Abstract
Prostate cancer is the most common cancer and the second leading cause of cancer deaths among males in most Western countries. Autologous cellular immunotherapy for the treatment of cancer seeks to induce tumor-specific immunity in the patient and is consequently dependent on a suitable target antigen and effective presentation of that antigen to the patient's immune system. Prostatic acid phosphatase (PAP) has been tested as a target antigen due to its high and apparently specific expression in the prostate. We used a variety of approaches to analyze PAP expression, including immunohistochemistry, in situ hybridization, and quantitative polymerase chain reaction. We complemented these laboratory-based techniques with an in silico analysis of reported PAP expression in human cDNA libraries. Our studies confirmed that, while PAP expression is not restricted to prostate tissues, its expression in other human tissues is approximately 1-2 orders of magnitude less than that observed in the prostate. The relative specificity of PAP expression in the prostate supports its use as a target of autologous cellular immunotherapy. The approach described here, involving the use of multiple correlates of tissue-specific expression, is warranted as a prerequisite in selecting any suitable target for immunotherapy.
Keywords: Prostatic acid phosphatase, prostate cancer, immunotherapy, immunohistochemistry, quantitative polymerase chain reaction
Introduction
Immune therapy has emerged as a powerful new approach to cancer therapy. Monoclonal antibodies are now front line agents in several oncology settings [1]. Novel approaches to stimulating a patient's immune response to overcome a cancer are being assessed in multiple clinical trials [2]. One question that is still subject to dispute concerns which molecules constitute appropriate targets for such therapies. Though it is rare to find a molecule that is expressed uniquely in the transformed target tissue, a number of candidates have been advanced. Understanding the tissue distribution of a given target molecule is essential for determining potential side-effects of the therapy, as well as for judging potential opportunities to exploit the therapy for new indications. Sipu-leucel-T is a United States Food and Drug Administration (FDA)-approved autologous cellular immunotherapy that targets prostatic acid phosphatase (PAP) as a treatment for advanced prostate cancer, and has demonstrated evidence of survival prolongation in men with asymptomatic or minimally symptomatic metas-tatic castrate resistant (hormone refractory) prostate cancer in randomized controlled Phase 3 clinical trials [3, 4]. It is of interest to know which other tissues express PAP in order to evaluate cross-reactivity and clinical safety.
In humans, PAP is one of the major proteins secreted by prostate columnar epithelium secretory cells following puberty. PAP protein has been determined to be approximately 0.5 mg/g wet weight of prostate tissue [5, 6] and approximately 1 mg/mL in seminal fluid [7]. In healthy individuals, PAP serum levels are low, on the order of 1-3 ng/mL, whereas serum levels are elevated in many individuals with metastatic prostate cancer [8-10]. Data from immunohistochemistry (IHC) studies indicate that > 95% of normal adult prostate tissue samples, including normal tissue adjacent to tumor, strongly express PAP [5, 11, 12]. Analyses of PAP mRNA levels by RNA blotting methods [13] and quantitative polymerase chain reaction (qPCR) using pooled tissue samples [14] indicate high levels of PAP mRNA expression in normal prostate tissue. PAP has generally been considered a tissue-specific prostate antigen, highly expressed in both normal and malignant prostate cells.
Studies of PAP expression in non-prostate tissues have yielded conflicting results. The majority of these studies used IHC methodology. The studies have generally confirmed that the preponderance of PAP expression is in the prostate, though several studies have noted some extra-prostatic expression. PAP expression has been reported in liver cells, normal adult kidney [11, 15]; granulocytes, parietal cells of the stomach [15]; urethral glands [16, 17]; anal gland non-mucosal epithelium, rectal tissue [16]; salivary glands [18]; and ectopic prostate tissue in both uterine cervix and vagina [19].
In contrast, several studies failed to observe PAP staining in normal tissues, including bladder, breast, colon/rectum, epidermis, kidney, liver, lung, ovary, salivary glands, stomach, testes, and urethra [11, 12, 15, 16]. Using qPCR to measure relative levels of PAP mRNA transcripts, Cunha and colleagues [14] found that, relative to prostate, PAP mRNA was expressed at low levels in several normal tissues, most notably in placenta, kidney, and testis. The kidney expression levels were 192-fold less (0.5%) than those seen in normal prostate tissue. Pancreas, small intestine, leukocytes, lung, ovary, colon, and spleen also exhibited low but detectable levels of PAP mRNA.
Several IHC studies provided evidence for PAP expression in normal pancreatic islet cells. Relative to prostate tissue extracts, normal pancreatic tissue had low but detectable PAP, as measured by electrophoresis [20]. Li and co-workers observed weak occasional PAP IHC staining of pancreatic islets cells [15]. Likewise, Cohen et al. found weak diffuse PAP immunostaining in islets cells, but concluded the weak PAP signal was non-specific [21]. Additional studies have found PAP expressed in normal pancreatic tissue [11, 12, 18].
The correlation between increased PAP serum levels and metastatic prostate cancer has been well established [8]. Detection of PAP in serum was the primary prostate cancer screening test used until the 1990s when it was supplanted by the more sensitive and specific assay for prostate-specific antigen (PSA). There is renewed interest in PAP as a prognostic tissue marker for T4 tumors [22], as a serum marker in clinical staging of prostate cancer [23], and for predicting recurrence after radical prostatectomy [24]. PAP is expressed in > 95% of the primary prostate adenocarcinomas as determined by IHC [11, 12, 15]. Goldstein observed that 80% (176 of 219) of PAP positive prostate adenocarcinomas from patients with Gleason scores of 6 to 10 expressed PAP in more than 25% of the malignant cells [25]. Initial Phase 3 clinical protocols for the autologous cellular immunotherapy sipuleucel-T required subjects to have a tumor specimen submitted to a central pathology facility for IHC testing for PAP expression. Eligibility criteria required PAP expression in ≥ 25% of malignant cells by IHC. Of the 368 castrate resistant prostate cancer (CRPC) patients screened in two Phase 3 clinical trials for sipuleucel-T, 94% of the primary tumor specimens expressed PAP (unpublished results).
Other methods have been used to determine PAP expression in prostate cancer. PAP mRNA was present in a high percentage of prostate adenocarcinomas as determined by Northernblot hybridization methods [26]. PAP peptide specific cytotoxic T lymphocytes (CTLs) were isolated from the peripheral blood mononuclear cells in 4 of 9 patients with prostate cancer but not from 3 healthy donors [27].
Additional IHC studies have suggested PAP expression in non-prostate derived malignancies. PAP staining was observed in Warthan's tumors, mixed carcinomas, and pleomorphic adenomas of the salivary gland [18].
One recent study [28] questioned the specificity of PAP expression in the prostate. This study used RT-PCR to show widespread expression of PAP in mouse tissues, and IHC to demonstrate expression in human skeletal muscle. In addition, this study also suggested that PAP may exist in a form localized to the plasma membrane in addition to its well characterized secreted form.
Because of the disparate results regarding PAP expression reported in the literature, we undertook a series of studies on PAP expression using a variety of methodologies, including IHC, qPCR, in situ hybridization, and virtual Northern analysis. This comprehensive approach has confirmed that while the overwhelming majority of PAP expression is in the prostate, it is possible to observe low levels of PAP expression in several other normal tissues as well. This observation can be put to use in shaping clinical safety monitoring protocols in trials targeting PAP. We also observed that PAP may be expressed in some breast and colon cancers, but at levels considerably lower than that seen in prostate cancer.
Materials and methods
Materials
Antibodies to PAP, Aspergillus niger glucose oxide, vimentin, CD31, and normal rabbit Ig were obtained from Dako North America, Inc. Biotinylated horse anti-mouse IgG, biotinylated goat anti-rabbit IgG, Vectastain ABC-AP (alkaline phosphatase) kit, and Vector Red Substrate Kit were obtained from Vector Laboratories, Inc. PA2024 used for blocking studies is a recombinant fusion protein composed of human PAP linked to human granulocyte-macrophage colony-stimulating factor (GM-CSF), described elsewhere. For qPCR studies, First Choice Human Total RNA Survey Panel and individual total RNA's were obtained from Ambion, Inc. TaqMan reagents were obtained from Applied Biosystems, Incorporated. Other PCR reagents were purchased from Invitrogen Corporation. Oligonucleotide probes were designed and synthesized by GeneDetect. Reagents for hybridization and tyramide-amplification were provided by Dako.
Immunohistochemistry
Immunohistochemistry was performed by Life-Span BioSciences, Inc, Seattle WA. Antibody titration experiments were conducted with an antibody (DAKO, catalog #M0792; mouse monoclonal) to PAP to establish concentrations that would result in minimal background and maximal detection of signal. The antibody concentration chosen for this study was 0.156 μg/ mL. The antibody to PAP was used as the primary antibody, and the principal detection system consisted of a Vector anti-mouse secondary (BA-2000) and a Vector ABC-AP kit (AK-5000) with a Vector Red substrate kit (SK-5100), which produced a fuchsia-colored deposit. Tissues were also stained with positive control antibodies (CD31 and vimentin) to ensure that the tissue antigens were preserved and accessible for IHC analysis. Only tissues that were positive for CD31 and vimentin staining were selected for the remainder of the study. The negative control consisted of performing the entire IHC procedure on adjacent sections in the absence of primary antibody. Slides were imaged with a DVC 1310C digital camera coupled to a Nikon microscope.
A rabbit polyclonal antibody (pAb) against human PAP (N1518, Dako) was optimized in the same manner. Bound antibody was detected with a biotinylated goat anti-rabbit IgG antibody (BA-1000, Vector) and stained as above. The rabbit polyclonal nonspecific control antibody (N1699, Dako) was tested in the same way utilizing the same reagents and used for subsequent experiments neat, as received from the manufacturer. The optimal dilution of rabbit polyclonal anti-human PAP was determined to be 1:8. For blocking experiments, the PAP-specific titer of the polyclonal serum was assumed to be five times higher than that of the monoclonal.
To establish the specificity of the antibodies, blocking experiments were performed using a recombinant protein (PA2024) containing full-length human PAP [29]. The recombinant protein was titrated to determine optimal amounts for specificity studies. Prior to addition of the primary antibodies to the tissues, the antibodies were incubated with PA2024 for 60 minutes at room temperature. Tissue staining was performed as described above. Control samples consisted of staining adjacent serial tissue sections with a) antibody alone at a concentration of 0.146 μg/mL (mAb) or 1:8 (pAb), b) PA2024 in the absence of antibody at the same concentration(s) used for blocking, and c) secondary antibody alone.
Several different malignant human tissues (n = 10 per tissue), and corresponding normal tissues (n = 2 per tissue), were examined by IHC for PAP. In order to visualize potentially weak staining on non-prostate tissue samples, both the mouse anti-PAP mAb and rabbit anti-PAP pAb were used at much higher concentrations (10 μg/mL and undiluted, respectively). Incubation with secondary antibodies and staining procedures were performed as described above.
Only tissues staining positive for CD31 and vimentin were used for the study. Staining frequency and intensity were scored by a pathologist using standard references. Briefly, staining intensity was scored as follows: negative, blush, faint, moderate, and strong staining were scored respectively as 0, 1, 2, 3, and 4. Staining frequency was scored rare (0.1 – 10%), occasional or focal (10 – 30%), frequent (30 – 75%), or most (75 – 90%) as a percentage of all observed cells.
Quantitative polymerase chain reaction
The First Choice Human Total RNA Survey Panel mRNA tissue array (Ambion) and individual total RNAs (Ambion) were used to produce the cDNA in this study. cDNA was produced by random priming, using standard RT-PCR techniques. cDNA was quantified by ultraviolet absorption at 260nm.
Quantitative PCR was accomplished by utilizing the TaqMan technology as described by the vendor. Cycle parameters were as follows: 2 min at 50°C, 10 min at 95°C, then 40 cycles of 15 seconds at 95°C and 1 min at 60°C. Results were analyzed using the ΔΔCT Method [30].
In silico analysis
The National Cancer Institute's Cancer Genome Anatomy Project (CGAP) was utilized for virtual northern analysis of PAP expression using Sequence ID NM_001099 and cluster Hs.433060. http://cgap.nci.nih.gov/Tissues/VirtualNorthern?TEXT=0&ORG=Hs&CID=433060.
In situ hybridization
In situ hybridization was performed by Asterand UK Ltd. Two sense and antisense probes were designed and synthesized by GeneDetect. The antisense probes were designed to hybridize with bases 13-60 (5'-PAP) and 1047-1094 (3'-PAP) of human PAP mRNA (GenBank Accession No. BC016344). The probes were 3'-end labeled with multiple fluorescein residues to facilitate hybrid detection. Probes were hybridized to frozen sections of adenocarcinoma of breast and colon from 10 donors and to normal breast, normal colon, and normal prostate, each from 1 donor.
The in situ hybridization protocol consisted of pre-hybridization, hybridization, post-hybridization, and IHC detection stages. Serial tissue sections (12 μm) were mounted on charged, RNase-free, slides and stored at -70°C prior to use. For assay, the sections were fixed in 4% (w/v) paraformaldehyde (on ice) and washed 3 times in 0.1M phosphate buffer (PB. pH7.4). Endogenous peroxidases were quenched using 0.3% H202 in 0.1M PB and the sections were dehydrated in 100% ethanol and allowed to air dry.
Following air-drying, sections were incubated overnight at 37°C in hybridization buffer containing sense and antisense probes at approximately 25ng/mL. PolyT oligonucleotides were applied at the same concentration but at room temperature.
Following the overnight hybridization, the sections were washed and then incubated in anti-fluorescein-HRP. The sections were washed and then incubated in fluorescyl-tyramide. Following tyramide-mediated amplification, the sections were incubated in a second anti-fluorescein-HRP, rinsed in Tris-buffered saline with 0.05% Tween-20, and then incubated in diaminobenzidine for one minute. Following development of the chromagen, the sections were washed extensively in distilled water, counterstained with hematoxylin, dehydrated, and coverslipped under DePeX [31].
In order to validate the in situ hybridization detection of PAP mRNA in prostate gland, adjacent sections were processed for IHC demonstration of PAP expression.
Results
Immunohistochemistry analyses
PAP expression was easily detected with the monoclonal antibody in normal prostate and prostate carcinoma (Figure 1A and B). Negative control tissues (adrenal and placental) did not show staining with either anti-PAP antibody tested (not shown). In addition, complete elimination of staining for both antibodies was achieved when they were pre-incubated with recombinant PAP (PA2024). Complete elimination was observed for the monoclonal antibody when PA2024 was added at a 1000-fold molar excess (Figure 1C). As expected, sections stained with PA2024 alone were negative (data not shown). Finally, the isotype control antibodies did not show staining of any tissue at any dilutions tested (not shown). Similar results were obtained with the rabbit polyclonal antibody.
Figure 1.
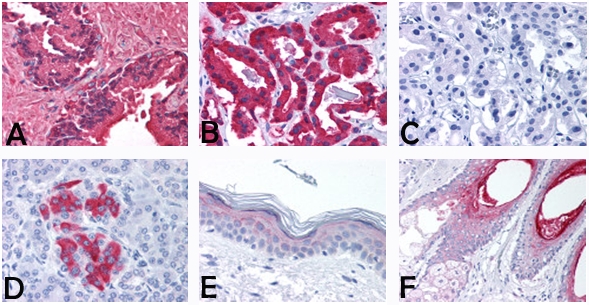
Representative stains of normal and carcinoma tissue. (A) Normal prostate from a 52-year-old male. (B and C) Prostate carcinoma from a 77-year-old male, 40×. Tissues from A, B, and C were stained with mouse anti-PAP mAb, 0.146 μg/mL (1 × 10-9 M); C was additionally preincubated with PA2024, 1:1000 molar ratio. (D) Normal pancreas from a 45-year-old male. (E) Squamous epithelium from a 64-year-old male. (F) Pilosebaceous unit samples from a 53-year-old male. Tissues from D, E, and F were stained with mouse anti-PAP mAb at 10 μg/mL, neat.
The PAP-specific antibodies were evaluated on a limited number of samples of both normal and malignant non-prostate tissues. Detection of PAP in these tissues required much higher antibody concentrations than used for prostate tissues. The distribution of staining observed on each tissue was nearly identical for both antibodies. In addition, the mouse IgG1 isotype control antibody and nonspecific rabbit polyclonal antibody control reagent were tested on the same tissues. As expected, all sections stained with the control antibodies were negative (not shown). Results obtained with both antibodies are summarized in Table 1.
Table 1.
Summary of IHC tissue results
| Antibody: | Mouse anti-PAP mAb M0792 |
|||
|---|---|---|---|---|
| Tissue | PAP Detected/Samples Tested | Intensity | Staining Frequency in Positive Samples | Stained Cell Type |
| Breast | 2/2 | 1 | Occasional | Epithelial |
| Breast, Carcinoma | 0/10 | 0 | N/A | None |
| Colon | 2/2 | 2-3 | Rare | Colonic Neuroendocrine |
| Colon, Carcinoma | 4/10 | 1-2 | Occasional (3/4) or Frequent (1/4) | Malignant |
| Lung | 0/2 | 0 | N/A | None |
| Lung, NSCLC | 2/10 | 1-2 | Occasional | Malignant |
| Ovary | 0/2 | 0 | N/A | None |
| Ovary, Carcinoma | 2/10 | 1-3 | Rare blush (1/2) or Frequent moderate (1/2) | Malignant |
| Pancreas | 2/2 | 2-3 | Rare | Islet cells |
| Pancreas, Carcinoma | 1/10 | 3 | Rare | Residual Islet cells |
| Skin | 2/2 | 1-4 | Frequent | Epidermis and Dermis |
| Prostate | 2/2 | 4 | All | Glandular epithelium and fibromuscular stroma |
| Prostate, Carcinoma | 10/10 | 4 | All | Malignant |
| Antibody: | Rabbit anti-PAP pAb N1518 | |||
| Breast | 0/2 | 0 | N/A | None |
| Breast, Carcinoma | 0/10 | 0 | N/A | None |
| Colon | 2/2 | 2-3 | Rare | Colonic Neuroendocrine |
| Colon, Carcinoma | 3/10 | 1-3 | Rare moderate (1/3) or many faint (2/3) | Malignant cells and Lymphocytes |
| Lung | 0/2 | 0 | N/A | None |
| Lung, NSCLC | 1/10 | 1-3 | Rare | Malignant cells and Lymphocytes |
| Ovary | 0/2 | 0 | N/A | None |
| Ovary, Carcinoma | 3/10 | 2-3 | Rare faint (2/3) or most moderate (1/3) | Malignant |
| Pancreas | 2/2 | 3 | Rare | Islet Cells |
| Pancreas, Carcinoma | 2/10 | 3 | Rare | Residual Islet Cells |
| Skin | 2/2 | 1-4 | Frequent | Epidermis and Dermis |
| Prostate | 2/2 | 4 | All | Glandular epithelium and fibromuscular stroma |
| Prostate, Carcinoma | 10/10 | 4 | All | Malignant |
N/A, not applicable
Weak staining was identified in a subset of pancreatic islet cells (Figure 1D), squamous epithelium (Figure 1E), and the pilosebaceous unit (Figure 1F) as well as in colonic neuroendocrine cells and skin adnexal structures (not shown). With the polyclonal antibody only, rare staining was also present in lymphocytes within malignant tissues (data not shown). Among other cell types, staining was present in 2 of 10 ovarian carcinoma samples (not shown), and in individual malignant cells in lung and colon carcinomas (not shown).
Additional tissues were analyzed using the monoclonal antibody. All remaining tissues included in the study were completely negative, with no background staining. These tissues included bone marrow (0/2), cerebellum (0/2), brain cortex (0/2), pituitary (0/2), brain putamen (0/2), brain vessels (0/4), small artery (0/2), aorta (0/2), carotid artery (0/2), pulmonary artery (0/2), renal artery (0/2), renal vein (0/2), and saphenous vein (0/2).
qPCR
The qPCR method quantifies differences in the mRNA expression level of a specific gene, PAP, normalized to an endogenous control, β-actin. The β-actin and majority of PAP Cycle Threshold (CT) values are below 35, therefore, small fold changes can be statistically significant (Applied BioSystems). The tissue with the lowest PAP mRNA level is arbitrarily set to a value of 1, in this case normal liver, and all other values are indexed to this level. The PAP mRNA expression value for normal prostate was 5525, and all expression ratios were calculated relative to this value. Results for all analyzed tissues are summarized in Table 2. Among the normal tissues surveyed, bladder expressed PAP mRNA at a highest ratio relative to prostate, though the observed expression level was still 50-fold less than that observed in the prostate. The calculated ratio of normal prostate PAP mRNA to normal kidney PAP mRNA was 178, which is comparable to the ratio of 192 reported in the literature [14]. Among the tumor samples tested, the cervical tumor sample expressed PAP mRNA at levels similar to that seen in the normal bladder, though again at levels some 50-fold less than that observed in the normal prostate. PAP mRNA levels in the PAP tumor samples were elevated relative to the normal prostate tissue by a factor of about 2.4; this result is in general agreement both with previous reports and with the relatively higher signal strength observed in the IHC study above.
Table 2.
qPCR relative values of PAP mRNA expression and percent of normal prostate expression
| Normal |
Tumor |
|||||
|---|---|---|---|---|---|---|
| Tissue | mRNA Expression Value | % of Normal Prostate | Samples Tested | mRNA Expression Value | % of Normal Prostate | Samples Tested |
| Breast | 4 | 0.07 | 1 | 7 | 0.13 | 1 |
| Bladder | 115 | 2.08 | 3 | 12 | 0.22 | 1 |
| Cervix | 12 | 0.22 | 4 | 116 | 2.09 | 1 |
| Colon | 4 | 0.07 | 3 | 6 | 0.11 | 1 |
| Kidney | 31 | 0.56 | 3 | 11 | 0.19 | 1 |
| Liver | 1 | 0.02 | 3 | 2 | 0.04 | 1 |
| Lung | 8 | 0.14 | 3 | 24 | 0.43 | 1 |
| Ovary | 8 | 0.14 | 3 | 22 | 0.39 | 1 |
| Pancreas | 16 | 0.28 | 1 | 5 | 0.09 | 1 |
| Prostate | 5525 | 100.00 | 3 | 13264 | 240.07 | 1 |
| Testes | 12 | 0.22 | 3 | 11 | 0.19 | 1 |
In silico analysis
The EST Virtual Northern composite was derived from databases at CGAP for PAP sequence (NCBI accession number NM_001099). The PAP gene was found in cDNA libraries from several normal and/or malignant tissue types. For each combination of tissue and histology, expression was computed by dividing the number of EST tags representing the gene by the total number of EST tags in all libraries with the given tissue/ histology. This ratio was then multiplied by 200,000, giving the number of EST tags per 200,000. This number is presented along with the relative percent expression compared to normal prostate in Table 3 for selected tissues.
Table 3.
PAP-specific EST transcripts per 200,000
| Tissues | Value | % of Normal Prostate | Value | % of Normal Prostate |
|---|---|---|---|---|
| All tissues | 21.2 | 2.7 | 16.8 | 2.2 |
| Colon | 0 | 0 | 6.5 | 0.8 |
| Breast | 0 | 0 | 79.2 | 10.2 |
| Muscle | 42.2 | 5.4 | 0 | 0 |
| Ovary | 17.3 | 2.2 | 0 | 0 |
| Pancreas | 0 | 0 | 0 | 0 |
| Pancreatic Islet | 12.2 | 1.6 | 0 | 0 |
| Prostate | 774.5 | 100.0 | 257.3 | 33.2 |
| Salivary Gland | 79.5 | 10.2 | 0 | 0 |
| Skin | 2.7 | 0.3 | 0 | 0 |
Interestingly, in silico analysis indicated a slight decrease in PAP expression in prostate cancer, somewhat at odds with results obtained in the other analyses. In no case was PAP seen to be up- or down-regulated in prostate cancer vs. healthy prostate tissue; the variation seen here may represent a systematic experimental variable, such as the difficulty in obtaining pure tissue for analysis, or the relative stability of the PAP mRNA in different environments.
In situ hybridization
Relatively high PAP EST levels in breast and colon carcinoma led us to conduct a more detailed examination of PAP mRNA expression in these tissues by in situ analysis. Sense and antisense oligonucleotide probes designed to the 5’ and 3’ regions of human PAP mRNA were hybridized to frozen sections of adenocarcinoma of breast and colon from 10 donors and to normal breast, normal colon, and normal prostate, each from one donor.
The intensities of the hybridization signals have been summarized in Table 4 using a simple color code, where the increasing darkness of blue indicates the intensity of the hybridization signals.
Table 4.
Intensity of PAP mRNA hybridization in normal versus tumor tissue
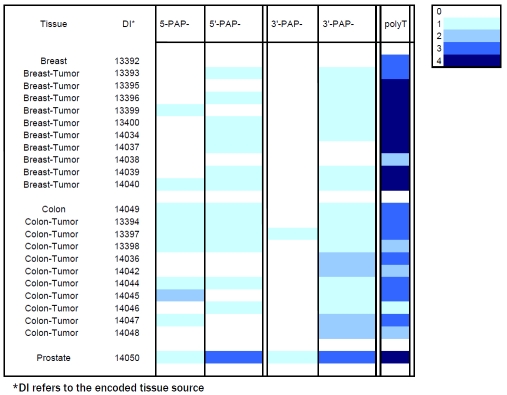 |
In the sections of prostate gland, expression of PAP mRNA was found to be largely restricted to the glandular and ductal epithelial cells and the level of expression was moderately high (Figure 2A and B).
Figure 2.
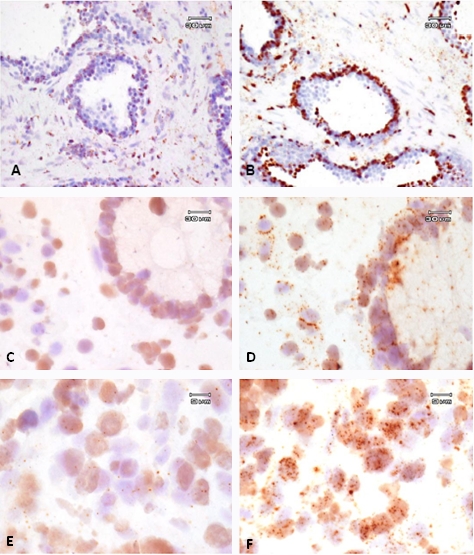
Representative in situ hybridization of PAP mRNA. High power photomicrographs (60×) showing expression of PAP mRNA in the glandular epithelium of a normal prostate gland from sample DI 14050 (A and B), mucosal epithelial cells of normal colon from sample DI 14049 (C and D), or cells within a caecal/colon adenocarcinoma from sample DI 14047 (E and F). Hybridization signals resulting from the incubation of the tissue sections with sense (A, C) and antisense (B, D) from the 5’ (A-B) probe set. 3’ probes gave similar results (not shown).
In the normal breast and colon the level of PAP mRNA expression, relative to the expression in normal prostate, was found to be very low. Similarly, in the samples of breast and colon adenocarcinoma, expression of PAP mRNA, although detected in the majority of tumor cells, was very low. Representative photomicrographs of normal colon (Panels C and D) and colon adenocarcinoma (Panels E and F) are shown in Figure 2; similar results were obtained in normal and cancerous breast tissue (not shown). Some nonspecific staining was visible in several tissues (Panels A, C, and E of Figure 2) and this is attributed to an interaction between the in situ detection reagents and the acellular collagen matrix.
As expected, the polyT hybridizations were more intense than either PAP antisense probes but varied between tumor types and between donors within the same tissue group. PolyT hybridization appeared to be higher in the breast tumor than in the colon tumor samples. Generally, sense probe hybridizations resulted in lower levels of staining than antisense hybridizations. The intensity of the sense probe hybridizations appeared to be lower with the 3'-probe compared with the 5'- probe. With the exception of the prostate gland, where expression was found to be moderately high, the intensity of the antisense hybridizations was low in both breast and colon tumor tissues.
Discussion
PAP is expressed at moderate to high levels in both normal and malignant prostate tissue, as determined by all methods described in this document.
Our observations confirm previous reports of PAP expression in a limited set of non-prostate normal tissues. The level of PAP expression in these tissues appears substantially less than the levels found in normal and malignant prostate. This conclusion is based on data from IHC of tissue samples, qPCR of mRNA isolated from human tissues, in silico analyses of CGAP EST and SAGE tag libraries, and in situ analysis of PAP mRNA expression in breast and colon carcinoma tissues.
The current study corroborates the findings of Li and co-workers [15] describing weak PAP staining of pancreatic islet cells relative to normal prostate. To our knowledge, this is the first report of expression of PAP in the pilosebaceous units of normal skin by IHC. PAP staining by IHC in non-prostate tissues was weak relative to levels observed in the prostate, and confined to only a few cells where observed. Moreover, the IHC data for non -prostate tissues presented here was collected using high concentrations of anti-PAP antibodies in order to detect weak signals. The staining observed in pancreatic islets and the pilosebaceous units of skin may have overemphasized relatively weak signals. Low level PAP expression was also observed in 2 of 10 ovarian and 3 of 10 colon carcinoma samples.
Published qPCR data suggested a hierarchical tissue distribution of PAP mRNA expression in normal tissue: prostate>>placenta > kidney >testis > pancreas > small intestine = leukocytes > lung > ovary [14]. The qPCR data presented here suggest a similar hierarchical tissue distribution of PAP mRNA: prostate>>bladder > kidney > pancreas > cervix = testis > lung = ovary. PAP mRNA in normal bladder was just over 2% of the level found in normal prostate.
The EST data presented here suggest a hierarchical tissue distribution of PAP mRNA expression: prostate > prostate cancer >> mammary gland cancer > normal salivary gland > normal ovary > normal pancreatic islet cells > colon cancer > normal skin. Expression of PAP mRNA in normal pancreatic islets was 1.5% of expression in normal prostate. Expression of PAP mRNA in breast cancer was 18.8% of that found in normal prostate. Note that EST databases are not fully curated, and the variety of experimental approaches makes accurate determination of expression levels from these databases problematic. In conjunction with other analytical approaches, however, they form a powerful correlative tool for determination of mRNA tissue distribution.
PAP mRNA is expressed in the epithelial cells lining the prostatic glands and ducts, consistent with the immunohistochemical analysis of PAP expression (see Figure 1). That the cellular distribution of PAP in normal and tumor tissues is at a very similar level is not unexpected as adenocarcinoma has an epithelial origin. In normal breast and colon, expression of PAP mRNA was very low. In both tissues, the expression of PAP mRNA was associated with ductal epithelial (breast) and mucosal epithelial cells (colon). The expression of PAP mRNA was also very low in all the samples of breast and colon adenocarcinoma analyzed. Expression was detected in the majority of tumor cells, but at a level close to that predicted to be the maximum sensitivity of the assay.
The data reported in this study are broadly consistent with the limited public information on the PAP expression in human cancers. The discrepancy with regard to expression in breast and colon carcinoma between the in silico and in situ analyses may reflect a difference in the reported PAP expression between tissues and cell lines. Wang et al [32] describe the expression of PAP mRNA and protein in a wide variety of adenocarcinoma cell lines (including breast and colon), but Solin et al [13], Kidwai et al [33], and Azumi et al [34] found that PAP was undetectable in breast and colon cancer tissues. In the present study we report that both breast and colon adenocarcinoma show very low levels of PAP mRNA expression, perhaps reflecting the sensitivity of the in situ hybridization method selected for this project, compared with more traditional target localization approaches.
The specificity of PAP expression in prostate tissues, while not absolute, supports its use in immunotherapies targeting prostate carcinoma. Interestingly, a review of the Phase 3 clinical safety profile of sipuleucel-T suggests no indication of immunotoxicity directed to other tissues that may express PAP. It is clear that the tissue distribution of PAP expression is different between mouse and man, and caution should be used in using mouse studies to predict human expression of this protein [28]. A greater knowledge of the human tissue distribution of immunotherapy targets will help in designing clinical safety protocols for monitoring adverse events associated with the use of these therapeutic regimens and, while the expression of PAP in other malignancies might be too low to serve as a target for PAP specific immunotherapies, such studies serve to help identify additional clinical indications for such approaches to cancer treatment.
Understanding the tissue distribution of targets for therapeutic intervention is key to understanding both the range and limitations of the proposed treatment. Tissue distribution can be addressed by a number of experimental approaches. While each approach can be powerful, each is also subject to artifact or limitations in interpretability. The approach described here, involving the use of multiple correlates of tissue-specific expression, is warranted as a prerequisite in selecting suitable pharmaceutical targets.
Sipuleucel-T is an autologous cellular immunotherapy that targets PAP as a treatment for advanced prostate cancer, and has demonstrated evidence of survival prolongation in men with asymptomatic or minimally symptomatic metastatic castrate resistant prostate cancer in randomized controlled Phase 3 clinical trials [3, 4]. We employed 4 independent approaches to study the distribution of PAP in normal and malignant tissues. The observed range of distribution varies somewhat depending on the technique used, but all methods converge on the conclusion that PAP is expressed in both normal and malignant prostate tissue to a significantly greater degree than is observed in any other tissue type.
Acknowledgments
This work was funded by Dendreon Corporation. We are indebted to David Urdal, PhD, Nicole Provost, PhD, and Mark Frohlich, MD for helpful conversations, to Robert Sims, MD for study design contributions, and to Kim Miller for writing assistance on behalf of Dendreon Corporation.
References
- 1.Stern M, Herrmann R. Overview of monoclonal antibodies in cancer therapy: present and promise. Crit Rev Oncol Hematol. 2005;54:11–29. doi: 10.1016/j.critrevonc.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Huber CH, Wolfel T. Immunotherapy of cancer: from vision to standard clinical practice. J Cancer Res Clin Oncol. 2004;130:367–374. doi: 10.1007/s00432-004-0550-2. [DOI] [PubMed] [Google Scholar]
- 3.Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, Redfern CH, Ferrari AC, Dreicer R, Sims RB, Xu Y, Frohlich MW, Schellhammer PF. Sipuleucel-T Immunotherapy for Castration-Resistant Prostate Cancer. N Engl J Med. 2010;363:411–422. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 4.Small EJ, Schellhammer PF, Higano CS, Redfern CH, Nemunaitis JJ, Valone FH, Verjee SS, Jones LA, Hershberg RM. Placebo-controlled phase III trial of immunologic therapy with sipuleucel-T (APC8015) in patients with metastatic, asymptomatic hormone refractory prostate cancer. J Clin Oncol. 2006;24:3089–3094. doi: 10.1200/JCO.2005.04.5252. [DOI] [PubMed] [Google Scholar]
- 5.Goldfarb DA, Stein BS, Shamszadeh M, Petersen RO. Age-related changes in tissue levels of prostatic acid phosphatase and prostate specific antigen. J Urol. 1986;136:1266–1269. doi: 10.1016/s0022-5347(17)45310-9. [DOI] [PubMed] [Google Scholar]
- 6.Yam LT. Clinical significance of the human acid phosphatases: a review. Am J Med. 1974;56:604–616. doi: 10.1016/0002-9343(74)90630-5. [DOI] [PubMed] [Google Scholar]
- 7.Ronnberg L, Vihko P, Sajanti E, Vihko R. Clomiphene citrate administration to normogo-nadotropic subfertile men: blood hormone changes and activation of acid phosphatase in seminal fluid. Int J Androl. 1981;4:372–378. doi: 10.1111/j.1365-2605.1981.tb00721.x. [DOI] [PubMed] [Google Scholar]
- 8.Ahmann FR, Schifman RB. Prospective comparison between serum monoclonal prostate specific antigen and acid phosphatase measurements in metastatic prostatic cancer. J Urol. 1987;137:431–434. doi: 10.1016/s0022-5347(17)44057-2. [DOI] [PubMed] [Google Scholar]
- 9.Simsek U, Kutlu S, Yavascaouglu I, Oktay B, Ozyurt M. Seasonal variation of prostatic acid phosphate and prostate-specific antigen in patients without prostatic malignancy. Eur Urol. 1992;21(Suppl 1):111–114. doi: 10.1159/000474906. [DOI] [PubMed] [Google Scholar]
- 10.Robles JM, Morell AR, De Torres JA, Rosello AS. Clinical behavior of prostatic specific antigen and prostatic acid phosphatase: a comparative study. Int J Biol Markers. 1989;4:87–94. doi: 10.1177/172460088900400205. [DOI] [PubMed] [Google Scholar]
- 11.Haines AM, Larkin SE, Richardson AP, Stirling RW, Heyderman E. A novel hybridoma antibody (PASE/4LJ) to human prostatic acid phosphatase suitable for immunohistochemistry. Br J Cancer. 1989;60:887–892. doi: 10.1038/bjc.1989.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jobsis AC, De Vries GP, Meijer AE, Ploem JS. The immunohistochemical detection of prostatic acid phosphatase: its possibilities and limitations in tumour histochemistry. Histochem J. 1981;13:961–973. doi: 10.1007/BF01002636. [DOI] [PubMed] [Google Scholar]
- 13.Solin T, Kontturi M, Pohlmann R, Vihko P. Gene expression and prostate specificity of human prostatic acid phosphatase (PAP): evaluation by RNA blot analyses. Biochim Biophys Acta. 1990;1048:72–77. doi: 10.1016/0167-4781(90)90024-v. [DOI] [PubMed] [Google Scholar]
- 14.Cunha AC, Weigle B, Kiessling A, Bachmann M, Rieber EP. Tissue-specificity of prostate specific antigens: comparative analysis of transcript levels in prostate and non-prostatic tissues. Cancer Lett. 2006;236:229–238. doi: 10.1016/j.canlet.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 15.Li CY, Lam WK, Yam LT. Immunohistochemical diagnosis of prostatic cancer with metastasis. Cancer. 1980;46:706–712. doi: 10.1002/1097-0142(19800815)46:4<706::aid-cncr2820460412>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 16.Kamoshida S, Tsutsumi Y. Extraprostatic localization of prostatic acid phosphatase and prostate-specific antigen: distribution in cloacogenic glandular epithelium and sex-dependent expression in human anal gland. Hum Pathol. 1990;21:1108–1111. doi: 10.1016/0046-8177(90)90146-v. [DOI] [PubMed] [Google Scholar]
- 17.Tepper SL, Jagirdar J, Heath D, Geller SA. Homology between the female paraurethral (Skene's) glands and the prostate. Immunohistochemical demonstration. Arch Pathol Lab Med. 1984;108:423–425. [PubMed] [Google Scholar]
- 18.Elgamal AA, Ectors NL, Sunardhi-Widyaputra S, Van Poppel HP, Van Damme BJ, Baert LV. Detection of prostate specific antigen in pancreas and salivary glands: a potential impact on prostate cancer overestimation. J Urol. 1996;156:464–468. doi: 10.1097/00005392-199608000-00040. [DOI] [PubMed] [Google Scholar]
- 19.McCluggage WG, Ganesan R, Hirschowitz L, Miller K, Rollason TP. Ectopic prostatic tissue in the uterine cervix and vagina: report of a series with a detailed immunohistochemical analysis. Am J Surg Pathol. 2006;30:209–215. doi: 10.1097/01.pas.0000180446.17517.b8. [DOI] [PubMed] [Google Scholar]
- 20.Lam KW, Li O, Li CY, Yam LT. Biochemical properties of human prostatic acid phosphatase. Clin Chem. 1973;19:483–487. [PubMed] [Google Scholar]
- 21.Cohen C, Bentz MS, Budgeon LR. Prostatic acid phosphatase in carcinoid and islet cell tumors. Arch Pathol Lab Med. 1983;107:277. [PubMed] [Google Scholar]
- 22.Grande M, Carlstrom K, Lundh-Rozell B, Stege R, Pousette A. Changes in tissue prostatic acidic phosphatase during endocrine treatment of patients with prostatic carcinoma. Scand J Urol Nephrol. 2005;39:393–398. doi: 10.1080/00365590500193304. [DOI] [PubMed] [Google Scholar]
- 23.Merrick GS, Butler WM, Wallner KE, Allen Z, DeFilippo JL, Adamovich E. Enzymatic prostatic acid phosphatase in the clinical staging of patients diagnosed with prostate cancer. W V Med J. 2005;101:116–119. [PubMed] [Google Scholar]
- 24.Moul JW, Connelly RR, Perahia B, McLeod DG. The contemporary value of pretreatment prostatic acid phosphatase to predict pathological stage and recurrence in radical prostatectomy cases. J Urol. 1998;159:935–940. [PubMed] [Google Scholar]
- 25.Goldstein NS. Immunophenotypic characterization of 225 prostate adenocarcinomas with intermediate or high Gleason scores. Am J Clin Pathol. 2002;117:471–477. doi: 10.1309/G6PR-Y774-X738-FG2K. [DOI] [PubMed] [Google Scholar]
- 26.Hakalahti L, Vihko P, Henttu P, Autio-Harmainen H, Soini Y, Vihko R. Evaluation of PAP and PSA gene expression in prostatic hyperplasia and prostatic carcinoma using northern-blot analyses, in situ hybridization and immunohistochemical stainings with monoclonal and bispecific antibodies. Int J Cancer. 1993;55:590–597. doi: 10.1002/ijc.2910550413. [DOI] [PubMed] [Google Scholar]
- 27.Inoue Y, Takaue Y, Takei M, Kato K, Kanai S, Harada Y, Tobisu K, Noguchi M, Kakizoe T, Itoh K, Wakasugi H. Induction of tumor specific cytotoxic T lymphocytes in prostate cancer using prostatic acid phosphatase derived HLA-A2402 binding peptide. J Urol. 2001;166:1508–1513. [PubMed] [Google Scholar]
- 28.Quintero IB, Araujo CL, Pulkka AE, Wirkkala RS, Herrala AM, Eskelinen EL, Jokitalo E, Hellstrom PA, Tuominen HJ, Hirvikoski PP, Vihko PT. Prostatic acid phosphatase is not a prostate specific target. Cancer Res. 2007;67:6549–6554. doi: 10.1158/0008-5472.CAN-07-1651. [DOI] [PubMed] [Google Scholar]
- 29.Burch PA, Breen JK, Buckner JC, Gastineau DA, Kaur JA, Laus RL, Padley DJ, Peshwa MV, Pitot HC, Richardson RL, Smits BJ, Sopapan P, Strang G, Valone FH, Vuk-Pavlovic S. Priming tissue-specific cellular immunity in a phase I trial of autologous dendritic cells for prostate cancer. Clin Cancer Res. 2000;6:2175–2182. [PubMed] [Google Scholar]
- 30.Bookout AL, Cummins CL, Mangelsdorf DJ, Pesola JM, Kramer MF. High-throughput real-time quantitative reverse transcription PCR. Curr Protoc Mol Biol. 2006 doi: 10.1002/0471142727.mb1508s73. Chapter 15: Unit 15 18. [DOI] [PubMed] [Google Scholar]
- 31.van de Corput MP, Dirks RW, van Gijlswijk RP, van de Rijke FM, Raap AK. Fluorescence in situ hybridization using horseradish peroxidase-labeled oligodeoxynucleotides and tyramide signal amplification for sensitive DNA and mRNA detection. Histochem Cell Biol. 1998;110:431–437. doi: 10.1007/s004180050304. [DOI] [PubMed] [Google Scholar]
- 32.Wang Y, Harada M, Yano H, Ogasawara S, Takedatsu H, Arima Y, Matsueda S, Yamada A, Itoh K. Prostatic acid phosphatase as a target molecule in specific immunotherapy for patients with nonprostate adenocarcinoma. J Immunother. 2005;28:535–541. doi: 10.1097/01.cji.0000175490.26937.22. [DOI] [PubMed] [Google Scholar]
- 33.Kidwai N, Gong Y, Sun X, Deshpande CG, Yeldandi AV, Rao MS, Badve S. Expression of androgen receptor and prostate-specific antigen in male breast carcinoma. Breast Cancer Res. 2004;6:R18–23. doi: 10.1186/bcr733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azumi N, Traweek ST, Battifora H. Prostatic acid phosphatase in carcinoid tumors. Immunohistochemical and immunoblot studies. Am J Surg Pathol. 1991;15:785–790. doi: 10.1097/00000478-199108000-00009. [DOI] [PubMed] [Google Scholar]


