Abstract
Background
Urgent/emergent status is often associated with increased risk among cardiac operations. The objective of this study was to analyze outcomes and cost differences in patients undergoing elective versus urgent/emergent mitral valve replacement (MVR) and repair operations.
Methods
From 2003-2008, 1,477 patients underwent isolated, primary mitral valve (MV) operations at 11 different centers in the Commonwealth of Virginia. Patients were stratified into four groups: elective MVR (n=419), elective MV repair (n=674), urgent/emergent MVR (n=261) and urgent/emergent MV repair (n=123). Preoperative risk, operative features, outcomes, and total costs were evaluated.
Results
MVR patients had more risk factors, including advanced age. Female gender and severe mitral regurgitation were more common among MV repairs. MVR incurred higher operative mortality (5.2% vs. 1.2%, p<0.001), more major complications (20.6% vs. 6.5%, p<0.001), longer postoperative (10.8 days vs. 6.2 days, p<0.001) and intensive care unit (117.7 hours vs. 51.4 hours, p<0.001) duration, and greater total costs ($45,166 vs. $26,229, p<0.001) compared to MV repair operations. Postoperative length of stay was longer for elective MVR patients compared to elective MV repair patients (p<0.001) as well as for urgent/emergent MVR patients compared to urgent/emergent MV repair patients (p=0.001). Total hospital costs were also higher for both elective MVR (p<0.001) and urgent/emergent MVR (p<0.001) compared to elective MV repair and urgent/emergent MV repair. Risk adjusted operative mortality (OR=11.4, p<0.001) and major complication rates (OR=7.6, p<0.001) were highest for urgent/emergent MVR.
Conclusions
Mitral valve repair is associated with lower morbidity, mortality and total costs compared to mitral valve replacement. For urgent/emergent operations, the improved outcomes with mitral repair over replacement are even more profound.
Keywords: Mitral Valve Replacement, Mitral Valve Repair, Urgent, Emergent, Outcomes
Introduction
Mitral valve (MV) disease is a common surgical condition within the United States. MV repair is the preferred treatment over mitral valve replacement (MVR) or medical management for patients with severe mitral regurgitation (MR) [1-7]. According to the Society of Thoracic Surgeons (STS) national database, overall repair rates average approximately 55% for isolated MV operations [8]; however, larger centers have documented an increasing ability to successfully perform MV repairs over time [9-12]. Proponents of mitral repair argue that preservation of the intrinsic mitral apparatus during MV repair has beneficial effects on long-term left ventricular function [13-15]. Furthermore, the efficacy of MV repair has been demonstrated for both degenerative and ischemic MV etiology [11, 12, 16-18].
The setting (elective or urgent/emergent) in which a cardiac operation is performed has been shown to impact postoperative outcomes. The majority of published series report outcomes in elective MV operations and exclude urgent/emergent operations despite the fact that urgent/emergent operative status independently predicts survival among MV replacements [19, 20]. In fact, studies have implicated both urgent/emergent operative status and mitral valve replacements as independent risk factors for in-hospital mortality among patients undergoing mitral valve operations [18]. To our knowledge, a direct examination of the interaction between MVR or MV repair and elective versus urgent/emergent operative status has not been previously reported.
The objective of this study was to examine the effect of operative status on outcomes and resource utilization among primary, isolated mitral valve operations. We hypothesized that patients undergoing urgent/emergent MV repair or replacement have increased operative risk, postoperative morbidity and total costs compared to those undergoing elective MV operations.
Patients and Methods
Patients
Due to the absence of patient identifiers in collected data and the fact that the data is collected for purposes other than research, data analyses were exempt from the University of Virginia Institutional Review Board (IRB), and participating institutions were exempt from Health Insurance Portability and Accountability Act (HIPAA) consideration by the use of the Small Business Agreement for Business Associates agreements between each hospital, participating surgeons and the Virginia Cardiac Surgery Quality Initiative (VCSQI). All MV operations were entered prospectively into the National STS clinical database by 11 different centers within the Commonwealth of Virginia participating in the VCSQI program. We retrospectively reviewed all patients undergoing primary, isolated mitral valve operations as reported by the VCSQI from January 2003 to December 2008. Primary MV operations were defined as those occurring in the absence of a prior sternotomy or cardiac operation. Patients were stratified according to operative status and cardiac operation into four groups: elective MVR (n=419), elective MV repair (n=674), urgent/emergent MVR (n=261) and urgent/emergent MV repair (n=123).
Patient characteristics, risk factors, operative features, postoperative outcomes and total hospital costs were evaluated. We used established STS definitions for all preoperative and operative variables as well as for postoperative outcomes [21]. Operative mortality included patient deaths that occurred prior to hospital discharge or within 30 days of operation. Major complications included the composite incidence of perioperative myocardial infarction, postoperative stroke, renal failure, or prolonged ventilation. Total hospital costs were estimated calculations as reported by the VCSQI.
Statistical Analysis
The primary outcomes of interest were operative mortality, major complication rate, postoperative length of stay, and total costs. All group comparisons were unpaired. Continuous variables were compared using analysis of variance (ANOVA), and categorical variables were compared using χ2 analysis or Fisher's exact tests as appropriate.
Multivariable logistic regression was performed to assess the independent affects of known preoperative risk factors on the odds of in-hospital death and postoperative major complication rate among patients undergoing mitral valve operations. All preoperative variables entered as covariates (patient age, gender, ejection fraction, cardiopulmonary bypass time, aortic cross clamp time, and operative group) were selected a priori based upon established clinical risk in mitral valve operations. The estimated odds of death were adjusted for all covariates. The discrimination achieved by these models was assessed using the area under the Receiver Operating Characteristics curve (AUC). AUC values of 1.0 indicate perfect discrimination between outcome groups, while values of 0.5 indicate results equal to chance.
Categorical variable comparisons are expressed as a percentage of the group of origin. Continuous variables are reported as means ± standard error of the mean (SEM). Odds ratios (OR) with a 95% confidence interval (CI) are used to report the results of logistic regression models. Reported p-values are two-tailed. Statistical significance was identified by p-values of less than 0.05. Data manipulation and analysis were performed using SPSS software, version17 (SPSS, Chicago, IL).
Results
Patient Risk Factors and Operative Features
All Patients
A total of 1,477 patients underwent primary, isolated MV replacement (n=676, 45.8%) or repair (n=801, 54.2%) in Virginia during the five-year study period. All patient demographics, preoperative risk factors, and operative features are presented in Table 1. MVR patients had a higher incidence of preoperative risk factors. Mean patient age was higher for those patients undergoing MVR. Female patients more frequently underwent MV Repair and had a higher incidence of severe mitral regurgitation. Mitral stenosis was more common among those undergoing MVR. Shorter aortic cross clap and cardiopulmonary bypass times were observed for the MV repair group. The majority of MV repair operations consisted of a reconstruction with annuloplasty, and the majority of MVR utilized bioprosthetic valves.
Table 1.
Patient demographics, preoperative risk factors and operative features for all patients undergoing mitral valve replacement versus repair operations.
| Variable | MVR (n=676) | MV Repair (n=801) | P-value |
|---|---|---|---|
| PREOPERATIVE | |||
| Patient Age | 60.8±0.5 | 57.0±0.5 | <0.001 |
| Sex (Female) | 293 (43.4%) | 483 (60.6%) | <0.001 |
| Hypertension | 412 (60.9%) | 401 (50.1%) | <0.001 |
| Peripheral Arterial Disease | 51 (7.5%) | 30 (3.7%) | 0.002 |
| Stroke | 72 (10.7%) | 35 (4.4%) | <0.001 |
| Diabetes Mellitus | 131 (19.4%) | 79 (9.9%) | <0.001 |
| Heart Failure | 377 (55.8%) | 254 (31.7%) | <0.001 |
| Atrial fibrillation | 166 (24.6%) | 74 (9.2%) | <0.001 |
| NYHA Class | |||
| Class I | 88 (13.0%) | 185 (23.1%) | <0.001 |
| Class II | 194 (28.7%) | 340 (42.4%) | <0.001 |
| Class III | 240 (35.5%) | 217 (27.1%) | 0.001 |
| Class IV | 154 (22.8%) | 59 (7.4%) | <0.001 |
| Infective Endocarditis | 123 (18.2%) | 65 (8.1%) | <0.001 |
| Renal Failure | 59 (8.7%) | 29 (3.6%) | <0.001 |
| Renal Failure (Hemodialysis) | 46 (6.8%) | 21 (2.6%) | <0.001 |
| Ejection Fraction (%) | 53.5±0.5 | 54.9±0.4 | 0.03 |
| Mitral Stenosis | 139 (20.6%) | 17 (2.1%) | <0.001 |
| Mitral Regurgitation (Moderate) | 82 (12.1%) | 98 (12.2%) | 0.94 |
| Mitral Regurgitation (Severe) | 485 (71.7%) | 658 (82.1%) | <0.001 |
| OPERATIVE | |||
| Valve Replacement | |||
| Bioprosthetic | 389 (57.5%) | - | - |
| Mechanical | 287 (42.5%) | - | - |
| Valve Repair Technique | |||
| Annuloplasty Only | - | 237 (29.6%) | - |
| Reconstruction with Annuloplasty | - | 541 (67.5%) | - |
| Reconstruction without Annuloplasty | - | 23 (2.9%) | - |
| Aortic Cross Clamp Time (min) | 94.8±1.5 | 86.1±1.3 | <0.001 |
| Cardiopulmonary Bypass Time (min) | 138.1±2.1 | 123.3±1.6 | <0.001 |
Elective MV Operations
Similar trends in risk factors were observed among patients undergoing elective MV operations (Table 2). A total of 1,093 patients underwent elective MVR (n=419, 38.3%) or MV repair (n=674, 61.7%). Preoperative atrial fibrillation was more frequent in the elective MVR group. The incidence of preoperative peripheral arterial disease, ventricular arrhythmia and endocarditis were similar between groups, while severe mitral regurgitation was more common in the elective MV repair group. Aortic cross clamp and cardiopulmonary bypass times were shorter in elective MV repair compared to elective MVR.
Table 2.
Patient demographics, preoperative risk factors and operative features for patients undergoing mitral valve operations by operative group.
| Variable | Elective | Urgent/Emergent | ||||
|---|---|---|---|---|---|---|
| MVR (n=419) | MV Repair (n=674) | P-value | MVR (n=261) | MV Repair (n=123) | P value | |
| PREOPERATIVE | ||||||
| Patient Age | 60.3±0.7 | 56.8±0.5 | <0.001 | 61.4±0.8 | 58.2±1.2 | 0.03 |
| Sex (Female) | 243 (58.0%) | 265 (39.3%) | <0.001 | 144 (55.2%) | 50 (40.7%) | 0.01 |
| Hypertension | 256 (61.1%) | 330 (49.0%) | <0.001 | 158 (60.5%) | 69 (56.1%) | 0.44 |
| Peripheral Arterial Disease | 25 (6.0%) | 23 (3.4%) | 0.05 | 26 (10.0%) | 7 (5.7%) | 0.18 |
| Stroke | 40 (9.5%) | 23 (3.4%) | <0.001 | 32 (12.3%) | 12 (9.8%) | 0.61 |
| Diabetes Mellitus | 70 (16.7%) | 62 (9.2%) | <0.001 | 61 (23.4%) | 17 (13.8%) | 0.03 |
| Heart Failure | 180 (43.0%) | 168 (24.9%) | <0.001 | 199 (76.2%) | 83 (67.5%) | 0.08 |
| Atrial fibrillation | 93 (22.2%) | 54 (8.0%) | <0.001 | 73 (28.0%) | 20 (16.3%) | 0.02 |
| NYHA Class | ||||||
| Class I | 73 (17.4%) | 164 (24.3%) | 0.01 | 17 (6.5%) | 19 (15.4%) | 0.01 |
| Class II | 154 (36.8%) | 315 (46.7%) | 0.001 | 40 (15.3%) | 25 (20.3%) | 0.24 |
| Class III | 156 (37.2%) | 174 (25.8%) | <0.001 | 84 (32.2%) | 43 (35.0%) | 0.64 |
| Class IV | 36 (8.6%) | 21 (3.1%) | <0.001 | 120 (46.0%) | 36 (29.3%) | 0.002 |
| Infective Endocarditis | 41 (9.8%) | 45 (6.7%) | 0.07 | 82 (31.4%) | 20 (16.3%) | 0.002 |
| Renal Failure | 23 (5.5%) | 16 (2.4%) | 0.01 | 36 (13.8%) | 12 (9.8%) | 0.32 |
| Renal Failure (Hemodialysis) | 18 (4.3%) | 11 (1.6%) | 0.01 | 28 (10.7%) | 9 (7.3%) | 0.19 |
| Ejection Fraction (%) | 54.4±0.6 | 55.7±0.4 | 0.06 | 52.1±0.8 | 50.7±1.3 | 0.34 |
| Mitral Valve Stenosis | 100 (23.9%) | 13 (1.9%) | <0.001 | 39 (14.9%) | 4 (3.3%) | 0.003 |
| Mitral Regurgitation (Moderate) | 13.4% | 12.3% | 0.64 | 26 (10.0%) | 15 (12.2%) | 0.60 |
| Mitral Regurgitation (Severe) | 70.2% | 82.6% | <0.001 | 194 (74.3%) | 99 (80.5%) | 0.20 |
| OPERATIVE | ||||||
| Aortic Cross Clamp Time (min) | 93.5±1.9 | 86.4±1.4 | 0.002 | 97.2±2.4 | 84.0±3.6 | 0.002 |
| Cardiopulmonary Bypass Time (min) | 133.9±2.5 | 123.8±1.7 | 0.001 | 144.4±3.7 | 120.5±4.4 | <0.001 |
Urgent/ Emergent Operations
Fewer preoperative differences existed between patients undergoing urgent/emergent MVR compared to urgent/emergent MV repair operations (Table 2). Female patients more frequently underwent urgent/emergent MVR compared to MV repair, and the mean age was slightly higher in the MVR group. MVR patients had higher rates of preoperative diabetes, atrial fibrillation, and NYHA Class IV functional status. Similar to elective cases, urgent/emergent MV repair patients had shorter aortic cross clamp and cardiopulmonary bypass times compared to MV replacement patients.
Outcomes for Mitral Valve Replacement and Repair
In the entire cohort, outcomes were worse for MVR compared to MV repair. MVR incurred higher operative mortality (5.2% vs. 1.2%, p<0.001) and major complication rates (20.6% vs. 6.5%, p<0.001) compared to MV repair (Figure 1). Moreover, MVR patients had longer postoperative (10.8±0.5 days vs. 6.2±0.2 days, p<0.001) and intensive care unit (4.9±0.4 days vs. 2.1+0.1 days, p<0.001) lengths of stays (Figure 2) compared to MV repair patients. MVR also conferred greater total costs ($45,166±1,754 vs. $26,229±623, p<0.001).
Figure 1.
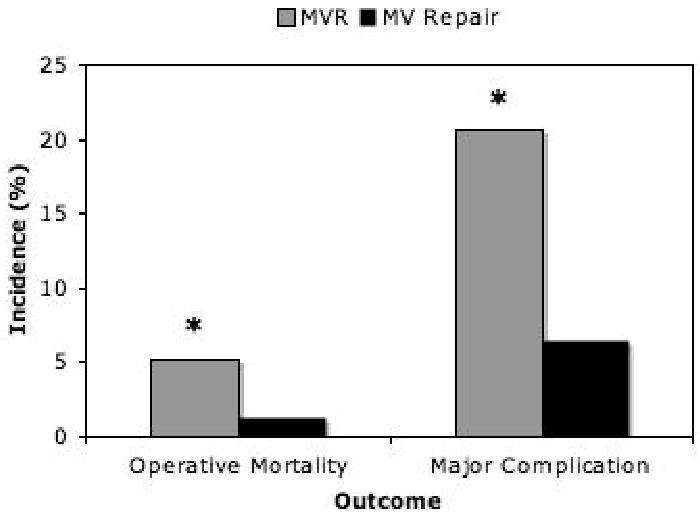
Operative mortality and major complication rate following primary, isolated mitral valve replacement versus repair operations.
Figure 2.
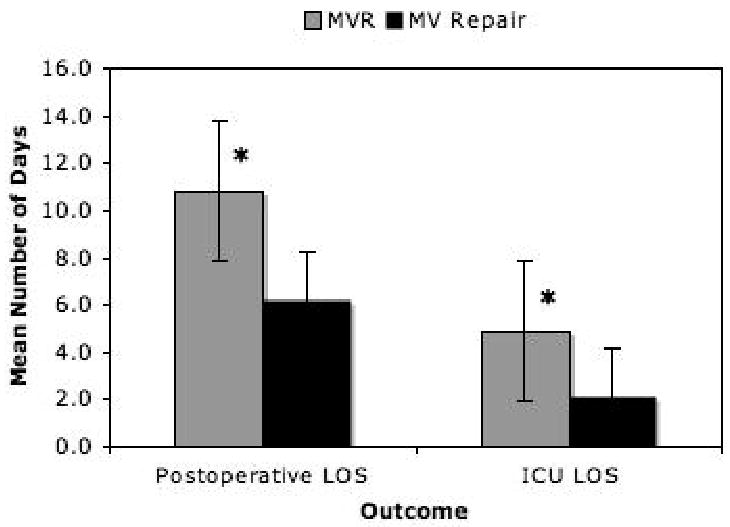
Mean postoperative and intensive care unit (ICU) length of stay following primary, isolated mitral valve replacement versus repair operations.
A comparison of postoperative outcomes stratified by operative status is presented in Table 3. Elective MVR was associated with increased morbidity, longer postoperative length of stay, and higher total costs compared to elective MV repair. However, despite more complications, operative mortality was similar and low for both elective MVR and elective repair. In contrast, more dramatic differences in postoperative mortality and morbidity were observed in patients undergoing urgent/emergent MV operations. Urgent/emergent MVR was associated with higher major complications rates, longer postoperative length of stay, higher total costs and significantly higher operative mortality compared to urgent/emergent MV repair.
Table 3.
Postoperative outcomes for patients undergoing mitral valve operations by operative group.
| Outcome | Elective | Urgent/Emergent | ||||
|---|---|---|---|---|---|---|
| MVR (n=419) | MV Repair (n=673) | P-value | MVR (n=257) | MV Repair (n=128) | P-value | |
| Operative Mortality | 7 (1.7%) | 5 (0.7%) | 0.23 | 28 (10.9%) | 5 (3.9%) | 0.03 |
| Major Complication | 54 (12.9%) | 32 (4.8%) | <0.001 | 85 (33.1%) | 20 (15.6%) | 0.001 |
| Myocardial Infarction | 0 (0.0%) | 0 (0.0%) | N/A | 0 (0.0%) | 0 (0.0%) | N/A |
| Stroke | 9 (2.1%) | 6 (0.9%) | 0.11 | 10 (3.9%) | 5 (3.9%) | >0.99 |
| Renal Failure | 18 (4.3%) | 10 (1.5%) | 0.01 | 27 (10.5%) | 3 (2.3%) | 0.01 |
| Prolonged Ventilation | 44 (10.5%) | 22 (3.3%) | <0.001 | 76 (29.6%) | 18 (14.1%) | 0.002 |
| Hemodialysis | 10 (2.4%) | 4 (0.6%) | 0.01 | 17 (6.6%) | 0 (0.0%) | 0.002 |
| Pneumonia | 18 (4.3%) | 9 (1.3%) | 0.004 | 20 (7.8%) | 5 (3.9%) | 0.27 |
| Gastrointestinal Event | 11 (2.6%) | 2 (0.3%) | 0.001 | 17 (6.6%) | 2 (1.6%) | 0.04 |
| Sepsis | 4 (1.0%) | 1 (0.1%) | 0.07 | 16 (6.2%) | 3 (1.6%) | 0.07 |
| Bleeding or Tamponade | 9 (2.1%) | 22 (3.3%) | 0.35 | 17 (6.6%) | 6 (4.7%) | 0.65 |
| Postoperative Length of Stay (Days) | 8.8±0.4 | 5.7±0.2 | <0.001 | 14.1±0.9 | 9.1±0.9 | 0.001 |
| ICU Length of Stay (Days) | 3.3±0.4 | 1.9±0.1 | <0.001 | 7.4±0.9 | 3.4±0.6 | 0.003 |
| Total Cost ($) | 37,793±1,509 | 24,599±552 | <0.001 | 58,104±3,775 | 35,522±2,623 | <0.001 |
Risk Adjusted Mortality and Major Complications
Multivariable logistic regression results evaluating the effect of the interaction between mitral valve operation type and operative setting on mortality and complications are displayed in Tables 4 and 5, respectively. Adjusted operative mortality was associated with patient age, cardiopulmonary bypass time and aortic cross clamp time. Mortality was also highly associated with urgent/emergent MV repair (OR=4.3, p=0.03) and was very highly associated with urgent/emergent MVR (OR=11.4, p<0.001) compared to elective MV repair. Adjusted major complication rate was associated with patient age, ejection fraction, cardiopulmonary bypass time, elective MVR, urgent/emergent MV repair, and was highly associated with urgent/emergent MVR (OR=7.63, p<0.001). These models achieved adequate discrimination with AUC =0.88 and 0.80, respectively. To assess the effect of mitral valve operation type and operative status independently, separate logistic regression models were performed. Performance of an MVR procedure was an independent predictor of operative mortality (OR=2.91 (1.38-6.17), p=0.01) and major complications (OR=2.43 (1.67-3.53), p<0.001) compared to MV repair. Similarly, urgent/emergent operative status independently increased the odds of operative mortality (6.85 (3.31-14.21), p<0.001) and major complications (OR=3.13 (2.23-4.39), p<0.001) compared to elective operative status.
Table 4.
Multivariate logistic regression reflecting the combined effect of mitral valve operation and operative setting on adjusted operative mortality.
| Covariate | Odds Ratio | 95% Confidence Interval | P-value |
|---|---|---|---|
| Male (Reference) | 1.00 | - | - |
| Female | 1.20 | 0.62-2.33 | 0.60 |
| Age (years) | 1.04 | 1.01-1.06 | 0.01 |
| Ejection Fraction (%) | 0.99 | 0.96-1.01 | 0.27 |
| Cardiopulmonary Bypass Time (min) | 1.02 | 1.01-1.02 | <0.001 |
| Aortic Cross Clamp Time (min) | 0.98 | 0.97-0.99 | <0.001 |
| Elective MV repair (Reference) | 1.00 | - | - |
| Elective MVR | 1.33 | 0.39-4.52 | 0.65 |
| Urgent/Emergent MV Repair | 4.28 | 1.16-15.76 | 0.03 |
| Urgent/Emergent MVR | 11.41 | 4.20-31.02 | <0.001 |
Area Under Receiver Operative Curve=0.88.
Table 5.
Multivariate logistic regression reflecting the combined effect of mitral valve operation and operative setting on adjusted major complication rate.
| Covariate | Odds Ratio | 95% Confidence Interval | P-value |
|---|---|---|---|
| Male (Reference) | 1.00 | - | - |
| Female | 1.21 | 0.84-1.72 | 0.30 |
| Age (years) | 1.02 | 1.01-1.04 | 0.001 |
| Ejection Fraction (%) | 0.98 | 0.97-0.99 | 0.003 |
| Cardiopulmonary Bypass Time (min) | 1.01 | 1.00-1.01 | 0.01 |
| Aortic Cross Clamp Time (min) | 0.99 | 0.98-0.99 | 0.02 |
| Elective MV Repair (Reference) | 1.00 | - | - |
| Elective MVR | 2.47 | 1.53-3.98 | <0.001 |
| Urgent/Emergent MV Repair | 3.20 | 1.71-5.97 | <0.001 |
| Urgent/Emergent MVR | 7.63 | 4.77-12.20 | <0.001 |
Area Under Receiver Operative Curve=0.80.
Comment
This study more clearly defines the interaction between elective versus urgent/emergent operative status and type of mitral valve operation, and it highlights the short-term benefits of mitral valve repair over replacement. Within this large, multi-institutional patient cohort, mitral valve repair was performed in 54% of patients, which is similar to nationwide repair rates. Mitral valve replacement incurred higher operative mortality, more major complications, longer postoperative lengths of stay, and higher total hospital costs compared to mitral valve repair. On multivariable logistic regression, mitral valve replacement was significantly associated with adjusted in-hospital mortality and major complications. Furthermore, urgent/emergent mitral valve replacement was the single most important predictor of postoperative morbidity and mortality. We believe this study provides important contributions to current literature examining outcomes of mitral valve operations.
Elective versus urgent and/or emergent operative status can greatly impact postoperative outcomes in cardiac surgery. Other studies have suggested that urgent and/or emergent operative status can independently increase a patient's risk of poor outcomes and mortality for MV operations [18, 20]. In a series of 1,844 patients over 17 years who underwent primary MVR with and without concomitant coronary artery bypass grafting (CABG), Thourani et al. [20] reported that urgent/emergent operative status significantly increased the odds of both in-hospital mortality (OR=4.37, p<0.0001) and 10-year mortality (OR=1.40, p=0.03). In a follow-up study comparing outcomes of MV repair versus replacement ± CABG, this same group [18] demonstrated similar results, reporting that urgent and emergent operative status was highly associated with both in-hospital (OR=3.03 and 9.18, respectively) and long-term (OR=1.43 and 2.06, respectively) mortality. Although these reports further implicate the role of urgent and/or emergent operative status within MV operations, the interaction between either isolated MV repair or replacement and operative status has not been well established.
In the present study, we not only demonstrated but also quantified an important interaction between the performance of either a MV repair or replacement in an elective or urgent/emergent operative setting within a multi-institutional, statewide database. Our results suggest that an urgent/emergent MV repair independently conferred a 4.3-fold increase in the odds of operative mortality while an urgent/emergent MVR increased the odds of operative morality by a factor of 11.4 compared to elective MV repair. Similarly, urgent/emergent MVR (OR=7.63) conferred the highest adjusted odds of major complications compared to elective MV repair while urgent/emergent MV repair provided an adjusted 3.2-fold increase and elective MVR a 2.5-fold increase in major complications.
The number of studies directly comparing mortality and long-term survival of MV repair versus replacement are increasing. Most reports are single-institution series, while large, multi-institutional, population-based studies comparing MV operations are limited. Operative mortality and long-term survival advantages favor MV repair over replacement [3, 16, 18, 22, 23]. The STS national database reported operative mortality for isolated MV repair is 1.7% compared to 5.9% for MV replacement [8]. In a propensity matched study of 625 MV repairs and 625 replacements, Thourani et al. [18] reported 4.3% in-hospital mortality for MV repair versus 6.9% for replacements (p=0.049) and significantly better 10-year survival for MV repairs (62% vs. 46%). Recently, Ailawadi et al. reported similar mortality advantages (7.1% vs. 23.4%, p=0.01) and survival benefits (p=0.04) favoring MV repair over replacement among elderly patients [16]. In the present study, we demonstrated lower unadjusted operative mortality rates for MV repairs, and the difference between operative mortality following urgent/emergent MVR and MV repair operations was even more profound. The higher incidence of preoperative patient risk factors may have favored higher overall unadjusted operative morality rates for MV replacements. However, after adjusting for confounding variables, MV replacement operations (OR=2.92, p=0.01) were independently correlated with operative mortality compared to MV repairs. These results are consistent with those of previously published studies [3, 16, 18].
Other outcomes measures further highlight disparate differences between MV operations performed in the elective and urgent/emergent operative setting. Several recent series have documented longer postoperative hospital stays for patients undergoing MVR compared to MV repair operations [16, 18, 24]. In a recent review of over 58,000 MV operations, Gammie et al. [24] documented a median postoperative length of stay of 7.0 days for MVR versus 6.0 days (p<0.001) for MV repair. These trends are consistent with our report with shorter postoperative lengths of stay for MV repair (6.2±0.2 days) compared to MVR (10.8±0.5 days, p<0.001).
The economic implications of MV surgery remain ill defined. In this study, the average total hospital costs per patient were higher in those undergoing MVR operations. Further, we observed that urgent/emergent operative status markedly increased total hospital costs compared to elective operations. Importantly, the cost data obtained by the VCSQI is imperfect and reflect estimated values. However, despite these estimations, it is evident that the combination of a MVR performed in an urgent/emergent setting significantly increases the financial burden on both patients and the overall healthcare system. Although further investigation with more accurate cost reporting is warranted to truly assess the effect of various factors during MV surgery, the trends reported herein are consistent with those of previous studies [20]. Another report examined total hospital costs and resource utilization among patients undergoing MVR ± CABG and demonstrated that isolated, urgent/emergent MVR had significantly higher total hospitals costs and overall resource utilization compared to isolated, elective MVR [20].
Our study generated some unique observations that deserve further discussion. For example, the absence of perioperative myocardial infarction in either MVR or MV repair groups was surprising. Similarly, on multivariate analysis, aortic cross clamp time was associated with improved operative mortality and major complications; however, on univariate comparison cross clamp times were longer in each MVR group. These paradoxical findings represent an inherent difficulty with scrutinizing a large, de-identified data registry. As a result, we are unable to further investigate these findings and are unable to comment on their true clinical significance.
This study has several limitations to mention. As with any retrospective review, the inherent selection bias is possible. Additionally, the difference in patient risk factors between MVR and MV repair groups may account for some of the differences in observed outcomes. The use of established STS definitions for all patient risk factors, operative features and postoperative outcomes limits the ability to extrapolate our results to a broader patient group. We were also constrained during data collection by the presence of completely de-identified data points. As a result, we are unable to scrutinize certain data such as valve morphology, valve etiology, or surgical approach via sternotomy or non-sternotomy, and we are only able to comment on short-term outcomes. Longer follow-up would add impact to the observed trends in outcomes following MV operations. The use of estimated cost information obtained from the VCSQI is imperfect. Furthermore, the low incidence of operative mortality following MV operations limited modeling efforts for adjusted outcomes. The covariates entered into our models represent well-established risk factors for cardiac operations and reflect important differences between patients that may impact outcome. The inclusion of more covariates during regression analyses may have helped define smaller differences between the odds of adjusted outcomes; however, in order to avoid overestimation of the models, this would have required a larger patient cohort than the 1,477 patient studied here. The calculated length of stay and total hospital costs included in our data analyses reflect unadjusted means and are not corrected for the potential confounding influence of other risk factors. Finally, the potential influence of an unmeasured confounder may, in part, explain some of the estimated effects observed between operative groups during logistic regression modeling. Nevertheless, the markedly improved outcomes of MV repair over replacement in both the elective and urgent/emergent setting provides an important clinical contribution as it highlights a significant operative interaction that continues to be defined within published cardiac literature.
Conclusions
In this study, we conclude that mitral valve repair is associated with lower morbidity, mortality and total hospital costs compared to mitral valve replacement. For urgent/emergent operations, the improved outcomes in mitral valve repair over replacement are even more profound. These important interactions should be considered when evaluating the operative setting and surgical benefits for patients undergoing MV operations. Attempts to alter the operative risk to an elective setting may improve outcomes.
Acknowledgments
We would like to thank George J. Stukenborg, PhD of the University of Virginia Department of Public Health Sciences for his statistical collaboration in this study.
Funding: NIH/NHLBI T32 Training Grant HL007849 (DL, SH), TSFRE Research Grant (GA)
Footnotes
Presented at the 46th Annual Meeting of the Society of Thoracic Surgeons, Fort Lauderdale, FL, January 25-27, 2010
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Braunberger E, Deloche A, Berrebi A, Abdallah F, Celestin JA, Meimoun P, Chatellier G, Chauvaud S, Fabiani JN, Carpentier A. Very long-term results (more than 20 years) of valve repair with carpentier's techniques in nonrheumatic mitral valve insufficiency. Circulation. 2001;104(12 Suppl 1):I8–11. [PubMed] [Google Scholar]
- 2.Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, Detaint D, Capps M, Nkomo V, Scott C, Schaff HV, Tajik AJ. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med. 2005;352(9):875–83. doi: 10.1056/NEJMoa041451. [DOI] [PubMed] [Google Scholar]
- 3.Enriquez-Sarano M, Schaff HV, Orszulak TA, Tajik AJ, Bailey KR, Frye RL. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis. Circulation. 1995;91(4):1022–8. doi: 10.1161/01.cir.91.4.1022. [DOI] [PubMed] [Google Scholar]
- 4.Gillinov AM, Cosgrove DM, Blackstone EH, Diaz R, Arnold JH, Lytle BW, Smedira NG, Sabik JF, McCarthy PM, Loop FD. Durability of mitral valve repair for degenerative disease. J Thorac Cardiovasc Surg. 1998;116(5):734–43. doi: 10.1016/S0022-5223(98)00450-4. [DOI] [PubMed] [Google Scholar]
- 5.Gillinov AM, Wierup PN, Blackstone EH, Bishay ES, Cosgrove DM, White J, Lytle BW, McCarthy PM. Is repair preferable to replacement for ischemic mitral regurgitation? J Thorac Cardiovasc Surg. 2001;122(6):1125–41. doi: 10.1067/mtc.2001.116557. [DOI] [PubMed] [Google Scholar]
- 6.Grossi EA, Goldberg JD, LaPietra A, Ye X, Zakow P, Sussman M, Delianides J, Culliford AT, Esposito RA, Ribakove GH, Galloway AC, Colvin SB. Ischemic mitral valve reconstruction and replacement: comparison of long-term survival and complications. J Thorac Cardiovasc Surg. 2001;122(6):1107–24. doi: 10.1067/mtc.2001.116945. [DOI] [PubMed] [Google Scholar]
- 7.Suri RM, Schaff HV, Dearani JA, Sundt TM, 3rd, Daly RC, Mullany CJ, Enriquez-Sarano M, Orszulak TA. Survival advantage and improved durability of mitral repair for leaflet prolapse subsets in the current era. Ann Thorac Surg. 2006;82(3):819–26. doi: 10.1016/j.athoracsur.2006.03.091. [DOI] [PubMed] [Google Scholar]
- 8.National Adult Cardiac Surgery Database. Society of Thoracic Surgeons. 2009 [Google Scholar]
- 9.Detaint D, Sundt TM, Nkomo VT, Scott CG, Tajik AJ, Schaff HV, Enriquez-Sarano M. Surgical correction of mitral regurgitation in the elderly: outcomes and recent improvements. Circulation. 2006;114(4):265–72. doi: 10.1161/CIRCULATIONAHA.106.619239. [DOI] [PubMed] [Google Scholar]
- 10.Seeburger J, Borger MA, Falk V, Kuntze T, Czesla M, Walther T, Doll N, Mohr FW. Minimal invasive mitral valve repair for mitral regurgitation: results of 1339 consecutive patients. Eur J Cardiothorac Surg. 2008;34(4):760–5. doi: 10.1016/j.ejcts.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Dibardino DJ, Elbardissi AW, McClure RS, Razo-Vasquez OA, Kelly NE, Cohn LH. Four decades of experience with mitral valve repair: Analysis of differential indications, technical evolution, and long-term outcome. J Thorac Cardiovasc Surg. 2009 doi: 10.1016/j.jtcvs.2009.08.058. [DOI] [PubMed] [Google Scholar]
- 12.Svensson LG, Atik FA, Cosgrove DM, Blackstone EH, Rajeswaran J, Krishnaswamy G, Jin U, Gillinov AM, Griffin B, Navia JL, Mihaljevic T, Lytle BW. Minimally invasive versus conventional mitral valve surgery: A propensity-matched comparison. J Thorac Cardiovasc Surg. 2009 doi: 10.1016/j.jtcvs.2009.09.038. [DOI] [PubMed] [Google Scholar]
- 13.David TE, Uden DE, Strauss HD. The importance of the mitral apparatus in left ventricular function after correction of mitral regurgitation. Circulation. 1983;68(3 Pt 2):II76–82. [PubMed] [Google Scholar]
- 14.Komeda M, David TE, Rao V, Sun Z, Weisel RD, Burns RJ. Late hemodynamic effects of the preserved papillary muscles during mitral valve replacement. Circulation. 1994;90(5 Pt 2):II190–4. [PubMed] [Google Scholar]
- 15.Lee EM, Shapiro LM, Wells FC. Importance of subvalvular preservation and early operation in mitral valve surgery. Circulation. 1996;94(9):2117–23. doi: 10.1161/01.cir.94.9.2117. [DOI] [PubMed] [Google Scholar]
- 16.Ailawadi G, Swenson BR, Girotti ME, Gazoni LM, Peeler BB, Kern JA, Fedoruk LM, Kron IL. Is mitral valve repair superior to replacement in elderly patients? Ann Thorac Surg. 2008;86(1):77–85. doi: 10.1016/j.athoracsur.2008.03.020. discussion 86. [DOI] [PubMed] [Google Scholar]
- 17.Gazoni LM, Kern JA, Swenson BR, Dent JM, Smith PW, Mulloy DP, Reece TB, Fedoruk LM, Lisle TC, Peeler BB, Kron IL. A change in perspective: results for ischemic mitral valve repair are similar to mitral valve repair for degenerative disease. Ann Thorac Surg. 2007;84(3):750–7. doi: 10.1016/j.athoracsur.2007.04.098. discussion 58. [DOI] [PubMed] [Google Scholar]
- 18.Thourani VH, Weintraub WS, Guyton RA, Jones EL, Williams WH, Elkabbani S, Craver JM. Outcomes and long-term survival for patients undergoing mitral valve repair versus replacement: effect of age and concomitant coronary artery bypass grafting. Circulation. 2003;108(3):298–304. doi: 10.1161/01.CIR.0000079169.15862.13. [DOI] [PubMed] [Google Scholar]
- 19.Christakis GT, Weisel RD, David TE, Salerno TA, Ivanov J. Predictors of operative survival after valve replacement. Circulation. 1988;78(3 Pt 2):I25–34. [PubMed] [Google Scholar]
- 20.Thourani VH, Weintraub WS, Craver JM, Jones EL, Gott JP, Brown WM, 3rd, Puskas JD, Guyton RA. Influence of concomitant CABG and urgent/emergent status on mitral valve replacement surgery. Ann Thorac Surg. 2000;70(3):778–83. doi: 10.1016/s0003-4975(00)01641-6. discussion 83-4. [DOI] [PubMed] [Google Scholar]
- 21.Society of Thoracic Surgeons Adult Cardiac Surgery Database. STS Adult Cardiac Data Specifications, Version 2.61. 2007 August 24; Available at ( http://www.sts.org/documents/pdf/AdultCVDataSpecifications2.61.pdf)
- 22.Akins CW, Hilgenberg AD, Buckley MJ, Vlahakes GJ, Torchiana DF, Daggett WM, Austen WG. Mitral valve reconstruction versus replacement for degenerative or ischemic mitral regurgitation. Ann Thorac Surg. 1994;58(3):668–75. doi: 10.1016/0003-4975(94)90725-0. discussion 75-6. [DOI] [PubMed] [Google Scholar]
- 23.Cohn LH, Kowalker W, Bhatia S, DiSesa VJ, St John-Sutton M, Shemin RJ, Collins JJ. Comparative morbidity of mitral valve repair versus replacement for mitral regurgitation with and without coronary artery disease. 1988. Updated in 1995. Ann Thorac Surg. 1995;60(5):1452–3. doi: 10.1016/0003-4975(95)00379-y. [DOI] [PubMed] [Google Scholar]
- 24.Gammie JS, Sheng S, Griffith BP, Peterson ED, Rankin JS, O'Brien SM, Brown JM. Trends in mitral valve surgery in the United States: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg. 2009;87(5):1431–7. doi: 10.1016/j.athoracsur.2009.01.064. discussion 37-9. [DOI] [PubMed] [Google Scholar]


