction.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest
ETHICS APPROVAL
This study was approved as exempt by the University of Miami Institutional Review Board for human subjects research.
LICENSE STATEMENT
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in Tobacco Control and any other BMJPGL products to exploit all subsidiary rights, as set out in our licence. http://group.bmj.com/products/journals/instructions-for-authors/licence-forms
References
- 1.Agrawal Y, Platz EA, Niparko JK. Prevalance of hearing loss and differences by demographic characteristics among US adults. JAMA. 2008;168(14):1522–1530. doi: 10.1001/archinte.168.14.1522. [DOI] [PubMed] [Google Scholar]
- 2.Chia E-M, Wang JJ, Rochtchina E, Cumming RR, Newall P, Mitchell P. Hearing Impairment and Health-Related Quality of Life: The Blue Mountains Hearing Study. Ear and Hearing. 2007;28:187–195. doi: 10.1097/AUD.0b013e31803126b6. [DOI] [PubMed] [Google Scholar]
- 3.Zwerling C, Sprince NL, Davis CS, Whitten PS, Wallace RR, Heeringa SG. Occupational injuries among older workers with disabilities: a prospective cohort study of the Health and Retirement Survey, 1992 to 1994. Am J Public Health. 1998 Nov;88(11):1691–1695. doi: 10.2105/ajph.88.11.1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mann JR, Zhou L, McKee M, McDermott S. Children with Hearing Loss and Increased Risk of Injury. Annals of Family Medicine. 2007;5:528–533. doi: 10.1370/afm.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohr PE, Feldman JJ, Dunbar JL, McConkey-Robbins A, Niparko JK, Rittenhouse RK, Skinner MW. The societal costs of severe to profouond hearing loss in the United States. International Journal of Technology Assessment in Health Care. 2000;16(4):1120–1135. doi: 10.1017/s0266462300103162. [DOI] [PubMed] [Google Scholar]
- 6.Muhr P, Mansson B, Hellstrom PA. A study of hearing changes among military conscripts in the Swedish Army. Int J Audiology. 2006;45:247–151. doi: 10.1080/14992020500190052. [DOI] [PubMed] [Google Scholar]
- 7.Cruickshanks KJ, Klein R, Klein BE, Wiley TL, Nondahl DM, Tweed TS. Cigarette smoking and hearing loss: The Epidemiology of hearing loss study. JAMA. 1998;279(21):1715–1719. doi: 10.1001/jama.279.21.1715. [DOI] [PubMed] [Google Scholar]
- 8.Stark J, Toppila E, Pyyko I. Smoking as a risk factor in sensory neural hearing loss among workers exposed to occupational noise. Acta Oto-Laryngologica. 1999;119(3):302–305. doi: 10.1080/00016489950181288. [DOI] [PubMed] [Google Scholar]
- 9.Agrawal Y, Platz EA, Niparko JK. Risk Factors for Hearing Loss in Adults: Data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otology and Neurotology. 2009;30:139–145. doi: 10.1097/MAO.0b013e318192483c. [DOI] [PubMed] [Google Scholar]
- 10.Carlsson P-I, Fransen E, Stenberg E, Bondeson M-L. The influence of genetic factors, smoking and cardiovascular diseases on human noise susceptibility. Audiological Medicine. 2007;5:82–91. [Google Scholar]
- 11.Ferritite S, Santana V. Joint Effects of Smoking, Noise Exposure, and Age on Hearing Loss. Occupational Medicine. 2005;55:48–53. doi: 10.1093/occmed/kqi002. [DOI] [PubMed] [Google Scholar]
- 12.Gopinath B, Flood VM, McMahon CM, Burlutsky G, Smith W, Mitchell P. The effects of smoking and alcohol consumption on age-related hearing loss: The blue mountains hearing study. Ear Hear. 2010:277–282. doi: 10.1097/AUD.0b013e3181c8e902. [DOI] [PubMed] [Google Scholar]
- 13.National Center for Health Statistics. About the National Health and Nutrition Examination Survey – An Introduction. [Tuesday, September 1, 2009]; Available at http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 14.National Center for Health Statistics. National Health and Nutrition Examination Survey Response Rates & CPS Population Totals. [Tuesday, September 1, 2009]; Available at http://www.cdc.gov/nchs/nhanes/nhanes_cps_totals.htm.
- 15.Benowitz NL. Cotinine as a biomarker of environmental tobacco smoke exposure. Epidemiolo Rev. 1996;18(2):188–204. doi: 10.1093/oxfordjournals.epirev.a017925. [DOI] [PubMed] [Google Scholar]
- 16.Benowitz NL, Bernert JT, Caraballo RS, Holiday DB, Wang J. Optimal serum cotinine levels for distinguishing cigarette smokers and nonsmokers within different racial/ethnic groups in the United States Between 1999 and 2004. Am Journal of Epidemiology. 2009;169(2):236–248. doi: 10.1093/aje/kwn301. [DOI] [PubMed] [Google Scholar]
- 17.Clark JD, 3rd, Wilkinson JD, LeBlanc WG, et al. Inflammatory markers and secondhand tobacco smoke exposure among U.S. workers. Am J Ind Med. 2008 Aug;51(8):626–32. doi: 10.1002/ajim.20591. [DOI] [PubMed] [Google Scholar]
- 18.Bainbridge KE, Hoffman HJ, Cowie CC. Diabetes and Hearing Impairment in the United States: Audiometric Evidence from the National Health and Nutrition Examination Survey, 1999 to 2004. Annals of Internal Medicine. 2008;149(1):1–10. doi: 10.7326/0003-4819-149-1-200807010-00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gelfand SA. Essentials of Audiology. 2. New York: Thieme; 2001. [Google Scholar]
- 20.SAS Institute Inc. SAS 9.2 System. Cary, NC: SAS Institute Inc.; [Google Scholar]
- 21.ANRF. Summary of 100% smokefree state laws and population protected by state and local laws. American Non-Smokers’ Rights Foundation. [August 23, 2009];2008 July 1; http:\\www.no-smoke.org/pdf/SummaryUSPopList.pdf.
- 22.Barone JA, Peters JM, Garabrant DH, Bernstein L, Krebsbach R. Smoking as a risk factor in noise induced hearing loss. J Occup Med. 1987;29:741–745. [PubMed] [Google Scholar]
- 23.Carlsson P-I, Fransen E, Stenberg E, Bondeson M-L. The influence of genetic factors, smoking and cardiovascular diseases on human noise susceptibility. Audiological Medicine. 2007;5:82–91. [Google Scholar]
- 24.Fechter LD. Promotion of noise-induced hearing loss by chemical contaminants. J Toxicol Environ Health A. 2004;67:727–740. doi: 10.1080/15287390490428206. [DOI] [PubMed] [Google Scholar]
- 25.Maffei G, Miani P. Experimental tobacco poisoning. Resultant structural modifications of the cochlea and tuba acustica. Arch Otolaryngol. 1962;75:386–396. doi: 10.1001/archotol.1962.00740040397002. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. The Health Effects of Environmental Tobacco Smoke. Maryland: Centers for Disease Control Center for Health Promotion and Education Office on Smoking and Health Rockville U.S. Department Of Health And Human Services, Public Health Service; 1986. The Health Consequences of Involuntary Smoking: A Report of the Surgeon General. [Google Scholar]
- 27.United States Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services. Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health; 2006. Introductions and conclusions; pp. 1–26. [PubMed] [Google Scholar]
- 28.McCartney JS, Fried PA, Watkinson B. Central auditory processing in school-age children prenatally exposed to cigarette smoke. Neurotoxicol Teratol. 1994;16:269–276. doi: 10.1016/0892-0362(94)90048-5. [DOI] [PubMed] [Google Scholar]
- 29.Al-Delaimy WK. Hair as a biomarker for exposure to tobacco smoke. Tob Control. 2002;11:176–182. doi: 10.1136/tc.11.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eriksen MP, Cerak RL. The diffusion and impact of clean indoor air laws. Annu Rev Public Health. 2008;29:171–85. doi: 10.1146/annurev.publhealth.29.020907.090920. [DOI] [PubMed] [Google Scholar]


