Abstract
Co-infections contribute to HIV-related pathogenesis and often increase viral load in HIV-infected people. We did a systematic review to assess the effect of treating key co-infections on plasma HIV-1-RNA concentrations in low-income countries. We identified 18 eligible studies for review: two on tuberculosis, two on malaria, six on helminths, and eight on sexually transmitted infections, excluding untreatable or non-pathogenic infections. Standardised mean plasma viral load decreased after the treatment of co-infecting pathogens in all 18 studies. The standardised mean HIV viral-load difference ranged from −0·04 log10 copies per mL (95% CI −0·24 to 0·16) after syphilis treatment to −3·47 log10 copies per mL (95% CI −3·78 to −3·16) after tuberculosis treatment. Of 14 studies with variance data available, 12 reported significant HIV viral-load differences before and after treatment. Although many of the viral-load reductions were 1·0 log10 copies per mL or less, even small changes in plasma HIV-RNA concentrations have been shown to slow HIV progression and could translate into population-level benefits in lowering HIV transmission risk.
Introduction
Sustainable and affordable therapeutic and preventive strategies for HIV and AIDS in settings with limited health-care resources represent a formidable public health challenge. Despite widespread implementation of antiretroviral therapy programmes, medications were inaccessible or not yet indicated for 71% of the world’s HIV-infected people at the end of 2008.1 Antiretroviral therapy improves HIV prognosis and reduces infectiousness through the reduction of plasma and genital viral load. However, treatment requires a life-long, daily regimen supported by periodic laboratory tests to monitor the efficacy and toxicity of treatment. Furthermore, patients without opportunistic infections and with higher CD4 cell counts (ie, >350×106/L) might be advised to defer antiretroviral therapy in settings with limited health-care resources. Thus, there remains a compelling imperative to prevent HIV transmission and to improve the prognosis of individuals infected with HIV in settings where antiretroviral therapy is either not yet available or indicated.
In the 1980s, before the era of antiretroviral therapy, much attention was given to HIV co-infections and their effect on host immunity.2 In-vitro data early in the HIV epidemic showed that infections endemic to low-income countries upregulate HIV transcription and robustly activate cellular immunity.3–6 Subsequent human studies have suggested that treatment of co-infections could translate into small HIV viral-load reductions.7–12 A greater focus on co-infections among patients not yet on antiretroviral therapy is warranted for several reasons: there is a high burden of co-infections in HIV-endemic zones; many co-infections non-specifically activate host immunity;6,13–17 some organisms can directly facilitate HIV replication;18,19 and small HIV viral-load reductions could translate into benefits in disrupting viral transmission and improving AIDS-free survival.20
Despite increasing evidence for its salience to HIV outcomes, the effect of co-infection clearance on HIV viral load has not yet been systematically reviewed or quantitatively summarised. We therefore did a systematic review of published studies that assess the effect of treating co-infections that are common in low-income countries on plasma concentrations of HIV-1 RNA, a primary surrogate for HIV transmission risk and disease progression.
Methods
Search strategy
We searched PubMed, Medline, AEGIS, Embase, and LILACS databases for studies published between Jan 1, 1987, and April 1, 2010, and available conference proceedings from the American Society of Tropical Medicine and Hygiene (2004–09), International AIDS Society (1987–2009), and the Conference on Retroviruses and Opportunistic Infections (1997–2010). In our search, we used permutations of key terms including “HIV”, “RNA”, “viral load”, “co-infection”, and “treatment”, as well as those specific infections endemic to low-income countries and those commonly studied in the context of HIV co-infection: “tuberculosis”, “malaria”, “helminth”, “hepatitis”, “herpes”, “HTLV”, “cytomegalovirus”, “leishmania”, “sexually transmitted infection”, “gonorrhea”, “chlamydia”, “syphilis”, “pneumonia”, “influenza”, “measles”, “chagas”, “trypanosome”, and “dengue”. Additional references were identified from bibliographies of published manuscripts included in our review. All populations, languages, and ages of patients were included.
Selection criteria
We followed QUOROM (Quality of Reporting of Meta-analyses), PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses), and STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines of the Cochrane Collaboration for the meta-analysis and review of randomised trials and observational studies.21–23 Our initial search included all human studies that assessed the effect of co-infection treatment on changes in plasma HIV-RNA concentrations. Studies were eligible for inclusion in our final analysis if they were prospective (randomised or non-randomised), contained a comparator group, and presented plasma viral-load data for patients before and after treatment of co-infection. We did not study co-infections that are untreatable or non-pathogenic, such as GB virus type C. We excluded crosssectional studies, case studies, case series, and all other studies that did not follow plasma viral load prospectively or have a comparison group. We also excluded studies that used comparison groups that comprised co-infected participants who did not respond to treatment. We only reviewed articles published since 1987, when reliable and reproducible HIV-RNA assays were first available. We grouped studies according to the type of co-infection assessed. We assessed the primary outcome—viral-load change after successful treatment of co-infection—at the longest follow-up reported in each study. We log-transformed viral-load measures at all data points, if not already done in the studies reviewed. We used a linear model to assess the contribution of publication bias and found no significant effect on the data for this review (data not shown).
Data abstraction and synthesis
Two reviewers (KM and SV) identified eligible studies, abstracted relevant data, and then verified outcomes and analyses with each another. No discrepancies were identified between the two reviewers. We abstracted the following data: authors, year of publication, co-infection type and treatment, population type and study setting, study design, sample size, mean CD4-cell count of the study population, and magnitude and direction of viral-load change on co-infection acquisition or clearance. Our primary outcome of interest was the effect of co-infection treatment on plasma HIV-RNA concentration. Secondary outcome measures included clinical disease progression and mortality. The primary outcome was continuous and assessed with a standardised mean difference (SMD) and corresponding 95% CI. The mean difference was standardised according to the SD of the control population because pooled variance data were not available for most studies. Unpublished data were requested from the investigators if required, primarily for the purpose of calculating SMDs. Given the heterogeneity between studies in type of co-infection, population, and design, we did not pool outcomes nor calculate summary estimates.
Results
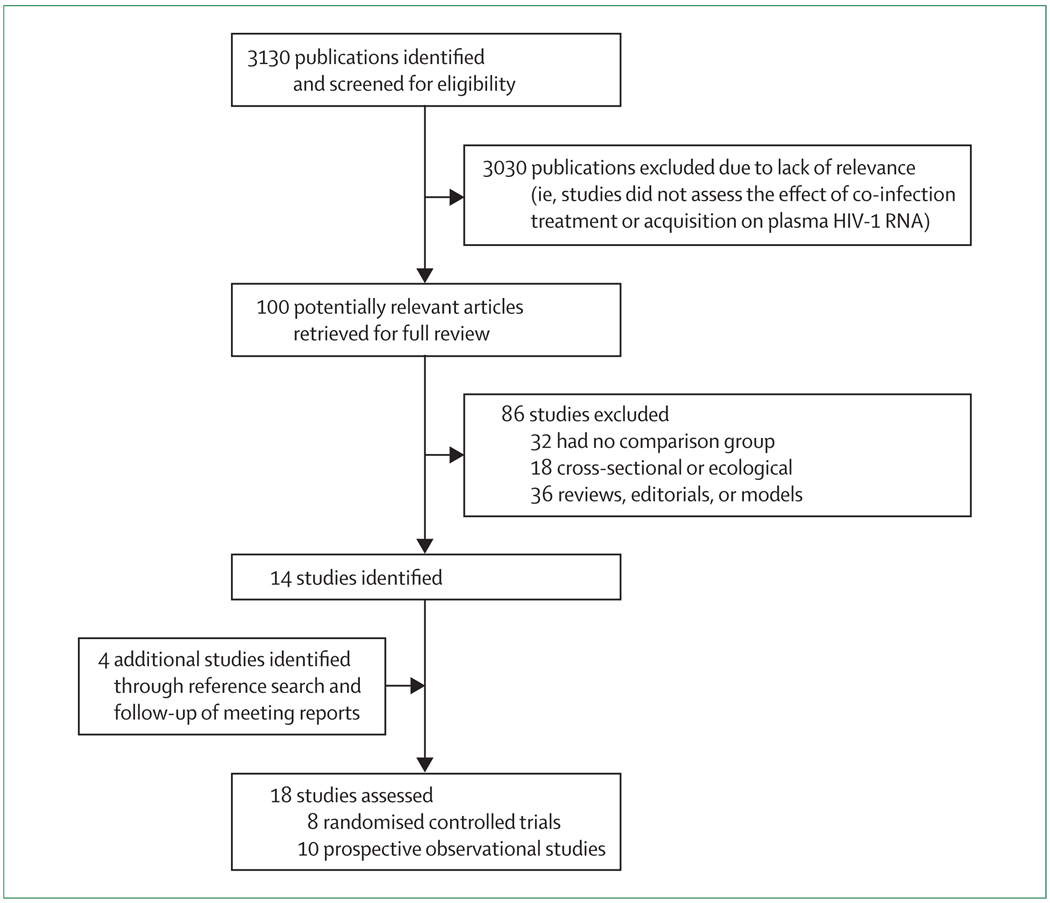
The search yielded 3130 articles, of which 100 were relevant for full review and 14 were eligible for inclusion.6,7,10–12,24–32 Four additional studies were identified by cross-referencing bibliographies of all potentially relevant articles or following up meeting reports.33–36 Of the 18 eligible studies, ten were observational6,10–12,24,28–30,32,34 and eight were randomised controlled trials (figure 1).7,25–27,31,33,35,36 Unpublished data were requested from the investigators for ten of the 18 studies.10–12,24–27,33,34,36 All ten investigators responded and six provided the requested data,12,25–27,33,34 including means and SDs for viral-load assessments. For the four studies for which variance data were not available,10,11,24,36 we constructed 95% CIs based on the weighted mean variability of the 14 other studies.6,7,12,25–35
Figure 1.
Flow chart of study selection
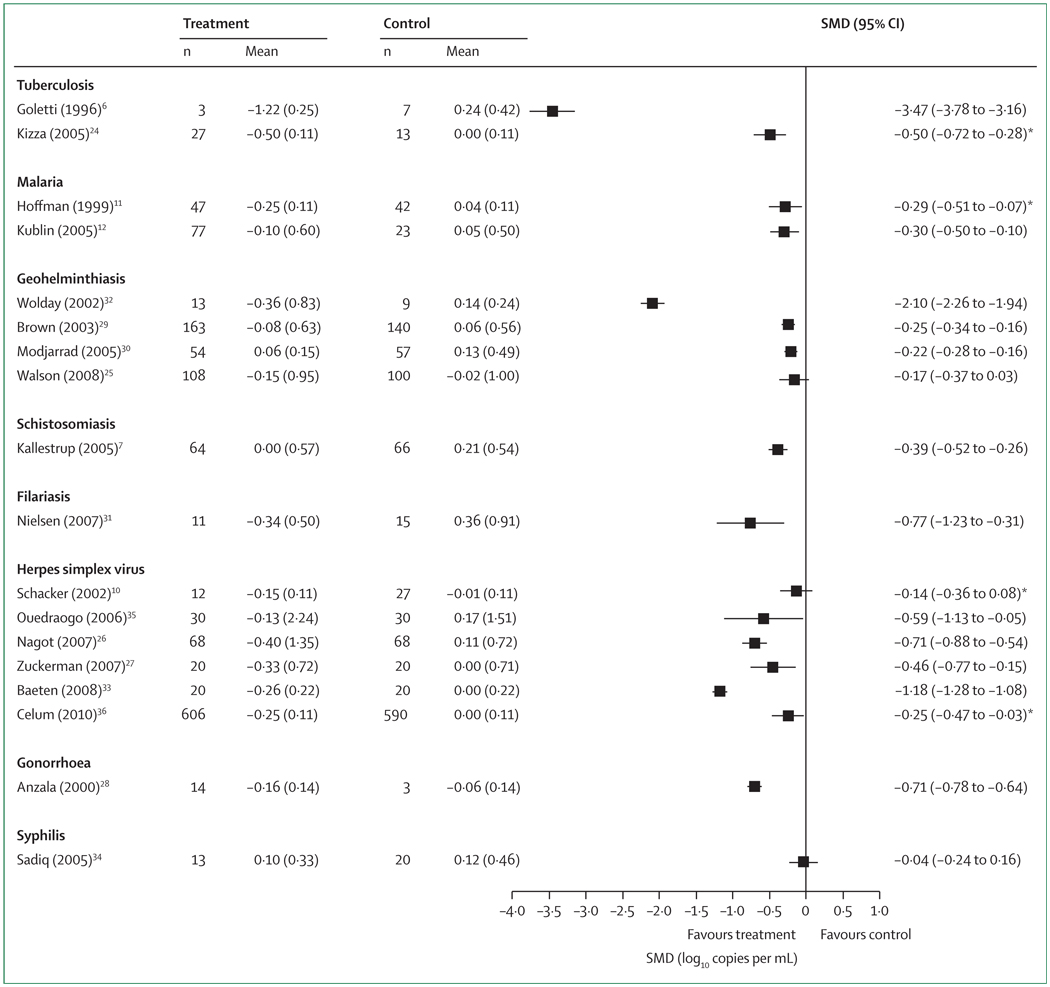
We stratified eligible studies according to the primary pathogens or infectious diseases that were treated: two studies on tuberculosis,6,24 two on malaria,11,12 four on intestinal helminths,25,29,30,32 one on schistosomiasis,7 one on filariasis,31 six on herpes simplex virus (HSV),10,26,27,33,35,36 one on gonorrhoea,28 and one on syphilis.34 All studies were entirely or predominantly among antiretroviral-naive adults. Mean or median CD4-cell counts across study populations ranged from 228×106/L to 577×106/L (table). Follow-up time after treatment of co-infection ranged from 2 weeks to 24 months. Although viral load was a primary or co-primary outcome in all 18 studies, most also assessed the effect of co-infection or treatment of co-infection on other immunological, virological, and clinical outcomes. Standardised mean plasma viral load decreased after the treatment of co-infecting pathogens in all studies included in our analysis (figure 2). The SMD ranged from −0·04 log10 copies per mL after syphilis treatment to −3·47 log10 copies per mL in one study of tuberculosis treatment. Of the 14 studies that had variance data available,6,7,12,25–35 all but two studies25,35 reported significant differences in HIV viral load before and after treatment.
Table.
Characteristics of study populations from the 18 studies included in the systematic review
| Study design | Duration of follow-up (months) |
Sample size (N) |
CD4-cell count (×106/L)* |
HIV viral-load assay | Other prospective data | |
|---|---|---|---|---|---|---|
| Tuberculosis | ||||||
| Goletti (1996)6 | Cohort | 10 | 10 | 560 | bDNA | CD4 cells, CD25, interleukin 2 |
| Kizza (2005)24 | Cohort | 6 | 40 | 220 | RT-PCR | TNF, neopterin, CD14, interleukin 6 |
| Malaria | ||||||
| Hoffman (1999)11 | Cohort | 1 | 89 | 163 | NASBA | TNF |
| Kublin (2005)12 | Cohort | 2 | 100 | 345 | RT-PCR | ‥ |
| Geohelminthiasis | ||||||
| Wolday (2002)32 | Cohort | 6 | 22 | 265 | RT-PCR | CD4 cells, HLA-DR |
| Brown (2003)29 | Cohort | 6 | 303 | 263 | bDNA | CD4 cells, mortality |
| Modjarrad (2005)30 | Cohort | 4 | 111 | 322 | bDNA | CD4 and CD8 cells |
| Walson (2008)25 | RCT | 3 | 208 | 557 | RT-PCR | CD4 cells |
| Schistosomiasis | ||||||
| Kallestrup (2005)7 | RCT | 3 | 130 | 386 | RT-PCR | CD4 cells |
| Filariasis | ||||||
| Nielsen (2007)31 | Crossover RCT | 6 | 26 | 27% | RT-PCR | CD4 and CD8 cells |
| Herpes simplex virus | ||||||
| Schacker (2002)10 | Cohort | 5 | 39 | 313 | bDNA | ‥ |
| Ouedraogo (2006)35 | RCT | 3 | 60 | 228 | RT-PCR | Genital HIV RNA |
| Nagot (2007)26 | RCT | 3 | 136 | 446 | RT-PCR | Genital HIV RNA |
| Zuckerman (2007)27 | Crossover RCT | 2 | 40 | 406 | RT-PCR | CD4 cells, rectal HIV RNA |
| Baeten (2008)33 | Crossover RCT | 2 | 40 | 372 | RT-PCR | Cervical HIV RNA |
| Celum (2010)36 | RCT | 24 | 1196 | 470 | RT-PCR | HIV transmission |
| Gonorrhea | ||||||
| Anzala (2000)28 | Cohort | 0·5 | 17 | 302 | RT-PCR | CD4 and CD8 cells, TNF, interleukins 4, 6, and 10 |
| Syphilis | ||||||
| Sadiq (2005)34 | Cohort | 6 | 104 | 485 | RT-PCR | CD4, seminal HIV RNA |
Unless otherwise indicated. bDNA=branched DNA. NASBA=nucleic-acid sequence-based assay. RCT=randomised controlled trial. RT-PCR=real-time PCR. TNF=tumour necrosis factor.
Figure 2. Changes in HIV-1 RNA concentration (log10 copies per mL) after treatment of co-infection (18 studies).
*For the four studies without variance data published or provided,10,11,24,36 SMDs and 95% CIs were calculated on the basis of the average variability found in the other studies. SMD=standardised mean difference.
In a US cohort of HIV-infected adults with culture-positive Mycobacterium tuberculosis, Goletti and colleagues6 noted that HIV-RNA concentrations increased by 0·7–2·2 log10 copies per mL during the acute phase of infection, and decreased by a similar order of magnitude at 3 months and 10 months after therapy. Despite a small sample size (n=10), the variability of viral-load measurements was relatively small. Similar results, but of smaller magnitude, were found in the study by Kizza and colleagues,24 in which viral load declined by 0·5 log10 copies per mL at 6 months after successful completion of tuberculosis therapy, but by only 0·2 log10 copies per mL when compared with 12-month follow-up timepoints.
In a prospective study of 47 HIV-infected Malawians, Hoffman and colleagues11 found that median HIV-RNA concentrations in the plasma of malaria-infected patients were 0·83 log10 copies per mL higher than those of individuals without smear-positive malaria. The change in plasma viral load also differed between the two groups: co-infected patients had a 0·25 log10 copies per mL reduction compared to a 0·04 log10 copies per mL increase among controls. Kublin and colleagues12 noted a comparatively smaller reduction in viral load with successful malaria elimination (−0·10 log10 copies per mL), but a nearly identical standardised viral-load reduction (−0·30 log10 copies per mL) to that reported by Hoffman and colleagues.11
Wolday and colleagues32 found that treatment of enteric helminth infection was associated with a 0·36 log10 copies per mL decline in HIV plasma viral load in co-infected individuals, and that mean baseline plasma HIV-RNA concentrations were associated with the intensity of helminth infection. A viral-load increase of 0·14 log10 copies per mL in the control group and a narrow variance of that change showed a −2·10 log10 copies per mL SMD. Much more modest reductions in viral load (<0·2 log10 copies per mL) with anthelmintic treatment were seen in subsequent studies.25,29,30 Among these four studies, more than 90% of study participants were infected with one or more of the following helminth species: Ascaris lumbricoides, Trichuris trichiura, Necator americanus, and Ancylostoma duodenale. Two randomised trials that assessed the interaction between HIV and other types of helminths (schistosomes and filaria) showed a larger effect of 0·4 log10 copies per mL and 0·8 log10 copies per mL viral-load reduction after successful helminth clearance.7,31
Six studies reported on the effect of HSV suppression on plasma HIV-RNA concentrations. SMDs indicated that herpes suppression significantly reduces HIV viral load by 0·46–1.18 log10 copies per mL.10,26,27,33,35,36 Variance data were not available from two studies to calculate a true SMD.10,36 However, the published results showed significant declines of 0·14 log10 copies per mL and 0·25 log10 copies per mL, respectively, with HSV suppressive therapy.
Among a group of female sex workers in Kenya, plasma HIV-RNA concentrations decreased over the course of several months by 0·16 log10 copies per mL among those presenting with various sexually transmitted diseases (ie, gonococcal cervicitis, acute pelvic inflammatory disease, and genital herpes) and decreased over the same time period by 0·06 log10 copies per mL in sex workers with no apparent co-infection.28 Sadiq and colleagues34 found that HIV-RNA concentrations in both plasma compartments initially decreased with syphilis infection, but then increased almost to baseline after treatment.
Discussion
Our systematic review suggests that treatment of the major co-infections of the world’s HIV-infected populations would be likely to reduce HIV viral load at an individual and population level. Although most studies eligible for this Review showed significant reductions in viral load, several studies failed to show a clinically significant change that exceeds the inherent 0·2–0·3 log10 copies per mL fluctuation of viral-load measures.37–39 Nevertheless, our analysis showed a viral-load decline of at least 0·3 log10 copies per mL in ten of the 18 studies reviewed.6,7,24,26–28,31–33,35 In our previous systematic review,20 we found evidence that changes in plasma HIV-RNA concentrations of as little as 0·3–1·0 log10 copies per mL were associated with a large theoretical effect on the risk of viral transmission by heterosexual contact and time to an AIDS-defining event or death. Specifically, a 1·0 log10 copies per mL drop in plasma viral load corresponds to a halving of transmission risk and a 2-year delay in the development of AIDS. Treatment of co-infections prevalent among HIV-infected patients in low-income countries might therefore result in decreases in plasma HIV-RNA concentrations that are large enough to have a substantial public-health effect. In HIV-endemic areas in particular, expansion of primary-care services with diagnostic and therapeutic capabilities for common co-infections might be expected to help slow the HIV epidemic.
M tuberculosis is the most common serious co-infecting pathogen in HIV-infected patients living in low-income countries. Results from reviewed studies, although not entirely consistent, suggest that M tuberculosis increases HIV replicative activity. Additional studies have examined the effect of tuberculosis acquisition on HIV viral load. Whalen and colleagues40 reported an increase of 0·43 log10 copies per mL in 20 co-infected Ugandan adults 1 year after M tuberculosis diagnosis, but did not report post-treatment values. Day and colleagues41 found that tuberculosis infection, both pulmonary and disseminated, was associated with a 0·24 log10 copies per mL increase in viral load. Other studies have reported conflicting data on the association between tuberculosis acquisition and plasma HIV-RNA concentrations, but none of these studies included comparison groups.41–50
In-vivo studies of localised tuberculosis have also found that pleural HIV-RNA concentrations are increased by 0·6–1·0 log10 copies per mL when compared with plasma and lung segments with no evident disease.51,52 Results from these experimental studies agree with mathematical models that predict, under steady-state conditions for HIV replication and T-lymphocyte and macrophage turnover, an increase in HIV concentrations in co-infected people (three to ten times [0·5–1·0 log10 copies per mL] in one model) compared with those with HIV infection alone.53 The two studies from our current analysis are compatible with results of other investigations that did not meet our inclusion criteria. Although based on small numbers of patients, all the published studies are consistent in the direction and magnitude of effect of tuberculosis treatment on HIV viral load.
Experimental data suggest that Plasmodium falciparum infection might cause an increase in HIV replication through the induction of proinflammatory cytokines, and might increase susceptibility to HIV acquisition (ie, from mother to child) by upregulation of chemokine receptors.15,54 Human data on the direct effect of antimalarial treatment on HIV viral load have been more equivocal. In one study, 12 HIV-infected patients from China co-infected with Plasmodium vivax were found to have more than 1·0 log10 copies per mL rise in viral load, which, after giving antimalarial treatment, returned to baseline concentrations.55 Other studies from sub-Saharan Africa, where malaria incidence and mortality are among the highest in the world, have not shown the same effect.56 Two prevalence surveys and two ecological studies suggested a negligible effect of malaria co-infection on plasma HIV-RNA concentrations.57–60 Instead of defining cases by positive parasite identification on blood smear, the studies used surrogates of malaria infection, such as antibody response or period of endemicity. Thus, study inferences might be compromised by potential misclassification of cases.
Data on the interaction between plasmodial parasites and HIV in the placenta of African pregnant women have agreed more closely with the studies eligible for this Review. Results from primigravidae and multigravidae suggested that acute malaria significantly increases the likelihood of mother-to-child transmission of HIV.61–64 Nevertheless, the mechanism of increased transmission risk in this population is not well understood (ie, increased placental HIV-RNA concentration, disruption of placental architecture, localised inflammation resulting in the recruitment of infected T lymphocytes and macrophages). Therefore, these pregnancy-based reports do little to resolve the discrepancies among HIV–malaria co-infection studies.
Functional studies of immune effectors in HIV– helminth co-infected populations have shown a reduced capacity to mount T-cell-derived responses to various antigens.65 Results of in-vitro experiments and animal studies suggest that the diminution in cellular immune activity is attributable to a state of hyporesponsiveness and anergy, and to increased apoptotic activity of lymphocyte subsets.66,67 A hallmark characteristic of helminth-induced immune dysregulation is a shift from a T-helper type 1 to a predominantly T-helper type 2 cytokine profile.68 Specifically, investigators have found that increases in interleukins 4 and 10 are accompanied by reductions in the secretion of interferon γ and interleukin 12.13,68 Concomitant with this T-helper type 1 to 2 switch in cytokine pattern expression is an upregulation of HIV coreceptors CC chemokine receptor 5 and CXC chemokine receptor 4 on lymphocyte and monocyte subpopulations. This might suggest that chronically immune-activated individuals who are HIV uninfected might be more susceptible to HIV infection than are helminth-free individuals.69 Initial evidence from human populations has subsequently verified experimental data. After helminth infections were treated, patients’ immune profiles normalised, immunological responses to antiretroviral therapy improved, and rates of HIV disease progression slowed.68,70–72 Wolday and colleagues32 responded that immune activation caused by chronic helminthiasis might depend on the causal pathogen, burden of infection, and mode of interaction with host immunity.
By contrast, Lawn and colleagues8 did not find any association between treatment of schistosomiasis and reductions in plasma HIV-RNA concentrations in 30 co-infected Kenyan adults. Elliott and colleagues73 also failed to find a significant association between HIV viral load and a composite of helminth infections in a cohort of co-infected Ugandan adults, although these results came from a cross-sectional analysis that did not use a criterion standard of helminth detection, except for schistosomal infections, which constituted a quarter of the helminth-infected group.
Sexually transmitted infections are thought to increase the risk of HIV acquisition, primarily by facilitating transmission through inflammation and ulceration of the genital mucosa, but also by increasing concentrations of HIV RNA in the plasma and genital secretions of the infected transmitter.74–76 A meta-analysis of nine studies estimated that, for each 0·5 log10 copies per mL increment in seminal HIV-RNA concentrations, the probability of male-to-female heterosexual transmission doubled.77 This finding implies that reduction of systemic HIV-RNA concentrations leads to a reduced viral burden in the seminal compartment. The strength of the correlation between the two compartments might differ between populations and between co-infections and HIV status (and perhaps HIV subtype). In a large study of HIV-1-discordant couples, viral load declined after HSV-2 suppressive therapy, but transmission did not fall as predicted.36
By contrast, treatment of other viral co-infections (eg, hepatitis C virus, cytomegalovirus, and measles) might be less likely to result in reductions in plasma HIV viral load than examples presented thus far. Although studies have suggested that hepatitis C virus co-infection accelerates the natural course of HIV,78,79 the evidence is not strong enough for an association between hepatitis C virus infection and changes in surrogate markers of HIV disease progression.80–82 Other viruses have been shown to enhance, suppress, or have no effect on HIV replication,19,83,84 suggesting that the mechanism by which HIV and other viruses interact is likely to be multifactorial and species specific.
Visceral and cutaneous leishmaniasis, recognised as an important co-infection in Latin America, parts of southeast Asia, southern Europe, and the eastern Mediterranean, have also been implicated as cofactors in HIV progression. Studies have shown that leishmanial promastigotes induce HIV replication and cause a steady rise in serum HIV-RNA concentrations of co-infected patients.85–87 One study reported reductions in plasma HIV-RNA load after successful anti-leishmanial chemotherapy.88 Similarly, the acquisition of and convalescence from Pneumocystis jirovecii pneumonia, a common opportunistic fungus, has been found to correlate with a respective rise and subsequent decline in HIV-RNA concentrations.16,89
Conclusions
Despite compelling evidence from immunological studies that co-infections activate host immunity, which in turn enhances HIV replication, evidence that treatment of or recovery from co-infection reduces HIV viral load has been elusive. Results from studies that have assessed changes in HIV-RNA concentrations after successful treatment or suppression of a co-infection varied in magnitude from an increase of 0·04 log10 copies per mL to a reduction of 3·47 log10 copies per mL. Interpretation of most studies is impaired by small sample sizes, heterogeneous populations, and varying follow-up times. Therefore, a remaining question of primary importance is whether co-infections cause only bursts in immune activation and resultant plasma viraemia or whether they initiate sustained changes in the steady-state dynamics of HIV replication and host immunity.
If co-infections cause only transient spikes in viral load, they might have a negligible effect on prognosis and risk of transmission. Alternatively, co-infections might shift the so-called viral setpoint upward for months such that patients progress faster and become more infectious. Data from vaccine studies have suggested that routine immunisations might cause transient increases of plasma HIV RNA in patients with increased lymphocyte subsets and lymphoproliferative responses,90–97 but do not affect the patients’ disease course.98,99 We believe that there is an ethical obligation to treat patients in co-infection studies. Hence, natural history data are too limited to either support or refute the hypothesis that co-infections establish sustained increases in non-specific immune activity and consequent HIV viral load.
The evidence is consistent that treatment or suppression of co-infection reduces HIV viral load. Thus, we believe that there is a compelling case for improving primary care for HIV-infected patients to help prevent, diagnose, and treat important co-infections. For example, at the public-health level, tuberculosis programmes and mass deworming should be integrated into HIV care and public-health efforts. In global efforts to provide antiretroviral therapy, good primary care and systematic control of co-infections should be included as part of a reasonable care and prevention package, providing the obvious disease-specific benefits as well as the additional benefits of slowing HIV-related disease progression and its transmission to others.20
Acknowledgments
This work was supported by NIH grants T32GM00836, R03TW05929, and 5P30AI054999. Meredith Bortz assisted with copyediting.
Footnotes
Contributors
KM and SHV conceived the systematic review, identified eligible studies, abstracted relevant data, verified outcomes and analyses with each other, and co-wrote the paper. KM did the SMD analyses.
Conflicts of interest
We declare that we have no conflicts of interest.
Contributor Information
Kayvon Modjarrad, Department of Medicine, and Institute for Global Health, Vanderbilt University School of Medicine, Nashville, TN, USA.
Sten H Vermund, Department of Pediatrics, and Institute for Global Health, Vanderbilt University School of Medicine, Nashville, TN, USA.
References
- 1.WHO. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector. Geneva: World Health Organization; Progress report. 2009
- 2.Fauci AS. Multifactorial nature of human immunodeficiency virus disease: implications for therapy. Science. 1993;262:1011–1018. doi: 10.1126/science.8235617. [DOI] [PubMed] [Google Scholar]
- 3.Bentwich Z. Concurrent infections that rise the HIV viral load. J HIV Ther. 2003;8:72–75. [PubMed] [Google Scholar]
- 4.Stein DS. Herpes virus infections, HIV, and disease progression. AIDS Clin Care. 1995;7:11–14. 18. [PubMed] [Google Scholar]
- 5.Webster A. Cytomegalovirus as a possible cofactor in HIV disease progression. J Acquir Immune Defic Syndr. 1991;4 suppl 1:S47–S52. [PubMed] [Google Scholar]
- 6.Goletti D, Weissman D, Jackson RW, et al. Effect of Mycobacterium tuberculosis on HIV replication. Role of immune activation. J Immunol. 1996;157:1271–1278. [PubMed] [Google Scholar]
- 7.Kallestrup P, Zinyama R, Gomo E, et al. Schistosomiasis and HIV-1 infection in rural Zimbabwe: effect of treatment of schistosomiasis on CD4 cell count and plasma HIV-1 RNA load. J Infect Dis. 2005;192:1956–1961. doi: 10.1086/497696. [DOI] [PubMed] [Google Scholar]
- 8.Lawn SD, Karanja DM, Mwinzia P, et al. The effect of treatment of schistosomiasis on blood plasma HIV-1 RNA concentration in coinfected individuals. AIDS. 2000;14:2437–2443. doi: 10.1097/00002030-200011100-00004. [DOI] [PubMed] [Google Scholar]
- 9.Walson JL, John-Stewart G. Treatment of helminth co-infection in HIV-1 infected individuals in resource-limited settings. Cochrane Database Syst Rev. 2008;1:CD006419. doi: 10.1002/14651858.CD006419.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schacker T, Zeh J, Hu H, Shaughnessy M, Corey L. Changes in plasma human immunodeficiency virus type 1 RNA associated with herpes simplex virus reactivation and suppression. J Infect Dis. 2002;186:1718–1725. doi: 10.1086/345771. [DOI] [PubMed] [Google Scholar]
- 11.Hoffman IF, Jere CS, Taylor TE, et al. The effect of Plasmodium falciparum malaria on HIV-1 RNA blood plasma concentration. AIDS. 1999;13:487–494. doi: 10.1097/00002030-199903110-00007. [DOI] [PubMed] [Google Scholar]
- 12.Kublin JG, Patnaik P, Jere CS, et al. Effect of Plasmodium falciparum malaria on concentration of HIV-1-RNA in the blood of adults in rural Malawi: a prospective cohort study. Lancet. 2005;365:233–240. doi: 10.1016/S0140-6736(05)17743-5. [DOI] [PubMed] [Google Scholar]
- 13.Bentwich Z, Kalinkovich A, Weisman Z. Immune activation is a dominant factor in the pathogenesis of African AIDS. Immunol Today. 1995;16:187–191. doi: 10.1016/0167-5699(95)80119-7. [DOI] [PubMed] [Google Scholar]
- 14.Borkow G, Bentwich Z. Chronic immune activation associated with chronic helminthic and human immunodeficiency virus infections: role of hyporesponsiveness and anergy. Clin Microbiol Rev. 2004;17:1012–1030. doi: 10.1128/CMR.17.4.1012-1030.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pisell TL, Hoffman IF, Jere CS, et al. Immune activation and induction of HIV-1 replication within CD14 macrophages during acute Plasmodium falciparum malaria coinfection. AIDS. 2002;16:1503–1509. doi: 10.1097/00002030-200207260-00007. [DOI] [PubMed] [Google Scholar]
- 16.Sulkowski MS, Chaisson RE, Karp CL, Moore RD, Margolick JB, Quinn TC. The effect of acute infectious illnesses on plasma human immunodeficiency virus (HIV) type 1 load and the expression of serologic markers of immune activation among HIV-infected adults. J Infect Dis. 1998;178:1642–1648. doi: 10.1086/314491. [DOI] [PubMed] [Google Scholar]
- 17.Weissman D, Barker TD, Fauci AS. The efficiency of acute infection of CD4+ T cells is markedly enhanced in the setting of antigen-specific immune activation. J Exp Med. 1996;183:687–692. doi: 10.1084/jem.183.2.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Celum CL. The interaction between herpes simplex virus and human immunodeficiency virus. Herpes. 2004;11 suppl 1:36A–45A. [PubMed] [Google Scholar]
- 19.Mercader M, Nickoloff BJ, Foreman KE. Induction of human immunodeficiency virus 1 replication by human herpesvirus 8. Arch Pathol Lab Med. 2001;125:785–789. doi: 10.5858/2001-125-0785-IOHIVR. [DOI] [PubMed] [Google Scholar]
- 20.Modjarrad K, Chamot E, Vermund SH. Impact of small reductions in plasma HIV RNA levels on the risk of heterosexual transmission and disease progression. AIDS. 2008;22:2179–2185. doi: 10.1097/QAD.0b013e328312c756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 22.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 23.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 24.Kizza HM, Rodriguez B, Quinones-Mateu M, et al. Persistent replication of human immunodeficiency virus type 1 despite treatment of pulmonary tuberculosis in dually infected subjects. Clin Diagn Lab Immunol. 2005;12:1298–1304. doi: 10.1128/CDLI.12.11.1298-1304.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walson JL, Otieno PA, Mbuchi M, et al. Albendazole treatment of HIV-1 and helminth co-infection: a randomized, double-blind, placebo-controlled trial. AIDS. 2008;22:1601–1609. doi: 10.1097/QAD.0b013e32830a502e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nagot N, Ouedraogo A, Foulongne V, et al. Reduction of HIV-1 RNA levels with therapy to suppress herpes simplex virus. N Engl J Med. 2007;356:790–799. doi: 10.1056/NEJMoa062607. [DOI] [PubMed] [Google Scholar]
- 27.Zuckerman RA, Lucchetti A, Whittington WL, et al. Herpes simplex virus (HSV) suppression with valacyclovir reduces rectal and blood plasma HIV-1 levels in HIV-1/HSV-2-seropositive men: a randomized, double-blind, placebo-controlled crossover trial. J Infect Dis. 2007;196:1500–1508. doi: 10.1086/522523. [DOI] [PubMed] [Google Scholar]
- 28.Anzala AO, Simonsen JN, Kimani J, et al. Acute sexually transmitted infections increase human immunodeficiency virus type 1 plasma viremia, increase plasma type 2 cytokines, and decrease CD4 cell counts. J Infect Dis. 2000;182:459–466. doi: 10.1086/315733. [DOI] [PubMed] [Google Scholar]
- 29.Brown M, Kizza M, Watera C, et al. Helminth infection is not associated with faster progression of HIV disease in coinfected adults in Uganda. J Infect Dis. 2004;190:1869–1879. doi: 10.1086/425042. [DOI] [PubMed] [Google Scholar]
- 30.Modjarrad K, Zulu I, Redden DT, et al. Treatment of intestinal helminths does not reduce plasma concentrations of HIV-1 RNA in coinfected Zambian adults. J Infect Dis. 2005;192:1277–1283. doi: 10.1086/444543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nielsen NO, Friis H, Magnussen P, Krarup H, Magesa S, Simonsen PE. Co-infection with subclinical HIV and Wuchereria bancrofti, and the role of malaria and hookworms, in adult Tanzanians: infection intensities, CD4/CD8 counts and cytokine responses. Trans R Soc Trop Med Hyg. 2007;101:602–612. doi: 10.1016/j.trstmh.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 32.Wolday D, Mayaan S, Mariam ZG, et al. Treatment of intestinal worms is associated with decreased HIV plasma viral load. J Acquir Immune Defic Syndr. 2002;31:56–62. doi: 10.1097/00126334-200209010-00008. [DOI] [PubMed] [Google Scholar]
- 33.Baeten JM, Strick LB, Lucchetti A, et al. Herpes simplex virus (HSV)-suppressive therapy decreases plasma and genital HIV-1 levels in HSV-2/HIV-1 coinfected women: a randomized, placebo-controlled, cross-over trial. J Infect Dis. 2008;198:1804–1808. doi: 10.1086/593214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sadiq ST, McSorley J, Copas AJ, et al. The effects of early syphilis on CD4 counts and HIV-1 RNA viral loads in blood and semen. Sex Transm Infect. 2005;81:380–385. doi: 10.1136/sti.2004.012914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ouedraogo A, Nagot N, Vergne L, et al. Impact of suppressive herpes therapy on genital HIV-1 RNA among women taking antiretroviral therapy: a randomized controlled trial. AIDS. 2006;20:2305–2313. doi: 10.1097/QAD.0b013e328010238d. [DOI] [PubMed] [Google Scholar]
- 36.Celum C, Wald A, Lingappa JR, et al. Acyclovir and transmission of HIV-1 from persons infected with HIV-1 and HSV-2. N Engl J Med. 2010;362:427–439. doi: 10.1056/NEJMoa0904849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bartlett JA, DeMasi R, Dawson D, Hill A. Variability in repeated consecutive measurements of plasma human immunodeficiency virus RNA in persons receiving stable nucleoside reverse transcriptase inhibitor therapy or no treatment. J Infect Dis. 1998;178:1803–1805. doi: 10.1086/314503. [DOI] [PubMed] [Google Scholar]
- 38.Brambilla D, Reichelderfer PS, Bremer JW, et al. The contribution of assay variation and biological variation to the total variability of plasma HIV-1 RNA measurements. AIDS. 1999;13:2269–2279. doi: 10.1097/00002030-199911120-00009. [DOI] [PubMed] [Google Scholar]
- 39.Yamashita TE, Modjarrad K, Munoz A. Variability of HIV-1 RNA before AIDS and highly active antiretroviral therapy. AIDS. 2003;17:1264–1266. doi: 10.1097/00002030-200305230-00023. [DOI] [PubMed] [Google Scholar]
- 40.Whalen CC, Nsubuga P, Okwera A, et al. Impact of pulmonary tuberculosis on survival of HIV-infected adults: a prospective epidemiologic study in Uganda. AIDS. 2000;14:1219–1228. doi: 10.1097/00002030-200006160-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Day JH, Grant AD, Fielding KL, et al. Does tuberculosis increase HIV load? J Infect Dis. 2004;190:1677–1684. doi: 10.1086/424851. [DOI] [PubMed] [Google Scholar]
- 42.Collins KR, Quinones-Mateu ME, Toossi Z, Arts EJ. Impact of tuberculosis on HIV-1 replication, diversity, and disease progression. AIDS Rev. 2002;4:165–176. [PubMed] [Google Scholar]
- 43.Corbett EL, De Cock KM. The clinical significance of interactions between HIV and TB: more questions than answers. Int J Tuberc Lung Dis. 2001;5:205–207. [PubMed] [Google Scholar]
- 44.Del Amo J, Malin AS, Pozniak A, De Cock KM. Does tuberculosis accelerate the progression of HIV disease? Evidence from basic science and epidemiology. AIDS. 1999;13:1151–1158. doi: 10.1097/00002030-199907090-00002. [DOI] [PubMed] [Google Scholar]
- 45.Hoshino Y, Tse DB, Rochford G, et al. Mycobacterium tuberculosis-induced CXCR4 and chemokine expression leads to preferential X4 HIV-1 replication in human macrophages. J Immunol. 2004;172:6251–6258. doi: 10.4049/jimmunol.172.10.6251. [DOI] [PubMed] [Google Scholar]
- 46.Kalou M, Sassan-Morokro M, Abouya L, et al. Changes in HIV RNA viral load, CD4+ T-cell counts, and levels of immune activation markers associated with anti-tuberculosis therapy and cotrimoxazole prophylaxis among HIV-infected tuberculosis patients in Abidjan, Cote d’Ivoire. J Med Virol. 2005;75:202–208. doi: 10.1002/jmv.20257. [DOI] [PubMed] [Google Scholar]
- 47.Lawn SD, Shattock RJ, Acheampong JW, et al. Sustained plasma TNF-alpha and HIV-1 load despite resolution of other parameters of immune activation during treatment of tuberculosis in Africans. AIDS. 1999;13:2231–2237. doi: 10.1097/00002030-199911120-00005. [DOI] [PubMed] [Google Scholar]
- 48.Morris L, Martin DJ, Bredell H, et al. Human immunodeficiency virus-1 RNA levels and CD4 lymphocyte counts, during treatment for active tuberculosis, in South African patients. J Infect Dis. 2003;187:1967–1971. doi: 10.1086/375346. [DOI] [PubMed] [Google Scholar]
- 49.Schon T, Wolday D, Elias D, et al. Kinetics of sedimentation rate, viral load and TNF-alpha in relation to HIV co-infection in tuberculosis. Trans R Soc Trop Med Hyg. 2006;100:483–488. doi: 10.1016/j.trstmh.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 50.Toossi Z, Mayanja-Kizza H, Hirsch CS, et al. Impact of tuberculosis (TB) on HIV-1 activity in dually infected patients. Clin Exp Immunol. 2001;123:233–238. doi: 10.1046/j.1365-2249.2001.01401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lawn SD, Pisell TL, Hirsch CS, Wu M, Butera ST, Toossi Z. Anatomically compartmentalized human immunodeficiency virus replication in HLA-DR+ cells and CD14+ macrophages at the site of pleural tuberculosis coinfection. J Infect Dis. 2001;184:1127–1133. doi: 10.1086/323649. [DOI] [PubMed] [Google Scholar]
- 52.Nakata K, Rom WN, Honda Y, et al. Mycobacterium tuberculosis enhances human immunodeficiency virus-1 replication in the lung. Am J Respir Crit Care Med. 1997;155:996–1003. doi: 10.1164/ajrccm.155.3.9117038. [DOI] [PubMed] [Google Scholar]
- 53.Kirschner D. Dynamics of co-infection with M tuberculosis and HIV-1. Theor Popul Biol. 1999;55:94–109. doi: 10.1006/tpbi.1998.1382. [DOI] [PubMed] [Google Scholar]
- 54.Xiao L, Owen SM, Rudolph DL, Lal RB, Lal AA. Plasmodium falciparum antigen-induced human immunodeficiency virus type 1 replication is mediated through induction of tumor necrosis factor-alpha. J Infect Dis. 1998;177:437–445. doi: 10.1086/514212. [DOI] [PubMed] [Google Scholar]
- 55.Chen X, Xiao B, Shi W, et al. Impact of acute vivax malaria on the immune system and viral load of HIV-positive subjects. Chin Med J (Engl) 2003;116:1810–1820. [PubMed] [Google Scholar]
- 56.WHO. [accessed April 29, 2010];Malaria and HIV/AIDS interactions and implications: conclusions of a technical consultation convened by WHO, 23–25 June, 2004. WHO/HIV/2004.8. http://whqlibdoc.who.int/hq/2004/WHO_HIV_2004.08_eng.pdf.
- 57.Ariyoshi K, Schim van der Loeff M, Berry N, Jaffar S, Whittle H. Plasma HIV viral load in relation to season and to Plasmodium falciparum parasitaemia. AIDS. 1999;13:1145–1146. doi: 10.1097/00002030-199906180-00023. [DOI] [PubMed] [Google Scholar]
- 58.Ayouba A, Nerrienet E, Menu E, et al. Mother-to-child transmission of human immunodeficiency virus type 1 in relation to the season in Yaounde, Cameroon. Am J Trop Med Hyg. 2003;69:447–449. [PubMed] [Google Scholar]
- 59.Inion I, Mwanyumba F, Gaillard P, et al. Placental malaria and perinatal transmission of human immunodeficiency virus type 1. J Infect Dis. 2003;188:1675–1678. doi: 10.1086/379737. [DOI] [PubMed] [Google Scholar]
- 60.Kashamuka M, Nzila N, Mussey L, et al. Short report: analysis of anti-malaria immune response during human immunodeficiency virus infection in adults in Kinshasa, Democratic Republic of the Congo. Am J Trop Med Hyg. 2003;68:376–378. [PubMed] [Google Scholar]
- 61.Ayisi JG, van Eijk AM, Newman RD, et al. Maternal malaria and perinatal HIV transmission, western Kenya. Emerg Infect Dis. 2004;10:643–652. doi: 10.3201/eid1004.030303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Brahmbhatt H, Kigozi G, Wabwire-Mangen F, et al. The effects of placental malaria on mother-to-child HIV transmission in Rakai, Uganda. AIDS. 2003;17:2539–2541. doi: 10.1097/00002030-200311210-00020. [DOI] [PubMed] [Google Scholar]
- 63.Brahmbhatt H, Sullivan D, Kigozi G, et al. Association of HIV and malaria with mother-to-child transmission, birth outcomes, and child mortality. J Acquir Immune Defic Syndr. 2008;47:472–476. doi: 10.1097/QAI.0b013e318162afe0. [DOI] [PubMed] [Google Scholar]
- 64.Kapiga SH, Bang H, Spiegelman D, et al. Correlates of plasma HIV-1 RNA viral load among HIV-1-seropositive women in Dar es Salaam, Tanzania. J Acquir Immune Defic Syndr. 2002;30:316–323. doi: 10.1097/00126334-200207010-00008. [DOI] [PubMed] [Google Scholar]
- 65.Borkow G, Leng Q, Weisman Z, et al. Chronic immune activation associated with intestinal helminth infections results in impaired signal transduction and anergy. J Clin Invest. 2000;106:1053–1060. doi: 10.1172/JCI10182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kalinkovich A, Weisman Z, Bentwich Z. Chemokines and chemokine receptors: role in HIV infection. Immunol Lett. 1999;68:281–287. doi: 10.1016/s0165-2478(99)00059-0. [DOI] [PubMed] [Google Scholar]
- 67.Messele T, Abdulkadir M, Fontanet AL, et al. Reduced naive and increased activated CD4 and CD8 cells in healthy adult Ethiopians compared with their Dutch counterparts. Clin Exp Immunol. 1999;115:443–450. doi: 10.1046/j.1365-2249.1999.00815.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bentwich Z, Weisman Z, Moroz C, Bar-Yehuda S, Kalinkovich A. Immune dysregulation in Ethiopian immigrants in Israel: relevance to helminth infections? Clin Exp Immunol. 1996;103:239–243. doi: 10.1046/j.1365-2249.1996.d01-612.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kalinkovich A, Borkow G, Weisman Z, Tsimanis A, Stein M, Bentwich Z. Increased CCR5 and CXCR4 expression in Ethiopians living in Israel: environmental and constitutive factors. Clin Immunol. 2001;100:107–117. doi: 10.1006/clim.2001.5040. [DOI] [PubMed] [Google Scholar]
- 70.Bentwich Z. Good worms or bad worms: do worm infections affect the epidemiological patterns of other diseases? Parasitol Today. 2000;16:312. doi: 10.1016/s0169-4758(00)01693-8. [DOI] [PubMed] [Google Scholar]
- 71.Galai N, Kalinkovich A, Burstein R, Vlahov D, Bentwich Z. African HIV-1 subtype C and rate of progression among Ethiopian immigrants in Israel. Lancet. 1997;349:180–181. doi: 10.1016/S0140-6736(05)60982-8. [DOI] [PubMed] [Google Scholar]
- 72.Weisman Z, Kalinkovich A, Borkow G, Stein M, Greenberg Z, Bentwich Z. Infection by different HIV-1 subtypes (B and C) results in a similar immune activation profile despite distinct immune backgrounds. J Acquir Immune Defic Syndr. 1999;21:157–163. [PubMed] [Google Scholar]
- 73.Elliott AM, Mawa PA, Joseph S, et al. Associations between helminth infection and CD4+ T cell count, viral load and cytokine responses in HIV-1-infected Ugandan adults. Trans R Soc Trop Med Hyg. 2003;97:103–108. doi: 10.1016/s0035-9203(03)90040-x. [DOI] [PubMed] [Google Scholar]
- 74.Gray RH, Wawer MJ, Brookmeyer R, et al. Probability of HIV-1 transmission per coital act in monogamous, heterosexual, HIV-1-discordant couples in Rakai, Uganda. Lancet. 2001;357:1149–1153. doi: 10.1016/S0140-6736(00)04331-2. [DOI] [PubMed] [Google Scholar]
- 75.Grosskurth H, Mosha F, Todd J, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: randomised controlled trial. Lancet. 1995;346:530–536. doi: 10.1016/s0140-6736(95)91380-7. [DOI] [PubMed] [Google Scholar]
- 76.Rotchford K, Strum AW, Wilkinson D. Effect of coinfection with STDs and of STD treatment on HIV shedding in genital-tract secretions: systematic review and data synthesis. Sex Transm Dis. 2000;27:243–248. doi: 10.1097/00007435-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 77.Chakraborty H, Sen PK, Helms RW, et al. Viral burden in genital secretions determines male-to-female sexual transmission of HIV-1: a probabilistic empiric model. AIDS. 2001;15:621–627. doi: 10.1097/00002030-200103300-00012. [DOI] [PubMed] [Google Scholar]
- 78.Sabin CA, Telfer P, Phillips AN, Bhagani S, Lee CA. The association between hepatitis C virus genotype and human immunodeficiency virus disease progression in a cohort of hemophilic men. J Infect Dis. 1997;175:164–168. doi: 10.1093/infdis/175.1.164. [DOI] [PubMed] [Google Scholar]
- 79.Zylberberg H, Pol S. Reciprocal interactions between human immunodeficiency virus and hepatitis C virus infections. Clin Infect Dis. 1996;23:1117–1125. doi: 10.1093/clinids/23.5.1117. [DOI] [PubMed] [Google Scholar]
- 80.Brau N. Update on chronic hepatitis C in HIV/HCV-coinfected patients: viral interactions and therapy. AIDS. 2003;17:2279–2290. doi: 10.1097/00002030-200311070-00002. [DOI] [PubMed] [Google Scholar]
- 81.Negredo E, Domingo P, Sambeat MA, Rabella N, Vazquez G. Influence of coinfection with hepatitis viruses on human immunodeficiency plasma viral load. Arch Intern Med. 1999;159:2367–2368. doi: 10.1001/archinte.159.19.2367. [DOI] [PubMed] [Google Scholar]
- 82.Sabin CA. Hepatitis C virus and HIV coinfection. AIDS Patient Care STDs. 1998;12:199–207. doi: 10.1089/apc.1998.12.199. [DOI] [PubMed] [Google Scholar]
- 83.Jere C, Cunliffe NA, Hoffman IF, et al. Plasma HIV burden in Malawian children co-infected with rotavirus. AIDS. 2001;15:1439–1442. doi: 10.1097/00002030-200107270-00016. [DOI] [PubMed] [Google Scholar]
- 84.Lefrere JJ, Roudot-Thoraval F, Morand-Joubert L, et al. Carriage of GB virus C/hepatitis G virus RNA is associated with a slower immunologic, virologic, and clinical progression of human immunodeficiency virus disease in coinfected persons. J Infect Dis. 1999;179:783–789. doi: 10.1086/314671. [DOI] [PubMed] [Google Scholar]
- 85.Pintado V, Martin-Rabadan P, Rivera ML, Moreno S, Bouza E. Visceral leishmaniasis in human immunodeficiency virus (HIV)-infected and non-HIV-infected patients. A comparative study. Medicine (Baltimore) 2001;80:54–73. doi: 10.1097/00005792-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 86.Preiser W, Cacopardo B, Nigro L, et al. Immunological findings in HIV-Leishmania coinfection. Intervirology. 1996;39:285–288. doi: 10.1159/000150531. [DOI] [PubMed] [Google Scholar]
- 87.Zhao C, Papadopoulou B, Tremblay MJ. Leishmania infantum enhances human immunodeficiency virus type-1 replication in primary human macrophages through a complex cytokine network. Clin Immunol. 2004;113:81–88. doi: 10.1016/j.clim.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 88.Berhe N, Wolday D, Hailu A, et al. HIV viral load and response to antileishmanial chemotherapy in co-infected patients. AIDS. 1999;13:1921–1925. doi: 10.1097/00002030-199910010-00015. [DOI] [PubMed] [Google Scholar]
- 89.Shaunak S, Veryard C, Javan C. Severe Pneumocystis carinii pneumonia increases the infectious titre of HIV-1 in blood and can promote the expansion of viral chemokine co-receptor tropism. J Infect. 2001;43:3–6. doi: 10.1053/jinf.2001.0885. [DOI] [PubMed] [Google Scholar]
- 90.Brichacek B, Swindells S, Janoff EN, Pirruccello S, Stevenson M. Increased plasma human immunodeficiency virus type 1 burden following antigenic challenge with pneumococcal vaccine. J Infect Dis. 1996;174:1191–1199. doi: 10.1093/infdis/174.6.1191. [DOI] [PubMed] [Google Scholar]
- 91.Couch RB. Influenza, influenza virus vaccine, and human immunodeficiency virus infection. Clin Infect Dis. 1999;28:548–551. doi: 10.1086/515171. [DOI] [PubMed] [Google Scholar]
- 92.Donovan RM, Moore E, Bush CE, Markowitz NP, Saravolatz LD. Changes in plasma HIV RNA levels and CD4 cell counts after vaccination of pediatric patients. AIDS. 1997;11:1054–1056. [PubMed] [Google Scholar]
- 93.Ho DD. HIV-1 viraemia and influenza. Lancet. 1992;339:1549. doi: 10.1016/0140-6736(92)91321-x. [DOI] [PubMed] [Google Scholar]
- 94.O’Brien WA, Grovit-Ferbas K, Namazi A, et al. Human immunodeficiency virus-type 1 replication can be increased in peripheral blood of seropositive patients after influenza vaccination. Blood. 1995;86:1082–1089. [PubMed] [Google Scholar]
- 95.Ramilo O, Hicks PJ, Borvak J, et al. T cell activation and human immunodeficiency virus replication after influenza immunization of infected children. Pediatr Infect Dis J. 1996;15:197–203. doi: 10.1097/00006454-199603000-00004. [DOI] [PubMed] [Google Scholar]
- 96.Stanley SK, Ostrowski MA, Justement JS, et al. Effect of immunization with a common recall antigen on viral expression in patients infected with human immunodeficiency virus type 1. N Engl J Med. 1996;334:1222–1230. doi: 10.1056/NEJM199605093341903. [DOI] [PubMed] [Google Scholar]
- 97.Vigano A, Bricalli D, Trabattoni D, et al. Immunization with both T cell-dependent and T cell-independent vaccines augments HIV viral load secondarily to stimulation of tumor necrosis factor α. AIDS Res Hum Retroviruses. 1998;14:727–734. doi: 10.1089/aid.1998.14.727. [DOI] [PubMed] [Google Scholar]
- 98.Schneider RF, Rosen MJ. Pneumococcal infections in HIV-infected adults. Semin Respir Infect. 1999;14:237–242. [PubMed] [Google Scholar]
- 99.Zanetti AR, Amendola A, Besana S, Boschini A, Tanzi E. Safety and immunogenicity of influenza vaccination in individuals infected with HIV. Vaccine. 2002;20 suppl 5:B29–B32. doi: 10.1016/s0264-410x(02)00511-x. [DOI] [PubMed] [Google Scholar]