Abstract
Purpose
To report surgical results of canaloplasty surgery for primary open-angle glaucoma (POAG) in Japanese patients.
Methods
Eleven eyes of 9 POAG patients underwent canalopasty surgery at Toyama University Hospital. Three eyes of 3 patients underwent canaloplasty alone and 8 eyes of 6 patients underwent canaloplasty combined with cataract surgery. Canaloplasty was performed with a 10-0 polypropylene tensioning suture and an iTrack™ 250A microcatheter. All patients were followed up for 12 months. Changes in intraocular pressure (IOP) and postoperative complications were examined.
Results
Mean preoperative IOP was 23.4 ± 5.5 mm Hg. Mean number of antiglaucoma drops was 2.8 ± 0.6 before canaloplasty and decreased to 1.2 ± 0.8 at 12 months after canaloplasty (p < 0.01). Mean IOP decreased postoperatively, being 13.7 ± 2.8 mm Hg at 1 month, 12.8 ± 3.5 mm Hg at 3 months, 14.0 ± 4.4 mm Hg at 6 months, and 15.0 ± 4.1 mm Hg at 12 months. The most frequent postoperative complication was mild hyphema (45.5%), which disappeared within 14 days after surgery.
Conclusions
Canaloplasty may be an alternative surgery for POAG patients to reduce IOP to a value of approximately 15 mm Hg.
Key Words: Canaloplasty, Primary open-angle glaucoma, Intraocular pressure, Complications
Introduction
Canaloplasty is a new nonpenetrating glaucoma surgery that is expected to increase physiological aqueous outflow from the anterior chamber through the trabeculo-Descemet's window into Schlemm's canal [1, 2]. Using the flexible iTrack™ 250A microcatheter (iScience Interventional, Menlo Park, Calif., USA), designed especially for canaloplasty, 10-0 polypropylene tensioning suture is installed into Schlemm's canal circumferentially. Canaloplasty is not widely performed in Japan. We studied the surgical results of canaloplasty surgery for Japanese primary open-angle glaucoma (POAG) patients.
Case Report
Nine patients (11 eyes) of POAG treated at Toyama University Hospital between December 2008 and June 2009 were included in this study. Three eyes of 3 patients underwent canaloplasty alone and 8 eyes of 6 patients underwent canaloplasty combined with phacoemulsification/aspiration and intraocular lens implantation (PEA + IOL).
This study was approved by the Institutional Review Board of the University of Toyama. Written informed consent was obtained from each of the patients after they were provided with sufficient information about the procedures.
The mean age of the patients was 71.7 ± 8.5 years (mean ± standard deviation). The mean preoperative intraocular pressure (IOP) was 23.4 ± 5.5 mm Hg. The mean number of antiglaucoma drops used before canaloplasty was 2.8 ± 0.6.
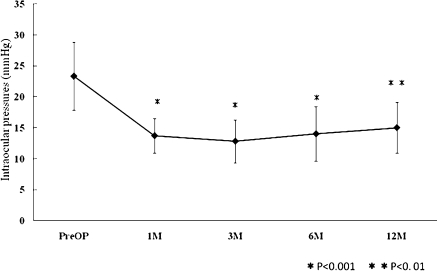
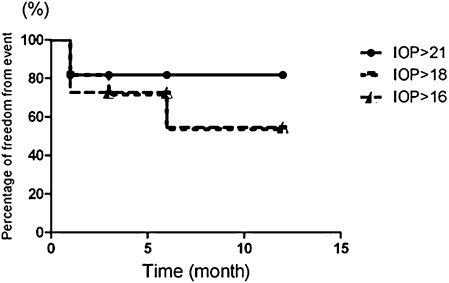
All patients who underwent canaloplasty alone had undergone cataract surgery previously. Surgical techniques were as follows. Briefly, after limbal conjunctival peritomy, a superficial parabolic flap approximately 4 mm wide and 5 mm long was created at the 12 o'clock limbus. Then a deep flap was created within the margin of the superficial flap. PEA + IOL were performed from beneath the superficial flap. The deep flap was excised and a trabeculo-Descemet's window was formed. After injection of viscoelastic material into the ostia of Schlemm's canal, 10-0 polypropylene tensioning suture was installed using an iTrack 250A microcatheter. The superficial flap and the conjunctiva were closed in a watertight manner. The IOP was measured at 1, 3, 6, and 12 months postoperatively. Mean IOPs were 13.7 ± 2.8 mm Hg at 1 month, 12.8 ± 3.5 mm Hg at 3 months, 14.0 ± 4.4 mm Hg at 6 months, and 15.0 ± 4.1 mm Hg at 12 months (fig. 1). Statistical analysis was carried out by a paired t test and Dunn's multiple comparison analysis. All postoperative mean IOPs were significantly decreased compared to the preoperative IOP of 23.4 ± 5.5 mm Hg (p < 0.001 or p < 0.01). fig. 2 shows an image of the anterior segment optical coherence tomography (CASIA; Tomey Corporation, Nagoya, Japan), which indicated the tensioned and dilated Schlemm's canal (arrows) at 12 months after canaloplasty surgery. A Kaplan-Meier survival model was used for cumulative probability of qualified success with or without medications (fig. 3). The qualified success rate of an IOP of 21, 18, and 16 mm Hg or less at 12 months was 81.8, 54.5, and 54.5%, respectively (fig. 3). The mean postoperative number of antiglaucoma drops was significantly reduced to 1.2 ± 0.8 (p < 0.01). Postoperative complications are shown in table 1. The most frequent postoperative complication was mild hyphema (45.5%), which disappeared within 14 days after the surgery without detrimental effect.
Fig. 1.
Changes of mean IOP after canaloplasty surgery.
Fig. 2.
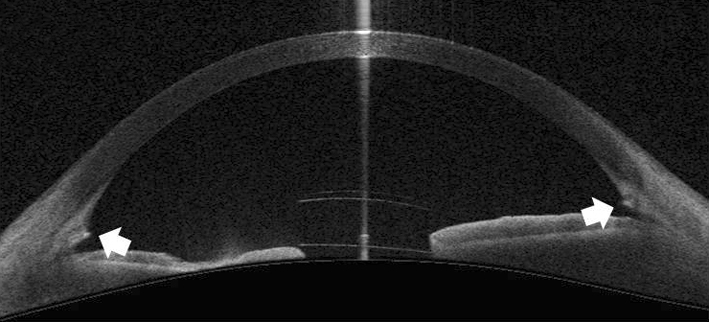
A horizontal image of anterior segment optical coherence tomography of a patient 12 months after canaloplasty surgery. Arrows show the tensioned and dilated Schlemm's canal.
Fig. 3.
Kaplan-Meier analysis for IOP.
Table 1.
Postoperative complications in canaloplasty surgery
| Hyphema | 5/11 eyes |
| Intraocular pressure spike (>30 mm Hg) | 2/11 eyes |
| Descemet's membrane detachment | 1/11 eyes |
| Prolapse of 10-0 prolene into anterior chamber | 1/11 eyes |
| Mild vitreous hemorrhage | 1/11 eyes |
Discussion
We have previously reported on the feasibility of canaloplasty in Japan [3]. Grieshaber et al. [4] reported the long-term outcomes of canaloplasty for POAG in black African patients. Their mean postoperative IOP was 15.4 ± 5.2 mm Hg at 12 months. We showed a similar mean postoperative IOP of 15.0 ± 4.1 mm Hg at 12 months after canaloplasty. Because this was a retrospective study, we could show only qualified success rates. Canaloplasty reduced the mean postoperative number of antiglaucoma drops and it may be suitable to reduce the IOP to a value of approximately 15 mm Hg.
No serious intraoperative or postoperative complications were experienced in our study. Mild hyphema was the most frequent postoperative complication (45.5%). During the installation of the iTrack 250A microcatheter into Schlemm's canal, mild bleeding from the trabecular tissue into the anterior chamber was frequently found. Microperforation of the trabecular meshwork might occur during the catheterization. Koch et al. [5] reported that anterior chamber hemorrhage with hyphema was found in 15 of 21 eyes (71.4%) on day 1 after canaloplasty, and the eyes without hyphema showed higher IOP than those with hyphema. It is possible that microperforation may be one of the mechanisms of IOP reduction by canaloplasty surgery.
Although long-term results of canaloplasty have not been clarified yet, canaloplasty may be an alternative method for Japanese patients with POAG when the desired pressure is around 15 mm Hg.
Disclosure Statement
The authors have no financial/conflicting interests to disclose.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Lewis RA, von Wolff K, Tetz M, et al. Canaloplasty: circumferential viscodilation and tensioning of Schlemm's canal using a flexible microcatheter for the treatment of open-angle glaucoma in adults: interim clinical study analysis. J Cataract Refract Surg. 2007;33:1217–1226. doi: 10.1016/j.jcrs.2007.03.051. [DOI] [PubMed] [Google Scholar]
- 2.Shingleton B, Tetz M, Korber N. Circumferential viscodilation and tensioning of Schlemm canal (canaloplasty) with temporal clear corneal phacoemulsification cataract surgery for open-angle glaucoma and visually significant cataract: one-year results. J Cataract Refract Surg. 2008;34:433–440. doi: 10.1016/j.jcrs.2007.11.029. [DOI] [PubMed] [Google Scholar]
- 3.Kitagawa K, Hayashi A. Clinical trial of a flexible microcatheter iTrack 250A for canaloplasty. Folia Japonica de Ophthalmologica Clinica. 2009;2:924–928. [Google Scholar]
- 4.Grieshaber MC, Pienaar A, Olivier J, Stegmann R. Canaloplasty for primary open-angle glaucoma: long-term outcome. Br J Ophthalmol. 2010;94:1478–1482. doi: 10.1136/bjo.2009.163170. [DOI] [PubMed] [Google Scholar]
- 5.Koch JM, Heiligenhaus A, Heinz C: Canaloplasty and transient anterior chamber haemorrhage: a prognostic factor? Klin Monbl Augenheilkd 2010, Epub ahead of print. [DOI] [PubMed]