Abstract
Objective
To quantify the repeatability and reproducibility of fetal cardiac ventricular volumes obtained utilizing STIC and VOCAL™.
Methods
A technique was developed to compute ventricular volumes using the sub-feature: Contour Finder: Trace. Twenty-five normal pregnancies were evaluated for the following: (1) to compare the coefficient of variation (CV) in ventricular volumes between 15° and 30° rotation; (2) to compare the CV between three methods of quantifying ventricular volumes: (a) Manual Trace (b) Inversion Mode and (c) Contour Finder: Trace; and (3) to determine repeatability by calculating agreement and reliability of ventricular volumes when each STIC was measured twice by 3 observers. Reproducibility was assessed by obtaining two STICs from each of 44 normal pregnancies. For each STIC, 2 ventricular volume calculations were performed, and agreement and reliability were evaluated. Additionally, measurement error was examined.
Results
(1) Agreement was better with 15° rotation than 30° (15°: 3.6%, 95% CI: 3.0 – 4.2 versus 30°: 7.1%, 95% CI: 5.8 – 8.6; p<0.001); (2) ventricular volumes obtained with Contour Finder: Trace had better agreement than those obtained using either Inversion Mode (Contour Finder: Trace: 3.6%, 95% CI 3.0 – 4.2 versus Inversion Mode: 6.0%, 95% CI 4.9 – 7.2; p < 0.001) or Manual Trace (10.5%, 95% CI 8.7 – 12.5; p < 0.001); (3) ventricular volumes were repeatable with good agreement and excellent reliability for both intra-observer and inter-observer measurements; and 4) ventricular volumes were reproducible with negligible difference in agreement and good reliability. In addition, bias between STIC acquisitions was minimal (<1%; mean percent difference −0.4%, 95% limits of agreement: −5.4 – 5.9).
Conclusions
Fetal echocardiography utilizing STIC and VOCAL allows repeatable and reproducible calculation of ventricular volumes with the sub-feature Contour Finder: Trace.
Keywords: Four-dimensional ultrasonography, three-dimensional echocardiography, fetal echocardiography, fetus, Contour-Finder, ventricular volume, cardiac function, ultrasonography, inversion mode
Introduction
Three-dimensional (3D)/4-dimensional (4D) ultrasonography can be used to interrogate the fetal heart and obtain information about cardiac function. Thus far, three methods have been reported which employ 3D/4D ultrasonography in evaluating fetal ventricular volume,1-5 stroke volume,2-6 cardiac output,5,6 and ejection fraction.1,2,5 These include: (1) Manual Trace of the ventricular boundaries with Spatio-Temporal Image Correlation (STIC)4,6 (GE Voluson 730 Expert and E-8; GE Healthcare, Kretztechnik, Zipf, Austria; and iU-22; Philips Healthcare, Bothell, WA) or SONOReal (Biomedicom, Jerusalem, Israel);1 (2) calculation of volumes by the modified Simpson’s rule either with STIC5 or with the aid of computer generated 3D reconstruction (TomTec Imaging Systems, Munich, Germany);3 and (3) utilization of a combination of the post processing applications Virtual Organ Computed-aided AnaLysis (VOCAL) and Inversion mode.2
In previous reports, investigators examined the repeatability of each technique using different study designs and analysis methods.1-6 Yet Bartlett and Frost described in detail the approach to assess repeatability (measured variation under identical conditions) and reproducibility (variation under changing conditions).7 Measurements of agreement, such as the coefficient of variation (CV) and calculation of reliability, quantified by the intra-class correlation (ICC), allow statistical evaluation of each. Messing et al.2 as well as Rizzo et al.4 evaluated reliability using ICC, Esh-Broder et al.1 and Uittenborgaard et al.5 quantified agreement, as measured by the CV, while Molina et al.6 and Meyer-Wittkopf et al.3 utilized other measures of repeatability. The results are difficult to interpret because of different study designs and analysis techniques. Moreover, since the assessments of repeatability did not include examination of both agreement and reliability, as recommended by Bartlett and Frost,7 a comprehensive understanding of the repeatability of 3D/4D ultrasonography remains incomplete. Furthermore, there is a paucity of data regarding the reproducibility of these techniques. The objective of this study was to quantify the repeatability and reproducibility in the computation of fetal cardiac ventricular volumes obtained utilizing STIC and VOCAL.
Materials and Methods
Examination technique
Ultrasound examinations were performed using a system with STIC capability (Voluson 730 Expert and E8) utilizing a motorized curved array transabdominal transducer (2-5 or 4-8 MHz). A transverse view of the fetal chest at the level of the four chamber view was obtained from which STIC data sets were acquired. The acquisition time was 10 seconds with a sweep angle that was sufficient to encompass the fetal cardiac structures (25 to 35 degrees). Color Doppler ultrasonography was not utilized during the acquisition process. Adequate cardiac data sets were accepted for post-processing if acoustic shadowing (signal loss in the sound path secondary to echogenic structures), dropout (signal loss in the sound path without intervening structures), and motion artifact were absent.
Analysis was performed offline (4D View versions 5.0 – 7.0, GE Healthcare, Milwaukee, WI) in a standardized manner. In the A plane of the multi-planar display, the fetal heart was re-oriented such that the left ventricle was located on the left side of the screen with the apex of the heart directed up. The interventricular septum was then rotated to 90° in both the A plane and the C plane. The atrioventricular (AV) valves were located by scrolling from front to back in the A plane. The image was then optimized by selecting chroma color 1 (Sepia) and SRI 5. After the image brightness and contrast settings were optimized, end systole and end diastole were identified by scrolling through each frame and identifying the image preceding atrioventricular (AV) valve opening (end systole) and following AV valve closure (end diastole).2,4-6
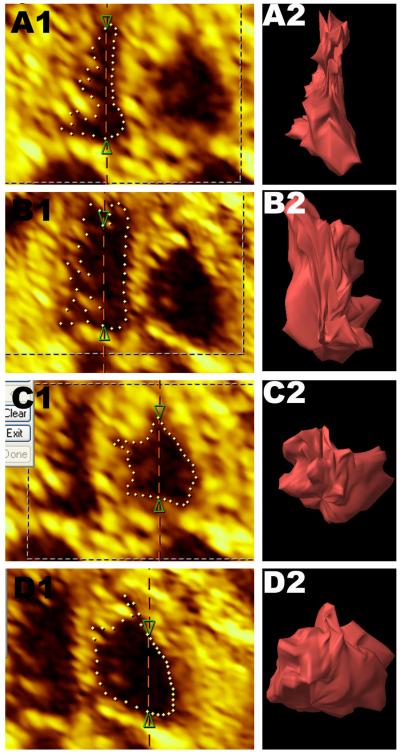
Cardiac ventricular volumes were calculated in a semi-automated fashion utilizing VOCAL. VOCAL II was selected and the Contour Finder: Trace option was utilized with 15° of rotation and a sensitivity of 1 (default = 5). The image was enlarged and the reference dot repositioned into the ventricle of interest. Because of the complex geometry of the ventricles, the location of the reference dot within the ventricle was selected to meet the software requirement that the contour only cross the rotation line twice. With these selections, 12 rotational steps were made, and a volume was computed. Data sets were accepted for analysis if the ventricular septum, ventricular walls, and AV valves were visible throughout each rotational step (Figure 1). To perform the technique Manual Trace, offline analysis was altered by choosing Manual after VOCAL II was selected. The technique Inversion Mode was performed by first utilizing Manual Trace to trace the contour of the ventricle including the myocardium. Next, the post-processing application Inversion Mode was selected and the ventricular volume was calculated by adjusting the threshold volume such that only black voxels with in the ventricle were included when rendered (Figure 2).
Figure 1.
Selected VOCAL rotational steps utilizing Contour Finder: Trace for each ventricle in end systole and end diastole (A: Left ventricle in systole; B: Left ventricle in diastole; C: Right ventricle in systole; D: Right ventricle in diastole) at the level of the four chamber view (A1-D1) and the rendered image (A2-D2).
Figure 2.
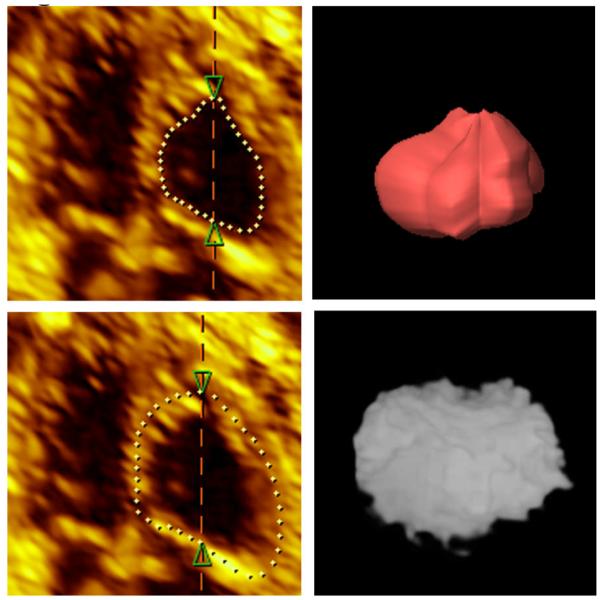
VOCAL rotational step (left) and rendered image (right) utilizing Manual Trace (top) and Inversion Mode (bottom) for the right ventricle in diastole.
How much variation is present when cardiac data sets are collected and evaluated?
A series of experiments were constructed to evaluate the variability in fetal ventricular volume measurements. Singleton pregnancies between 19 and 40 weeks gestation with sonographic dating of pregnancy performed prior to 24 weeks were eligible for study. Patients in our antenatal clinic were assessed by 2 sonologists and were excluded if medical complication of pregnancy, fetal anomaly, abnormal fetal growth, or suboptimal fetal position were present. All women provided written informed consent prior to sonographic examination. Participation was approved by the Institutional Review Boards of Wayne State University and the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
To assess the repeatability of ventricular volume measurements, 2 enrollment periods were utilized. Ten patients were selected for proof of concept followed by an additional 15 patients. Twenty five cardiac data sets were evaluated for the following comparisons. First, the CV in ventricular volume calculations was compared by varying the degrees of rotation from 15° (12 rotational steps) to 30° (6 rotational steps). A single sonologist utilizing Contour Finder: Trace obtained two measurements per STIC data set for each technique. Second, 3 methods which quantify cardiac ventricular volumes from STIC data sets utilizing VOCAL were evaluated by comparing the CV obtained with Contour Finder: Trace, Inversion Mode,2 and Manual Trace,4 each with 15° rotation. A single sonologist obtained two measurements per STIC data set per technique. Third, the repeatability of volume measurements obtained with Contour Finder: Trace was evaluated. Each data set was independently measured twice by three sonologists. Agreement was assessed for each observer by computing the CV, and reliability for both intraobserver and interobserver calculations was assessed utilizing ICC. The technique was considered repeatable if there was good agreement (CV < 10%) as well as good reliability (ICC > 0.90).8,9
The reproducibility of ventricular volume measurements utilizing STIC and VOCAL™ with Contour Finder: Trace was assessed by performing a method comparison study,7 which consisted of 44 consecutive pregnancies. A single sonologist collected 2 data sets on the same patient during a period of time not greater than 30 minutes. A second sonologist calculated ventricular volumes, utilizing Contour Finder: Trace, twice for each STIC data set. Agreement and reliability were evaluated by computing the CV and ICC, respectively. The technique was considered reproducible if there was negligible difference (<1%) in agreement between data sets as well as good reliability (ICC >0.90). Measurement error introduced in STIC acquisition was examined by constructing a Bland-Altman plot utilizing the technique described by Bartlett and Frost.7
Study population
A pilot study of 10 cardiac data sets was used to test proof of concept, which provided statistically significant results. The final sample size of 25 was arbitrarily selected for the method comparison study because it provided a larger population relative to the available literature.1,2,4,5 Planned comparisons for the reproducibility study included comparisons between data sets as well as between the left and right ventricle in systole and diastole, each of which was made in a paired manner. Preliminary data suggested that the difference in the mean CV between the left and right sides was 0.2% with a standard deviation no greater than 1. To achieve a power of 80% at this degree of difference in the mean CV with an alpha of 0.05, a sample size of 180 patients would be required. However, if a difference in the mean CV of 0.5% or greater is considered, it would better reflect a clinically relevant endpoint demonstrating no difference at a CV of 1%, or negligible variation. At this level of difference in the mean CV with the same standard deviation, a sample size of 33 would be required to achieve a power of 80%. Preliminary results suggest a 15% rate of rejection upon rendering. Additionally, the requirement of 2 STIC volumes decreases the probability of successful acquisition from 85% to 72%; therefore, to ensure that the sample size is adequate, a total of 44 patients were recruited to participate in the reproducibility study.
Statistical analysis
The Shapiro-Wilk and Kolmogorov-Smirnov tests were used to test for normal distribution. If a normal distribution was absent the data were transformed using a square root transformation. For normally distributed data, repeated measures ANOVA with Bonferroni post hoc analysis and paired t-tests were used to determine the differences of the mean among groups, and the Pearson correlation coefficient was utilized to assess correlations. Nonparametric statistics were employed if the data was not normally distributed, and the Spearman rank correlation coefficient was utilized to assess correlations. Repeatability and reproducibility were assessed between and among observers by examining the CV and ICC. Agreement was considered good if the mean CV was less than 10% and negligible if the mean CV was less than 1%; additionally, reliability was considered acceptable if the ICC was greater than 0.80, good if greater than 0.90, and excellent if greater than 0.95. Bias was considered to be absent and measurement error variance stable if there was no correlation between measurement differences and measurement means utilizing the technique described by Bartlett and Frost.7 For all comparisons, P <.05 was considered statistically significant. Statistical analyses were performed with SPSS package version 14 (SPSS Inc, Chicago IL, USA).
Results
Volumes Produced With VOCAL and Contour Finder: Trace Using 15° Rotation Provide a High Degree of Agreement Compared to Other Techniques
Twenty five normal fetuses were evaluated at a median gestational age of 26.9 weeks (range, 20.0 – 35.4). Patients were assessed for eligibility during 2 enrollment periods. During the first enrollment period, 25 patients were evaluated and 15 were excluded (medical complication of pregnancy [n=11], abnormal fetal growth [n=1], and suboptimal fetal position [n=3]). In the second enrolment period, 27 patients were evaluated and 12 were excluded (medical complication of pregnancy [n=7], fetal anomaly [n=1], abnormal fetal growth [n=2], and suboptimal fetal position [n=2]). Significantly improved agreement, as measured by the mean CV, was found using 15° compared to 30° rotation (15°: 3.6% versus 30°: 7.1%; P<.001; Table 1a). This effect remained significant for the left ventricle in systole (15°: 4.8% versus 30°: 9.1%; P<.001; Table 1a) and diastole (15°: 2.5% versus 30°: 6.5%; P<.05; Table 1a), as well as for the right ventricle in systole (15°: 4.0% versus 30°: 7.5%; P<.05; Table 1a).
Table 1A.
Comparison of Ventricular Volume Calculations Using VOCAL™ With the Subfeature Contour Finder: Trace at Rotations of 15° and 30°
| 15° | 30° | P | |
|---|---|---|---|
| Overall | 3.6 (3.0 – 4.2) | 7.1 (5.8 – 8.6) | <0.001* |
| LVS | 4.8 (3.6 – 6.3) | 9.1 (6.2 – 12.5) | <0.001* |
| LVD | 2.5 (1.6 – 3.5) | 6.5 (3.9 – 9.7) | <0.05* |
| RVS | 4.0 (2.5 – 5.7) | 7.5 (4.7 – 10.8) | <0.05* |
| RVD | 3.3 (2.2 – 4.8) | 5.8 (3.4 – 8.8) | ns* |
Values of agreement are expressed as mean percent CV (95% confidence interval [CI])
RVS – right ventricle in systole
RVD – right ventricle in diastole
LVS – left ventricle in systole
LVD – left ventricle in diastole
paired t-test
Next, the mean CV’s obtained from the following techniques with 15° rotation were compared: Contour Finder: Trace, Inversion Mode, and Manual Trace. There was a significant difference between methods (F=1230.2, P < .001) with Contour Finder: Trace providing a lower mean CV than either Inversion Mode (Contour Finder: Trace: 3.6%, versus Inversion Mode: 6.0%; P <.001; Table 1b) or Manual Trace (10.5%; P <.001; Table 1b).
Table 1B.
Comparison of 3 Different Techniques for Calculating Fetal Cardiac Ventricular Volumes From STIC Data Sets Utilizing VOCAL
| Manual Trace 15° | Inversion Mode 15° | P | Contour Finder 15° | P | |
|---|---|---|---|---|---|
| Overall | 10.5 (8.7 – 12.5) | 6.0 (4.9 – 7.2) | <0.001* | 3.6 (3.0 – 4.2) | <0.001* |
| LVS | 15.2 (10.6 – 20.8) | 6.1 (3.2 – 9.9) | <0.01* | 4.8 (3.6 – 6.3) | <0.001*† |
| LVD | 9.0 (7.5 – 11.5) | 6.5 (4.7 – 8.5) | ns* | 2.5 (1.6 – 3.5) | <0.01* |
| RVS | 13.1 (8.6 – 18.6) | 5.9 (3.8 – 8.5) | <0.05* | 4.0 (2.5 – 5.7) | <0.001*† |
| RVD | 6.1 (3.7 – 8.9) | 5.6 (3.9 – 7.6) | ns* | 3.3 (2.2 – 4.8) | ns* |
Values of agreement are expressed as mean percent CV (95% CI). Abbreviations are as in Table 1A.
Repeated measures analysis of variance with post hoc analysis
Significance only for Contour Finder versus Manual Trace
For left ventricular volumes, there were significantly different mean CVs in systole (F=290.3, P < .001). Post hoc analysis indicated that Contour Finder: Trace had a lower mean CV than Manual Trace (Contour Finder: Trace: 4.8% versus Manual Trace: 15.2%; P <.001; Table 1b). Additionally, Inversion Mode also had a lower mean CV than Manual Trace (Inversion Mode: 6.1%; versus Manual Trace: 15.2%; P <.01; Table 1b). Furthermore, significantly different mean CVs were found between techniques for the left ventricle in diastole (F=484.5, P <.001). Post hoc analysis demonstrated that Contour Finder: Trace had a significantly lower mean CV than Inversion Mode (Contour Finder: Trace: 2.5%; versus Inversion Mode: 6.5%; P <.01; Table 1b) as well as Manual Trace (9.0%; P <.01; Table 1b).
For right ventricular volumes, the mean CVs were significantly different between techniques in systole (F=433.2, P <.001). Post hoc testing indicated that Contour Finder: Trace had a lower mean CV than Manual Trace (Contour Finder: Trace: 4.0%; versus Manual Trace:13.1%; P <.001; Table 1b). In addition, Inversion Mode also had a lower mean CV than Manual Trace (Inversion Mode: 5.9%; versus Manual Trace:13.1%; P <.05; Table 1b). When right ventricular volumes in diastole were computed, the mean CVs were significantly different between techniques (F=258.2, P <.001); however, post hoc testing did not reveal significance, although there was a trend towards a lower CV for Contour Finder: Trace compared to both Inversion Mode and Manual Trace (Table 1b).
Calculating Ventricular Volumes With STIC and VOCAL™ Utilizing Contour Finder: Trace and 15° Rotation is Repeatable and Reproducible
Repeatability
Agreement for each of 3 observers, as measured by the mean CV, was less than 10% using the same 25 STIC data sets (Observer 1: 2.8%; Observer 2: 3.6%; Observer 3: 6.3%; Table 2). There was no significant correlation between CV and gestational age at the time of STIC acquisition (Observer 1: R = 0.06, P = 0.54; Observer 2: R = −0.01, P = 0.95; Observer 3: R = −0.05, P = 0.60). Intra-observer reliability was excellent with ICCs greater than 0.95 for each observer (Observer 1: 0.998; Observer 2: 0.996; Observer 3: 0.990; Table 2). Additionally, interobserver reliability was also excellent with an ICC > 0.95 (ICC: 0.96, 95% CI 0.94 – 0.97; Table 2).
Table 2.
Repeatability of Ventricular Volumes Utilizing VOCAL With the Subfeature Contour Finder: Trace
| Observer 1 (n=25) | Observer 2 (n=25) | Observer 3 (n=25) | |
|---|---|---|---|
| Agreement* | 2.8% ( 2.3 – 3.3) | 3.6% (3.0 – 4.3) | 6.3% ( 5.2 – 7.6) |
| Intra-observer reliability# |
0.998 (0.996 – 0.998) | 0.996% (0.994 – 0.997) | 0.990% ( 0.985 – 0.993) |
| Inter-observer reliability# |
0.96 (0.94 – 0.97) | ||
Agreement expressed as mean percent CV (95% CI)
Reliability expressed as ICC (95% CI)
Reproducibility
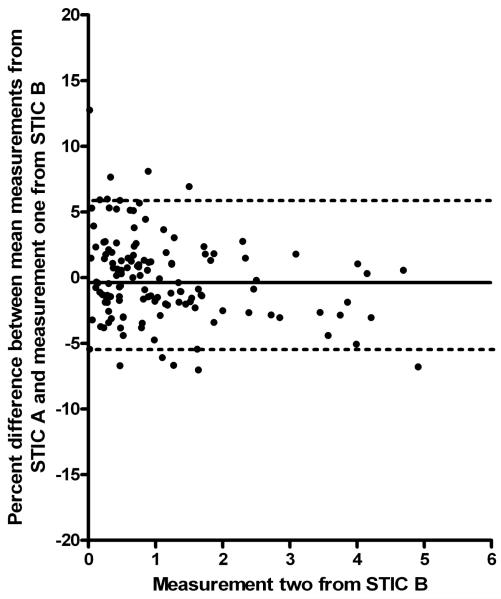
Forty-four normal fetuses were evaluated at a median gestational age of 29.1 weeks (range, 18.0 – 36.6). Thirty-three fetuses (75%) had two (A and B) successful STIC acquisitions. There was no difference in the agreement (mean CV) between STIC data sets (STIC A: 4.0% versus STIC B: 3.8%; P = .64; Table 3). With the same STIC data set, intra-STIC reliability was excellent with ICCs greater than 0.95 for each STIC (STIC A: 0.998; STIC B: 0.997; Table 3). Additionally, inter-STIC reliability was good with ICCs > 0.90 (Table 3). A Bland-Altman plot comparing the percent difference between volume calculations from each STIC acquisition (A and B) indicated that minimal bias was introduced between acquisitions (mean percent difference −0.4%, 95% limits of agreement: −5.4 – 5.9; Figure 3). Moreover, there was no correlation between the percent difference and the second measurement from STIC B (rs=0.02, P = 0.11; Figure 3) indicating that neither the bias nor the error variance changed over the measurement range.
Table 3.
Reproducibility of Ventricular Volumes Utilizing VOCAL With the Subfeature Contour Finder: Trace
| STIC Data Set A | STIC Data Set B | |
|---|---|---|
| Agreement* | 4.0% (3.5 – 4.7) | 3.8% (3.2 – 4.6)¶ |
| Intra-observer reliability# |
0.998 (0.997 – 0.998) | 0.997 (0.996 – 0.998) |
| Inter-observer reliability# |
0.94 (0.92 – 0.96) | |
Agreement expressed as mean percent CV (95% CI)
Paired t-test not significant (t=0.47; p=ns)
Reliability expressed as ICC (95% CI)
Figure 3.
Bland – Altman plot of the bias, expressed in percent, between STIC acquisitions (Mean: −0.4%, 95% limits of agreement −5.4 – 5.9). There was no correlation between the percent difference and the second measurement from STIC B (rs=0.02, P=.11).
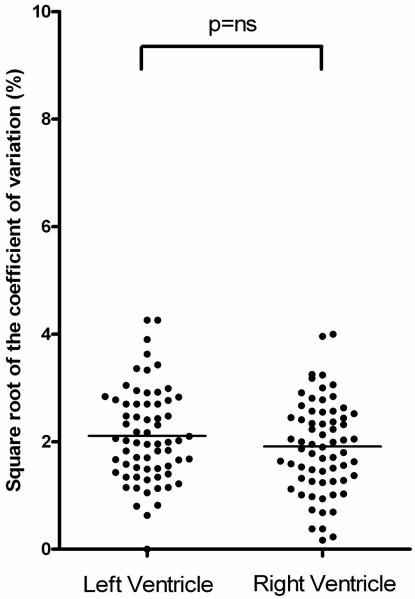
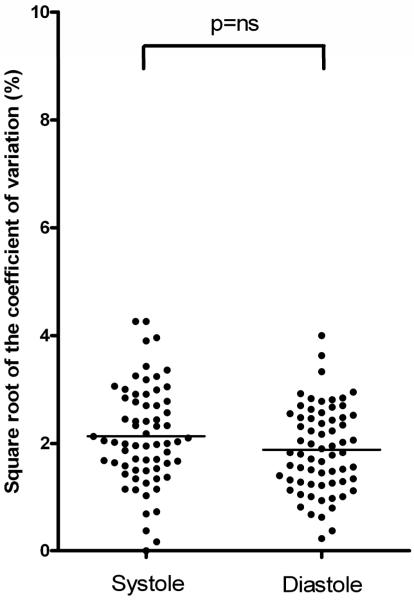
Measurement agreement between the left and right ventricle, as well as systole and diastole, was also considered. There was no significant difference in the mean CV of STIC A when the left and right ventricles were compared (Left: 4.5%; versus Right: 3.7%; P = .23; Figure 4); additionally, no significant difference was present when the mean CV of STIC A in systole was compared to diastole (Systole: 4.5%; versus Diastole: 3.5%; P = .10; Figure 5).
Figure 4.
Square root transformed CV for the left and right ventricles. There was no significant difference in the mean square root transformed CV between the left and right ventricles (Left: 4.5%, 95% CI: 3.6 – 5.4 versus. Right: 3.7%, 95% CI: 2.9 – 4.5; t=1.2, p=.23; data untransformed after comparison)
Figure 5.
Square root transformed CV for systole and diastole. There was no significant difference in the mean square root transformed CV (Systole: 4.5%, 95% CI: 3.7 – 5.6 versus. Diastole: 3.5%, 95% CI: 2.9 – 4.3; t=1.7, P = .1; data untransformed after comparison)
Last, the left and right ventricle in systole and diastole were compared between STIC data sets (A and B) to assess any specific effect on measurement agreement. Right ventricular volumes did not have significantly different mean CV’s in either systole (STIC A: 4.3%; versus STIC B: 4.3%; P = .94; Table 4) or diastole (STIC A: 3.0%; versus. STIC B: 2.8%; P = .67; Table 4). Similarly, the left ventricle did not have significantly different mean CVs in systole (STIC A: 4.8%; versus. STIC B: 6.1%; P = .24; Table 4); however, in diastole there was a significant difference between the mean CVs (STIC A: 4.1%; versus. STIC B: 2.7%; P = .04; Table 4).
Table 4.
Agreement for Each Ventricle in Systole and Diastole
| STIC Data set A* | STIC Data set B* | Difference in means |
t | p | |
|---|---|---|---|---|---|
| RVS | 4.3% (3.1 – 5.8) | 4.3% (3.0 – 5.7) | 0.01% | 0.08 | ns |
| RVD | 3.0% (2.1 – 4.1) | 2.8% (2.0 – 3.7) | 0.2% | 0.45 | ns |
| LVS | 4.8% (3.4 – 6.4) | 6.1% (3.9 – 8.8) | 1.3% | −1.19 | ns |
| LVD | 4.1% (3.1 – 5.3) | 2.7% (2.0 – 3.6) | 1.4% | 2.19 | 0.04 |
Agreement expressed as mean percent CV (95% CI). Abbreviations are as in Table 1A.
Discussion
Calculating Fetal Ventricular Volumes: STIC and VOCAL Versus 2-Dimensional Techniques
Several techniques have been described which quantitate ventricular volumes utilizing 2-dimensional fetal echocardiography. Doppler interrogation of either the AV10-12 or semilunar13-25 valves has been used in conjunction with the respective valvular diameters to produce ventricular volume estimates. A significant limitation inherent in these calculations involves quantifying the area through which blood flows, because of the necessity of measuring a diameter. In the case of the outflow tracts, the diameter of either the pulmonary or aortic valve has a good CV of less than 10% with a range from 3.6% to 8.4%;14,19,25,26 however, this diameter must be halved and then squared to quantify an area. Therefore, the variation in the calculated volume should, and indeed does, increase. Specifically, the CV is greater than 10% for both the calculated stroke volume (16%) and cardiac output (16%).26 Additionally, measurement of the atrioventricular valves in two-dimensions requires the geometric assumption that the valves are circular, an assumption that is not correct.27
Cross-sectional measurements of the left and right ventricle using either orthogonal ventricular measurments28-30 or a biplane multiple-disc method, the Simpson rule,16 have also been used to estimate ventricular volumes. These methods require one to assume that the ventricle has a conical geometry or that the ventricular endocardium is smooth, neither of which is valid.31-33 The result is a CV that exceeds 10% in the estimation of left ventricular end diastolic volume (13%) and stroke volume (14%) using the Simpson method26 and a CV greater than 30% for the estimation of left ventricular end diastolic volume (32%) and stroke volume (36%) using M-mode and the Teichholz formula.26
Fetal echocardiography utilizing 3D/4D techniques provides the sonologist with a means to minimize the effect of several technical factors. There is a dramatic reduction in the examination time required when STIC data sets are employed since acquisitions take no more than 12.5 seconds to complete.34 Furthermore, measurements are not angle dependent, and no anatomical assumptions are made in computing ventricular volumes. For these reasons, several investigations have been conducted to evaluate the utility of cardiac data sets obtained with 3D/4D techniques in calculating cardiovascular parameters.1-6
Prior to reporting fetal cardiovascular data each investigator assessed the repeatability of their technique with varying study designs and analytic methodology. Esh-Broder et al.1 noted that the mean CV of the ejection fraction in 4 patients was 16%. Myer-Wittkopf and colleagues3 examined the percentage of the mean SD of differences noting values of 9% for diastole and 11% for systole. More recently, investigators have utilized STIC and VOCAL, both of which have been validated in vitro,35,36 to assess fetal cardiovascular parameters. Messing et al.2 examined the reliability of volume estimates in 11 patients, using a combination of the post processing applications VOCAL and Inversion Mode, with ICCs of 0.98 (95% CI 0.96 – 0.99) for Intraobserver reliability and 0.96 (95% CI 0.92 – 0.98) for interobserver reliability. Similarly, Rizzo and colleagues4 examined ICCs for stroke volume estimates, obtained with VOCAL and Manual Trace, in 10 patients with excellent reliability (Intraobserver: 0.98, 95% CI 0.92 – 0.99 and Interobserver: 0.95, 95% CI 0.88 – 0.97). Molina et al6 reported that the mean percent difference of stroke volumes measured in 50 patients by a single observer with VOCAL and Manual Trace was −2.1% (95% CI: −18.4 – 14.2) for the left ventricle and −0.8% (95% CI: −16.4 – 18.0) for the right ventricle. Most recently, Uittenborgaard et al5 utilized STIC with a combination of manually traced ventricular boarders and the Simpson method to provide volume calculations. They estimated that the CV for stroke volumes obtained by a single observer from 12 fetuses was 13.7%. The results are difficult to interpret because of the varied study designs and analytic techniques. Furthermore, a comprehensive understanding of ventricular volume repeatability is limited because previous work has not included an assessment of both agreement and reliability, as recommended by Bartlett and Frost.7 Lastly, the reproducibility of ventricular volume measurements remains unaddressed.
The use of Contour Finder: Trace in Calculating Fetal Ventricular Volumes
Similar to other multidimensional applications,37-41 we have described a standardized technique to orient and analyze fetal cardiac data sets using the sub-feature Contour Finder: Trace from the VOCAL application. In this setting, a consistent approach allows an individual to become accustomed to the contours of the ventricle since they are presented in the same orientation with each rotation. Additionally, the feature Contour Finder: Trace employs a sophisticated algorithm, which helps to find the contour of the ventricle as the mouse is moved along the ventricular wall. While it is likely that combining the standardized orientation of data sets with the consistency of a computer algorithm will increase the repeatability and reproducibility of volume measurements, the use of this technology has not been explored; therefore, we sought to examine the repeatability of ventricular volume measurements utilizing VOCAL and Contour Finder: Trace with 15° rotation by comparing this technique to others available in the literature.2,4,6
Uniform agreement is lacking in literature evaluating VOCAL techniques concerning the number of rotational steps used to provide cardiac ventricular volume calculations. Messing and colleagues2 as well as Rizzo and colleagues4 have reported techniques utilizing 15° rotation (12 steps) while Molina et al6 reported results using 30° rotation (6 steps). We found significantly better agreement with 15° rotation compared to 30° using VOCAL with Contour Finder: Trace; an effect likely due to the complicated geometry of the fetal ventricles.31-33 Furthermore, while the overall agreement at 30° rotation reported here provided a clinically acceptable CV of less than 10%, the value of the 95% confidence interval of the CV for both the left and right ventricle in systole was greater than 10%, a variation that may not be clinically useful.
Two techniques have been described utilizing STIC and VOCAL to calculate cardiovascular parameters.2,4,6 When we compared the agreement in ventricular volume measurements obtained by each technique at 15° rotation, we noted that volumes calculated with Contour Finder: Trace were more repeatable than volumes obtained with either Inversion Mode2 or Manual Trace.4,6 Importantly, volume calculations obtained utilizing Manual Trace achieved CVs greater than 10%.
Ultrasonographic volume calculations utilizing STIC and VOCAL™ are repeatable and reproducible
To further quantify the variability inherent in volume measurements, we sought to examine repeatability and reproducibility. Good agreement was noted for each of three observers, as well as excellent intraobserver and interobserver reliability, suggesting that ventricular volume measurements obtained with Contour Finder: Trace are repeatable. Furthermore, the acquisition of two cardiac data sets obtained serially allowed for an assessment of the reproducibility of STIC and VOCAL, information which is currently absent in the literature. As expected, good agreement was present for each of the two data sets with excellent reliability for measurements taken on the same data set. There was no significant difference found between the paired mean CV, suggesting that a negligible amount of variability exists between acquisitions (<1%); additionally, the reliability of measurements taken between data sets was good (ICC >0.90). We did not observe a significant difference in the mean CV when ventricular side (left or right) was considered. In addition, the phase in the cardiac cycle (systole or diastole) did not significantly alter the mean CV. When each ventricle in systole and diastole was considered, only the left ventricle in diastole demonstrated significant difference in the mean CV between data sets. The absolute difference was 1.4%, and, while statistically significant, it is unlikely that a CV of this magnitude is clinically relevant. Moreover, a Bland-Altman plot comparing the percent difference between volume calculations from each STIC acquisition indicated that minimal bias (<1%) was introduced between acquisitions. Taken together, the excellent agreement and good reliability provides evidence to support the hypothesis that ventricular volumes, obtained utilizing Contour Finder: Trace, are reproducible.
Limitations
There are several limitations to the present study. First, there is currently no gold standard to serve as a means of comparison for the calculation of fetal ventricular volumes. Second, it is important to note that the product of a STIC data set is a computer generated, single cardiac cycle which is an assemblage of 20 to 30 real cardiac cycles. It is possible that some degree of smoothing or averaging of the ventricular borders could occur, introducing a degree of error into the calculations performed, a factor which remains to be explored.42 Furthermore, adequate volume data sets are limited by fetal position, movement, or respirations, as well as acoustic shadowing and drop out. Last, while the acquisition time of a STIC is at most 12.5 seconds, there is a significant learning curve and time commitment (approximately 8-10 minutes) required to orient and analyze the data. These factors have limited the widespread adoption of multidimensional imaging techniques, a trend that is changing as practitioners become accustomed to these newer tools.
Conclusions
Ventricular volumes obtained utilizing STIC and VOCAL with Contour Finder: Trace, provide repeatable and reproducible calculations. Taken together, the available literature2,4,6 and these results support the continued use of this technique, of which the clinical application is the calculation of the fetal cardiovascular parameters end systolic volume, end diastolic volume, stroke volume, cardiac output, and ejection fraction.
Acknowledgment
This research was supported (in part) by the Perinatology Research Branch, Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS.
Reference List
- 1.Esh-Broder E, Ushakov FB, Imbar T, Yagel S. Application of free-hand three-dimensional echocardiography in the evaluation of fetal cardiac ejection fraction: a preliminary study. Ultrasound Obstet Gynecol. 2004;23:546–551. doi: 10.1002/uog.1059. [DOI] [PubMed] [Google Scholar]
- 2.Messing B, Cohen SM, Valsky DV, et al. Fetal cardiac ventricle volumetry in the second half of gestation assessed by 4D ultrasound using STIC combined with inversion mode. Ultrasound Obstet Gynecol. 2007;30:142–151. doi: 10.1002/uog.4036. [DOI] [PubMed] [Google Scholar]
- 3.Meyer-Wittkopf M, Cole A, Cooper SG, Schmidt S, Sholler GF. Three-dimensional quantitative echocardiographic assessment of ventricular volume in healthy human fetuses and in fetuses with congenital heart disease. J Ultrasound Med. 2001;20:317–327. doi: 10.7863/jum.2001.20.4.317. [DOI] [PubMed] [Google Scholar]
- 4.Rizzo G, Capponi A, Cavicchioni O, Vendola M, Arduini D. Fetal cardiac stroke volume determination by four-dimensional ultrasound with spatio-temporal image correlation compared with two-dimensional and Doppler ultrasonography. Prenat Diagn. 2007;27:1147–1150. doi: 10.1002/pd.1870. [DOI] [PubMed] [Google Scholar]
- 5.Uittenbogaard LB, Haak MC, Spreeuwenberg MD, Van Vugt JM. Fetal cardiac function assessed with four-dimensional ultrasound imaging using spatiotemporal image correlation. Ultrasound Obstet Gynecol. 2009;33:272–281. doi: 10.1002/uog.6287. [DOI] [PubMed] [Google Scholar]
- 6.Molina FS, Faro C, Sotiriadis A, Dagklis T, Nicolaides KH. Heart stroke volume and cardiac output by four-dimensional ultrasound in normal fetuses. Ultrasound Obstet Gynecol. 2008;32:181–187. doi: 10.1002/uog.5374. [DOI] [PubMed] [Google Scholar]
- 7.Bartlett JW, Frost C. Reliability, repeatability and reproducibility: analysis of measurement errors in continuous variables. Ultrasound Obstet Gynecol. 2008;31:466–475. doi: 10.1002/uog.5256. [DOI] [PubMed] [Google Scholar]
- 8.Reed GF, Lynn F, Meade BD. Use of coefficient of variation in assessing variability of quantitative assays. Clin Diagn Lab Immunol. 2002;9:1235–1239. doi: 10.1128/CDLI.9.6.1235-1239.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 10.Allan LD, Chita SK, Al-Ghazali W, Crawford DC, Tynan M. Doppler echocardiographic evaluation of the normal human fetal heart. Br Heart J. 1987;57:528–533. doi: 10.1136/hrt.57.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reed KL, Meijboom EJ, Sahn DJ, et al. Cardiac Doppler flow velocities in human fetuses. Circulation. 1986;73:41–46. doi: 10.1161/01.cir.73.1.41. [DOI] [PubMed] [Google Scholar]
- 12.De Smedt MC, Visser GH, Meijboom EJ. Fetal cardiac output estimated by Doppler echocardiography during mid- and late gestation. Am J Cardiol. 1987;60:338–342. doi: 10.1016/0002-9149(87)90238-4. [DOI] [PubMed] [Google Scholar]
- 13.Kenny JF, Plappert T, Doubilet P, et al. Changes in intracardiac blood flow velocities and right and left ventricular stroke volumes with gestational age in the normal human fetus: a prospective Doppler echocardiographic study. Circulation. 1986;74:1208–1216. doi: 10.1161/01.cir.74.6.1208. [DOI] [PubMed] [Google Scholar]
- 14.Kiserud T, Ebbing C, Kessler J, Rasmussen S. Fetal cardiac output, distribution to the placenta and impact of placental compromise. Ultrasound Obstet Gynecol. 2006;28:126–136. doi: 10.1002/uog.2832. [DOI] [PubMed] [Google Scholar]
- 15.Mielke G, Benda N. Cardiac output and central distribution of blood flow in the human fetus. Circulation. 2001;103:1662–1668. doi: 10.1161/01.cir.103.12.1662. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt KG, Silverman NH, Hoffman JI. Determination of ventricular volumes in human fetal hearts by two-dimensional echocardiography. Am J Cardiol. 1995;76:1313–1316. doi: 10.1016/s0002-9149(99)80365-8. [DOI] [PubMed] [Google Scholar]
- 17.Sutton MS, Gill T, Plappert T, Saltzman DH, Doubilet P. Assessment of right and left ventricular function in terms of force development with gestational age in the normal human fetus. Br Heart J. 1991;66:285–289. doi: 10.1136/hrt.66.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Ghazali W, Chapman MG, Allan LD. Doppler assessment of the cardiac and uteroplacental circulations in normal and complicated pregnancies. Br J Obstet Gynaecol. 1988;95:575–580. doi: 10.1111/j.1471-0528.1988.tb09486.x. [DOI] [PubMed] [Google Scholar]
- 19.Al-Ghazali W, Chita SK, Chapman MG, Allan LD. Evidence of redistribution of cardiac output in asymmetrical growth retardation. Br J Obstet Gynaecol. 1989;96:697–704. doi: 10.1111/j.1471-0528.1989.tb03285.x. [DOI] [PubMed] [Google Scholar]
- 20.Capponi A, Rizzo G, Rinaldo D, Arduini D, Romanini C. Cardiac flow after fetal blood sampling in normally grown and growth-retarded fetuses. Prenat Diagn. 1995;15:1007–1016. doi: 10.1002/pd.1970151105. [DOI] [PubMed] [Google Scholar]
- 21.Chaddha V, Simchen MJ, Hornberger LK, et al. Fetal response to maternal exercise in pregnancies with uteroplacental insufficiency. Am J Obstet Gynecol. 2005;193:995–999. doi: 10.1016/j.ajog.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 22.Gardiner H, Brodszki J, Eriksson A, Marsal K. Volume blood flow estimation in the normal and growth-restricted fetus. Ultrasound Med Biol. 2002;28:1107–1113. doi: 10.1016/s0301-5629(02)00565-3. [DOI] [PubMed] [Google Scholar]
- 23.Makikallio K, Jouppila P, Rasanen J. Retrograde aortic isthmus net blood flow and human fetal cardiac function in placental insufficiency. Ultrasound Obstet Gynecol. 2003;22:351–357. doi: 10.1002/uog.232. [DOI] [PubMed] [Google Scholar]
- 24.Rizzo G, Arduini D. Fetal cardiac function in intrauterine growth retardation. Am J Obstet Gynecol. 1991;165:876–882. doi: 10.1016/0002-9378(91)90431-p. [DOI] [PubMed] [Google Scholar]
- 25.Verburg BO, Jaddoe VW, Wladimiroff JW, et al. Fetal hemodynamic adaptive changes related to intrauterine growth: the Generation R Study. Circulation. 2008;117:649–659. doi: 10.1161/CIRCULATIONAHA.107.709717. [DOI] [PubMed] [Google Scholar]
- 26.Simpson JM, Cook A. Repeatability of echocardiographic measurements in the human fetus. Ultrasound Obstet Gynecol. 2002;20:332–339. doi: 10.1046/j.1469-0705.2002.00799.x. [DOI] [PubMed] [Google Scholar]
- 27.Nordblom P, Bech-Hanssen O. Reference values describing the normal mitral valve and the position of the papillary muscles. Echocardiography. 2007;24:665–672. doi: 10.1111/j.1540-8175.2007.00474.x. [DOI] [PubMed] [Google Scholar]
- 28.Wladimiroff JW, McGhie J. Ultrasonic assessment of cardiovascular geometry and function in the human fetus. Br J Obstet Gynaecol. 1981;88:870–875. [PubMed] [Google Scholar]
- 29.Wladimiroff JW, Vosters R, McGhie JS. Normal cardiac ventricular geometry and function during the last trimester of pregnancy and early neonatal period. Br J Obstet Gynaecol. 1982;89:839–844. doi: 10.1111/j.1471-0528.1982.tb05037.x. [DOI] [PubMed] [Google Scholar]
- 30.Veille JC, Sivakoff M, Nemeth M. Evaluation of the human fetal cardiac size and function. Am J Perinatol. 1990;7:54–59. doi: 10.1055/s-2007-999447. [DOI] [PubMed] [Google Scholar]
- 31.Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: Anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117:1436–1448. doi: 10.1161/CIRCULATIONAHA.107.653576. [DOI] [PubMed] [Google Scholar]
- 32.Ho SY, Nihoyannopoulos P. Anatomy, echocardiography, and normal right ventricular dimensions. Heart. 2006;92(Suppl 1):i2–13. doi: 10.1136/hrt.2005.077875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sedmera D, Pexieder T, Vuillemin M, Thompson RP, Anderson RH. Developmental patterning of the myocardium. Anat Rec. 2000;258:319–337. doi: 10.1002/(SICI)1097-0185(20000401)258:4<319::AID-AR1>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 34.Uittenbogaard LB, Haak MC, Spreeuwenberg MD, Van Vugt JM. A systematic analysis of the feasibility of four-dimensional ultrasound imaging using spatiotemporal image correlation in routine fetal echocardiography. Ultrasound Obstet Gynecol. 2008;31:625–632. doi: 10.1002/uog.5351. [DOI] [PubMed] [Google Scholar]
- 35.Bhat AH, Corbett VN, Liu R, et al. Validation of volume and mass assessments for human fetal heart imaging by 4-dimensional spatiotemporal image correlation echocardiography: in vitro balloon model experiments. J Ultrasound Med. 2004;23:1151–1159. doi: 10.7863/jum.2004.23.9.1151. [DOI] [PubMed] [Google Scholar]
- 36.Martins WP, Ferriani RA, Barra DA, et al. Reliability and validity of tissue volume measurement by three-dimensional ultrasound: an experimental model. Ultrasound Obstet Gynecol. 2007;29:210–214. doi: 10.1002/uog.3916. [DOI] [PubMed] [Google Scholar]
- 37.Espinoza J, Kusanovic JP, Goncalves LF, et al. A novel algorithm for comprehensive fetal echocardiography using 4-dimensional ultrasonography and tomographic imaging. J Ultrasound Med. 2006;25:947–956. doi: 10.7863/jum.2006.25.8.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Myers SA, Fresquez M, Hamill N. Four-dimensional sonography of the fetal heart with spatiotemporal image correlation directed at the interventricular septum. J Ultrasound Med. 2007;26:1071–1075. doi: 10.7863/jum.2007.26.8.1071. [DOI] [PubMed] [Google Scholar]
- 39.Goncalves LF, Espinoza J, Romero R, et al. Four-dimensional fetal echocardiography with spatiotemporal image correlation (STIC): a systematic study of standard cardiac views assessed by different observers. J Matern Fetal Neonatal Med. 2005;17:323–331. doi: 10.1080/14767050500127765. [DOI] [PubMed] [Google Scholar]
- 40.DeVore GR, Polanco B, Sklansky MS, Platt LD. The ‘spin’ technique: a new method for examination of the fetal outflow tracts using three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2004;24:72–82. doi: 10.1002/uog.1085. [DOI] [PubMed] [Google Scholar]
- 41.Paladini D. Standardization of on-screen fetal heart orientation prior to storage of spatio-temporal image correlation (STIC) volume datasets. Ultrasound Obstet Gynecol. 2007;29:605–611. doi: 10.1002/uog.4049. [DOI] [PubMed] [Google Scholar]
- 42.DeVore GR, Falkensammer P, Sklansky MS, Platt LD. Spatio-temporal image correlation (STIC): new technology for evaluation of the fetal heart. Ultrasound Obstet Gynecol. 2003;22:380–387. doi: 10.1002/uog.217. [DOI] [PubMed] [Google Scholar]